Abstract
Background
The medical peer-review committees and arbitration boards of the Medical Associations of the individual German federal states assess claims for damages arising from alleged medical malpractice.
Methods
189 panel proceedings concerning alleged malpractice in the treatment of fractures in children were evaluated on the basis of the available documentation and decisions. The proceedings were evaluated with respect to the involved medical specialties and treatment facilities, the types of fracture and particular allegations in each case, the actual malpractice found to have been committed (if any), and the harm resulting from malpractice. The cases were derived from the nine German states for which the North German arbitration board is responsible.
Results
An actual malpractice was found to have been committed in 64% of cases, or about twice as frequently as the average rate among all cases going before an arbitration board in Germany. Most of the medical errors involved inaccurate diagnostic evaluation, misinterpretation of radiological findings, inappropriate treatment for the particular type of fracture involved (conservative rather than operative, or vice versa), or inadequate follow-up of the fracture (or none at all). The highest rate of a positive finding of malpractice involved fractures in the elbow region (77%). A mild or moderate degree of permanent injury due to malpractice was found in 37 cases (31%) and severe permanent injury in 16 cases (13%).
Conclusions
The appropriate treatment of fractures in children requires experience in clinical examination as well as knowledge of radiological anatomy and of the problematic fracture types and localizations. The results reported here should raise consciousness of the possibilities for medical error and thus help prevent future instances of malpractice.
Keywords: pediatric diseases, fracture, malpractice, physician liability, arbitration
The malpractice review committees and arbitration boards of the medical associations in Germany perform extrajudicial evaluations of claims of injury arising from alleged medical malpractice. The proceedings are carried out in accordance with German legislation and relevant judicial decisions relating to private law and civil procedure. At the end of each proceeding, the arbitration board issues a decision relating to the claims that were made; this decision is not binding upon any of the parties involved (i.e., neither the patient, nor the physician, nor the physician’s malpractice insurance carrier). The main aim of these proceedings, i.e., the avoidance of a lawsuit, is achieved in over 90% of cases. The North German Arbitration Board was established in November 1976. Since then, it has processed malpractice claims submitted by more than 77 000 patients. Its mode of operation has already been the subject of multiple articles (1– 5).
The finding that malpractice has or has not been committed is based on an expert review of the treatment process, in which not only the medical aspects per se, but also questions of communication and documentation must be considered. This article is not concerned with an evaluation of different methods of treatment, but rather with the types of conclusions that can be drawn by expert reviewers on the basis of current medical knowledge about the treatment of fractures in children. For more information on the current state of medical knowledge, the reader is encouraged to refer to well-known textbooks in pediatric traumatology (6– 9). The goal of the present analysis is to define a basis for quality control and error avoidance.
Methods
In this article, we present a statistical summary of 189 arbitration proceedings that were related to the treatment of fractures in children and that were carried out in the 8-year period from 2000 to 2007. The mean number of cases was about 24 per year. Cases before 2000 were not thoroughly documented with all of the statistical information needed for this type of evaluation. The individual cases were documented in the Medical Error Reporting System (MERS) of the North German Arbitration Board (11, 12); the authors individually evaluated each case, taking into consideration the facts of the case, the findings of the expert reviewers, and the decision of the arbitration board. All cases submitted for arbitration arose from experiences that medical laypersons (i.e., the patients and their families) considered to be negative, in the context of fracture treatment in children. The cases were highly diverse with respect to the complaints made, the facts in each case, and the methods by which they were evaluated. Because of this heterogeneity, calculations of statistical significance (e.g., with the chi-square test) would not appear to be reasonable for the findings that we will describe below, and were therefore not performed.
Results
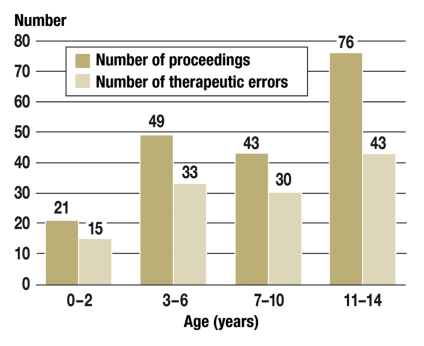
The age distribution of the children involved in the cases submitted for arbitration, which is shown in Figure 1, reflects the changing experiences of children in their environment as they grow (10). The frequency of claims relating to fracture treatment corresponds statistically to the epidemiology of fractures in children (7): in other words, there does not seem to be any particular age group in which claims are brought significantly more often. Four cases of birth trauma are included in the age group 0–2 years.
