Abstract
Objective
Characterize the incidence and possible etiologies of acid reflux events detected by pH and not identified by intraluminal impedance (MII) monitoring.
Methods
Acid reflux events detected by pH but not identified by MII (pH-only) were documented in 80 preterm and 39 term infants. Reason for failure of MII to detect these events were classified as failure to meet MII scoring criteria, presence of an air bolus, technical artifact, and no change in impedance. Events with no change in impedance were stratified to; 1) low impedance throughout the study (possible esophageal inflammation), 2) transient decrease in pre-event impedance (presence of refluxate), 3) occurrence <30 seconds of a preceding event and 4) no explanation.
Results
2572 events were detected by pH with 59% of events not identified by MII. A higher incidence of pH-only events occurred in preterm versus term infants (54±27% vs 42±23%, p=.025, respectively). Thirteen percent of pH-only events were missed due to MII scoring criteria, 12% due to technical artifact, 11% due to an air bolus and 64% had no change in impedance. Of the 978 events with no change in impedance 154 were associated with low impedance throughout the study, 430 with a transient decrease in pre-event impedance, and 175 were preceded by a reflux episode within 30sec.
Conclusion
There was a high incidence of acid reflux events detected by pH but not identified by MII. This occurred more often in the least mature infants and we speculate that delayed esophageal fluid clearance is the major underlying mechanism.
Keywords: Gastroesophageal reflux, intraluminal impedance, infant
Introduction
Acidic gastroesophageal reflux (GER) commonly occurs in the premature infant and placement of a pH catheter in the esophagus is the conventional diagnostic modality. Acidic events detected by this system have been traditionally defined as a drop in pH <4 for a specified duration 1. More recent technology has led to the implementation of the multiple intraluminal impedance (MII) based system for measurement of GER. In contrast to pH metry, MII technology relies on initial detection of a bolus indicated by a rapid retrograde fall from a pre-episode baseline impedance, to ≤50% of the baseline period on two or more sequential channels. The GER event is then identified as acid if it occurs in conjunction with a drop in pH <4. These separate means for detection of acid reflux have resulted in discrepancies in the number of acid reflux events reported by these two technologies.
There are currently limited infant data reporting the incidence of, or reasons for, inconsistencies in acid reflux detection1,2. Studies in symptomatic term infants have reported that 9 to 40% of pH events are missed by MII 4, 5. The inability of impedance to identify these events may be due to a variety of reasons including technical artifact, insignificant bolus size 6, catheter design, esophageal pathology (ie reflux esophagitis) and scoring rules. As MII has been shown to have the ability to detect a bolus as small as 0.1cc6, events missed due to an undetectable volume are probably a rare occurrence. Catheter designs vary by manufacturer where location of the pH sensor above two, rather than one impedance channel would increase the likelihood of an event detected by pH meeting scoring criteria by MII 7.
Esophageal pathology appears to limit the ability of MII to detect a bolus in adults with severe gastroesophageal reflux disease 8. Conductivity of the empty esophageal lumen has been reported as 2000–4000Ω in normal adults 9 with lower values of 1500–2000Ωin both symptomatic and asymptomatic infants 5, 10. Inflammation of the esophagus may result in lower impedance values 11 for the entire study due to increased conductivity of the esophageal wall. These low values of impedance may fall within the range of refluxate, limiting the ability of MII to distinguish the presence of a bolus. As infants reside in a reclining position it is also possible that a bolus may slowly accumulate in the esophagus. In contrast to low impedance levels for the entire study this would present as a transient decrease in impedance not meeting scoring criteria as a GER event. Lastly, detection of subsequent GER events by MII may be limited by incomplete clearance of a preceding event. This is consistent with data in adults with mild gastroesophageal reflux disease who exhibit a higher incidence of impaired propulsive volume clearance when compared to healthy controls 12.
As clinical reports and investigational studies of acid reflux indices may be based on pH, MII or both, a clear understanding of the reasons for possible discrepancies in the incidence of acid reflux between these two techniques is important for comparisons between infant studies and understanding of underlying pathophysiology. Therefore, the purpose of this study was to characterize the incidence of acid reflux events detected by pH and not identified by MII (pH only events), and possible etiologies for such events.
