Abstract
Background
It has been stated by hand surgeons that rheumatoid arthritis (RA) patients often are referred “too little and too late.” The purpose of this prospective study was to evaluate outcomes of RA patients with metacarpophalangeal (MCP) joint deformities (subluxation and ulnar deviation). We hypothesized that patients with more severe deformities would have worse outcomes after silicone MCP joint arthroplasty (SMPA).
Methods
70 patients who each had combined MCP joint ulnar drift and extensor lag greater than 50 degrees were recruited into this three-center study of SMPA. The patients were categorized into two groups based on degrees of deformity: <100° or ≥100°. Outcomes were assessed at 6 months and one year based on the Michigan Hand Outcomes Questionnaire (MHQ), grip/pinch strength, MCP joint deviation angles, Jebsen-Taylor test, and Arthritis Impact Measurement Scales questionnaire (AIMS2).
Results
There was no difference in outcomes at the one year follow-up between the two groups, after controlling for age, gender and baseline values. Each of the outcome scores was not different between the two groups, including the six domains in the MHQ, grip/pinch strength, Jebsen-Taylor test, and the AIMS2. But patients with more severe hand deformities have worse ulnar drift and extensor lag after reconstruction.
Conclusions
RA patients with more severe MCP joint diseases will attain similarly good outcomes after reconstruction when compared to those with less severe deformities. Despite the potential barriers to SMPA in RA patients with more severe hand deformities, surgical treatment is still beneficial.
Keywords: Outcomes, Michigan Hand Outcomes Questionnaire, silicone arthroplasty, rheumatoid arthritis, hand deformities, prospective study
Surgeons often complain that rheumatoid arthritis (RA) patients frequently present for consideration of reconstruction “too little and too late.” (1, 2) Patients who present late often have more severe hand deformities. More severe extensor lag and ulnar drift of the fingers in RA were postulated to lead to worse outcomes after reconstruction.(3, 4) The use of silicone metacarpophalangeal joint arthroplasty (SMPA) has remained the main treatment for RA patients with metacarpophalangeal (MCP) joint disease, and surgeons often feel that patients with less severe deformity are more optimal for surgical reconstruction, whereas rheumatologists frequently wait until the deformities are much more advanced before referring their patients to surgeons for consideration of reconstruction.(5, 6) In general, rheumatologists view the outcomes of surgical reconstruction of the rheumatoid hand as less than satisfactory, and they therefore tend to refer patients later, after medical treatment is no longer effective. We have shown in prior studies that there is great disagreement between hand surgeons and rheumatologists regarding the indications, timing, and perceived outcomes for a variety of hand reconstructive surgical procedures for the rheumatoid hand, not just for SMPA alone.(5, 6) These interdisciplinary differences in guiding the surgical treatment for common RA hand deformities may be based on personal opinions and training philosophies rather than evidence, and may lead to fewer and later referrals to hand surgeons for consideration of reconstruction.
A prospective study has demonstrated that SMPA was associated with excellent one-year outcomes, but this study did not have a control group.(7) Although SMPA is one of the most commonly performed procedures in RA hand surgery, the rate of such hand procedures is decreasing because of improved medications. Nevertheless, many patients will still develop the ulnar drift posture that limits their hand function. The principles of evidence-based medicine require that opinions must be supported by data, and the data must be generated through a high-level evidence study design in order to guide important decisions affecting patient care.
In this National Institutes of Health (NIH) -funded multi-center, international outcomes study on SMPA, we sought to evaluate critically whether patients who present with more severe deformities have worse outcomes after reconstruction. The main aim of this project is to follow a large prospective cohort of patients with pre-determined severe ulnar drift and extensor lag deformities who have enrolled into either the surgical arm or the medically-treated non-surgical arm to serve as controls. Thus far we have enrolled over 160 patients from three centers. This is the largest series in the world thus far to critically evaluate the outcomes of SMPA. A specific aim of this project is to determine whether patients with more severe ulnar drift and extensor lag will have worse outcomes after SMPA when compared to patients who have less severe deformities. The implication of this study question is to determine whether there is evidence to show that earlier reconstruction for the RA hand can yield better outcomes or whether patients with late stage disease at the MCP joint would have inferior results due to later reconstruction. We hypothesized that patients with worse deformities would have inferior outcomes when compared to patients with less severe deformities.