Figure 1.
Arbitration proceedings after the treatment of fractures in children (N = 189): age distribution and number of proceedings in which a therapeutic error was confirmed (n = 121, or 64%). The age distribution is practically identical for boys (n = 99) and girls (n = 90).
Table 1 shows the number of arbitration proceedings, the number of hospitals and/or doctors against whom claims were made, the claims and allegations that were made, and the findings regarding whether malpractice had, in fact, been committed. These are the basic data underlying the remainder of the analysis in this paper. In the discussion that follows, each of these figures will be looked at more closely, so that specific questions can be answered with relevant statistics.
Table 1. Arbitration proceedings after the treatment of fractures in children.
| n | % | ||
| Number of proceedings | 189 | 100 | |
| Proceedings in which malpractice was confirmed | 121 | 64 | |
| Total number of hospitals/doctors involved in proceedings | 213 | 100 | |
| Number of proceedings against: | |||
| A single hospital/doctor | 189 | 90 | |
| Two hospitals/doctors | 18 | 9 | |
| Three hospitals/doctors | 3 | 1 | |
| Number of persons/institutions found to have committed malpractice | |||
| (in 7 cases, two hospitals/doctors were found to have committed malpractice in a single case) | 128 | 60 | |
| Number of defined complaints/allegations that were made | 282 | 100 | |
| Confirmed malpractice related to the allegations | 174 | 62 | |
In 53 cases, more than one therapeutic error was found to have been committed. The evaluative procedure of the North German Arbitration Board takes the entire process of treatment into account, regardless of the particular statements of the claimant (i.e., an investigative evaluation is performed). Thus, therapeutic errors were sometimes found that had not been alleged in the patient’s original request for arbitration by the Board.
All of the medical specialties and treatment facilities involved in the cases submitted for arbitration are shown in Table 2. Non-surgical specialties were involved in 15 cases (7%). The percentage of errors is always given with the number of defined patient allegations (table 4) as the denominator. The 189 proceedings involved 213 hospitals and doctors, against whom a total of 282 allegations were made.
Table 2. Arbitration proceedings after the treatment of fractures in children.
| Specialty and site of treatment | Persons and institutions against whom proceedings were initiated, N1 | Complaints made, N2 | Therapeutic errors (avoidable errors confirmed by arbitration board), n | Therapeutic errors, (n/N2, expressed in percent) |
| Trauma surgery, including hand surgery | ||||
| Hospital, inpatient | 71 | 99 | 55 | 56 |
| Hospital, outpatient | 32 | 41 | 26 | 63 |
| Doctor’s office | 21 | 25 | 17 | 68 |
| Total: | 124 | 165 | 98 | 59 |
| General/visceral surgery | ||||
| Hospital, inpatient | 14 | 22 | 14 | 64 |
| Hospital, outpatient | 15 | 16 | 14 | 88 |
| Doctor’s office | 21 | 27 | 19 | 70 |
| Total: | 50 | 65 | 47 | 71 |
| Pediatric surgery | ||||
| Hospital, inpatient | 12 | 16 | 12 | 75 |
| Hospital, outpatient | 3 | 5 | 1 | 20 |
| Doctor’s office | 1 | 2 | 1 | 50 |
| Total: | 16 | 23 | 14 | 61 |
| Orthopedics | ||||
| Doctor’s office | 8 | 11 | 5 | 45 |
| Pediatrics | ||||
| Hospital | 4 | 5 | 1 | 20 |
| Doctor’s office | 1 | 2 | 2 | 100 |
| Total: | 5 | 7 | 3 | 43 |
| General medicine | ||||
| 3 | 4 | 4 | 100 | |
| Otorhinolaryngology | ||||
| Doctor’s office (1 facial & 2 nasal fractures) | 3 | 3 | 1 | 33 |
| Obstetrics | ||||
| Hospital | ||||
| (2 cases of birth trauma) | 2 | 2 | 1 | 50 |
| Anesthesiology | ||||
| Hospital | ||||
| (2 incidents involving general anesthesia) | 2 | 2 | 1 | 50 |
| Total | 213 | 282 | 174 | 62 |
Note: There were many cases in which more than one allegation was made and/or more than one error was confirmed.