Materials and Methods
In this retrospective study, we reviewed 119 twelve-hour overnight gastroesophageal reflux monitoring studies in 80 preterm (≤37 wks) and 39 term infants referred for recurrent apnea and suspected reflux at Rainbow Babies & Children’s Hospital over a period of 2 years (2006–2007). Demographic data are presented in Table 1.
Table 1.
Demographics
| Median (range) | |
|---|---|
| Gestational age at birth (wk) | 34 (23–40) |
| Preterm | 31 (23–37) |
| Term | 40 (38–40) |
| Post conceptional age at study (wk) | 40 (34–60) |
| Preterm | 38 (34–55) |
| Term | 46 (35–60) |
| Birth weight (kg) | 1.8 (.5–4.0) |
| Preterm | 1.3 (.5–3.8) |
| Term | 3.2 (2.1–4.0) |
| Weight at study (kg) | 3.0 (1.7–7.9) |
| Preterm | 2.5 (1.7–5.5) |
| Term | 3.9 (3.0–7.9) |
Gastroesophageal monitoring was performed with an impedance system (Sleuth, Sandhill, Highlands Ranch, CO) employing a 6.4 french catheter placed in the esophagus between T7 and T9 and verified by chest xray. The impedance catheter contained 7 impedance electrodes placed 1.2cm apart corresponding to a total of 6 impedance channels. In addition, a pH electrode was located 1cm from the tip of the catheter corresponding to impedance channel 6. Acidic MII events were defined as a drop in at least 2 consecutive impedance channels to ≤50% of the baseline preceding the event by <2 sec, accompanied by a drop in pH of <4. pH-only events were defined as a drop in pH of <4 for ≥5 seconds in duration with no event detected by impedance.
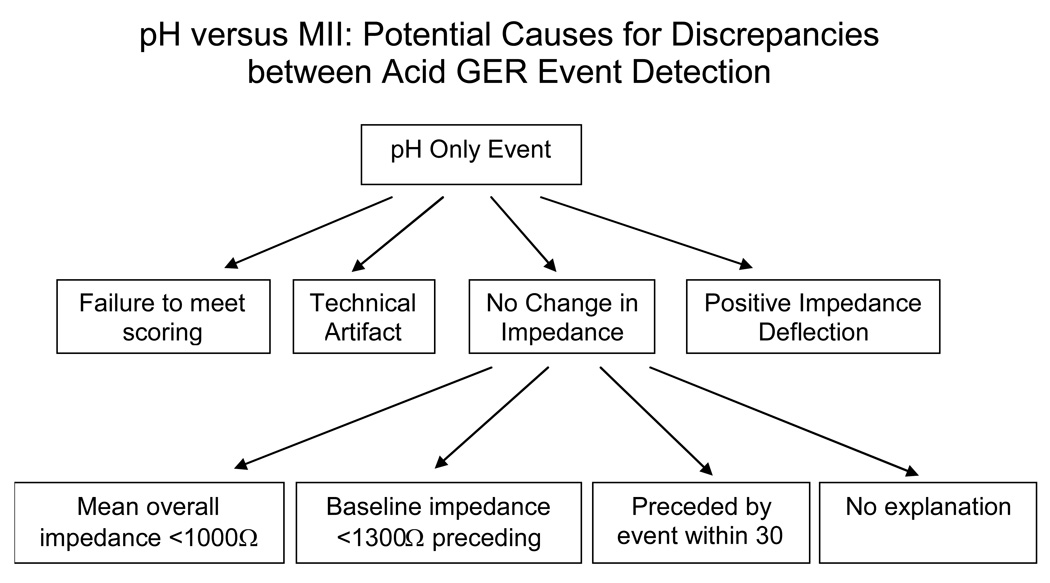
The number of events detected by pH but not meeting MII criteria was documented. Failure of impedance to detect an acid pH event was stratified as follows (Figure 1):
-
Failure to meet scoring threshold
change in impedance ≤50% of baseline on only one channel
fall in impedance on 2 or more channels but remaining >50% of the baseline
Technical artifact on the impedance channels
Positive deflection on impedance indicating an air bolus
No change in impedance on any channel
Figure 1.
