Abstract
Objective
To compare the cost effectiveness of sildenafil and papaverine-phentolamine injections for treating erectile dysfunction.
Design
Cost utility analysis comparing treatment with sildenafil (allowing a switch to injection therapy) and treatment with papaverine-phentolamine (no switch allowed). Costs and effects were estimated from the societal perspective. Using time trade-off, a sample of the general public (n=169) valued health states relating to erectile dysfunction. These values were used to estimated health related quality of life by converting the clinical outcomes of a trial into quality adjusted life years (QALYs).
Participants
169 residents of Rotterdam.
Main outcome measures
Cost per quality adjusted life year.
Results
Participants thought that erectile dysfunction limits quality of life considerably: the mean utility gain attributable to sildenafil is 0.11. Overall, treatment with sildenafil gained more QALYs, but the total costs were higher. The incremental cost effectiveness ratio for the introduction of sildenafil was £3639 in the first year and fell in following years. Doubling the frequency of use of sildenafil almost doubled the cost per additional QALY.
Conclusions
Treatment with sildenafil is cost effective. When considering funding sildenafil, healthcare systems should take into account that the frequency of use affects cost effectiveness.
Introduction
The registration of sildenafil has initiated debate about the socioeconomic aspects of this treatment for erectile dysfunction. Generally, governments are concerned about the affordability of sildenafil.1 It is not known whether sildenafil is cost effective. Although the clinical effects of sildenafil have been proved, uncertainty remains about the value of sildenafil to both patients and society.
We performed an economic evaluation of sildenafil according to the usual recommendations.2 We used cost utility analysis, a form of cost effectiveness analysis in which clinical outcomes are converted into quality adjusted life years (QALYs) gained. Both costs and effects were measured from the societal perspective. This means that treatment outcomes were valued by the general public and that all costs were considered—that is, medical costs, costs of patients, and costs in other sectors of society. Costs and effects were analysed over five years.
Participants and methods
We compared the costs of treatment with sildenafil with that of conventional treatment. Before the introduction of sildenafil, injection therapy was the treatment of choice for erectile dysfunction.1 Many patients, however, were unwilling to receive injection therapy and accordingly did not seek treatment. We therefore assumed that injection therapy was accepted by 10% of patients (Pfizer, Netherlands, personal communication, 1998, based on market research). The vasoactive substance was papaverine-phentolamine and not alprostadil, which is more commonly used, because papaverine-phentolamine is less expensive and equally effective. Papaverine-phentolamine injections are reimbursed in the Netherlands, but no decision has yet been taken about reimbursement for sildenafil.
We estimated utility values for different states of erectile dysfunction. These utilities were applied to the clinical outcomes before and after treatment in a clinical trial of sildenafil by Goldstein et al.3 We also estimated the costs of two treatment scenarios for erectile dysfunction and analysed these in a model comprising the probabilities of successful treatment, switching and discontinuation of treatment, and duration of successful treatment. A detailed description of our methods to analyse costs and effects is available.4
Clinical effects
The study by Goldstein et al is the largest dose escalation study reported.3 It was placebo controlled and the patient population consisted of men with erectile dysfunction due to various causes. Efficacy was assessed with the international index of erectile function.5 This instrument contains questions about the two primary end points of erectile dysfunction treatment as defined by the National Institutes of Health—that is, the ability to penetrate and the ability to maintain an erection sufficient for satisfactory sexual intercourse.6 These end points were used in the trial. Both questions have five response levels, so together they categorise the patients into 25 (5×5) erectile dysfunction states. These erectile dysfunction states were valued in a separate exercise (described below). The elicited utilities were applied to the health states of the patients in the study of Goldstein et al before and after treatment. The difference between the mean utility before and after treatment (controlled for placebo) is the mean gain in utility. Use of disease specific instruments to calculate QALYs is advocated by Brazier and Dixon7 and Drummond et al.8
Because we used previously reported trial data, we had to consider the limitations of these data for use in economic evaluation. Firstly, the trial was designed on an intention to treat basis,3 which meant that patients for whom sildenafil had no or insufficient effect remained in the trial. As we could not discriminate between patients with a sufficient or an insufficient response, we used the mean utility gain in the trial to calculate the utility gain of sildenafil. Consequently, we underestimated the utility gain in daily practice because only the utility gain of the successfully treated patients should be taken into account. Secondly, results of the international index of erectile function were not available for injection therapy, nor were any other data that allowed calculation of QALYs. We conservatively assumed that the utility gain of sildenafil and papaverine-phentolamine injections would be the same. Given the low acceptability of injection therapy,9,10 this assumption probably overestimates the benefits of injection therapy.