Table 4. Arbitration proceedings after the treatment of fractures in children.
| Numerical designation of error type in the classification system of the arbitration board (MERS) | Type of error, in the light of the special requirements of fracture treatment in childhood | Complaints | Therapeutic errors | |
| N | n | % n/N | ||
| 110*1 | Deficient medical competence (e.g., failure to refer or to obtain consultation, and the like) | 2 | 3 | 150 |
| 210 | Nonperformance of a physical examination, or failure to examine adequately in view of symptoms | 4 | 4 | 100 |
| 230 | Error in radiological diagnosis, failure to note a fracture, erroneous assessment of the fracture pattern | 64 | 51 | 80 |
| 300 | Failure to recognize the indication for surgical treatment, non-indicated treatments | 15 | 10 | 67 |
| 500 | ||||
| 310 | Faulty conservative treatment and follow-up of fracture | 93 | 48 | 52 |
| 400 | ||||
| 510 | Faulty operative treatment of fracture | 69 | 39 | 57 |
| 550 | Faulty postoperative care, especially failure to perform corrective procedures | 35 | 19 | 54 |
| Total | 282 | 174 | 62 | |
This table shows the number of complaints and errors corresponding to each of the categories in the classification system currently used by the Arbitration Board of the North German Medical Associations (two cases involving incidents under general anesthesia are not included.)
*1 In one case, an error was found by the Arbitration Board that had not been alleged by the claimant.
As one might expect, trauma surgery, including hand surgery in a few cases, was the most commonly involved specialty, accounting for 124 (58%) of the involved hospitals and doctors. It must be mentioned, however, that trauma surgery was always considered to have been the involved specialty for statistical purposes whenever trauma surgery was represented at the site of treatment (as demonstrated, e.g, by the letterhead over the doctor’s note), even if the treatment itself was not provided by a specialist in trauma surgery (e.g., because the trauma surgeon was on back-up call at the time). Clarification of organizational questions of responsibility within medical treatment units is not a task of the arbitration board.
The distribution of arbitration proceedings with respect to various sites of fracture differs markedly from the natural distribution of fractures; the discrepancy is particularly notable for a few specific fracture sites (table 3). Among all claims submitted to arbitration, the percentage involving transcondylar fractures of the humerus, for example, was three times as high as the epidemiological frequency of fractures at this site among all pediatric fractures. A similar situation obtains for elbow fractures and dislocations (five times as high) and for femur fractures (six times as high). In contrast, clavicular fractures, which are very common, accounted for only a single case submitted to arbitration (in which, in fact, no malpractice was found). Clinical experience yields no plausible explanation for the notably greater number of claims from girls than from boys with elbow fractures (M : F = 14 : 25), but the greater number of claims from boys with forearm fractures (M : F = 27 : 12) presumably reflects greater risk-taking in play and sports (7).
Table 3. Arbitration proceedings after the treatment of fractures in children.
