Abstract
Patients commonly present to primary care physicians with musculoskeletal symptoms. Clinicians certified in internal medicine must be knowledgeable about the diagnosis and management of musculoskeletal diseases, yet they often receive inadequate postgraduate training on this topic. The musculoskeletal problems most frequently encountered in our busy injection practice involve, in decreasing order, the knees, trochanteric bursae, and glenohumeral joints. This article reviews the clinical presentations of these problems. It also discusses musculoskeletal injections for these problems in terms of medications, indications, injection technique, and supporting evidence from the literature. Experience with joint injection and the pharmacological principles described in this article should allow primary care physicians to become comfortable and proficient with musculoskeletal injections.
GIM = General Internal Medicine; NSAID = nonsteroidal anti-inflammatory drug
Musculoskeletal diseases are commonly encountered in primary care practice,1 and physicians typically manage problems that would benefit from joint and soft tissue injections. Although musculoskeletal injection is one of the most frequently performed procedures among practicing internists,2 physicians receive inadequate training regarding musculoskeletal diseases and injection technique.3-6 The Accreditation Council for Graduate Medical Education7 and the American Board of Internal Medicine8 require resident physicians to understand arthrocentesis, yet residency training programs have traditionally provided limited instruction on this topic. Consequently, some training programs have instituted special musculoskeletal curricula that have been shown to improve physicians' confidence and ability with joint injections.3-5
The Mayo Clinic Division of General Internal Medicine (GIM) has created a musculoskeletal injection clinic. Our physicians perform musculoskeletal injections on patients and teach injection technique to internal medicine residents. In 2008, 563 injections were performed in the Mayo Clinic GIM Musculoskeletal Injection Clinic. The 3 most commonly injected sites were the knee (208 injections, 37%), greater trochanteric bursa (197 injections, 35%), and glenohumeral joint (96 injections, 17%). Properly performed joint injections are straightforward procedures that can be practiced by many primary care physicians. This article reviews the joint problems most commonly encountered in our GIM practice and summarizes the injectable medications, indications, and technique for musculoskeletal injection.
PHARMACOTHERAPY
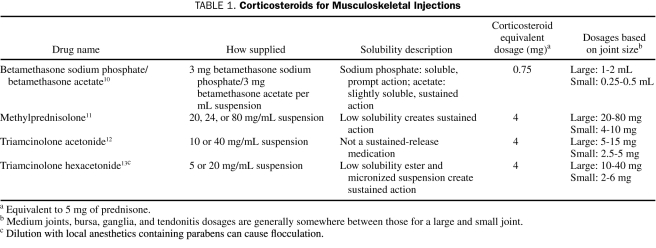
Musculoskeletal injections typically involve a combination of local anesthetics, which provide immediate analgesia and confirmation of accurate injection placement, and corticosteroids, which provide prolonged analgesia. The main corticosteroids used in the United States for joint and soft tissue injection are betamethasone sodium phosphate/acetate (Celestone Soluspan, Schering-Plough, Kenilworth, NJ), methylprednisolone (Depo-Medrol, Upjohn, Kalamazoo, MI), triamcinolone acetonide (Kenalog, Bristol-Meyers Squibb, Princeton, NJ), and triamcinolone hexacetonide (Aristospan, Sandoz, Princeton, NJ).9 Solubility description, corticosteroid equivalent dosage, and dosages based on joint size are listed in Table 1.10-13
TABLE 1.
Corticosteroids for Musculoskeletal Injections
Corticosteroid duration of action depends on the preparation. In general, the shortest-acting corticosteroid is triamcinolone acetonide and the longest-acting is triamcinolone hexacetonide. Longer-acting preparations have a slightly higher risk of complications, including tendon rupture and tissue atrophy, but these risks are nevertheless small.14
A national survey of joint injection practice showed that physicians' preferences for specific corticosteroids are linked to the regions in the United States where the practitioners have trained,9 perhaps explaining why uniform guidelines for recommended corticosteroid preparations are lacking. We often use triamcinolone hexacetonide for injections in the large intra-articular joints and greater trochanteric bursa, and triamcinolone acetonide for small intra-articular and soft tissue injections. Notably, despite more than 20 years of combined experience, we have observed no complications of tendon rupture or septic arthritis.