Methods
Patient Recruitment and Eligibility
Patients were recruited as part of the NIH-funded study to evaluate outcomes of SMPA. All aspects of the study were approved by the University of Michigan Institutional Review Board and the Institutional Review Boards at the Curtis National Hand Center and the Pulvertaft Hand Center. Written informed consents were obtained from all study patients. All study patients were informed of both the surgical and non-surgical treatment options, and they were considered by their rheumatologists and surgeons to be eligible for surgical treatment. Patients chose whether they wanted to participate in the surgical or non-surgical group. For the purpose of the specific aim of this paper, only the surgical patients are analyzed.
Potential study subjects were identified by the referring rheumatologists as having both ≥25° of MCP joint ulnar deviation and MCP joint extensor lag. These patients were then referred to one of the 3 study sites to determine eligibility using standard goniometry measurements taken by certified hand therapists. Patients were enrolled into the study if they had 50° or more mean combined MCP joint ulnar deviation and extensor lag after averaging the combined angles of the index, middle, ring, and small fingers. This entry criterion was selected, based on a consensus panel of surgery and rheumatology experts on RA hand surgery, to be the minimum deformity before SMPA may be considered. For patients with symmetrical deformities, in whom both hands were deemed eligible for the study, the patients chose the “study” hand that was evaluated over time.
Inclusion criteria also included a diagnosis of RA, age of 18 to 80 years, and the ability to complete questionnaires in English. Patients included in the study had SMPA on 4 fingers (index, middle, ring, and little). Patients were excluded if they had a severe medical condition that would preclude surgery, concomitant extensor tendon ruptures (which confound the outcomes because of a different therapy protocol), swan-neck or boutonniere deformities that required surgical correction (which affect the outcomes evaluation because of the additional finger operations), a previous MCP joint replacement on the study hand, or if they began taking disease-modifying antirheumatic drugs in the 3 months before enrollment (to avoid potential surgical complications from acute immunosuppression). We chose to exclude patients with concomitant extensor tendon ruptures because the surgical management would require a staged approach, first with joint replacements followed by extensor tendon reconstruction. The staged reconstruction is markedly different from the surgical protocol for SMPA without tendon reconstruction and may confound the outcomes assessment for this procedure.
All study patients were evaluated at study entry (baseline) and at 6-month, 1-year, 2-year, and 3-year follow-up intervals. Evaluations included completion of study questionnaires and physical measurements as described below. Because study patients are continuing their follow-up evaluations, the sample sizes at the 2-year and 3-year points are small. Therefore, the primary focus for this analysis is through the 1-year follow-up period.
Study Questionnaires
The Michigan Hand Outcomes Questionnaire (MHQ)(8, 9) is included as the main outcomes tool. The MHQ is a hand-specific outcomes questionnaire that contains 6 domains: (1) overall hand function, (2) activities of daily living, (3) pain, (4) work performance, (5) aesthetics, and (6) patient satisfaction. The MHQ was found to be highly responsive for evaluating hand function in RA patients.(7)
Patients also were asked to complete the Arthritis Impact Measurement Scales (AIMS2) questionnaire,(10) a health status questionnaire specifically designed to measure general health status in arthritis patients. It contains 12 scales that are categorized into 4 domains: physical, affect, symptom, and social interaction.
Physical Measurements
Patients underwent hand function assessments by a certified hand therapist at each study site who was specifically assigned to this project. The assessments consisted of measuring grip strength, 2-point, 3-point, and key pinch strengths, finger range of motion, ulnar deviation, and the Jebsen-Taylor test. The Jebsen-Taylor test was designed to simulate activities of daily living.(7, 9)
Statistical Analysis
Patients were categorized into two groups based on degree of deformity at baseline: <100° (less severe) or ≥100° (more severe). The degree of deformity was calculated as a sum of ulnar drift and extensor lag angle, ranged from 49° to 173°, and had a mean of 102° and a median of 103° at baseline. The cut-off point of 100° was determined based on the near equal distribution of subjects less or greater than this value. Demographic data were compared between the two groups using t-tests (age) or chi-square tests (male, Caucasian, income, education). Means and standard deviations were calculated for each outcome at baseline, 6-month follow-up, and 1-year follow-up. For all outcome measures, differences from the previous time period were calculated at the 6-month and 1-year follow-up period to reflect changes in outcome. We used multiple regression analyses to test for differences in outcomes at 6 month and at 12 month between patients with more severe deformities versus those with less severe deformities. For this comparison, outcomes at each follow-up month were modeled with an indicator for the more severe group as the primary predictor, while adjusting for age, gender and baseline values of the outcome variable. We also used a linear mixed-effects model (11) to assess if the outcome changes from 6 and 12 months were different between the less severe versus more severe groups, after controlling for age, gender and baseline values of the outcome variable. For grip strength calculations, we accounted for a 10% strength increase in the dominant hand if the right hand was dominant, but did not compensate if the left hand was dominant.(12)
Results
Table 1 presents the demographic data for these two groups. A total of 70 patients were included in the study, 33 in the less severe group and 37 in the more severe group. Both groups are comparable in the baseline demographic information.