| Fracture site | Percentage of fractures at this site during the period of bone growth (%)*1 | Number of proceedings | Sex distribution | Therapeutic errors | |||
| N | % N/189 | M | F | n | % n/N | ||
| Skull, face | 2 | 8 | 4.2 | 4 | 4 | 4 | 50 |
| Spine | < 1 | 1 | 0.5 | – | 1 | – | – |
| Chest (bones) | < 1 | – | – | – | – | – | – |
| Clavicle (n = 1), scapula (n = 1) | 7 | 2 | 1.1 | 1 | 1 | – | – |
| Humerus, subcapital and shaft | 3 | 8 | 4.2 | 3 | 5 | 3 | 38 |
| Humerus, transcondylar | 5 | 26 | 13.8 | 14 | 12 | 15 | 58 |
| Elbow fractures and subluxations | 4 | 39 | 20.7 | 14 | 25 | 30 | 77 |
| Forearm | 37 | 39 | 20.7 | 27 | 12 | 23 | 59 |
| Hand | 19 | 17 | 9.0 | 11 | 6 | 11 | 65 |
| Pelvis | < 1 | 1 | 0.5 | – | 1 | – | – |
| Femur | 2 | 24 | 12.5 | 14 | 10 | 17 | 71 |
| Leg, ankle | 11 | 18 | 9.6 | 8 | 10 | 14 | 78 |
| Foot | 10 | 6 | 3.2 | 3 | 3 | 4 | 67 |
| Total | – | 189 | 100.0 | 99 | 90 | 121 | 64 |
Allegations and frequency of confirmed errors in 189 proceedings, including 4 involving birth trauma; comparison of the number of proceedings with the frequency distribution of fracture sites during the period of bone growth.
*1 The percentages given here are reproduced from Marzi (6), sometimes after averaging or extrapolation. The numbers appearing in boldface type in this column and the fourth column (percentage of proceedings) indicate fracture sites for which there is a notable disproportion between the frequency of fractures and the frequency of complaints
Table 3 also includes four cases of birth trauma, which were as follows:
An undetected skull fracture after a forceps delivery, diagnosed only later because of a "growing fracture" and then surgically treated. In this case, both the forceps delivery and the failure to detect the fracture were judged to have been therapeutic errors. Mild neurological impairment was judged to have resulted from these errors.
One case of humerus fracture and one case of a fracture of the femoral shaft, both caused by rotation maneuvers. No malpractice was found to have been committed, nor were the fractures found to have had any effect on limb development.
A combined femoral and tibial fracture due to a technically difficult, reoperative caesarean section. No malpractice was found to have been committed. Limb development was normal.
The allegations that were made, and the therapeutic errors that were confirmed by the Arbitration Board, are listed in Table 4 according to the error classification and coding scheme of the Medical Error Reporting System (MERS) (11, 12). Most of the allegations and errors were easy to classify in this scheme. In 93 of the arbitration proceedings, two defined allegations were made, according to this classification system; in 53 cases, a medical error (malpractice) was confirmed.
The most frequent type of error by far was in the area of radiological diagnosis (80%). Errors of this type were classified as having arisen within the clinical specialty that was responsible for the treatment of the patient. The Arbitration Board could not assess the provisions within clinical departments regarding the assignment of individual responsibility for radiological fracture diagnosis. In some cases, a radiologist’s faulty diagnosis was uncritically accepted by the treating physician. Nor could it be determined from the medical record to what extent the subspecialty area of pediatric radiology was involved in the radiological diagnosis of each individual case.
Errors in the conservative treatment and follow-up of fractures mainly consisted of failure to perform closed reposition (or to perform it satisfactorily), resulting in a deformity after healing of the fracture, and failure to perform follow-up x-ray studies (or to perform adequate ones), resulting in the failure to diagnose a re-dislocation requiring correction. Other problems that commonly gave rise to malpractice claims were pressure injuries from plaster casts, which ranged from small pressure ulcers to Volkmann’s contractures (2 cases), as well as skin damage from the plaster or from the removal of the cast. The category of conservative fracture treatment had the highest percentage of rejected claims (48%). This fact is largely accounted for by the frequent occurrence, through no fault of the treating physician, of re-dislocation requiring a second surgical procedure. In such cases, the parents often incorrectly inferred from the re-dislocation that the primary treatment must have been faulty.
Out of all cases in which the alleged error related to the operative treatment of a fracture, an actual error was confirmed in 57%. Most of the time, the error involved the faulty performance of an osteosynthesis procedure, resulting in the need for corrective measures or in an unsatisfactory result after healing. Out of 15 allegations of failure to recognize the indication for surgery or of use of the wrong operative technique, 10 were followed by a determination that an error had, in fact, been committed. Code 550 encompassed all problems arising in the patient’s postoperative course, including omitted or faulty reoperative procedures. Fracture-related infections were not judged to have been due to a treatment error in any case.