Determining utilities for erectile dysfunction states
From a randomly selected sample of 45 000 people obtained from the Rotterdam telephone directory we recruited 354 people to participate in the valuation task. They were invited by telephone to attend a session of health state valuation and were offered about £10 plus travel expenses. In order to avoid selection bias, the invitation was made without referring to erectile dysfunction. Participants were given the opportunity to withdraw from the valuation sessions without financial consequences after they were informed about the subject of the study.
Participants valued 24 erectile dysfunction states on a scale from 0 to 1 using time trade-off.8 The 25th state described normal erectile functioning and was set at a value of 1.0. Time trade-off was measured relative to the life expectancy of the subjects. Before the valuation task, participants gained experience of the time trade-off method using general health states as defined by the EQ-5D questionnaire.11
Time trade-off responses were considered invalid if the participant showed a lexicographic response for the EQ-5D states, had too much missing data either on erectile dysfunction or EQ-5D states, or clearly did not understand the task. A lexicographic response mode means that when a respondent is faced with an option he or she will always choose one particular alternative, no matter how favourable the other might be. Subjects had to value the health states “for a person like yourself.” This means, for example, that older people gave values from their own perspective, and people without a sexually active partner would take this into account when performing the valuation task. The exception was that women were asked to imagine being a man with erectile dysfunction. Values are independent of the sexual activity of the respondents because the descriptions of erectile function referred to the relative number of successful attempts at intercourse. For example, a respondent might be asked the following: “If during the past four weeks, your condition was such that you were sometimes able to attain an erection, and you were (almost) never able to maintain your erection, how many years would you be willing to trade off to restore your erectile function?” This also implies that erectile function is valued the same in patients with different levels of sexual activity.
Because we had decided to obtain social valuations we asked a sample of the general public to value the clinical outcomes.8,12 The reasoning behind this decision relates to issues of equity and medical ethics.13 Some authors, however, claim that healthy people relatively similar to affected patients should value clinical outcomes.14 We therefore explored whether erectile dysfunction is valued differently in different subgroups. We used multivariate analysis of variance to determine whether age, sex, the availability of a partner, having children, sexual activity, and sexual satisfaction influenced the values of the general public.
Costs
All costs are expressed in 1999 British pounds (£1=1.62 euro). We used 1999 data to determine the Dutch cost prices. To determine the medical costs, we estimated resource use—for example, consultations and prescription charges (a lump sum charge to refund pharmacy costs and medicines) and multiplied the quantities by the unit prices. We estimated resource use of sildenafil and papaverine-phentolamine injections on the basis of consensus statements on both treatments.15 We refined this estimate by developing a low, baseline, and high cost scenario on the basis of clinical experience in two hospitals (University Medical Centre St Radboud, Nijmegen and Hospital St Antoniushove, Leidschendam). Costs outside the healthcare sector and productivity costs were assumed to be negligible.
The cost of sildenafil was based on observational data from the first quarter that sildenafil was available in the Netherlands.16 A general practitioner or urologist determined the effective dose in an academic or peripheral setting. An appropriate share of the costs of supporting departments was reflected in the cost of a visit to a urologist. The physician's costs were calculated on the basis of the estimated duration of an outpatient visit. The analysis included all costs related to the hospital, such as costs of salaries and supplies, costs of supporting departments, and overhead costs.