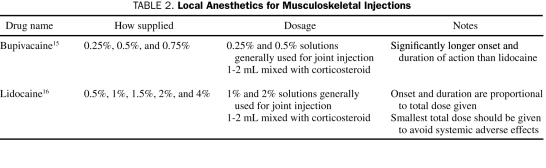
Local anesthetics frequently used for joint and soft tissue injections are bupivacaine (Hospira, Lake Forest, IL; Sensoricaine, AstraZeneca, Wilmington, DE) and lidocaine (Xylocaine, AstraZeneca, Wilmington, DE). Table 2 summarizes available concentrations, onset, duration, and dosages of these medications.15,16 We typically use lidocaine for intra-articular and bursal injections and bupivacaine for trigger point injections.
TABLE 2.
Local Anesthetics for Musculoskeletal Injections
Newer intra-articular pharmacotherapeutic options exist; however, these would generally not be used by primary care physicians. For example, hyaluronidate, which requires multiple injections, has been shown to decrease pain in patients with osteoarthritis.17,18 Likewise, intra-articular immunomodulators, such as infliximab, are being studied for the treatment of refractory inflammatory arthritis19; however, these intra-articular immunomodulators have yet to become common treatments.
GENERAL METHOD FOR MUSCULOSKELETAL INJECTION
Musculoskeletal injections are safe and comfortable with the use of proper technique. Adverse affects from the medications used in joint injection are rare. Intra-articular corticosteroid injections do not lead to the progression of osteoarthritis.20 Postinjection inflammation is caused by intra-articular injection of corticosteroid crystals and can mimic septic arthritis21; however, septic arthritis usually occurs later than postinjection inflammation and the findings are more persistent. Notably, the risk of septic arthritis from intra-articular injections is less than 0.03%.22 The risk of hyperglycemia in patients with diabetes is very small and transient,23 even for longer-acting corticosteroid preparations. Adrenal suppression from intra-articular corticosteroids has been described but usually lasts less than 2 weeks when it occurs.24 Other risks include skin hypo pigmentation, fat atrophy, tendon rupture, and facial flushing.21 A systematic review of the literature on corticosteroid injection for athletic injuries revealed the following complication rates: skin atrophy (2.4%), skin depigmentation (0.8%), localized erythema and warmth (0.7%), and facial flushing (0.6%).14
The intra-articular injection procedure is safe with experienced clinicians and appropriately selected patients. Risk of hemarthrosis is small even in those taking antiplatelet agents or warfarin,25,26 although most clinicians would discontinue or reverse the effects of these agents before elective injections in anticoagulated patients. Precautions should also be taken to avoid the risk of septic arthritis. In particular, the injection of joints that contain prosthetic hardware should be avoided; patients with such prosthetic hardware should be referred to an orthopedic surgeon. Additionally, injection should be avoided across suspected cellulitis, in areas of infectious arthritis or bursitis, in patients with bacteremia, or in severely immunocompromised patients.