The error codes 110 (inadequate medical competence) and 210 (failure to perform indicated diagnostic tests) were less commonly represented, but they nonetheless merit some brief comments in view of their fundamental importance:
Two fractures and one subluxation of the radial head were judged to have been overlooked because of inadequate medical competence. These cases occurred in hospital outpatient departments. The patients were clinically examined by a junior trainee or by a resident in a non-surgical specialty and were not presented to a specialist. The fractures and the subluxation were missed. The Arbitration Board determined that faulty procedure had been followed regarding the assumption of responsibility for the care of the patient, possibly because of faulty organization. Four further cases concerned fractures that were missed because of non-performance, or inadequate performance, of a physical examination, as a result of which no x-rays were obtained. The involved specialties in these cases were general surgery (2 cases), trauma surgery, and general medicine.
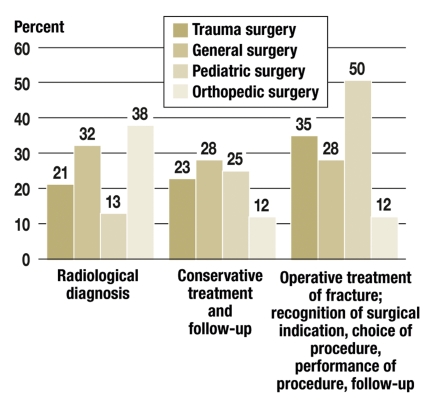
The frequency of errors in the various categories is shown in Table 4 and broken down by treating specialties in Figure 2. Figure 2 initially provides no more than a statistical overview, leading to the not very informative conclusion that all types of errors were made everywhere. Deeper analysis relating to particular sites and types of fracture requires the evaluation of further data, including the specifics of each case. Figure 2 shows a comparison of the frequency of common types of treatment error across surgical specialties. Statistical evaluation with a chi-square test reveals no significant differences among specialties.
Figure 2.
Arbitration proceedings after fracture treatment in children: comparison of the frequency of confirmed errors committed in each of the surgical specialties (in several cases, two errors were confirmed in a single proceeding).
Trauma surgery: N = 124, n = 98
General surgery: N = 50, n = 44
Pediatric surgery: N = 16, n = 14
Orthopedic surgery: N = 8, n = 5
N = number of hospitals/doctors involved in proceedings;
n = number of confirmed errors
When the results of the proceedings of the North German Arbitration Board were statistically evaluated in the framework of the MERS, the causal relationship between the (alleged and/or confirmed) therapeutic error and the damage to the patient’s health was categorized as follows:
damage resulting from malpractice,
damage as an undesired consequence of correct treatment,
damage as an inevitable consequence of the patient’s disease (or accidental injury) after correct treatment.
Seven different "damage classes" (DC 0 through 6) were defined as shown in Table 5 (no patient sustained a damage in DC 6, i.e., death). In 13 cases (11%), an error was confirmed but was not considered to have caused the subsequent damage. The damage was, at most, mild (DC 0–2) in 43% of cases, and of a more substantial degree (DC 3–5) in 57%. These figures reflect the highest damage class attained by each patient in his or her clinical course; one can, therefore, assume that permanent damage (DC 4 or 5) was often preceded by severe, transient damage (DC 2 or 3), even though this cannot be seen from Table 5. Mild to moderately severe permanent damage (DC 4) was almost always well compensated in the affected children and did not restrict their activities in any way, except that it limited some children’s participation in competitive sports. In contrast, severe, permanent damage often led to major disturbances of childhood development: functional disturbances, disfigurement due to the deformity of the affected limb, restricted play and sporting activities, limitation of occupational choices, and, sometimes, psychological sequelae and rejection by the child’s peer group. Having to give up a musical instrument was mentioned in some cases as well. Among the 16 cases of severe, permanent damage due to malpractice, 13 were related to elbow fractures, 2 to ankle fractures, and 1 to a talus fracture.