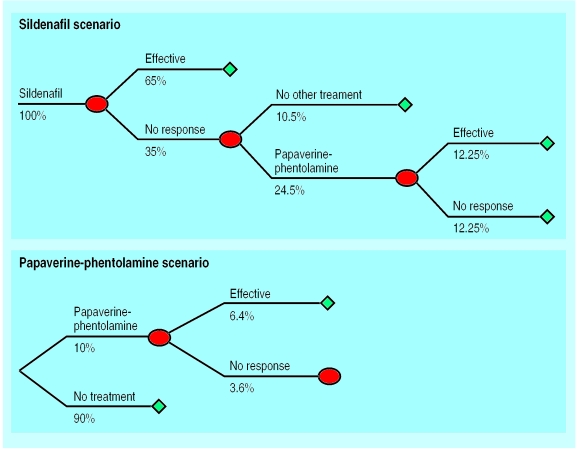
Cost effectiveness
We compared two scenarios: treatment with sildenafil and treatment with papaverine-phentolamine (figure). In the sildenafil scenario, we allowed patients to switch to papaverine-phentolamine injections, as these injections may be effective in patients in whom sildenafil has failed. Since sildenafil has already become the treatment of choice, although its cost is not reimbursed in the Netherlands, patients are unlikely to switch from injections to sildenafil. A switch was therefore not allowed in the papaverine-phentolamine scenario.
We compared the sildenafil and papaverine-phentolamine scenarios assuming use once a week. The maximum recommended frequency of papaverine-phentolamine injections is once a week, but use of sildenafil is not limited for medical reasons. Nevertheless, we believe that the assumption was appropriate as the utility values were elicited independently of the frequency of intercourse. Moreover, the marginal utility gain of increasing intercourse frequency from once to twice a week is unlikely to be as high as the increase between never being able to have intercourse and being able to have intercourse once a week.
The cost effectiveness of the different scenarios was analysed in a model comprising acceptability of treatment, probability of successful treatment, switching or discontinuation of treatment, and the duration of successful treatment. The patient flows in the model were determined on the basis of secondary data—for example, published clinical trials,9–20 Dutch observational data,16 and clinical experience in the two participating hospitals. We performed an incremental analysis of the costs and effects of sildenafil compared with papaverine-phentolamine. The results are presented as cost per QALY.
The acceptance rate of papaverine-phentolamine treatment could have been influenced by the fact that erectile dysfunction is no longer a taboo subject. In fact, an acceptance rate of 70% has been suggested as feasible.21 We therefore included this variable in a sensitivity analysis. Other variables included in the sensitivity analysis were resource use, values, effectiveness of treatment, and frequency of use. We performed univariate sensitivity analysis to determine which variables have the largest influence on the results. In the multivariate sensitivity analysis we explored to what extent results would change under a (unlikely) worst case scenario.
Results
Respondents
A total of 184 subjects (52%) failed to attend the interview sessions. This was probably because of extremely bad weather at the time of interview, which made it difficult for participants to reach the university. One person withdrew from the study after he was informed about the subject. A sample of 169 subjects valued the erectile dysfunction states; 89% (150) of the responses were valid. Age ranged from 18 to 80 years (mean age of 45.8 (SD 15.4) years). There were 81 men (54%) and 69 women, which is close to the sex distribution in the general population.
Effects
In Goldstein et al's study the international index of erectile function among men receiving sildenafil rose from 2.0 at baseline to 3.9 at end of treatment for ability to penetrate (placebo group 2.1 to 2.3) and from 1.5 to 3.6 for satisfactory sexual intercourse (placebo group 1.6 to 1.8).3 Table 1 gives the mean utilities that were elicited for the 24 erectile dysfunction states described by these two questions. The utilities ranged from 0.74 to 0.94. When these values are combined with trial data, the mean utility increased from 0.807 at baseline to 0.915 at end of treatment for men receiving sildenafil and from 0.819 to 0.821 for men receiving placebo. Therefore, the mean utility gain attributable to sildenafil is 0.11.