Table 1.
Patient Demographics
| Less Severe <100° (N = 33) |
More Severe ≥100° (N = 37) |
p-value | |
|---|---|---|---|
| Mean age (range) | 60.1 (22–80) | 60.2 (47–77) | 0.47 |
| Male (%) | 6 (18) | 7 (19) | 0.93 |
| Caucasian (%) | 28 (85) | 31 (84) | 0.38 |
| Income level (%) | |||
| <$20,000 | 10 (30) | 11 (30) | 0.89* |
| $20,000–$50,000 | 12 (37) | 16 (43) | |
| >$50,000 | 7 (21) | 7 (19) | |
| Not reported | 4 (12) | 3 (8) | |
| Education level (%) | |||
| High school graduate or less | 17 (52) | 19 (51) | 0.43* |
| Vocational training/ some college/associate degree |
10 (30) | 8 (22) | |
| College graduate and above | 3 (9) | 7 (19) | |
| Not reported | 3 (9) | 3 (8) |
Compared without including “not reported” category
As shown in Table 2, although both groups reported similar self-assessed function scores at baseline as indicated by the overall scores on the MHQ, patients in the more severe group had two-times the ulnar drift angle, almost two-times the extensor lag angle, and less than half the arc of motion. In other words, the more severe group presented with twice as much MCP joint deformity than the less severe group. There was no significant difference between the two groups in terms of grip strength or Jebsen-Taylor test.
Table 2.
Baseline Outcomes Scores Comparing the Two Cohorts
| Cohort | Less Severe <100° |
More Severe ≥100° |
p-value |
|---|---|---|---|
| Overall MHQ Score† | 38 ± 15 | 37 ± 20 | 0.98 |
| Grip Strength (kg) | 6.3 ± 6 | 5.2 ± 5 | 0.42 |
| Jebsen-Taylor Test (seconds) | 55 ± 26 | 57 ± 27 | 0.75 |
| Ulnar Drift (degree) | 28 ± 12 | 45 ± 15 | <.001 |
| Extensor Lag (degree) | 46 ± 16 | 82 ± 13 | <.001 |
| Arc of Motion (degree) | 29 ± 15 | 11 ± 8 | <.001 |
Michigan Hand Outcomes Questionnaire overall scores range from 0 to 100; the higher the score, the better the subject’s hand performance.
Values are expressed as the mean ± standard deviation
Both groups, despite large differences in their physical hand deformities, reported similar functional problems before surgery (Tables 3). After SMPA, both groups had excellent self-reported hand outcomes at the 1-year follow-up period, marked by large improvement in the various dimensions of the MHQ scores. At each 6 and 12 month follow-up period, all MHQ domains except work domain showed statistically significant improvement from baseline in both groups. More importantly, at 12 months after surgery, no differences in the MHQ domain scores were shown between patients with more versus less severe deformities after controlling for age, gender and baseline values of the outcome variables. In fact, although only marginally significant, patients with more severe deformity showed better outcomes than those with less severe deformity for the MHQ overall score (p = 0.08) and for the domains of function (p = 0.10) and activities of daily living (p = 0.07). Lastly, for all MHQ domains, the patterns of outcome changes were similar between the more versus less severe groups.
Table 3.