Events detected by pH and not identified by MII were stratified by the possible reason for discrepancy between the two modes of gastroesophageal reflux detection.
The latter category comprising acid events detected by pH with no change in impedance on any channel was further stratified into 4 categories:
Low impedance throughout the study – Based on previous data of normal conductivity of the esophagus ranging from 1500–2000Ω in symptomatic and asymptomatic infants 5, 10. Based on one standard deviation below the mean of published data, a lower overall mean impedance value of <1000Ω during the study was chosen as a threshold to identify the possible presence of esophageal inflammation.
Transient decrease in pre-event impedance – Threshold values for transient decreases in impedance due to the presence of refluxate but not meeting MII scoring criteria as GER were based on in vitro measurements of impedance for formula (Similac Advance infant formula with iron 20 cal/oz and Pregestimil Hypoallergenic infant formula with MCT oil 24 cal/oz) and breastmilk. A catheter was placed in a vial containing either shaken formula or breast milk. Values of impedance were documented across each of the 6 impedance channels. Based on these data the number of pH only events with no change in impedance having a baseline impedance value <1300Ω was recorded.
Occurrence within 30 seconds of a preceding event-To document the possibility of incomplete clearance of a previous event when baseline impedance values preceding the event exceeded 1300Ω, the presence of a preceding reflux event occurring <30 seconds before the pH-only event, as detected by either pH or MII, was recorded.
No explanation- pH events with no change in impedance by visual inspection and not meeting any of the above criteria were marked as having no explanation.
Baseline impedance was assessed by marking an area of at least 10 seconds in duration with a stable level of impedance. Statistical analysis included an unpaired t-test to compare the incidence of pH-only events in term versus preterm infants and linear regression to assess the association between age and the incidence of pH-only events. A p value of <.05 was used for statistical significance. The retrospective study protocol and waiver of consent were approved by the IRB.
Results
Levels of impedance were obtained for formula (Similac Advance infant formula with iron 20 cal/oz and Pregestimil Hypoallergenic infant formula with MCT oil 24 cal/oz) and breast milk. Impedance values for infant formula comprised a median of 700 (561–792Ω) for Similac and 448 (389–506Ω) for Pregestimil. Breast milk had a higher median impedance of 1018 (921–1263Ω). Based on the highest impedance level measured from breast milk and formula of 1263Ω, a baseline impedance level preceding the event of <1300Ω was defined as a potential measure of the presence of refluxate in the esophagus.
