Abstract
Purpose
The prevalence of exercise-induced bronchospasm (EIB) is significantly higher in athletes than the general population, and can result in significant morbidity in young, competitive athletes. Guidelines emphasize that education and written treatment protocols improve clinical outcomes for asthmatics. Evidence also supports objective testing when exercise-induced bronchospasm is suspected, immediate availability of rescue inhalers, and involvement of asthma specialists in the care of asthmatic athletes. We sought to determine how EIB is managed at National Collegiate Athletic Association (NCAA) sports medicine programs.
Methods
A survey consisting of multiple-choice questions related to exercise-induced bronchospasm in athletes was sent electronically to 3200 athletic trainers affiliated with NCAA sports medicine programs.
Results
541 athletic trainers responded. A minority of athletic trainers surveyed (21%) indicated an asthma management protocol exists at their institution. 22% indicated that pulmonologists are on staff in or consultants to the sports medicine department. Many indicated a short-acting beta-agonist is not required to be available at all practices (39%) and games (41%) and few athletic trainers indicated their programs utilize objective testing to diagnose EIB (17%). Regression modeling demonstrated education about EIB and involvement of pulmonologists significantly improved adherence to current consensus guidelines.
Conclusions
Based on our data, many NCAA sports medicine programs do not manage athletes with EIB according to current consensus guidelines. This may result in inaccurate diagnoses and may be detrimental to clinical outcomes and the overall health of student athletes. Providing education about EIB and involvement of pulmonologists significantly increase adherence to guidelines which likely improves clinical care of athletes and potentially athletic performance.
Keywords: asthma, sports, bronchoprovocation, symptoms, diagnosis
INTRODUCTION
Exercise-induced bronchospasm (EIB) describes airway narrowing that occurs in association with exercise. The prevalence of EIB in elite, Olympic athletes has been reported to be as much as five times greater than that of the general population (10, 13). The prevalence of EIB has also been recently shown to be significantly higher in a cohort of college athletes than in the general population (9). Acute episodes of bronchospasm that occur during exercise can result in significant morbidity in young competitive athletes (2) and may affect athletic performance.
Asthma guidelines emphasize that asthma education and written asthma treatment protocols improve clinical outcomes for asthmatics (7, 8). In addition, evidence strongly supports objective lung function testing when EIB is suspected clinically, because diagnoses of EIB made based solely on clinical symptoms very often are inaccurate (9, 12). Furthermore, evidence supports involvement of asthma specialists in the management of both EIB and chronic asthma, as specialists have been shown to be more likely to both diagnose EIB by objective measures (11) and to manage asthma per national asthma guidelines than primary care physicians (6).
The specific aims of this study were to determine how National Collegiate Athletic Association (NCAA) sports medicine programs diagnose and manage athletes who experience acute episodes of EIB and whether methods of diagnoses and approaches to management adhere to consensus guidelines. We also investigated whether formal involvement of pulmonologists in NCAA collegiate sports medicine departments influences adherence to guidelines. We conducted an internet survey of certified athletic trainers affiliated with NCAA sports medicine programs as a method to achieve the aims of the study.
METHODS
Electronic mailing addresses of certified athletic trainers affiliated with NCAA programs were obtained with permission from the National Athletic Trainers’ Association (NATA) membership roster. An Institutional Review Board-approved asthma management survey consisting of multiple-choice questions was created utilizing a survey service (www.surveymonkey.com). This survey was then electronically mailed to 3,200 certified athletic trainers. The survey was anonymous, individual respondents were insured of their anonymity prior to participation and could not be retrospectively identified based on their responses, and informed consent was implied by responding to the survey.