Rate of Recovery Using Patient-Rated Michigan Hand Outcomes Questionnaire
| Michigan Hand Outcomes Domain† |
Severity | Baseline | 6 Months | 1 Year | ||
|---|---|---|---|---|---|---|
| Raw Score |
Raw Score* |
Difference from Baseline |
Raw Score* |
Difference from 6 Months |
||
|
Overall Score |
<100° | 38 ± 15 | 62 ± 20 | 25 ± 17 | 56 ± 24 | −3 ± 11 |
| ≥100° | 37 ± 20 | 61 ± 21 | 23 ± 14 | 62 ± 20 | 2 ± 14 | |
| Function | <100° | 37 ± 20 | 66 ± 20 | 31 ± 19 | 56 ± 24 | −8 ± 14 |
| ≥100° | 36 ± 24 | 62 ± 20 | 25 ± 20 | 65 ± 24 | 5 ± 16 | |
| ADL | <100° | 38 ± 24 | 57 ± 29 | 19 ± 19 | 54 ± 32 | −1 ± 10 |
| ≥100° | 30 ± 27 | 53 ± 29 | 20 ± 23 | 56 ± 30 | 5 ± 15 | |
| Work | <100° | 40 ± 20 | 50 ± 28 | 10 ± 20 | 44 ± 31 | −1 ± 20 |
| ≥100° | 41 ± 25 | 50 ± 29 | 7 ± 22 | 50 ± 26 | −1 ± 19 | |
| Pain | <100° | 50 ± 26 | 33 ± 25 | 16 ± 29 | 37 ± 26 | 1 ± 16 |
| ≥100° | 49 ± 25 | 38 ± 24 | 12 ± 18 | 32 ± 22 | 8 ± 15 | |
| Aesthetic | <100° | 35 ± 19 | 70 ± 23 | 35 ± 31 | 65 ± 25 | −1 ± 20 |
| ≥100° | 29 ± 24 | 73 ± 22 | 41 ± 28 | 66 ± 26 | −7 ± 24 | |
| Satisfaction | <100° | 26 ± 18 | 64 ± 22 | 38 ± 22 | 57 ± 27 | −5 ± 18 |
| ≥100° | 27 ± 22 | 63 ± 27 | 35 ± 23 | 66 ± 26 | 4 ± 24 | |
Values are expressed as the mean ± standard deviation; ADL is activities of daily living.
All scores can range from 0 to 100; the higher the score, the better the subject’s hand outcome, except pain domain for which higher score represents worse outcome.
At both 6 month and 12 month, no MHQ domains showed significant difference between less versus more severe groups, adjusting for age, gender and baseline values of the outcome variables.
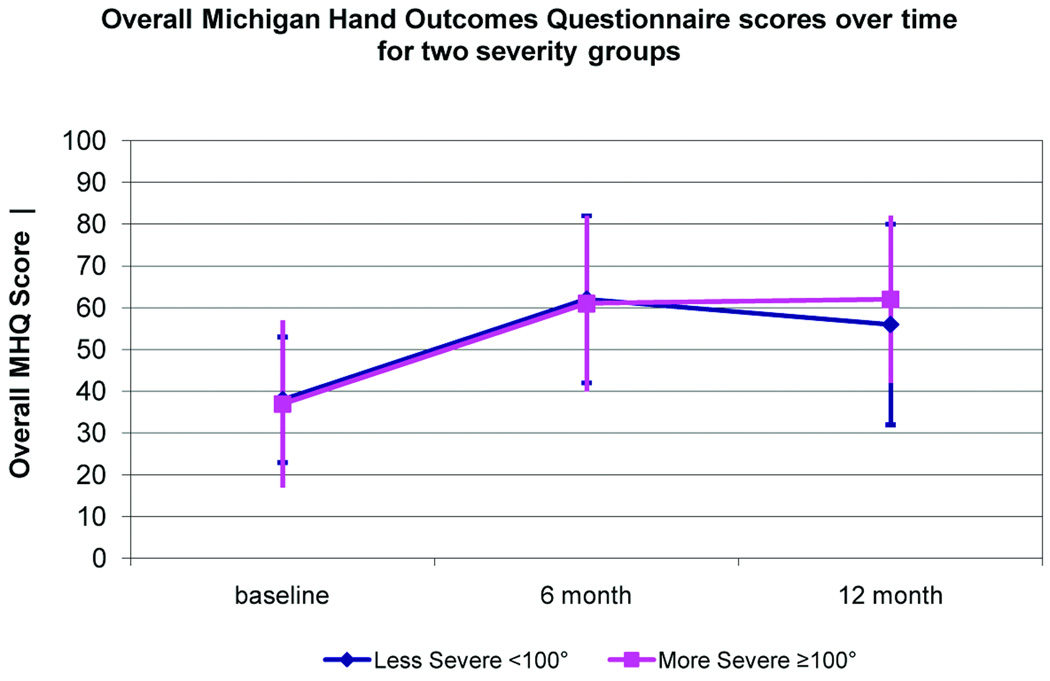
Figure 1 demonstrates that both groups had a similar pattern in outcome changes in the MHQ overall score at baseline, 6 month, and 1 year follow-up periods. SMPA patients showed significant improvement in the AIMS2 physical score, but did not significantly improve in the other dimensions of health-related quality-of-life domains based on the AIMS 2 scores (Table 4). Similar to the hand outcomes, at 12 months after surgery, no differences in the AIMS2 domain scores were seen between patients with more versus less severe deformities after controlling for age, gender and baseline values of the outcome variable.