There were a total of 2572 acid events detected by pH with 1057 of these events meeting impedance criteria as a GER event. The remaining 1517 (59%) acid events were detected by pH alone with a median of 7 (0–145) pH-only events per study. Seventeen studies (14%) had complete agreement between pH and MII. There was a higher mean percentage of pH-only events in preterm versus term infants (54±27% vs 42±23%, p=.025, respectively) with a significant decrease in the incidence of pH-only events with increasing gestational (r=.36, p<.0001) and post conceptional (r=.28, p<.005) age.
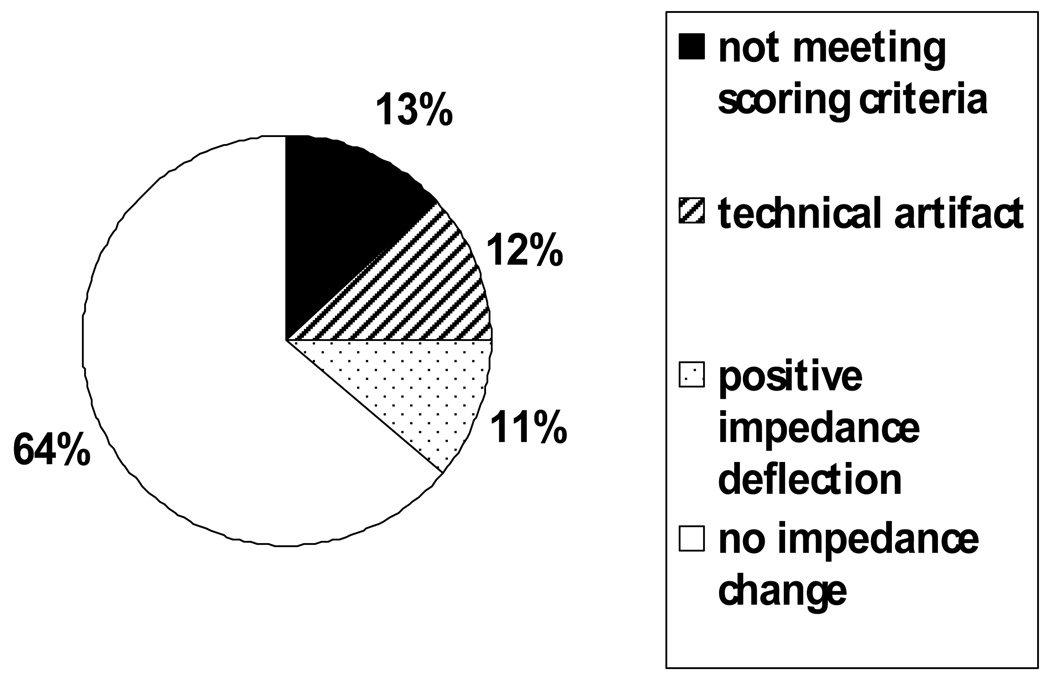
Reasons for failure of impedance to detect an acid based pH event included failure to meet current scoring rule criteria, defined as a drop in at least 2 consecutive impedance channels to ≤50% of baseline in 13% of the missed events (Figure 2). This comprised a decrease in impedance on only one channel in 118 events, and a decrease in impedance that remained >50% of baseline in 77 events. Technical artifact on the impedance channels accounted for 176 or 12% of the events missed by impedance. A positive deflection in impedance, indicating the presence of an air bolus, was seen in 168 events (11%).
Figure 2.
Events detected by pH were not identified by MII due to not meeting scoring criteria on MII (13%), technical artifact (12%), and the presence of a positive impedance deflection or air bolus (11%). The remaining 64% of acid reflux events detected by pH but not impedance had no indication of any change in impedance.
The vast majority of missed events (978 events or 64%) had no indication of a change in impedance. Seven infants had a mean impedance during the entire study of <1000Ω indicating the possibility of inflammation in the esophagus. One hundred fifty four pH-only events with no change in impedance occurred during these studies with 95 events attributed to one infant with a mean study impedance of 566Ω. This preterm infant presented with multiple malformations comprising prior gastroschisis repair, vocal cord paresis, and recurrent aspiration.
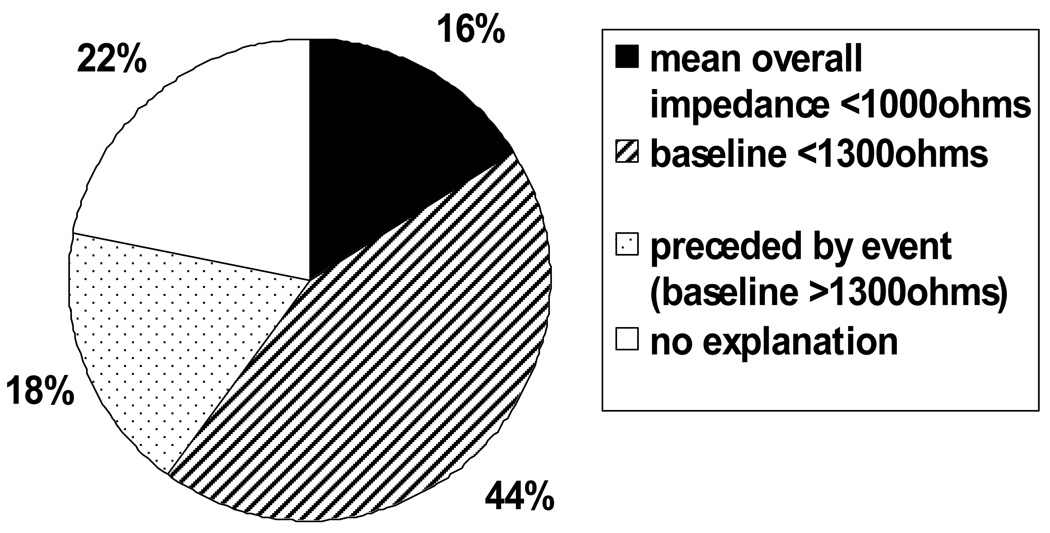
Although mean baseline impedance levels preceding the 978 events with no change in impedance was 1552±883 ohms, 430 events had baseline impedance levels of <1300Ω suggesting the possible presence of non-acid fluid in the esophagus preceding the pH-only event. One hundred seventy five (18%) of the remaining pH-only events had baseline impedance levels ≥1300Ω but were preceded by a reflux episode <30 seconds prior to the event (Figure 3). This represented a median of 5% of pH only events (range: 0–75%) for each infant. There was no explanation for the remaining 220 (22%) of pH-only events with no change in impedance.