Table 1.
Mean (SD) utility values assigned by general public for erectile dysfunction (n=150)
| Ability to maintain an erection | Ability to attain an erection
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Never | Few times | Sometimes | Most times | Always | |||||
| Never | 0.74 (0.18) | 0.79 (0.17) | 0.82 (0.17) | 0.82 (0.15) | 0.84 (0.17) | ||||
| Few times | 0.77 (0.18) | 0.83 (0.16) | 0.85 (0.16) | 0.86 (0.15) | 0.88 (0.16) | ||||
| Sometimes | 0.79 (0.16) | 0.85 (0.14) | 0.87 (0.14) | 0.90 (0.13) | 0.91 (0.13) | ||||
| Most times | 0.81 (0.17) | 0.86 (0.15) | 0.88 (0.14) | 0.94 (0.12) | 0.93 (0.13) | ||||
| Always | 0.82 (0.17) | 0.87 (0.15) | 0.91 (0.13) | 0.94 (0.11) | 1.00 | ||||
We analysed whether the values of the general public were influenced by age, sex, availability of a partner, having children, sexual activity, and sexual satisfaction. The only relation we found was that participants with children considered erectile dysfunction less of a problem than subjects without children. Since there were no differences between the values of men and women, we used averaged values in the QALY analysis. More extensive description of this analysis is available.22
Costs
Tables 2 and 3 show the resource use and the costs attributable to treatment of erectile dysfunction with sildenafil or papaverine-phentolamine injections. Papaverine-phentolamine is cheaper per dose, but it has to be prescribed by an urologist and therefore has higher initial costs (£484 versus £407 for sildenafil). Sildenafil has higher running costs: yearly treatment costs are £254 versus £233 for papaverine-phentolamine. The higher initial costs of papaverine-phentolamine are recovered after seven years.
Table 2.
Volumes of resource use for sildenafil and injection treatment*
| Resource | Sildenafil | Injection |
|---|---|---|
| General model: | ||
| Acceptability of treatment (%) | 100 | 10 |
| % treated by general practitioner | 80 | 10 |
| % treated by urologist | 20 | 90 |
| No of pills or injections a week | 1 | 1 |
| Establishing effective dose: | ||
| No of visits | 3.8 | 3.7 |
| Mean duration of visits (min) | 8.5 | 10.3 |
| No of prescriptions16 | 2.5 | 2.3 |
| % discontinuing treatment9 10 17-20 | 35 | 36 |
| % switching because of effectiveness | 50 | 0 |
| Remaining part of first year: | ||
| No of visits | 2.0 | 2.0 |
| Mean duration of visits (min) | 7.5 | 7.5 |
| No of prescriptions16 | 7.8 | 4.3 |
| % discontinuing treatment (%) | 10 | 14 |
| Each following year: | ||
| No of visits | 1.5 | 1.5 |
| Mean duration of visits (min) | 7.5 | 7.5 |
| No of prescriptions16 | 9.5 | 5.2 |
| % discontinuing treatment | 5 | 5 |
As far as possible estimations are supported by scientific publications. When no scientific publications were available, estimations were derived from the opinion of clinical experts in the two participating hospitals. Figures of acceptability of treatment and proportion of patients treated by general practitioner or urologist were provided by Pfizer (based on market research, 1998).
Table 3.
Unit costs (£) of sildenafil and injection treatment
| Units of resource use | Cost price (without value added tax) |
|---|---|
| Sildenafil tablet16 | 4.33* |
| Papaverine-phentolamine injection | 3.55 |
| Visit to general practitioner (<20 min) | 10.32 |
| Visit to urologist (weighted mean, university/ peripheral hospitals) | 1.29/min plus16.80 |
| Prescription rule (charge to refund pharmacy costs) | 3.14 |
The mean cost price per pill is based on the “effective dose distribution” across the different strengths of sildenafil.