Figure 1.
Graphical representation of the MHQ scores over the 3 time periods for the 2 cohorts.
Table 4.
Rate of Recovery Using Patient-Rated Arthritis Impact Measurement Scales
| Arthritis Impact Measurement Domain^ |
Severity | Baseline | 6 Months | 1 Year | ||
|---|---|---|---|---|---|---|
| Raw Score |
Raw Score* |
Difference from Baseline |
Raw Score* |
Difference from 6 Months |
||
| Physical | <100° | 3 ± 2 | 3 ± 2 | 1 ± 1 | 3 ± 2 | 0 ± 1 |
| ≥100° | 5 ± 3 | 4 ± 3 | 1 ± 1 | 4 ± 3 | 0 ± 1 | |
| Affect | <100° | 4 ± 2 | 4 ± 2 | 0 ± 1 | 4 ± 2 | 0 ± 1 |
| ≥100° | 4 ± 2 | 4 ± 2 | 0 ± 1 | 4 ± 2 | 0 ± 1 | |
| Symptom | <100° | 6 ± 3 | 5 ± 3 | 1 ± 2 | 5 ± 3 | 0 ± 2 |
| ≥100° | 6 ± 3 | 5 ± 3 | 0 ± 2 | 5 ± 2 | 1 ± 2 | |
|
Social Interaction |
<100° | 4 ± 2 | 4 ± 2 | 0 ± 1 | 4 ± 2 | 0 ± 1 |
| ≥100° | 4 ± 2 | 4 ± 2 | 0 ± 1 | 4 ± 2 | 0 ± 1 | |
Arthritis Impact Measurement Scales (AIMS2) scores can range from 0 to 10; the higher the score, the worse the subject’s health status.
At both 6 month and 12 month, no AIMS2 domains showed significant difference between less versus more severe groups, adjusting for age, gender and baseline values of the outcome variables.
There was no difference between the two groups in terms of grip and pinch strengths (Table 5). The improvements in grip and pinch strength at one year after SMPA were minimal, which corroborated the data from previous studies.(13–15) At one year, the Jebsen-Taylor results improved from baseline in both less severe (p = 0.06) and more severe (p = 0.004) groups, but no difference was found between the less and more severe groups (p = 0.24) after adjusting for age, gender and baseline values. After surgery, the more severe group still had more severe deformities in terms of ulnar drift and extensor lag when compared to the less severe group; however only ulnar drift was significantly different between the two groups (p = 0.008) at 12 month after controlling for age and gender. This difference, although statistically significant, may not be clinically significant. This finding is interesting because it shows that when patients present with worse deformities, it is much more difficult to correct them. At one year after surgery, there was no difference in arc of motion between the two groups (p = 0.79). Our hypothesis that RA patients with more severe hand deformities would have inferior outcomes when compared to patients with less severe deformities was rejected in this analysis. The more severe hand deformity group attained similar functional outcomes when compared to the less severe group, although the more severe hand deformity group still had significantly more deformity after reconstruction than the less severe group.
Table 5.