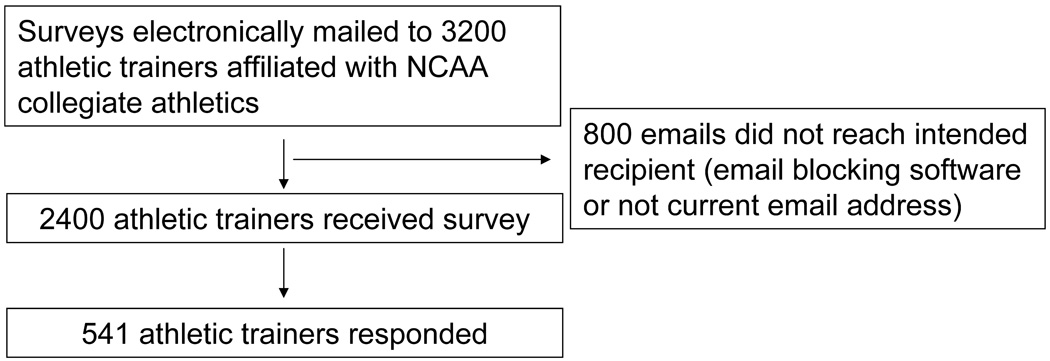
Of those initially emailed, 800 email addresses were found to be inaccessible (i.e. an inactive address or email blocking software). After the initial internet mailing, the survey was sent to all non-responders electronically two additional times. There were a total of 541 respondents resulting in an overall survey response rate of 23% (Figure 1).
Figure 1.
Study schema
The effects of having a pulmonologist as a consultant or staff in the sports medicine department and receiving education about diagnosis and management of EIB were analyzed. Analyses were done utilizing Pearson’s chi-square test and p-values were adjusted by Holm’s procedure for the multiple testing. P-values less than 0.05 were considered significant. Odds ratios were calculated utilizing logistic regression.
RESULTS
Diagnosis of EIB
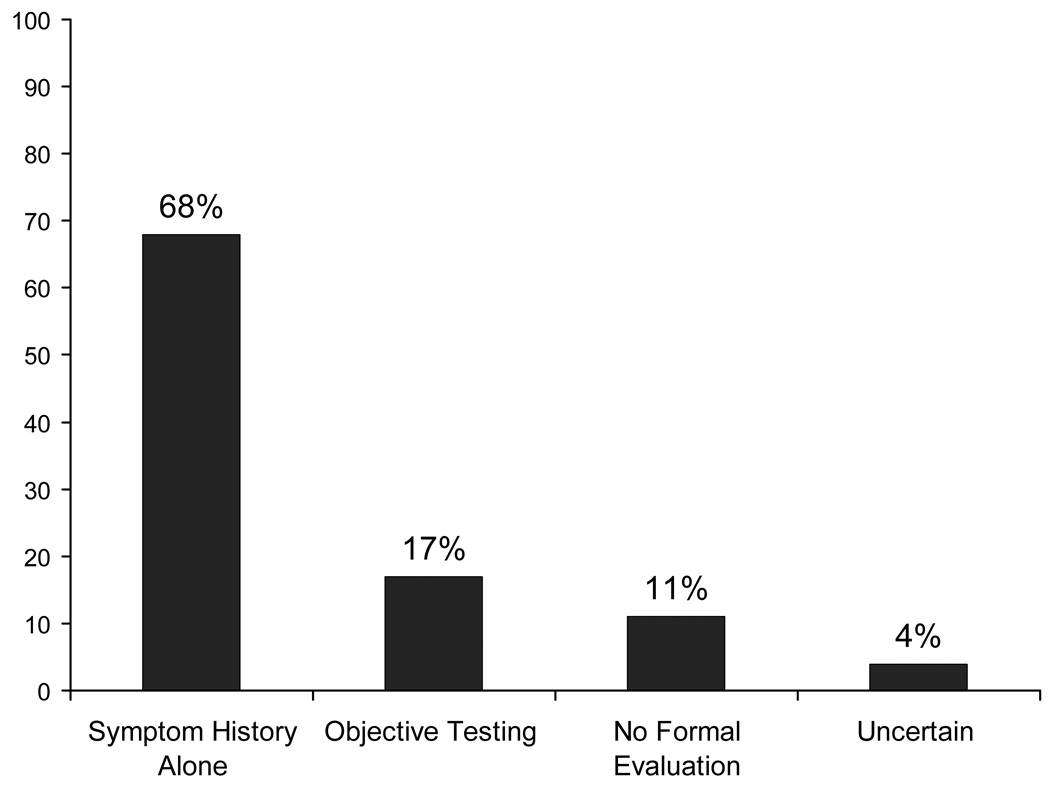
68 % of respondents indicated EIB was diagnosed based on symptom history alone compared to 17% that indicated EIB was evaluated in their programs by use of objective testing. Objective testing was defined as spirometry or some form of bronchoprovocation testing (exercise challenge, methacholine challenge, or eucapnic voluntary hyperventilation). In addition, 11% did not have an established approach for the evaluation of EIB (Figure 2).
