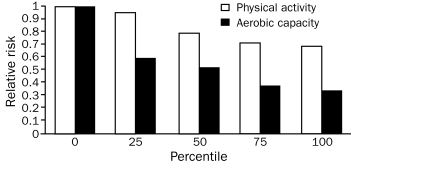
Guidelines and recommendations for conventional coronary risk factors are widely available, as are clinically relevant threshold values for the treatment of hypertension, cholesterol and its subfractions, overweight/obesity, and impaired fasting glucose. Although increasing levels of physical activity and aerobic capacity (cardiorespiratory fitness) are widely believed to be cardioprotective, Williams1 reported that these variables have significantly different associations with cardiovascular disease. Regarding physical activity (independent of aerobic fitness), the risk of cardiovascular disease decreased linearly when plotted as a function of the cumulative percentages of the samples ranked from least active to most active (Figure). However, when analyzed according to aerobic fitness, there was a precipitous decrease in cardiovascular disease risk when comparing the lowest (0) to the next-lowest (ie, 25th percentile) fitness category. Beyond this demarcation in aerobic fitness category, the reductions in relative risk paralleled those observed with increasing physical activity alone. Accordingly, there was a 64% decrease in the risk of heart disease from the least to the most aerobically fit and a 30% decrease from the least to the most physically active. It was concluded that being unfit (the least fit cohort) warrants consideration as an independent risk factor for coronary heart disease and deserves screening and intervention.
FIGURE.
The risks of coronary heart disease and cardiovascular disease decrease linearly in association with increasing percentiles of physical activity. In contrast, there is a precipitous decrease in risk when comparing the lowest to the next-lowest category for aerobic capacity. Beyond this demarcation, the reductions in risk parallel those observed with increasing physical activity but are essentially twice as great for aerobic capacity (cardiorespiratory fitness). Data from Med Sci Sports Exerc.1
Numerous epidemiological studies in apparently healthy men and women, those with comorbid conditions (eg, overweight/obesity, hypertension, type 2 diabetes mellitus), and those with suspected or known coronary artery disease have now identified a low level of aerobic fitness, expressed as metabolic equivalents (METs; 1 MET = a whole-body oxygen consumption of 3.5 mL O2/kg/min), as an independent risk factor for all-cause and cardiovascular mortality.2-10 Low-fit participants were approximately 2 to 5 times more likely to die during follow-up compared with their more fit counterparts. The study by Lyerly et al,11 published in the current issue of Mayo Clinic Proceedings, extends these analyses to a cohort at increased risk of cardiovascular disease, that is, middle-aged women with impaired fasting glucose (100.0-125.9 mg/dL; to convert to mmol/L, multiply by 0.0555) or previously undiagnosed diabetes (fasting glucose ≥126 mg/dL), with specific reference to the modulating influence of overweight/obesity as reflected by body mass index (BMI; computed as weight in kilograms divided by height in meters squared).
To evaluate the isolated and combined associations of aerobic fitness and BMI on the risk of mortality in women with impaired fasting glucose or undiagnosed diabetes, Lyerly et al conducted a retrospective analysis of data from the Aerobics Center Longitudinal Study of 3044 apparently healthy women (mean age, 47.4 years) who underwent preventive medical examinations, including a maximal treadmill exercise test (January 26, 1971-March 21, 2001). None of the study patients had previous cardiovascular events or a history of diabetes mellitus at baseline. Cardiorespiratory fitness was estimated from the attained speed, grade, and duration of maximal treadmill testing to volitional exhaustion or adverse signs/symptoms. Patients were categorized into age-adjusted low (bottom 20%), moderate (next 40%), or high (most fit 40%) groups.
See also page 780
During a mean follow-up of 15.6 years, 171 deaths were recorded. Those who died tended to be older, had lower levels of age-adjusted cardiorespiratory fitness, and were more likely to have major risk factors (ie, cigarette smoking, hypertension, hypercholesterolemia) compared with survivors. Accordingly, there was an inverse association between cardiorespiratory fitness, expressed as METs, and all-cause mortality, even after adjusting for potential confounding variables. An exercise capacity less than 7 METs was associated with a 1.5-fold higher risk of death compared with 9 or more METs (Ptrend=.05). Death rates in overweight/obese unfit (bottom 20%) women were more than double those in fit women (moderate and high cardiorespiratory fitness) with BMI of 25 kg/m2 or higher. In contrast, there was no association between overweight or obesity and overall deaths in this cohort of women with impaired fasting glucose or previously undiagnosed diabetes.