Rate of Recovery Using Objective Measurements
| Measurement | Severity | Baseline | 6 Months | 1 Year | ||
|---|---|---|---|---|---|---|
| Raw Score |
Raw Score* |
Difference from Baseline |
Raw Score* |
Difference from 6 Months |
||
|
Jebsen-Taylor Test (seconds) |
<100° | 55 ± 26 | 49 ± 21 | 3 ± 16 | 46 ± 17 | 3 ± 10 |
| ≥100° | 57 ± 27 | 47 ± 17 | 7 ± 13 | 42 ± 15 | 2 ± 6 | |
|
Grip Strength (kg) ^^ |
<100° | 6.3 ± 6 | 5.0 ± 4 | −1 ± 7 | 6.1 ± 5 | 1 ± 2 |
| ≥100° | 5.2 ± 5 | 4.2 ± 3 | −1 ± 4 | 6.3 ± 4 | 2 ± 3 | |
|
Two-Point Pinch Strength (kg) |
<100° | 2.5 ± 2 | 2.3 ± 1 | 0 ± 1 | 2.5 ± 2 | 0 ± 1 |
| ≥100° | 2.4 ± 2 | 2.3 ± 1 | 0 ± 1 | 2.8 ± 2 | 1 ± 1 | |
|
Three-Point Pinch Strength (kg) |
<100° | 2.6 ± 2 | 2.5 ± 1 | 0 ± 1 | 2.4 ± 2 | 0 ± 1 |
| ≥100° | 2.5 ± 1 | 2.4 ± 1 | 0 ± 1 | 2.7 ± 1 | 0 ± 1 | |
|
Key-Pinch Strength (kg) |
<100° | 3.4 ± 2 | 3.1 ± 2 | 0 ± 1 | 3.1 ± 2 | 0 ± 1 |
| ≥100° | 3.6 ± 2 | 3.0 ± 1 | 0 ± 2 | 3.0 ± 1 | 0 ± 1 | |
|
Ulnar Drift (degrees) |
<100° | 28 ± 12 | 10 ± 7 | 18 ± 11 | 9 ± 6 | 2 ± 7 |
| ≥100° | 45 ± 15 | 16 ± 14 | 27 ± 17 | 18 ± 14 | −1 ± 5 | |
|
Extensor Lag (degrees) |
<100° | 46 ± 16 | 24 ± 14 | 19 ± 16 | 26 ± 9 | 1 ± 7 |
| ≥100° | 82 ± 13 | 29 ± 15 | 52 ± 22 | 31 ± 18 | −9 ± 8 | |
|
Arc of Motion (degrees) |
<100° | 29 ± 15 | 33 ± 19 | 2 ± 18 | 30 ± 15 | 1 ± 11 |
| ≥100° | 11 ± 8 | 32 ± 16 | 22 ± 22 | 32 ± 16 | 1 ± 10 | |
Grip strength accounts for hand dominance
At both 6 month and 12 month, none of Jebsen-Taylor test, grip strength, 2-point pinch strength, 3-point pinch strength and key pinch strength showed significant difference between less versus more severe groups, adjusting for age, gender and baseline values of the outcome variables.
Discussion
Hand problems and deformities are frequent complaints for patients with RA. In the past, a lack of effective medications for a majority of patients with this debilitating disease resulted in persistently exuberant synovitis in the wrist and hand joints, which caused stretching of the supporting ligaments, typical wrist destructive patterns, and ulnar deviation and extensor lag of the fingers. In recent years, the introduction of newer medications has markedly decreased the severity of synovitis in RA and curbed the rapid development of RA hand deformities. Despite these advances, some patients may not be responsive to either conventional disease modifying drugs or the new biologic medications. These patients will develop eventual RA hand deformities. There is also a subset of patients who already have established hand deformities that will not be corrected by medication alone and are candidates for surgical treatment.
The management of rheumatoid hand and wrist problems is challenging because of significant disagreement between hand surgeons and rheumatologists regarding the appropriate treatment strategy for these problems. Surgeons are, in general, much more optimistic regarding the outcomes of surgical reconstruction. In contrast, rheumatologists tend to have a pessimistic view regarding hand and wrist reconstruction because they have a long-term relationship with the patients and have an opportunity to see recurrence of the deformities following reconstruction after a longer follow-up time. Unfortunately, rigorous outcomes studies are lacking in the field of RA hand surgery to provide high level evidence to guide physicians in the most optimal management of RA patients.