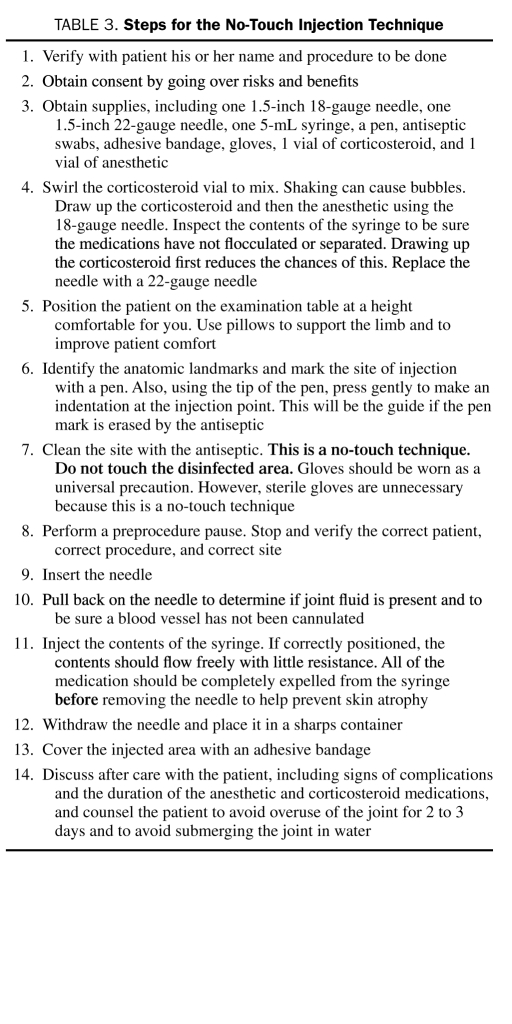
To reduce the risk of infection and improve patient comfort, we suggest some simple measures (Table 3). Joint injection models that provide auditory feedback for correct needle position provide effective training.5 Physicians should take the time to place themselves and patients in comfortable positions before the procedure. Surface landmarks (described in Musculoskeletal Injection for Specific Anatomic Regions) should be clearly identified, and the injection site may be marked with a pen, either by drawing an “X” with ink or marking a circular impression with the tip of the pen. The injection site should be cleansed with an antiseptic solution such as chlorhexidine; we avoid iodine solutions given the relatively high incidence of sensitivity to these agents. The skin should be cleansed with 3 consecutive swabs, using spiral motions from the center outward. Although radiographic guidance with ultrasonography or fluoroscopy may improve accuracy,27-29 it is expensive and is therefore not typically used by primary care physicians who are experienced with injections. However, if response to blind injection is suboptimal, it may be beneficial to use ultrasound guidance to ensure injection placement for subsequent injections.29
TABLE 3.
Steps for the No-Touch Injection Technique
MUSCULOSKELETAL INJECTION FOR SPECIFIC ANATOMIC REGIONS: CLINICAL PRESENTATION, INDICATIONS, TECHNIQUE, AND SUPPORTING EVIDENCE
Knee Joint
Knee pain is a common presenting symptom in primary care practice. Main indications for intra-articular knee injection are osteoarthritis, Baker cyst, and pes anserine bursitis.
Osteoarthritis is a slow and progressive disease that is linked to obesity and most commonly affects the medial compartment and patellofemoral joint; however, patients often describe diffuse knee pain. Although patients may report morning stiffness, it lasts only minutes. Furthermore, the pain typically worsens with activity. Physical examination usually reveals pain with passive range of motion, crepitus, and possibly a cool effusion. Treatments include gentle aerobic activity, quadriceps strengthening, nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and injections of intra-articular hyaluronidate and corticosteroids. Of course, treatment-refractory patients are referred to orthopedic surgeons for consideration of joint replacement.
Baker cysts are synovial fluid collections originating from the knee joint. Patients typically describe knee pain and stiffness and occasionally fullness in the popliteal fossa. Physical examination shows posterior swelling at the medial aspect of the joint where the semimembranous and medial head of the gastrocnemius intersect. A Baker cyst can rupture and mimic thrombophlebitis, causing a physical finding called phlegmasia cerulea dolens; therefore, ultrasonography is sometimes required to differentiate between these 2 diagnoses. Treatment options include physical therapy, needle aspiration, and corticosteroid injection. Because many Baker cysts are continuous with the knee joint, intra-articular knee injection is often effective.
Pes anserine bursitis also improves with corticosteroid injection. Patients usually present with inferomedial knee pain localized over the pes anserine bursa. On physical examination, palpable tenderness can be noted at the confluence of the sartorius, gracilis, and semitendinosus muscles. Moreover, pes anserine bursitis can be exacerbated by osteoarthritis of the knee. Treatments include hamstring stretching, quadriceps strengthening, and corticosteroid injection. Injections are placed directly into the bursa. Low-potency corticosteroids should be used to prevent tissue atrophy.