Figure 2.
How are athletes evaluated for exercise-induced bronchospasm at your institution?
Sideline management of EIB
46% of athletic trainers that responded had read the position statement of the National Athletic Trainers’ Association pertaining to diagnosis and management of asthma in athletes.
Only 21% of respondents stated that their athletic department has a specific written protocol for the management of acute episodes of bronchospasm that occur during games or practices.
61% of respondents indicated that their athletic program mandates that a short-acting beta-agonist is available at all practices. Similarly, 59% stated a short-acting beta-agonist is required to be available at all games.
52% indicated that after an athlete has had an episode of bronchospasm, the criteria to allow them to return to play is based on subjective improvement alone. 20% stated that athletes are permitted to return to play after a rescue bronchodilator is given and 18% indicated that objective improvement in peak-flow meter readings must be documented before athletes can return.
Effect of pulmonologists and education on adherence to guidelines
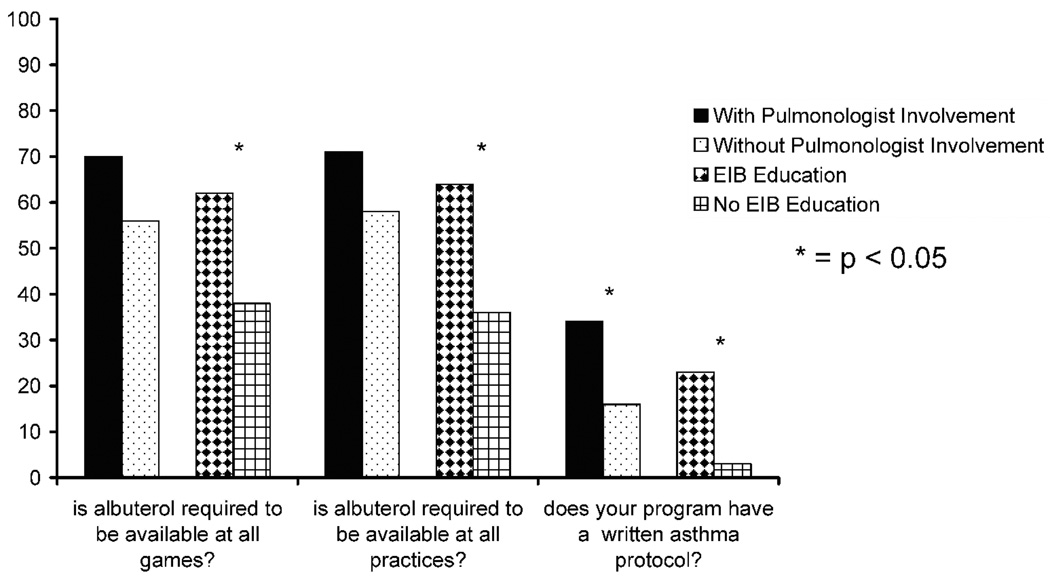
Pulmonologists were reported to be formal consultants or on staff in the sports medicine department in 22% of programs. Sports medicine programs with pulmonologists on staff were significantly more likely to have a written protocol for managing acute asthma attacks during practices or games (34% versus 16 %; p-value = 0.0004). In addition, programs with pulmonologists on staff were significantly more likely to use objective testing to document EIB (34% versus 12%; p-value < 0.0001). Programs with pulmonologists were also more likely and to have albuterol mandated to be readily available at practices (71 % versus 58 %; p-value = 0.1227) and at games (70 % versus 56 %; p-value = 0.0939) (Figure 3).