In an effort to derive an evidence-based approach in treating rheumatoid hand conditions, we initiated this NIH funded multi-center clinical trial to study the SMPA procedure. One of the most common and debilitating conditions in RA is MCP joint disease resulting in ulnar deviation and extensor lag of the fingers. Although some patients may adapt to the hand deformities, many have difficulties extending the fingers to get around objects. The inability to touch the fingers to the thumb makes fine pinch almost impossible. Despite over 40 years of using silicone arthroplasty for the MCP joint, a prospective outcome study with a control group for SMPA has never been performed. This study was designed through the collaboration between hand surgeons and rheumatologists in jointly evaluating and enrolling patients in order to define many important specific aims relating to the treatment of the rheumatoid hand. Although a randomized study design was considered, our pilot studies and focus group discussions with surgeons and patients indicated reluctance for all involved in randomizing patients to surgery versus no surgery. Patients requested autonomy in choosing this highly intensive procedure, and surgeons and rheumatologists were also uncomfortable with a randomized design because of their specific biases regarding the effectiveness of SMPA for the rheumatoid hand. Therefore, a level 2 evidence prospective cohort study was conceived to organize this unique cohort. This is the largest cohort study of RA patients with severe MCP joint disease to define the short- and long-term outcomes of this procedure.
This report provides evidence that challenges the commonly held view amongst surgeons that SMPA produces much better outcomes if the deformities are less severe. In our national survey, rheumatologists generally feel that patients should be referred for surgery much later when the deformity is more severe, whereas hand surgeons prefer to operate on the patients earlier.(6) This present study has shown that both the less and more severe groups derived great benefit after the SMPA procedure, which is demonstrated by the large effect sizes in the MHQ scores for all dimensions of hand outcomes. However, this study has also shown that it is much easier to correct the deformities and restore the patients’ hand posture if they are operated on earlier when the deformities are less severe. The more severe group still has statistically and clinically more significant deformities after reconstruction. The contracted structures contributing to ulnar drift are difficult to correct surgically, and it is quite possible that over the long term, patients with more severe deformities at baseline may develop more rapid recurrence of the deformities after reconstruction than the less severe group. It is conceivable that with the three-year follow-up time that is planned in this study, patients with less severe deformity may maintain their hand posture better than those with more severe deformity.
Evidence-based research is a key component of current health care initiatives to improve the quality of care based on data rather than intuition.(16–20) Rheumatologists demand outcomes data to support their decisions to refer their patients for reconstructive surgery. Surgeons similarly want high-level outcomes studies to guide treatments. The recommendation from this study is that even RA patients with severe deformities should still be referred by rheumatologists to hand surgeons for consideration of reconstruction. The pessimistic view regarding hand surgery is not borne out by this study because despite severe MCP joint disease, patients reported great satisfaction and functional gains. This study also supports the general view of surgeons that earlier surgery is beneficial before structural deterioration makes it more difficult to realign the fingers and restore functional anatomy.
The involvement of three geographically-separated centers in this study supports the concept that the results should be applicable to RA patients in general, provided they are cared for in facilities with specialized expertise. We hope this study will generate greater interest between surgery and rheumatology specialties in jointly evaluating outcomes of hand surgery procedures. Collaborative studies that involve both hand surgeons and rheumatologists may finally eliminate the unfortunate phrase of “too little, too late” from our vocabulary as we strive to enhance the quality-of-life for the RA population.
Acknowledgements
The authors acknowledge the assistance of the following participants of the SMPA Study Group: Sandra V. Kotsis, MPH, Patricia B. Burns, MPH, Melissa J. Shauver, MPH, Heidi Reichert, MA (University of Michigan), Lorraine A. Zellers, CRC (Curtis National Hand Center), Mary J. Bradley, MSc (Pulvertaft Hand Centre) and the referring rheumatologists in Michigan, Derby and Baltimore. The authors also greatly appreciate the assistance of Jeanne M. Riggs, OTR, CHT, Kurt Hiser, OTR, Carole Dodge, OTR, CHT, Jennifer Stowers, OTR, CHT, Cheryl Showerman, OTR, Jo Holmes, OTR, Victoria Jansen, PT and Helen Dear, OTR in taking measurements for the study patients. The PI appreciates the kind assistance of the Observational Study Safety Monitoring Board convened by Dr James S. Panagis, Medical Officer, NIAMS. The members of the Board are Andrew N. Pollak, M.D., University of Maryland, Chair; Philip E. Blazar, M.D., Brigham and Women's Hospital; Richard J. Looney, M.D, University of Rochester; William F. Rosenberger, Ph.D., George Mason University; Nicholas B. Vedder, M.D, University of Washington.
Supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR047328) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
Footnotes
Financial disclosure statement: The authors have no other financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Wynn Parry CB, Stanley JK. Synovectomy of the hand. Br J Rheumatol. 1993;32:1089–1095. doi: 10.1093/rheumatology/32.12.1089. [DOI] [PubMed] [Google Scholar]
- 2.Mannerfelt L. On surgery of the rheumatoid hand: consensus and controversy. J Hand Surg [Br] 1989;14:259–260. doi: 10.1016/0266-7681_89_90078-8. [DOI] [PubMed] [Google Scholar]
- 3.Nalebuff EA. Rheumatoid hand surgery - update. J Hand Surg. 1983;8A:678–682. doi: 10.1016/s0363-5023(83)80244-5. [DOI] [PubMed] [Google Scholar]
- 4.Chung KC, Kowalski CP, Kim HM, et al. Patient outcomes following Swanson silastic metacarpophalangeal joint arthroplasty in the rheumatoid hand: a systematic overview. J Rheumatol. 2000;27:1395–1402. [PubMed] [Google Scholar]
- 5.Alderman AK, Chung KC, Kim HM, et al. Effectiveness of rheumatoid hand surgery: contrasting perceptions of hand surgeons and rheumatologists. J Hand Surg. 2003;28A:3–11. doi: 10.1053/jhsu.2003.50034. [DOI] [PubMed] [Google Scholar]
- 6.Alderman AK, Ubel PA, Kim HM, et al. Surgical management of the rheumatoid hand: consensus and controversy among rheumatologists and hand surgeons. J Rheumatol. 2003;30:1464–1472. [PubMed] [Google Scholar]
- 7.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg. 2004;29A:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung KC, Pillsbury MS, Walters MR, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998;23A:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 9.Chung KC, Hamill JB, Walters MR, et al. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Meenan RF, Mason JH, Anderson JJ, et al. AIMS2: the content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis Rheum. 1992;35:1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- 11.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 12.Petersen P, Petrick M, Connor H, et al. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43:444–447. doi: 10.5014/ajot.43.7.444. [DOI] [PubMed] [Google Scholar]
- 13.Burgess SD, Kono M, Stern PJ. Results of revision metacarpophalangeal joint surgery in rheumatoid patients following previous silicone arthroplasty. J Hand Surg [Am] 2007;32:1506–1512. doi: 10.1016/j.jhsa.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 14.Synnott K, Mullett H, Faull H, et al. Outcome measures following metacarpophalangeal joint replacement. J Hand Surg [Br] 2000;25:601–603. doi: 10.1054/jhsb.2000.0402. [DOI] [PubMed] [Google Scholar]
- 15.Moller K, Sollerman C, Geijer M, et al. Osseointegrated silicone implants. 18 patients with 57 MCP joints followed for 2 years. Acta Orthop Scand. 1999;70:109–115. doi: 10.3109/17453679909011245. [DOI] [PubMed] [Google Scholar]
- 16.Chung KC, Ram AN. Evidence-based medicine, the fourth revolution in American medicine? Plast Reconstr Surg. doi: 10.1097/PRS.0b013e3181934742. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung KC, Burns PB, Davis Sears E. Outcomes research in hand surgery: where have we been and where should we go? J Hand Surg. 2006;31A:1373–1379. doi: 10.1016/j.jhsa.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 18.Devereaux PJ, Yusuf S. The evolution of the randomized controlled trial and its role in evidence-based decision making. J Intern Med. 2003;254:105–113. doi: 10.1046/j.1365-2796.2003.01201.x. [DOI] [PubMed] [Google Scholar]
- 19.Berwick DM, James B, Coye MJ. Connections between quality measurement and improvement. Med Care. 2003;41:I30–I38. doi: 10.1097/00005650-200301001-00004. [DOI] [PubMed] [Google Scholar]
- 20.Alderman AK, Chung KC. Measuring outcomes in hand surgery. Clin Plast Surg. 2008;35:239–250. doi: 10.1016/j.cps.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]