Cost effectiveness
Overall, sildenafil creates more benefits and more costs because more patients are treated (figure). Therefore, the main issue is whether the additional effects of sildenafil are worth the additional costs. This question is addressed in the incremental analysis shown in table 4. The incremental cost utility ratio of sildenafil compared with papaverine-phentolamine is £3639 per QALY in the first year, decreasing to £2630 per QALY after five years.
Table 4.
Costs and effects of treatment with sildenafil and papaverine-phentolamine injection and difference between two treatments
| Year | Successfully treated patients (%)
|
Incremental cumulative effects (QALY) | Incremental cumulative costs (£) | Incremental cost utility ratio (£/QALY) | |
|---|---|---|---|---|---|
| Sildenafil | Injection | ||||
| 1 | 77.25 | 6.40 | 7.79 | 28 368 | 3639 |
| 2 | 69.53 | 5.50 | 14.84 | 44 773 | 3017 |
| 3 | 66.05 | 5.23 | 21.53 | 60 356 | 2803 |
| 4 | 62.75 | 4.97 | 27.88 | 75 161 | 2695 |
| 5 | 59.61 | 4.72 | 33.92 | 89 226 | 2630 |
| ∞* | 2329 | ||||
In year N the incremental cost utility ratio is a function of the incremental cumulative costs divided by incremental cumulative effects over these N years. But if you look at the cost utility ratios in the first and second year separately, you get an incremental cost utility ratio of £3639 per QALY in the first year and £2329 per QALY in the second year. The incremental cost utility ratio is constant from the second year on: £2329 per QALY. So, in the long term, the influence of the first year treatment costs is diminishing and the incremental cost utility ratio approaches £2329 per QALY.
Sensitivity analysis
The frequency of use influences the outcomes considerably. Doubling the frequency of use of sildenafil increases the cost per additional QALY by 45% in the first year and 85% in each following year. The initial costs are relatively high because the costs of non-responders are added to the costs of responders. Hence, the effect of the frequency of use on the cost per additional QALY is moderated in the first year. In the long term, however, the main cost driver with sildenafil is the drug.
Assuming a lower utility gain (0.08) than observed in the valuation study, resulted in a 37.5% increase in cost per additional QALY.4 Effectiveness and acceptability also influenced the results significantly. The cost per additional QALY increased 38% with a lower effectiveness of sildenafil (50%), but decreased (1%) in each following year. Changes in acceptability had an opposite effect: when acceptability of papaverine-phentolamine injections is increased to 70%, the incremental cost utility ratio is 25% lower in the first year, but 10% higher from the second year onwards. Uncertainty about resource use did not influence the outcomes significantly; in the analysis of different cost scenarios (based on the number of visits and duration of visits), the high cost scenario increased the costs per additional QALY by only 8%.
When the uncertainty of all variables is combined into a worst case model (low utility gain and effectiveness and high costs, dropout, and acceptability), the incremental cost utility ratio is £9343 per QALY in the first year(156% increase), and £4691 in each following year(101% increase).
Discussion
The mean incremental cost utility ratio of sildenafil compared with papaverine-phentolamine was £3639 per QALY in the first year and improved in the following years. This cost utility ratio is generally favourable, as suggested acceptable thresholds of cost utility vary between £8000 and £25 000.23,24 Moreover, many interventions with less favourable cost utility ratios are currently being funded, such as breast cancer screening (£5780 per QALY) and kidney transplantation (£4710 per QALY).25 Uncertainty in the data did not hamper interpretation of the results: even in the worst case scenario, the incremental cost utility ratio of £9343 could be considered favourable. Our analysis therefore suggests that the clinical effect is derived at reasonable costs.