Figure 3.
Effect of pulmonologists and education on adherence to guidelines
Programs providing education on EIB were more likely to have a written protocol concerning management of EIB (23 % versus 3 %; p-value = 0.0073). In addition, programs providing EIB education were more likely to require a short-acting beta-agonist be available at all practices (64% versus 36%; p-value = 0.0007) and to require a short-acting beta-agonist to be available at all games (62% versus 38%; p-value = 0.0040) (Figure 3).
DISCUSSION
The objective of this study was to evaluate how exercise-induced bronchospasm is diagnosed and managed by athletic programs involved in NCAA athletics. This was accomplished through analysis of a survey completed by certified athletic trainers affiliated with NCAA sports programs. Current asthma guidelines emphasize the importance of objective lung function testing in the evaluation of EIB as well as the critical importance of having rescue bronchodilators immediately available when an episode of EIB occurs (1, 4, 7, 8). In addition, guidelines emphasize that asthma education and written asthma treatment protocols improve clinical asthma outcomes (8). Our study demonstrated that a symptom-based approach without objective testing is used in some cases, and many programs do not have written protocols for the sideline management of EIB. In addition, many programs surveyed do not mandate availability of short-acting beta-agonists at all practices and games. Furthermore, we showed that inclusion of pulmonologists on staff or as formal consultants in the sports medicine program increased the likelihood that collegiate programs surveyed had a written protocol for managing EIB, utilized objective testing to diagnose EIB, and mandated the availability of rescue inhalers at games and practices.
Results of our survey suggest that the diagnosis of EIB is made based upon symptoms alone in some cases at many of the programs surveyed. However, it is difficult to accurately measure how commonly objective testing is truly utilized in a retrospective survey. The question posed did not indicate a temporal time frame for objective testing, thus it is possible that some athletes were tested prior to matriculation based on symptoms or response to therapy. In addition, it is not possible for each respondent to know how each individual case is managed at their institution. All of the above limitations challenge our finding that 68 % of respondents indicated EIB was diagnosed based on symptom history alone at their institution. Nonetheless, the data demonstrated a very low recall of use of objective testing which suggests that the optimal diagnostic approach to EIB may not be performed in many cases.
Utilization of objective testing in the workup of suspected EIB is a critical issue as it has been shown in many studies that the diagnosis of EIB based solely on a subjective history without objective confirmation of the diagnosis is extremely inaccurate (5, 9, 12). Because there are several disorders that can mimic EIB including vocal cord dysfunction, cardiac disorders, and gastroesophageal reflux disease, subjective diagnosis of EIB without objective confirmation may result in many inaccurate diagnoses. Hallstrand et al (5) found screening history identified subjects with symptoms or a previous diagnosis suggestive of EIB in 40% of the participants, but only 13% of these persons actually had objectively documented EIB. Similarly, Parsons et al (9) demonstrated only 35% of athletes who complained of respiratory symptoms during exercise were found to be EIB-positive after testing. In addition, despite the evidence that objective testing is critical to confirm a diagnosis of EIB, many health-care providers still do not perform objective testing and treat EIB empirically based on history alone (11). Our data from this survey raise a concern that some programs may be inaccurately diagnosing EIB which potentially exposes athletes to both unnecessary morbidity and medications and possible associated side effects (10, 13).
Currently, it is not possible to predict when an individual athlete may experience significant bronchospasm during a practice or game. Therefore, it is critical that health-care personnel be prepared to manage such episodes when they abruptly occur. The NATA position statement recommends that athletic programs incorporate an asthma action plan for managing and urgently referring all athletes who experience significant attacks of breathing difficulties during practices or games (7). The vast majority of athletic trainers surveyed in our study indicated their institutions do not have such a written protocol for managing acute asthma attacks during games or practices. Similarly, the NATA statement recommends all patients with asthma should have a rescue inhaler available during games and practices, and that certified athletic trainers should have an extra rescue inhaler for each athlete for administration during emergencies (7). Most respondents to our survey stated that short-acting beta-agonists are currently mandated by their athletic department to be present at all practices and games. However, there were a significant number of athletic trainers affiliated with institutions that did not require inhalers to be present. As a result, many athletes who may experience a sudden episode of bronchospasm may not receive treatment as rapidly and effectively as they would have had a management plan and/or a rescue inhaler been immediately available.