Figure 3.
pH-only events accompanied by no change in impedance were associated with 1) a mean overall study impedance of <1000 ohms in 16% of events indicating possible esophageal inflammation, 2) a baseline impedance of <1300 Ω in 44% of events indicating the possible presence of fluid already in the esophagus before the pH-only event and 3) a reflux event preceding the pH-only event in 18% of events indicating incomplete reflux clearance. The remaining 22% of pH-only events had no explanation.
Discussion
This study has shown that 59% of acid based GER events detected by pH in neonates are not detected when impedance based monitoring criteria are employed to detect gastroesophageal reflux. Furthermore, the incidence of these missed events significantly decreased with advancing prenatal and postnatal maturation. Although scoring rule criteria, technical artifact, and the presence of an air bolus were causes for a portion of the missed events the majority of these events had no indication of any change in impedance. pH only events with no indication of a change in impedance were most commonly associated with a low preceding impedance level or occurred in close proximity to a prior GER event indicating the possibility of non-acid fluid being retained in the esophagus before the pH-only event occurred.
The decrease in the incidence of pH only events with increasing gestational and post conceptional age may be due to maturation of gastrointestinal motility. In healthy adults pH-only events are rare 13 with an increase in occurrence to 25% in patients with severe gastroesophageal reflux disease 8. Small studies of 34 and 17 symptomatic term infants have reported from 9 4 to over 40% 5 of pH events missed by MII. Our larger infant cohort of 119 infants has shown a higher incidence of pH-only events. This may be due to the inclusion of preterm infants in this study as the mean incidence in the term infants was 42% versus 54% in the preterm infants. We speculate that the higher proportion of pH only events in the immature infants may be due to immature peristalsis of the esophagus, sphincter tone and gastric emptying 14,15. Additionally, term infants are fed larger volumes which may provide greater buffering capacity.
Discrepancies between studies may also be due to catheter design as location of the pH sensor may vary in relation to the impedance channels. The pH sensor in this study corresponded to impedance channel 6. Data acquired with the pH sensor placed more proximally at impedance channel 5 5 should result in a lower incidence of pH-only events as the refluxate needs to cross two impedance channels before being detected by the pH sensor. Our data have also shown that 12% of pH-only events were not detected by impedance due to technical artifact. This is in agreement with previously published data in term infants 5. To our knowledge there are no current data regarding the incidence of missed events due to the presence of an air bolus or scoring rule criteria to compare with our findings.
One hundred fifty four (16%) pH-only events accompanied by no change in impedance were attributed to seven infants, each having a mean overall study impedance of <1000Ω. Simulated data have shown that the mucosal membrane is the predominating factor in determining impedance levels 16. Although data have shown an inverse relationship between both esophageal wall and mucosal membrane thickness and impedance 16 the actual threshold values for identification of these conditions are unclear. Conductivity of the empty esophageal lumen has been reported as 2000–4000Ω in adults 9 with lower values of 1500–2000Ω in both symptomatic and asymptomatic infants 5,10. The 1000Ω threshold was an arbitrarily cutoff chosen as a value less than the published baseline data for infants. Ninety five of the 154 events were attributed to one infant with a mean overall study impedance of 566Ω. This infant presented with a history of gastrochisis repair and recurrent aspiration. Although the occurrence of esophagitis in this infant population is rare, the low mean impedance may be indicative of esophageal inflammation. However, unless mean impedance values can be associated with confirmed gastroesophageal pathology absolute impedance thresholds may not be obtainable.