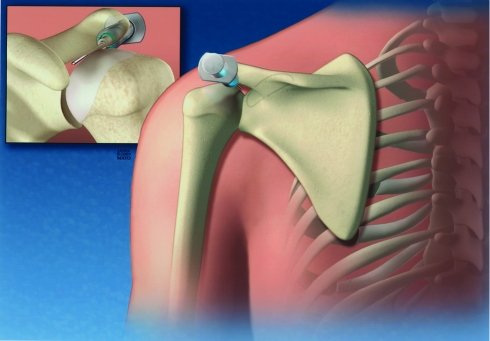
For intra-articular knee injections, we usually use 2 mL of triamcinolone hexacetonide (20 mg/mL) and 2 mL of lidocaine (2%). The technique for knee injection is described in Table 3. First, have the patient lie supine on the examination table with his/her head supported by a pillow. Place a rolled towel under the lower thigh to slightly angulate the knee and open the joint space. In our practice, a medial approach is most common (Figure 1). Palpate along the medial aspect of the patella, moving from superior to inferior in a clockwise motion. A small space or indentation will be felt at about the 3 o'clock position. Mark this point and insert the needle as described in Table 3. The angle of the needle should be parallel to the undersurface of the patella and aimed slightly superiorly to guide the needle toward the intercondylar notch, which decreases the risk of hitting the periosteum. Finish the injection using the steps outlined in Table 3.
FIGURE 1.
Anterior view of the right knee showing a medial approach intra-articular injection.
The Cochrane Collaboration systematically reviewed the literature on intra-articular corticosteroid treatment of knee osteoarthritis in 2006.30 Aggregate results from 28 trials (1973 combined participants) comparing intraarticular corticosteroids vs placebo, hyaluronidate, joint lavage, or other corticosteroids showed that intra-articular corticosteroids were more effective for pain reduction and patient global assessment at 1 week (number needed to treat, 3-4) and that pain reduction lasted for 2 to 3 weeks. However, evidence for functional improvement with corticosteroids was lacking, and at 4 to 24 weeks after injection, no evidence was found for improvement in pain or function. No differences were noted at 4 weeks in patients treated with corticosteroid vs hyaluronidate preparations. Finally, comparisons between types of corticosteroids showed that triamcinolone hexacetonide was superior to betamethasone.
Greater Trochanteric Bursa
Greater trochanteric bursitis is a very common condition resulting in pain over the greater trochanter. Imaging studies indicate that the pain can be from gluteus minimus or medius injury or inflammation of the bursa itself.31 Typical causes are running, local trauma, and gait disturbances, but it is often idiopathic. The pain can be severe, radiate to the buttock or anterior thigh, and be exacerbated by standing or sleeping on the affected side. Patients often describe “hip” pain; however, true intra-articular hip pain usually radiates to the groin. Trochanteric bursitis only rarely is caused by infection. On examination, palpation over the greater trochanter reproduces the pain. Three bursae (2 major and 1 minor) surround the greater trochanter. Major bursae are the subgluteus medius bursa (posterior and superior to the proximal edge of the greater trochanter) and the subgluteus maximus bursa (lateral to the greater trochanter). The minor bursa is the subgluteus minimus bursa (above and slightly anterior to the superior surface of the greater trochanter). Treatment options include NSAIDs, correction of gait abnormalities, postural and hip muscle strengthening, topical application of moist heat, ultrasonography, and corticosteroid injection.