Validity of assumptions
We made several assumptions that could be viewed as unfavourable to sildenafil. For instance, we underestimated the effects by not including partner satisfaction and we assumed the effects of oral and injection treatment to be equal. Furthermore, we used a relatively low rate of drop out for injection therapy, which results in a more favourable cost effectiveness ratio for injection therapy.9–20 Although such assumptions might introduce bias, the interpretation of the results is not greatly affected because the assumptions in the economic appraisal of sildenafil were conservative.
The utility values we elicited for erectile dysfunction did not take into account possible comorbidity. As in most cases total disutility is less than the sum of parts,26 we might have overestimated the effect. However, the sensitivity analysis showed that sildenafil remained cost effective with lower utility gains.
The subjective nature of the value of erectile functioning again raises issues about whose values should be used in economic appraisal of health care: the values of the general public or those of people at risk (in our case ageing men). However, we found that the utility values for sexual functioning were independent of background variables such as age, sex, and sexual activity. Therefore, neither the limitations in the representativeness of our sample, nor our choice to elicit values from the general public has influenced the results.
Implications
These findings should be interpreted in the light of the discussion about the affordability and value of sildenafil to society. Firstly, we have shown that erectile dysfunction limits quality of life considerably, in the eyes of the general public. Furthermore, our study shows that sildenafil is cost effective, and its reimbursement should therefore be considered. However, as frequency of use greatly affects cost, such reimbursement should not be unconditional.
What is already known on this topic
Clinical research suggests that sildenafil is an effective treatment for erectile dysfunction
Economic appraisal of sildenafil is needed given the prevalence of the disorder and controversy regarding funding of treatment
What this study adds
Erectile dysfunction is generally perceived as a disease that limits quality of life considerably
The clinical effect of sildenafil is derived at reasonable costs
Health service funding of sildenafil should be considered
Figure.
Patient flow for scenarios of treatment of erectile dysfunction with sildenafil or papaverine-phentolamine injections
Acknowledgments
We thank L Damen and P Rabsztyn, who provided us with details about the treatment scenarios. Blauw Call Centre Rotterdam recruited the general population subjects, L van der Hell assisted with the interviews, and Rosalind Rabin edited the English.
Footnotes
Funding: This research project was undertaken in support of the economic report requested by the Dutch Health Authorities to inform their decisions regarding the reimbursement of sildenafil. The research was supported by an unrestricted grant from Pfizer BV in the Netherlands.
Competing interests: All authors have received reimbursements from Pfizer for attending symposia or fees for consultancy and speaking or both.
References
- 1.Dinsmore W, Evans C. ABC of sexual health: erectile dysfunction. BMJ. 1999;318:387–390. doi: 10.1136/bmj.318.7180.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 3.Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker WA.for the Sildenafil Study Group. Oral sildenafil in the treatment of erectile dysfunction N Engl J Med 19983381397–1404. [DOI] [PubMed] [Google Scholar]
- 4.Stolk EA, Busschbach JJV, Caffa M, Meuleman EJH, Rutten FFH. The cost-utility of Viagra in the Netherlands. Rotterdam: Institute for Medical Technology Assessment; 1999. . (No 99.49.) [Google Scholar]