Table 5. Arbitration proceedings after the treatment of fractures in children.
| Damage class (DC) | Definition | n | % n/121 |
| 0 | No demonstrable damage or lack of causation (the damage cannot be shown to have been caused by the error) | 13 | 11 |
| 1 | Trivial damage (e.g., slight prolongation of the duration of treatment, pain suffered for a slightly longer time than necessary) | 13 | 11 |
| 2 | Mild to moderately severe, transient damage (e.g., prolonged duration of treatment with corrective procedures) | 26 | 21 |
| 3 | Severe, transient damage (e.g., long course of treatment with multiple complications and multiple corrective procedures, yet with restoration of normal function in the end) | 16 | 13 |
| 4 | Mild to moderately severe, permanent damage (e.g., mild to moderately severe, permanent impairment of joint or limb function, permanent nerve damage) | 37 | 31 |
| 5 | Severe, permanent damage (e.g., severe, permanent impairment of joint or limb function with deformity or Volkmann’s contracture; adverse effect on range of occupational choices) | 16 | 13 |
| Total | 121 | 100 |
Damage classes (DC) in 121 arbitration procedures in which an error was confirmed
Discussion
Statistical data on judicial proceedings related to medical malpractice in Germany are not available. Information on certain highly illustrative cases is sometimes made available to the public by decision of the highest courts in the individual German states, or of the Supreme Court. Nor are there many detailed publications available on extrajudicial malpractice proceedings. Madea and Dettmeyer have written an instructive book on medical malpractice in Germany (13). The North German Arbitration Board publishes an illustrative case report every month, which usually appears in Niedersäschsisches Ärzteblatt (journal of the Lower Saxony Medical Association) and on its website www.schlichtungsstelle.de. Some of these cases have concerned the treatment of fractures in children (14–17).
In contrast, a large amount of statistical data on judicial malpractice proceedings is available from the USA, partly in the form of serial publications dedicated to the subject. Many of these are produced by a collaboration of physicians, insurance companies, and legal institutions. Some good examples are the publications of Gwynne et al. (18), Phillips et al. (19), Selbst et al. (20), Skaggs and Pershad (21), and Studdert et al. (22). Nonetheless, we were unable to find data in the American literature on the treatment of fractures in children that might be usefully compared with the figures presented here. We met with a similar lack of data for international comparison once before, while performing an analogous study of therapeutic errors in acute appendicitis (23).
Among all cases brought before the North German Arbitration Board that are concerned with alleged malpractice involving children, fracture treatment is the most commonly represented category, with about 24 cases per year, while appendicitis is in second place, with about 10 per year. A like tendency is borne out by the relevant American statistics, in which fractures and appendicitis also occupy first and second place, respectively (19).
Fracture treatment in children is also the category in which alleged treatment errors are most commonly confirmed to have occurred, with a confirmation rate of 62% (table 4). The mean confirmation rate for all categories is approximately 30%.
A direct comparison of these data with the findings of clinical studies would be inappropriate, for two main reasons:
The frequency of errors in the treatment of certain types of fracture is highly disproportionate to their natural incidence (table 3).
Clinical studies do not differentiate complications due to malpractice from those not due to malpractice.
Fractures in children are classified by means of a clear and systematic conventional terminology (see textbooks on the subject); more complicated, scientific classifications of fractures are generally of little or no relevance to issues of potential malpractice. The fracture pattern is often described imprecisely in the medical records (and even, sometimes, in written expert opinions). This can have unfortunate consequences, particularly if the patient is sent to another institution to be treated, but the x-rays are not sent along with the patient. The following are some typical imprecise descriptions of fractures:
distal humerus fracture, instead of supra- or diacondylar humerus fracture;
elbow fracture, without any more precise specification;
proximal radius fracture, instead of fracture of the radial head;
distal radius fracture, without any statement regarding epiphyseal involvement;
ankle fracture, without any more precise specification.
When the treating physician uncritically accepts another physician’s imprecise classification of the fracture and does not personally inspect the patient’s x-rays, this in itself constitutes a therapeutic error.