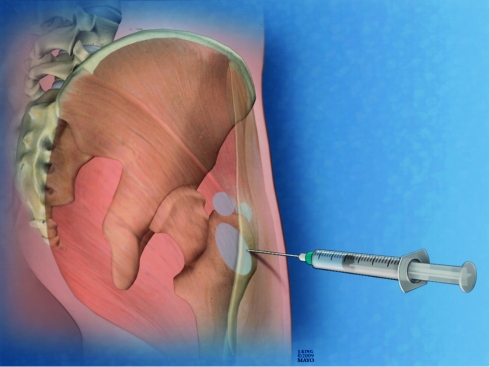
For injecting trochanteric bursae, we typically use 2 mL of triamcinolone hexacetonide (20 mg/mL) and 2 mL of lidocaine (2%). The technique for injecting a greater trochanteric bursa is described in Table 3. First, have the patient lie on their asymptomatic side with the painful hip facing up. The patient's head should be supported with a pillow. Drape the patient with sheets to cover the genitals and expose only the area of the greater trochanter. Ask the patient to point with 1 finger to the area of greatest pain; mark this with a pen (Figure 2). Remember that up to 3 bursae, arranged around the greater trochanter in a triangular configuration, can be affected (Figure 2). The injection is distributed across all affected bursae that are localized by the patient. The injection is completed by using the steps outlined in Table 3.
FIGURE 2.
Posterolateral view of the right hip showing the 2 major (subgluteus medius and subgluteus maximus) and 1 minor (subgluteus minimus) trochanteric bursae. Injections should target the bursae that are most painful.
Evidence supports the efficacy of corticosteroid injection therapy for trochanteric bursitis. Ege Rasmussen and FanØ32 showed that corticosteroid injections gave excellent response in two-thirds of patients, with improvement in the remaining cases. Shbeeb et al33 injected 75 patients with trochanteric bursitis with 6, 12, or 24 mg of betamethasone mixed with lidocaine, demonstrating responses in 77%, 69%, and 61% of patients at 1, 6, and 26 weeks, respectively. This study supported the observation that higher doses of betamethasone provide better pain relief.
Glenohumeral Joint
Several etiologies of shoulder pain respond to a single intra-articular corticosteroid injection. The main indications for shoulder injection are rotator cuff arthropathy, adhesive capsulitis, and subacromial bursitis.
Rotator cuff tendinopathy and arthropathy usually occur from years of repetitive shoulder trauma. Patients often describe pain localized over the anterior shoulder. Pain can be exacerbated by moving the arm overhead (eg, external rotation with hair combing) or behind the back (eg, internal rotation with taking a wallet from the back pocket). Physical examination may show crepitus on passive range of motion and limited internal and external rotation with active range of motion. Pain with abduction between 60° and 120°, known as the painful arc, is often seen. With provocative maneuvers, physicians may also demonstrate signs of tendon impingement by eliciting positive responses (ie, pain). Specifically, examiners elicit the Neer sign by stabilizing the scapula and applying maximal passive forward flexion to the internally rotated shoulder. To elicit Hawkins sign, the patient is examined with his or her arm at 90% and elbow flexed in the horizontal position to 90%. While supporting the elbow, the examiner then applies maximal internal rotation.34
Adhesive capsulitis, also known as frozen shoulder, typically occurs after prolonged immobility of the arm. Patients describe shoulder pain and stiffness with the inability to abduct at the shoulder more than just a few degrees in any direction. Shoulder examination reveals diffuse pain with palpation and reduced active and passive range of motion in all planes. Remarkably, findings on radiography will often be normal.
Patients with subacromial bursitis typically describe their shoulder pain as being worse at night, awakening them when they roll over in bed. The onset may be abrupt and caused by overuse. The pain is exacerbated by abducting the arm greater than 90°. Physical examination may show a reduced range of shoulder motion because of pain. As in rotator cuff tendinitis, the most painful arc of motion will be between 60° and 120°. Pain may occur laterally over the subacromial bursa. Range of motion testing may also reveal pain on internal and external rotation.