- 5.Rosen RC, Riley A, Wagner G, Osterloh IA, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 6.National Institutes of Health Consensus Conference. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- 7.Brazier J, Dixon S. The use of condition specific outcome measures in economical appraisal. Health Econ 1995:255-64. [DOI] [PubMed]
- 8.Drummond MF, O'Brien B, Stoddart GI, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 1997. [Google Scholar]
- 9.Mulhall JP, Jahoda AE, Cairney M, Goldstein B, Leitzes R, Woods J, et al. The causes of patient dropout from penile self-injection therapy for impotence. J Urol. 1999;162:1291–1294. [PubMed] [Google Scholar]
- 10.Althof S, Turner L, Levine S, Risen C, Kursch E, Bodner D, et al. Why do so many people drop out from auto-injection therapy for impotence? J Sex Marital Therapy. 1989;15:121–129. doi: 10.1080/00926238908403816. [DOI] [PubMed] [Google Scholar]
- 11.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 12.Gold MR, Patrick DL, Torrance GW, Fryback DG, Hadorn DC, Kamlet MS, et al. Identifying and valuing outcomes. In: Gold M, Siegle J, Russel L, Weinstein M, editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. pp. 82–134. [Google Scholar]
- 13.Williams A. Economics, QALYs and medical ethics. A health economist's perspective. York: Centre for Health Economics, York Health Economics Consortium, NHS Centre for Reviews and Dissemination; 1994. . (Discussion paper 121.) [DOI] [PubMed] [Google Scholar]
- 14.Hadorn DC. The role of public values in setting health care priorities. Soc Sci Med. 1991;32:773. doi: 10.1016/0277-9536(91)90303-t. [DOI] [PubMed] [Google Scholar]
- 15.Diagnosis and treatment of erectile dysfunction: step by step. Round table conference. Rotterdam: Medicom Excel; 1998. (In Dutch.) [Google Scholar]
- 16.Foundation of Pharmaceutical Statistics. Pharmaceutical statistics. The potency of Viagra in the Netherlands. Weekly Pharmaceutics 1999;134(6).
- 17.Meuleman EJH, Van Berkel JTH, Rabsztyn P, Damen L. Sildenafil (Viagra) in the treatment of erectile dysfunction. Ned Tijdschr Geneesk. 1998;142:2337–2341. . (In Dutch.) [PubMed] [Google Scholar]
- 18.Jarow JP, Burnett AL, Geringer AM. Clinical efficacy of sildenafil citrate based on etiology and response to prior treatment. J Urol. 1999;162:722. doi: 10.1097/00005392-199909010-00024. [DOI] [PubMed] [Google Scholar]
- 19.Jackson SE, Lue TF. Erectile dysfunction: Therapy health outcomes. Urology. 1998;51:874–882. doi: 10.1016/s0090-4295(98)00141-1. [DOI] [PubMed] [Google Scholar]
- 20.Korenman SG. New insights into erectile dysfunction: a practical approach. Am J Med. 1998;105:135–144. doi: 10.1016/s0002-9343(98)00191-0. [DOI] [PubMed] [Google Scholar]
- 21.Lycklama à Nijeholt AAB. The erection pill. Ned Tijdschr Geneesk. 1998;142:2332–2333. . (In Dutch.) [PubMed] [Google Scholar]
- 22.Stolk EA, Busschbach JJV. Differences in the values given by the general public and patients to health states of erectile dysfunction. In: Stolk EA, Busschbach JJV, editors. The cost-utility of Viagra in the Netherlands. Rotterdam: Institute for Medical Technology Assessment, Erasmus University; 1999. pp. 65–82. , appendix B. [Google Scholar]
- 23.Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can Med Ass J. 1992;146:473–481. [PMC free article] [PubMed] [Google Scholar]
- 24.Goldman L, Gordon DJ, Rifkind BM, Hulley SB, Detsky AS, Goodman DS, et al. Cost and health implications of cholesterol lowering. Circulation. 1992;85:1960–1968. doi: 10.1161/01.cir.85.5.1960. [DOI] [PubMed] [Google Scholar]
- 25.Maynard AK. Developing the health care market. Econ J. 1991;101:1277–1286. [Google Scholar]
- 26.Furlong W, Feeny D, Torrance GW, Goldsmith CH, DePauw S, Zhu Z, et al. Multiplicative multiattribute utility function for the health utilities index mark 3 (HUI 3) system: a technical report. Hamilton, Ontario: McMaster University Centre for Health Economics and Policy Analysis; 1998. pp. 5–6. . (Working paper 98-11.) [Google Scholar]