The treatment of fractures in children is not explicitly mentioned in the official training curricula for the pertinent medical specialties in Germany. The following can be considered prerequisites for the appropriate treatment of fractures in children:
experience in the clinical examination of injured children, particularly infants and toddlers; recognition of the fact that pain can be projected to sites other than the fracture site itself;
knowledge of the radiological anatomy of the juvenile skeleton;
knowledge of the main problematical areas—elbow, femoral neck, ankle;
availability of a textbook on the treatment of fractures in children, as an aid to the proper diagnosis and treatment of rare fracture types;
access to a referral center for the further diagnostic evaluation and treatment of rare or problematic fracture types.
Without going into further detail regarding specific types of fractures, the experience of the North German Arbitration Board reveals that the following errors typically occur in the treatment of fractures in children:
imprecise clinical examination (infants and toddlers); failure to obtain x-rays; x-rays of the wrong area of the body;
misinterpretation of x-rays, resulting in a fracture or dislocation being overlooked or misdiagnosed;
erroneous assessment of the degree of stability of a fracture when treated conservatively; undiagnosed and untreated re-dislocation;
failure to inform the child’s parents about the possibility of re-dislocation of an unstable fracture after correct initial reposition, leading the parents to suspect that the initial treatment was incorrect; failure to give adequate information about treatment;
failure to treat a re-dislocation in timely fashion, with surgery if necessary;
inappropriately waiting for the patient’s further growth to compensate for shaft fractures that are markedly dislocated, either primarily or secondarily, in younger or older children (see textbooks);
faulty evaluation of fractures that have healed with a deformity; failure to perform timely corrective measures when the patient is still young enough for remodeling to occur;
joint mobilization under general anesthesia when the injury has already healed with a deformity, i.e., when the limitation of movement has an anatomical cause;
ordering physical therapy (passive movement exercises) when the limited range of motion is due to a deformity—this is a common error (6).
The high remodeling potential of bone in children (which declines as they grow older) explains why nearly all fractures in childhood will heal without any negative consequences if properly treated. In the rare cases of problematic healing that are attributable to the fracture type itself, there is generally a deformity or functional disturbance due to the direct or indirect involvement of the growth apparatus, ischemic bony necrosis (in fractures of the radial head, femoral heck, and talus), or a comminuted fracture. Overall, the vast majority of fractures in children can be expected to heal with full restoration of normal anatomy and function, particularly when the fracture involves the bony shaft or epiphysis. Thus, problematic healing in the form of a persistent deformity and/or functional disturbance, when the fracture is not of a type for which problems of this kind are frequent, generally arouses concern that there may have been a therapeutic error. Nonetheless, the burden of proof that such an error has been committed is still upon the claimant, unless there are other considerations that affect the required standard of evidence.
"The treatment of fractures in growing children is not a task that can be reserved for highly specialized centers; it must be universally available at a high level of medical competence. The structure of care varies from one place to another, and thus multiple specialties are involved: general, pediatric, and trauma surgery as well as orthopedic surgery, pediatrics, and general medicine … " (24).