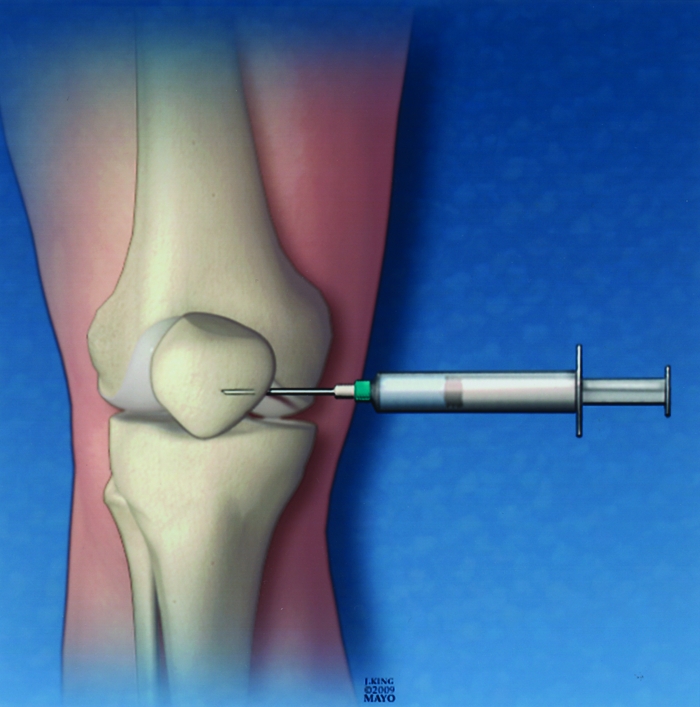
For glenohumeral joint injections, we use 2 mL of triamcinolone hexacetonide (20 mg/mL) and 2 mL of lidocaine (2%). The method for shoulder injection involves the no-touch technique described in Table 3. Start with the patient sitting on the examination table at a height that is comfortable for you. We often use a posterior approach for shoulder injection. Specifically, palpate just the scapular spine and move laterally until you feel a space or indentation. Mark this spot (Figure 3). Next locate the coracoid process anteriorly. When inserting the needle, direct it toward the tip of the coracoid process. Complete the injection by using the no-touch technique described in Table 3. For subacromial injections, the same medications and basic technique are used. However, insert the needle in the space posterolateral to the acromion process. The needle should be inserted parallel to the ground and at a depth of approximately 3 cm.
FIGURE 3.
Posterior view of the left shoulder showing the needle directed toward the coracoid process anteriorly. The inset in the upper left corner shows the same joint from an anterior view. Notice the needle placement within the glenohumeral joint.
Regarding the effectiveness of shoulder injections, the Cochrane Collaboration systematically studied the literature on corticosteroid injection for shoulder pain in 2003,35 reviewing 26 trials with a median of 52 participants, noting variability in number, site and dosage of injection, and methodology. For rotator cuff disease, subacromial corticosteroid injection showed a small benefit over placebo and no benefit over NSAID therapy. For adhesive capsulitis, 2 trials suggested a possible early benefit to intra-articular corticosteroid injection vs placebo, but data were insufficient to draw firm conclusions. Our usual practice is to first attempt conservative therapy. If NSAIDs are ineffective or contraindicated, then joint injection is offered.
CONCLUSION
Musculoskeletal problems are common in primary care and often respond to injections containing both corticosteroids and short-acting anesthetics. Patients frequently present with symptoms involving the shoulder, trochanteric bursa, and knee. Evidence generally supports corticosteroid injection for these anatomic locations. The risks associated with joint injection are very low with proper injection technique and in appropriately selected patients. Experience with joint injection and the pharmacological principles described in this article should allow primary care physicians to become comfortable and proficient with musculoskeletal injections.
Supplementary Material
On completion of this article, you should be able to (1) describe the general method for musculoskeletal joint injection; (2) describe the clinical presentation, indications, technique, and supporting evidence for musculoskeletal injection of the 3 most commonly encountered injectable problems; and (3) compare and contrast the available anesthetics and corticosteroids used in musculoskeletal injection.
CME Questions About Musculoskeletal Injection
-
Which one of the following injectable corticosteroid preparations has the longest duration of action?
Methylprednisolone
Triamcinolone hexacetonide
Betamethasone sodium phosphate/acetate
Triamcinolone acetonide
Bupivacaine
-
Toward which one of the following anatomic landmarks should the needle be directed when performing a glenohumeral joint injection?