Fitness and Mortality in Women
One of the seminal epidemiological studies to examine the association between cardiorespiratory fitness and all-cause mortality involved 3120 apparently healthy women who underwent a medical examination and a progressive treadmill test to estimate aerobic capacity.2 During an average follow-up of slightly more than 8 years, 43 women died. In general, the higher the initial level of aerobic fitness, the lower the subsequent death rate from cancer and heart disease. In agreement with the findings of Lyerly et al,11 women with an aerobic capacity of 9 METs or greater had the lowest mortality rate.
Blair et al3 examined the relative risk for all-cause mortality for 4 major risk factors (ie, current or recent cigarette smoking, systolic hypertension [blood pressure ≥140 mm Hg], hypercholesterolemia [cholesterol level ≥240 mg/dL; to convert to mmol/L, multiply by 0.0259], BMI ≥27 kg/m2), as well as low aerobic fitness (20% least fit) in 7080 women who underwent preventive medical examinations. The average follow-up interval was 8.4 years. Unfit women were 2.23 times as likely to die during follow-up compared with their fit counterparts. Two provocative findings emerged: moderate fitness seemed to protect against the influence of other risk factors on mortality, and high-fit women with any combination of smoking, hypertension, or hypercholesterolemia had lower adjusted death rates than low-fit women with none of these risk factors.
Gulati et al10 studied a cohort of 5721 asymptomatic middle-aged women who were followed up for approximately 8 years. After adjustment for age and traditional risk factors using the Framingham Risk Score, the risk of all-cause death doubled or tripled for those in the lowest fitness category (<5 METs) compared with the subgroup with the highest exercise capacity (>8 METs). Kavanagh et al9 evaluated the predictive value of cardiopulmonary exercise testing in 2380 women with known coronary artery disease who were referred for exercise-based cardiac rehabilitation and followed up for an average of 6.1 years. Directly measured peak oxygen uptake (peak Vo2) at program entry proved to be a powerful predictor of cardiovascular and all-cause mortality. The peak Vo2 threshold above which there was a marked benefit in prognosis was 13.0 mL O2/kg/min (3.7 METs). Beyond that threshold, each 1 mL O2/kg/min (ie, 0.3 MET) increase in peak Vo2 conferred a 10% reduction in cardiac mortality.
Collectively, the aforementioned referenced studies and numerous other reports support the hypothesis that cardiorespiratory fitness provides a strong, graded inverse association with cardiovascular and all-cause mortality in healthy and unhealthy populations, irrespective of sex, BMI, major risk factors, and other comorbid conditions. To our knowledge, the findings of Lyerly et al11 are the first to clarify the prognostic value of cardiorespiratory fitness levels in middle-aged women with either impaired fasting glucose or previously undiagnosed diabetes mellitus, both of which are associated with an elevated risk of premature mortality.12
Physical Activity in Prevention and Treatment of Diabetes Mellitus
There is a pathophysiological cascade by which physical inactivity predisposes to a cluster of metabolic diseases, including impaired fasting glucose and diabetes mellitus, and the associated cardiovascular sequelae. With a hypokinetic lifestyle, skeletal muscle down-regulates its capacity to convert nutritional substrates to energy, specifically adenosine triphosphate. Inactive skeletal muscle's impaired ability to oxidize glucose and fatty acids is presumably mediated by several mechanisms, including decreased mitochondrial concentration; a reduced ability to remove glucose from blood due to fewer capillaries and diminished glucose transporter; and an attenuated capacity to hydrolyze blood triglycerides to free fatty acids, secondary to decreased lipoprotein lipase activity and reduced insulin sensitivity.13 Collectively, these metabolic derangements serve to reduce the capacity to burn fuel, resulting in hyperinsulinemia, hypertriglyceridemia, and ultimately increased cardiovascular risk.
In contrast, regular moderate to vigorous leisure-time physical activity (ie, activity sufficient to improve aerobic fitness) counteracts these deleterious adaptations and diminishes the risk factors associated with the development of diabetes mellitus (eg, excessive adiposity, elevated fasting blood glucose levels). An increase in physical activity also improves insulin action at the adipocyte, with or without a concomitant reduction in body weight and fat stores.14 This is an important (and often overlooked) salutary effect, suggesting that physical activity is as efficacious in preventing insulin resistance as is losing body weight.