Educational interventions in many forms have been shown to be beneficial in terms of improving both asthma care and asthma patient outcomes (14). In our study, the likelihood that athletic trainers surveyed had both written asthma management protocols and requirements for inhalers to be present at all practices and games at their institution was significantly increased if education related to exercise-induced bronchospasm was provided.
Asthma specialists have been shown to be more likely to adhere to asthma guidelines than primary care physicians (6). Asthma specialists have also been shown to be more likely to diagnose asthma by objective measures and more likely to provide patients with written asthma action plans than primary care physicians (6). The findings in our study also support previous data that show involvement of pulmonologists improves adherence to guidelines related to the diagnosis and management of EIB (7). Our findings support a multidisciplinary approach to the diagnosis and management of EIB in athletes and argue for increased involvement of asthma specialists in the care of athletes.
Despite the beneficial effect of education and pulmonologists, it clear that other factors are also important in determining whether asthma protocols exist or whether inhalers are present at practices and games. Almost 90% of respondents indicated that they received some form of education about EIB. However, only 23% of respondents who received education had asthma protocols. In addition, only 64% of respondents who received education were mandated to have inhalers at practices and only 62% at games. Similarly, respondents with pulmonologists in their sports medicine program were more likely to have protocols (34%) and to require inhalers be available at all practices (71%) and games (70%), but many programs with pulmonologists still did not have protocols or mandate inhalers be available. Based on our study, providing education about EIB and involving pulmonologists in the management of EIB are critical factors in managing athletes with asthma, however more study is needed to examine what barriers may exist or what other factors may be important in implementing appropriate management of EIB.
Our study was limited by a 23% response rate and thus may not be representative of how EIB is diagnosed and managed at all collegiate programs. In addition, we did not address current practices of the athletes themselves. It is certainly possible that athletes with known asthma participating in collegiate sports currently bring their own short-acting beta-agonists to practices and games. However, both children and adults historically have been shown to have poor adherence to asthma treatment, with adherence rates as low as 50% (3). Therefore, reliance on athletes to be responsible themselves for making sure inhalers are available if there is an urgent need for a rescue inhaler is likely not a safe or effective strategy. Furthermore, some states prohibit athletic trainers from carrying an inhaler unless it was specifically prescribed by a physician for a specific athlete, which may also be a contributing factor to the number of programs that do not mandate inhalers be available at all games and practices. We were
CONCLUSIONS
Our data revealed that a minority of athletic trainers surveyed have written asthma management protocols at their institution as recommended by the recent NATA position statement. In addition, many athletic trainers surveyed indicated that their sports medicine program does not mandate that a short acting beta agonist is available at all practices and games. Based on responses to our survey, a symptom-based assessment for EIB without objective testing is used in some cases at NCAA collegiate programs. It is unclear how commonly this diagnostic approach is used, but it may result in inaccurate diagnoses and may be detrimental to clinical outcomes and the overall health of student athletes. Our findings demonstrate both education about EIB and involvement of pulmonologists are measures that significantly improve adherence to current guidelines and may potentially improve clinical outcomes and athletic performance.
Acknowledgements
The results of this study do not constitute endorsement by the ACSM.
Funding Sources: National Center for Research Resources, K23 RRO17579.
Footnotes
Disclosure: Dr. Parsons is a member of the Speakers' Bureaus of GlaxoSmithKline, Inc. and Schering-Plough, Inc. Dr. Mastronarde is a member of the Speakers' Bureaus of GlaxoSmithKline, Inc.,Schering-Plough, Inc., and AstraZeneca, Inc.No other authors have conflicts of interest to disclose.
Contributor Information
Jonathan P. Parsons, Email: jonathan.parsons@osumc.edu.
Vincent Pestritto, Email: Vincent.pestritto@osumc.edu.