Coracoid process
Acromion process
Spine of the scapula
Acromioclavicular joint
Sternoclavicular joint
-
To prevent which one of the following is the corticosteroid drawn up before the local anesthetic when preparing the syringe for a joint injection?
Clogging the needle
Inactivation of the local anesthetic
Contamination of the sterile corticosteroid preparation
Inactivation of the corticosteroid
Flocculation of the medications
-
Which one of the following conditions can Baker cysts most closely mimic when they rupture?
Pes anserine bursitis
Retropatellar pain syndrome
Thrombophlebitis
Osteoarthritis
Adhesive capsulitis
-
Which one of the following symptoms is frequently observed in patients with greater trochanteric bursitis?
Discomfort when moving through the painful arc
Hip pain when sleeping on the affected side
Hip pain that radiates to the groin
Phlegmasia cerulea dolens
Inferomedial knee pain
This activity was designated for 1 AMA PRA Category 1 Credit(s).™
Because the Concise Review for Clinicians contributions are now a CME activity, the answers to the questions will no longer be published in the print journal. For CME credit and the answers, see the link on our Web site at mayoclinicproceedings.com.
REFERENCES
- 1.Stafford RS, Saglam D, Causino N, et al. Trends in adult visits to primary care physicians in the United States. Arch Fam Med. 1999;8(1):26-32 [DOI] [PubMed] [Google Scholar]
- 2.Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007;146(5):355-360 [DOI] [PubMed] [Google Scholar]
- 3.Cuccurullo S, Brown D, Petagna AM, Platt H, Strax TE. Musculoskeletal injection skills competency in physical medicine and rehabilitation residents: a method for development and assessment. Am J Phys Med Rehabil. 2004;83(6):479-485 [DOI] [PubMed] [Google Scholar]
- 4.Houston TK, Connors RL, Cutler N, Nidiry MA. A primary care musculoskeletal clinic for residents: success and sustainability. J Gen Intern Med. 2004;19(5, pt 2):524-529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogelgesang SA, Karplus TM, Kreiter CD. An instructional program to facilitate teaching joint/soft-tissue injection and aspiration. J Gen Intern Med. 2002;17(6):441-445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84-A(4):604-608 [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education (ACGME) Web site. http://www.acgme.org. http://www.acgme.org Accessed July 7, 2009.
- 8.Duffy FD, Holmboe ES. What procedures should internists do [editorial]? Ann Intern Med. 2007;146(5):392-393 [DOI] [PubMed] [Google Scholar]
- 9.Centeno LM, Moore ME. Preferred intraarticular corticosteroids and associated practice: a survey of members of the American College of Rheumatology. Arthritis Care Res. 1994;7(3):151-155 [DOI] [PubMed] [Google Scholar]
- 10.Celestone [package insert] Kenilworth, NJ: Schering Corporation; 1999. [Google Scholar]
- 11.Depo-Medrol [package insert] Kalamazoo, MI: Pharmacia & Upjohn Company; 2002. [Google Scholar]
- 12.Kenalog [package insert] Princeton, NJ: Bristol-Meyers Squibb; 2006. [Google Scholar]
- 13.Aristospan [package insert] Princeton, NJ: Sandoz Inc; 2006. [Google Scholar]
- 14.Nichols AW. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin J Sport Med. 2005;15(5):370-375 [DOI] [PubMed] [Google Scholar]
- 15.Bupivacaine [package insert] Lake Forest, IL: Hospira Inc; 2004. [Google Scholar]
- 16.Lidocaine [package insert] Schaumburg, IL: Abraxis Pharmaceuticals; 2006. [Google Scholar]
- 17.Punzi L. Intra-articular sodium hyaluronate reduces pain and improves function in osteoarthritis of knee. Clin Exp Rheumatol. 2001;19(1):9-10 [PubMed] [Google Scholar]