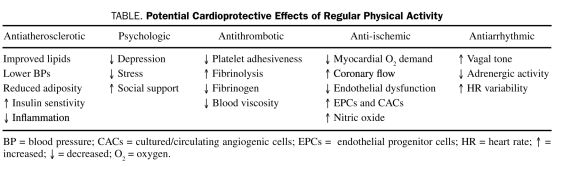
Cardioprotective Effects of Exercise
Two meta-analyses15,16 have shown that regular exercise participation can decrease the overall risk of cardiovascular events by up to 50%, presumably from multiple mechanisms, including antiatherosclerotic, anti-ischemic, antiarrhythmic, antithrombotic, and psychological effects (Table). Because more than 40% of the risk reduction associated with exercise cannot be explained by changes in risk factors, Green et al17 proposed a cardioprotective “vascular conditioning” effect, including enhanced nitric oxide vasodilator function, improved vascular reactivity, altered vascular structure, or combinations thereof. Decreased vulnerability to arrhythmias and increased resistance to ventricular fibrillation have also been postulated to reflect exercise-related adaptations in autonomic control. As a consequence of endurance training, sympathetic drive at rest is reduced and vagal tone is increased. Moreover, recent epidemiological studies have shown that each 1-MET increase in cardiorespiratory fitness confers an 8% to 17% reduction in cardiovascular and all-cause mortality.18
TABLE.
Potential Cardioprotective Effects of Regular Physical Activity
Contemporary Exercise Recommendations
As a follow-up to the updated physical activity recommendations from the American College of Sports Medicine and the American Heart Association,19 on October 7, 2008, the US Department of Health and Human Services issued Physical Activity Guidelines for Americans.20 These evidence-based recommendations were developed to clarify the types and amounts of physical activity needed to improve and maintain health, with specific reference to children and adolescents, young and middle-aged adults, older adults, and people with disabilities and/or chronic medical conditions. Key guidelines for adults (aged 18-64 years) are listed below.
For substantial health benefits, adults should do at least 150 minutes a week of moderate-intensity aerobic physical activity, 75 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Lesser amounts of physical activity may be beneficial, especially compared with a habitually sedentary lifestyle. Aerobic activity should be performed in bouts of at least 10 minutes and preferably spread throughout the week.
For additional health benefits, adults should increase their aerobic physical activity to 300 minutes a week of moderate intensity, 150 minutes a week of vigorous intensity, or an equivalent combination of moderate and vigorous intensity.
Adults should also do muscle-strengthening activities that involve all major muscle groups on 2 or more days a week because these activities provide independent and additive health benefits.
Unfortunately, structured exercise programs have been only marginally effective for encouraging people to be more physically active. Thus, patients should be counseled to integrate multiple short bouts of physical activity into their daily lives. Pedometers can be helpful in this regard,21 as can programs in which they are used (eg, America on the Move) to enhance awareness of physical activity by progressively increasing daily step totals.
Implications for Health Care Professionals
Although the inverse association between aerobic fitness and cardiovascular and all-cause mortality has been widely promulgated among physiologists and epidemiologists, the medical community has, to a lesser extent, embraced cardiorespiratory fitness as one of the strongest and most consistent prognostic markers in persons with and without heart disease. Low-fit individuals can especially benefit from exercise counseling to improve survival.22 Overweight/obese individuals in particular are often completely sedentary23 and should be strongly encouraged to engage in regular walking so they can move out of the least fit, least active, “high-risk” cohort (bottom 20%). An overwhelming body of scientific and clinical data, including the findings of Lyerly et al, suggest that estimation or measurement of cardiorespiratory fitness can provide independent and additive information to the Framingham risk score and other clinical markers of risk stratification (eg, left ventricular ejection fraction).24 Accordingly, physicians and allied health care professionals should expand their medical evaluations and coronary risk factor profiling to include objective data regarding their patients' aerobic capacity expressed relative to age and sex norms. Avoidance of the lowest category of cardiorespiratory fitness may be the easiest and least costly to introduce, and likely the easiest to maintain, of all interventions shown to favorably modify cardiovascular and related health outcomes.