Table 2 shows that this statement is correct. If injuries in children are to be treated by physicians from a wide range of specialties, then all treating physicians must possess the requisite knowledge of how to deal with these injuries. The initially consulted physician must make a critical and realistic assessment of his or her own clinical competence when confronted with the decision whether to treat the child’s injury personally, or else to refer the child to a more experienced physician or clinical center.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Neu J. Juristischer Leitfaden für ärztliche Gutachter. Arbeitspapier der norddeutschen Schlichtungsstelle. 2007 [Google Scholar]
- 2.Neu J, Scheppokat KD, Vinz H. Behandlungsrisiko und iatrogener Schaden. „Unfallberichte“ aus der norddeutschen Schlichtungsstelle. Z Ärztl Fortbild Qual Gesundh Wesen. 2004;98:567–574. [PubMed] [Google Scholar]
- 3.Scheppokat KD. Lehren aus den Erfahrungen einer Schlichtungsstelle für Arzthaftpflichtfragen. Therap Umschau. 2005;62:185–190. doi: 10.1024/0040-5930.62.3.185. [DOI] [PubMed] [Google Scholar]
- 4.Scheppokat KD, Neu J. Zur ärztlichen Begutachtung in Arzthaftpflichtfragen. VersR. 2001;52:2–7. [Google Scholar]
- 5.Scheppokat KD, Neu J. Medical Data and Quality Management. Dtsch Arztebl. 2007;104(46):2691–2696. [Google Scholar]
- 6.v Laer L, Kraus R, Linhart WE. Frakturen und Luxationen im Kindesalter. Stuttgart, New York: Thieme Verlag; 2007. [Google Scholar]
- 7.Marzi J, editor. Kindertraumatologie. Darmstadt: Steinkopf-Verlag; 2006. [Google Scholar]
- 8.Rockwood ChA, Wilkins KE, Beaty JH. Fractures in children. Philadelphia, New York: Lippincott-Raven; 1996. [Google Scholar]
- 9.Weinberg AM, Tscherne H. Unfallchirurgie im Kindesalter. Berlin, Heidelberg, New York: Springer Verlag; 2006. [Google Scholar]
- 10.Machan FG, Vinz H. Die Oberarmschaftfraktur im Kindesalter. Unfallchirurgie. 1993;19:166–174. doi: 10.1007/BF02588040. [DOI] [PubMed] [Google Scholar]
- 11.Neu J. MERS: Fehlerprophylaxe mittels Medical Error Reporting System. www.schlichtungsstelle.de.
- 12.Schaffartzik W, Neu J. Definition des ärztlichen Behandlungsfehlers. Trauma BerufsKH. 2008;10(Suppl. 2):196–199. [Google Scholar]
- 13.Madea B, Dettmeyer R, editors. Medizinschadensfälle und Patientensicherheit. Köln: Deutscher Ärzteverlag; 2007. [Google Scholar]
- 14.Vinz H. Nicht erkannte und daher nicht rechtzeitig behandelte isolierte Radiusköpfchenluxation bei einem Kind. Niedersächs Ärztebl. 2000;2:34–35. [Google Scholar]
- 15.Vinz H. Kompartmentsyndrom mit Ausgang in eine Volkmannsche Kontraktur nach supracondylärer Oberarmfraktur. Niedersächs Ärztebl. 2002;10:70–71. [Google Scholar]
- 16.Vinz H. Fehlerhafte Osteosynthese und unterlassene Kontrolle einer supracondylären Humerusfraktur. Niedersächs Ärztebl. 2003;6:25–26. [Google Scholar]
- 17.Vinz H. Fehlerhafte Diagnose und Behandlung einer epiphysären Fraktur im Bereich des oberen Sprunggelenkes bei einem Kind. Niedersächs Ärztebl. 2006;3:25–26. [Google Scholar]
- 18.Gwynne A, Barber P, Tavener F. A review of 105 negligent claims against accident and emergency departments. J Accid Emerg Med. 1997;14:243–245. doi: 10.1136/emj.14.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips RL, Bartholomev LA, Dovey SM, et al. Learning from malpractice claims about negligent adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121–126. doi: 10.1136/qshc.2003.008029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selbst StM, Friedman MJ, Singh SB. Epidemiology and etiology of malpractice lawsuits involving children in US Emergency Departments and Urgent Care Centers. Pediat Emerg Care. 2005;21:165–169. [PubMed] [Google Scholar]
- 21.Skaggs D, Pershad J. Pediatr elbow trauma. Pediatr Emerg Care. 1997;13:425–434. doi: 10.1097/00006565-199712000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Studdert DM, Thomas EJ, Burstin HR, et al. Negligent care and malpractice claiming behavior in Utah and Colorado. Medical Care. 2000;38:250–260. doi: 10.1097/00005650-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Vinz H, Neu J. Arzthaftpflichtverfahren im Zusammenhang mit der Diagnose und der Therapie der akuten Appendizitis. Z Ärztl Fortbild Qual Gesundh Wesen. 2007;101:553–563. doi: 10.1016/j.zgesun.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 24.Kraus R, Schneidmüller D, Röder C. Häufigkeit von Frakturen der langen Röhrenknochen im Wachstumsalter. Dtsch Arztebl. 2005;102(12):838–842. [Google Scholar]