- 18.Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Viscosupplementation for the treatment of osteoarthritis of the knee [update of Cochrane Database Syst Rev. 2005;(2):CD005321] Cochrane Database Syst Rev. 2006;(2):CD005321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakellariou GT, Kakavouli G, Chatzigiannis I. Intraarticular injection of infliximab [letter]. J Rheumatol. 2006;33(9):1912-1913 [PubMed] [Google Scholar]
- 20.Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial [published correction appears in Arthritis Rheum. 2003;48(11):3300] Arthritis Rheum. 2003;48(2):370-377 [DOI] [PubMed] [Google Scholar]
- 21.Cole BJ, Schumacher HR., Jr Injectable corticosteroids in modern practice. J Am Acad Orthop Surg. 2005;13(1):37-46 [DOI] [PubMed] [Google Scholar]
- 22.Charalambous CP, Tryfonidis M, Sadiq S, Hirst P, Paul A. Septic arthritis following intra-articular steroid injection of the knee: a survey of current practice regarding antiseptic technique used during intra-articular steroid injection of the knee. Clin Rheumatol. 2003December;22(6):386-390 Epub 2003 Oct 15 [DOI] [PubMed] [Google Scholar]
- 23.Black DM, Filak AT. Hyperglycemia with non-insulin-dependent diabetes following intraarticular steroid injection. J Fam Pract. 1989;28(4):462-463 [PubMed] [Google Scholar]
- 24.Mader R, Lavi I, Luboshitzky R. Evaluation of the pituitary-adrenal axis function following single intraarticular injection of methylprednisolone. Arthritis Rheum. 2005;52(3):924-928 [DOI] [PubMed] [Google Scholar]
- 25.Thumboo J, O'Duffy JD. A prospective study of the safety of joint and soft tissue aspirations and injections in patients taking warfarin sodium. Arthritis Rheum. 1998;41(4):736-739 [DOI] [PubMed] [Google Scholar]
- 26.Goupille P, Thomas T, Noël E, GREP A practice survey of shoulder glucocorticoid injections in patients on antiplatelet drugs or vitamin K antagonists. Joint Bone Spine 2008May;75(3):311-314 Epub 2008 Apr 18 [DOI] [PubMed] [Google Scholar]
- 27.Chen MJ, Lew HL, Hsu TC, et al. Ultrasound-guided shoulder injections in the treatment of subacromial bursitis. Am J Phys Med Rehabil. 2006;85(1):31-35 [DOI] [PubMed] [Google Scholar]
- 28.Cohen SP, Narvaez JC, Lebovits AH, Stojanovic MP. Corticosteroid injections for trochanteric bursitis: is fluoroscopy necessary? A pilot study. Br J Anaesth 2005;94(1):100-106 Epub 2004 Oct 29 [DOI] [PubMed] [Google Scholar]
- 29.Naredo E, Cabero F, Beneyto P, et al. A randomized comparative study of short term response to blind injection versus sonographic-guided injection of local corticosteroids in patients with painful shoulder. J Rheumatol. 2004;31(2):308-314 [PubMed] [Google Scholar]
- 30.Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee [update of Cochrane Database Syst Rev. 2005;(2):CD005328] Cochrane Database Syst Rev. 2006;(2):CD005328 [DOI] [PubMed] [Google Scholar]
- 31.Kong A, Van der Vliet A, Zadow S. MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome. Eur Radiol. 2007July;17(7):1772-1783 Epub 2006 Dec 6 [DOI] [PubMed] [Google Scholar]
- 32.Ege Rasmussen KJ, Fanø N. Trochanteric bursitis: treatment by corticosteroid injection. Scand J Rheumatol. 1985;14(4):417-420 [DOI] [PubMed] [Google Scholar]
- 33.Shbeeb MI, O'Duffy JD, Michet CJ, Jr, O'Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol. 1996;23(12):2104-2106 [PubMed] [Google Scholar]
- 34.Pappas GP, Blemker SS, Beaulieu CF, McAdams TR, Whalen ST, Gold GE. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. J Shoulder Elbow Surg. 2006;15(1):40-49 [DOI] [PubMed] [Google Scholar]
- 35.Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003;(1):CD004016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.