In some infants non-acid refluxate may slowly accumulate in the esophagus resulting in a transient decrease in impedance that does not meet criteria as a GER event by MII. During this time, the pH may oscillate around 4 as acid refluxate rises from the esophagus and mixes with the bolus resulting in one or more events detected by pH. As the MII baseline preceding these events would already be low no further drop in impedance would occur. To identify periods where non-acid refluxate may already be present during the baseline preceding an event impedance levels for fluid were needed. Therefore, we estimated impedance values in various refluxate compositions by performing in vitro measurements for formula and breast milk. These comparisons were used to establish a value of <1300Ω as an estimate of the possible presence of a bolus in the esophagus preceding an acid event.
In vitro impedance values were shown to be dependent on the fluid composition. The infants enrolled in this study followed normal clinical practice which includes a multitude of feeding types including breast milk, formula, fortifiers and combinations thereof. It is possible that these various feeding regimens along with additional gastric contents in the esophagus could affect the impedance measurements in vivo resulting in under detection of the presence of a weakly acidic or non-acid bolus preceding the pH-only event using the threshold of <1300Ω in this study.
We speculate that in events with a baseline impedance >1300Ω, the presence of a reflux event occurring <30sec before the event might indicate incomplete clearance of a previous bolus. During an MII event, multiple acid events may occur due to mixing of fluid in the esophagus causing intermittent contact of ions with the pH electrode. Ninety percent of pH-only events reported in term infants 5 have been associated with this occurrence. In the current study, multiple pH events that occurred during an MII event, while the impedance levels still remained below 50% of baseline, were characterized as being associated with that single MII event and excluded from the analysis. However, 175 of pH-only events having a baseline level >1300Ω and no associated change in impedance occurred within 30 seconds of the resolution of a preceding event. Data in adults with mild gastroesophageal reflux disease have shown a higher incidence of impaired propulsive volume clearance when compared to healthy controls 12 indicated by a decrease in post-deglutitive impedance. However, the lower levels of impedance were still within normal baseline ranges reported in healthy adults. Therefore, given the close timing of the events in this study, an association between reflux clearance and the pH-only event could not be excluded with confidence.
Twenty two percent of the pH-only events with no change in impedance were not associated with a low baseline impedance, low overall mean impedance or a preceding GER event. It may be that mechanical limitations of the catheter (ie electrode spacing 16) prohibited detection of small bolus volumes during these events. However, this seems unlikely as previous data have shown that bolus transport volumes of as small as .1cc 6 can be detected with the catheter design used in our study. As a few ions on the pH electrode may cause the pH to fall below 4 this may instead reflect oversensitivity of the pH electrode in detecting acid reflux events.
In 17 infants no discrepancies between pH and MII were found. As the number of events detected by pH in the majority of these infants was low this may have minimized the chances of an event being missed by MII. Although this study did not look at apnea, recent studies have relied on MII to detect both acid and non-acid reflux and further assess the association between apnea and gastroesophageal reflux with conflicting results17,18,19. The results from this study are important in identifying the limitations of this technology to assist in discerning whether or not a true relationship between apnea and gastroesophageal reflux exists.
In conclusion, gastroesophageal events detected by impedance and identified as acid by an accompanying pH electrode may underestimate the incidence of acid reflux detected by pH alone. Our data suggest that detection of gastroesophageal events by MII may be frequently limited by delayed fluid clearance from the esophagus which may be exacerbated in the preterm infant. Therefore, MII alone should not be the primary diagnostic technique to screen for acid reflux until the technical limitations in infants are better understood. In addition, studies in infants with low overall mean impedance levels should be interpreted with caution. Future research is needed to improve the detection of refluxate by MII and to determine the clinical significance of pH only events. Until that time acid reflux events from both MII and pH alone should be reported for each study.