Gary Phillips, Email: gary.phillips@osumc.edu.
Christopher Kaeding, Email: christopher.kaeding@osumc.edu.
Thomas M. Best, Email: tom.best@osumc.edu.
Gail Wadley, Email: gail.wadley@osumc.edu.
John G. Mastronarde, Email: john.mastronarde@osumc.edu.
REFERENCES
- 1.Allen TW. Sideline management of asthma. Curr Allergy Asthma Rep. 2006;6(3):252–255. doi: 10.1007/s11882-006-0043-2. [DOI] [PubMed] [Google Scholar]
- 2.Becker JM, Rogers J, Rossini G, Mirchandani H, D'Alonzo GE., Jr Asthma deaths during sports: report of a 7-year experience. JAllergy ClinImmunol. 2004;113(2):264–267. doi: 10.1016/j.jaci.2003.10.052. [DOI] [PubMed] [Google Scholar]
- 3.Bender BG. Overcoming barriers to nonadherence in asthma treatment. J Allergy Clin Immunol. 2002;109(6 Suppl):S554–S559. doi: 10.1067/mai.2002.124570. [DOI] [PubMed] [Google Scholar]
- 4.Bolin D, Goforth M. Sideline documentation and its role in return to sport. Clin J Sport Med. 2005;15(6):405–409. doi: 10.1097/01.jsm.0000187078.20348.2c. [DOI] [PubMed] [Google Scholar]
- 5.Hallstrand TS, Curtis JR, Koepsell TD, et al. Effectiveness of screening examinations to detect unrecognized exercise-induced bronchoconstriction. JPediatr. 2002;141(3):343–348. doi: 10.1067/mpd.2002.125729. [DOI] [PubMed] [Google Scholar]
- 6.Janson S, Weiss K. A National Survey of Asthma Knowledge and Practices Among Specialists and Primary Care Physicians. J Asthma. 2004;41(3):343–349. doi: 10.1081/jas-120026093. [DOI] [PubMed] [Google Scholar]
- 7.Miller MG, Weiler JM, Baker R, Collins J, D'Alonzo G. National athletic trainers' association position statement: management of asthma in athletes. J Athl Train. 2005;40(3):224–245. [PMC free article] [PubMed] [Google Scholar]
- 8.National Heart Lung and Blood Institute Expert Panel Report 3. Guidelines for the diagnosis and management of asthma. Bethesda: 2007 Report No.: #07-4051.
- 9.Parsons JP, Kaeding C, Phillips G, Jarjoura D, Wadley G, Mastronarde JG. Prevalence of exercise-induced bronchospasm in a cohort of varsity college athletes. Med Sci Sports Exerc. 2007;39(9):1487–1492. doi: 10.1249/mss.0b013e3180986e45. [DOI] [PubMed] [Google Scholar]
- 10.Parsons JP, Mastronarde JG. Exercise-induced bronchoconstriction in athletes. Chest. 2005;128(6):3966–3974. doi: 10.1378/chest.128.6.3966. [DOI] [PubMed] [Google Scholar]
- 11.Parsons JP, O'Brien JM, Lucarelli MR, Mastronarde JG. Differences in the evaluation and management of exercise-induced bronchospasm between family physicians and pulmonologists. J Asthma. 2006;43(5):379–384. doi: 10.1080/02770900600709880. [DOI] [PubMed] [Google Scholar]
- 12.Rundell KW, Im J, Mayers LB, Wilber RL, Szmedra L, Schmitz HR. Self-reported symptoms and exercise-induced asthma in the elite athlete. MedSciSports Exerc. 2001;33(2):208–213. doi: 10.1097/00005768-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Rundell KW, Jenkinson DM. Exercise-induced bronchospasm in the elite athlete. Sports Med. 2002;32(9):583–600. doi: 10.2165/00007256-200232090-00004. [DOI] [PubMed] [Google Scholar]
- 14.Tapp S, Lasserson TJ, Rowe B. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev. 2007;3:CD003000. doi: 10.1002/14651858.CD003000.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]