References
- 1.Williams PT. Physical fitness and activity as separate heart disease risk factors: a meta-analysis. Med Sci Sports Exerc. 2001;33(5):754-761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blair SN, Kohl HW, III, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA 1989;262(17):2395-2401 [DOI] [PubMed] [Google Scholar]
- 3.Blair SN, Kampert JB, Kohl HW, III, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA 1996;276(3):205-210 [PubMed] [Google Scholar]
- 4.Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med. 2000;132(8):605-611 [DOI] [PubMed] [Google Scholar]
- 5.Wei M, Kampert JB, Barlow CE, et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA 1999;282(16):1547-1553 [DOI] [PubMed] [Google Scholar]
- 6.Church TS, Kampert JB, Gibbons LW, Barlow CE, Blair SN. Usefulness of cardiorespiratory fitness as a predictor of all-cause and cardiovascular disease mortality in men with systemic hypertension. Am J Cardiol. 2001;88(6):651-656 [DOI] [PubMed] [Google Scholar]
- 7.Laukkanen JA, Lakka TA, Rauramaa R, et al. Cardiovascular fitness as a predictor of mortality in men. Arch Intern Med. 2001;161(6):825-831 [DOI] [PubMed] [Google Scholar]
- 8.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793-801 [DOI] [PubMed] [Google Scholar]
- 9.Kavanagh T, Mertens DJ, Hamm LF, et al. Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol. 2003;42(12):2139-2143 [DOI] [PubMed] [Google Scholar]
- 10.Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity and the risk of death in women: the St James Women Take Heart Project. Circulation 2003September;108(13):1554-1559 Epub 2003 Sep 15 [DOI] [PubMed] [Google Scholar]
- 11.Lyerly GW, Sui X, Lavie CJ, Church TS, Hand GA, Blair SN. The association between cardiorespiratory fitness and risk of all-cause mortality among women with impaired fasting glucose or undiagnosed diabetes mellitus. Mayo Clin Proc. 2009;84(9):780-786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barr EL, Zimmet PZ, Welborn TA, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Circulation 2007July10;116(2):151-157 Epub 2007 Jun 18 [DOI] [PubMed] [Google Scholar]
- 13.Chakravarthy MV, Booth FW. Hot Topics: Exercise Philadelphia, PA: Hanley and Belfus (Elsevier); 2003. [Google Scholar]
- 14.Kelley DE, Goodpaster BH. Effects of physical activity on insulin action and glucose tolerance in obesity. Med Sci Sports Exerc. 1999;31(11) (suppl):S619-S623 [DOI] [PubMed] [Google Scholar]
- 15.Powell KE, Thompson PD, Caspersen CJ, Kendrick JS. Physical activity and the incidence of coronary heart disease. Annu Rev Public Health 1987;8(May):253-287 [DOI] [PubMed] [Google Scholar]
- 16.Berlin JA, Colditz GA. A meta-analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol. 1990;132(4):612-628 [DOI] [PubMed] [Google Scholar]
- 17.Green DJ, O'Driscoll G, Joyner MJ, Cable NT. Exercise and cardiovascular risk reduction: time to update the rationale for exercise? J Appl Physiol. 2008August;105(2):766-768 Epub 2008 Jan 3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Franklin BA, Gordon NF. Contemporary Diagnosis and Management in Cardiovascular Exercise Newtown, PA: Handbooks in Health Care Company; 2009:74-88 [Google Scholar]
- 19.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007August;116(9):1081-1093 Epub 2007 Aug 1 [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services Physical activity guidelines for Americans. http://www.hhs.gov/news/facts/physicalactivityguidelines.html. http://www.hhs.gov/news/facts/physicalactivityguidelines.html Released October 7, 2008. Accessed August 3, 2009.
- 21.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007;298(19):2296-2304 [DOI] [PubMed] [Google Scholar]
- 22.Blair SN, Kohl HW, III, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA 1995;273(14):1093-1098 [PubMed] [Google Scholar]
- 23.Vanhecke TE, Franklin BA, Miller WM, deJong AT, Coleman CJ, McCullough PA. Cardiorespiratory fitness and sedentary lifestyle in the morbidly obese. Clin Cardiol. 2009;32(3):121-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dutcher JR, Kahn J, Grines C, Franklin B. Comparison of left ventricular ejection fraction and exercise capacity as predictors of two- and five-year mortality following acute myocardial infarction. Am J Cardiol. 2007February15;99(4):436-441 Epub 2006 Dec 20 [DOI] [PubMed] [Google Scholar]