Reference
- 1.Wenzl TG, Moroder C, Trachterna M, et al. Esophageal pH monitoring and impedance measurement: a comparison of two diagnostic tests for gastroesophageal reflux. JPGN. 2002;34:519–523. doi: 10.1097/00005176-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Sondheimer J. Expanding the definition of reflux. JPGN. 2002;34(5):511–512. doi: 10.1097/00005176-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Rudolph CD, Mazur LJ, Liptak G, et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: Recommendations of the north American society for pediatric gastroenterology and nutrition. JPGN. 2001;32(2):S1–S31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 4.Condino AA, Sondheimer J, Pan Z, et al. Evaluation of infantile acid and nonacid gastroesophageal reflux combined pH monitoring and impedance measurement. JPGN. 2006;42:16–21. doi: 10.1097/01.mpg.0000188008.66752.72. [DOI] [PubMed] [Google Scholar]
- 5.Skopnik H, Silny J, Heiber O, et al. Gastroesophageal reflux in infants: evaluation of a new intraluminal impedance technique. JPGN. 1996;23(5):591–598. doi: 10.1097/00005176-199612000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Peter CS, Wiechers C, Bohnhorst B, et al. Detection of small bolus volumes using multiple intraluminal impedance in preterm infants. JPGN. 2003;36:381–384. doi: 10.1097/00005176-200303000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Vandenplas Y, Salvatore S, Devreker T, et al. Gastro-oesophageal reflux disease: oesopheal impedance versus pH monitoring. Acta Paediatica. 2007;96:956–962. doi: 10.1111/j.1651-2227.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 8.Shay SS, Bomeli S, Richter J. Multichannel intraluminal impedance accurately detects fasting, recumbent reflux events and their clearing. Am J Physiol Gastrointest Liver Physiol. 2002;283:G376–G383. doi: 10.1152/ajpgi.00470.2001. [DOI] [PubMed] [Google Scholar]
- 9.Tutuian R, Castell DO. Review article: complete gastro-esophageal reflux monitoring combined pH and impedance. Aliment Pharmacol Ther. 2006;24(2):27–37. doi: 10.1111/j.1365-2036.2006.03039.x. [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Alonso M, Moya MJ, Cabo JA, et al. Twenty-four-hour esophageal impedance-pH monitoring in healthy preterm neonates: Rate and characteristics of acid, weakly acidic, and weakly alkaline gastroesphageal reflux. 2006;118(2):e299–e308. doi: 10.1542/peds.2005-3140. [DOI] [PubMed] [Google Scholar]
- 11.Wise JL, Murray JA. Utilising multichannel intraluminal impedance for diagnosing GERD: a review. Dis Esophagus. 2007;20(2):83–88. doi: 10.1111/j.1442-2050.2007.00654.x. [DOI] [PubMed] [Google Scholar]
- 12.Domingues GR, Winograd R, Lemme EM, et al. Characteristics of oesophageal bolus transport in patients with mild oesophagitis. Eur J Gastroenterol Hepatol. 2005;17:323–332. doi: 10.1097/00042737-200503000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring : A multcenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99(6):1037–1043. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez A, Wong WW, Shulman RJ. Factors regulating gastric emptying in preterm infants. J Pediatr. 2006;149:475–479. doi: 10.1016/j.jpeds.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 15.Jadcherla SR, Hoffman RG, Shaker R. Effect of maturation of the magnitude of mechanosensitive and chemosensitive reflexes in the premature human esophagus. J Pediatr. 2006;149:77–82. doi: 10.1016/j.jpeds.2006.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Zaben A, Chandrasekar V. Effect of esophagus status and catheter configuration on multiple intraluminal impedance measurements. Physiol Meas. 2005;26:229–238. doi: 10.1088/0967-3334/26/3/008. [DOI] [PubMed] [Google Scholar]
- 17.Peter CS, Sprodowski N, Bohnhorst B, et al. Gastroesophageal reflux and apnea of prematurity: no temporal relationship. Pediatrics. 2002;109:8–11. doi: 10.1542/peds.109.1.8. [DOI] [PubMed] [Google Scholar]
- 18.Wenzl TG, Schenke S, Peschgens T, et al. Association of apnea and nonacid gastroesophageal reflux in infants: investigations with the intraluminal impedance technique. Pediatr Pulmonol. 2001;31:144–149. doi: 10.1002/1099-0496(200102)31:2<144::aid-ppul1023>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 19.Slocum C, Arko M, Di Fiore JM, et al. Impact of feeding on gastroesophageal reflux, apnea, bradycardia, and desaturation in preterm infants. PAS. 2008 doi: 10.1038/jp.2008.226. [DOI] [PMC free article] [PubMed] [Google Scholar]