Abstract
Background
The natural history of patients with pathologically proven frontotemporal lobar degeneration (FTLD) is important from clinical and biologic perspectives, but is not well documented quantitatively.
Methods
We examine longitudinal decline in cognitive functioning in an autopsy-proven cohort of patients with the clinical diagnosis of a FTLD spectrum disorder or FTLD pathology using a panel of neuropsychological measures. Patients are categorized according to findings at autopsy into tau-positive FTLD, tau-negative FTLD, and frontal variant-Alzheimer disease (fvAD) subgroups.
Results
Patients decline significantly over time on all neuropsychological measures. Moreover, several measures differentiate between histopathologically distinct subgroups throughout the course of the disease process. This includes a significant double dissociation involving relative difficulty on a visual constructional measure in tau-positive patients compared to relatively impaired visual confrontation naming in tau-negative patients. Longitudinal measures of FAS naming fluency and animal naming fluency also distinguish tau-positive patients and tau-negative patients with FTLD from patients with fvAD. Other measures show significant decline but do not distinguish between histopathologic groups longitudinally.
Conclusion
Our findings suggest different longitudinal patterns of cognitive decline in pathologically defined subgroups of patients. Measures consistently distinguishing between patient subgroups can be used to bolster diagnostic accuracy throughout the course of these diseases, while measures demonstrating undifferentiated longitudinal decline may serve as useful endpoints in treatment trials.
Few quantitative studies of cognitive and social decline in the early onset dementias have been reported, despite their importance for crucial clinical and neurobiological issues such as diagnosis, prognosis, treatment trials, and understanding the nature of the dementing process. Cross-sectional comparisons of patients with an autopsy-confirmed neurodegenerative disease suggest distinct cognitive profiles of impairment in frontotemporal lobar degeneration (FTLD) compared to Alzheimer disease (AD). These findings are important because pathologically proven AD is misdiagnosed clinically as FTLD in 15% to 33% of clinical-pathologic series.1–3 Patients with a pathologically proven form of FTLD are more impaired on executive measures such as category naming fluency (particularly naming words beginning with the letters FAS), for example, while patients with AD are most compromised on measures of episodic memory.4,5 Likewise, contrasts of patients with pathologically distinct forms of FTLD6 associate tau-positive diseases such as dementia with Pick bodies (PiD) and corticobasal degeneration (CBD) with significant impairments on measures of executive functioning such as category naming fluency and visual constructions, while tau-negative diseases such as frontotemporal lobar degeneration with tau-negative but ubiquitin/TDP-43 immunoreactive-positive inclusions (FTLD-U) are associated with significant deficits on language measures such as visual confrontation naming.1,7
A comprehensive clinical assessment of the natural history of autopsy-defined cases with FTLD was recently reported.8 This work is important for characterizing the clinical history of these patients, but difficult to use for practical purposes such as treatment trials since these observations are not quantitative. Longitudinal decline in language9 and social10 domains also has been described, but the survey nature of these measures may cloud the precise source of the deficit under examination. The present study used several quantitative neuropsychological measures to examine the longitudinal course of patients with FTLD with known histopathologic abnormalities, and to distinguish these cases from AD with an atypical presentation.
METHODS
Subjects
An autopsy registry of over 500 neurodegenerative cases at the Center for Neurodegenerative Disease Research of the University of Pennsylvania was examined to identify patients with a clinical diagnosis of an FTLD spectrum disorder or with FTLD pathology who also had neuropsychological evaluations performed on several occasions. This search generated a list of 42 cases. Two cases were excluded because their initial clinical evaluations did not occur until >100 months after reported disease onset. This yielded a final cohort of 40 patients. Clinic visits occurred from 1988 through 2006, and all autopsies were performed at the University of Pennsylvania from 1995 through 2006. All cases participated in an informed consent procedure approved by the Institutional Review Board of the University of Pennsylvania. Table 1 summarizes the demographic characteristics of the participants.
Table 1.
Mean ± SD clinical and demographic characteristics and clinical and pathologic diagnosis
| Tau-positive, n = 17 |
Tau-negative, n = 11 |
Frontal-variant AD, n = 12 |
|
|---|---|---|---|
| Age at initial evaluation, y | 64.82 ± 12.80 | 63.91 ± 8.69 | 63.67 ± 11.02 |
| Education, y | 15.35 ± 2.67 | 16.09 ± 2.30 | 14.67 ± 2.15 |
| Disease duration at initial evaluation, mo* | 31.88 ± 20.43 | 29.82 ± 28.47 | 38.33 ± 24.99 |
| Survival* (mo) | 66 (16) | 78 (76) | 117 (80) |
| MMSE at initial evaluation | 19.88 ± 7.04† | 22.55 ± 6.68 | 21.75 ± 4.20 |
| Mean frequency of protocol administrations | 2.94 ± 2.25 | 4.82 ± 5.04 | 5.08 ± 2.91 |
| Mean time between protocol administrations, mo | 5.62 ± 5.67 | 5.69 ± 7.31 | 7.37 ± 5.07 |
| Duration of testing (1st eval to last eval), mo | 13.76 ± 14.21 | 23.64 ± 25.57 | 28.58 ± 20.74 |
| Clinical syndromic diagnosis at onset‡ | |||
| Progressive nonfluent aphasia | 6 | 0 | 3 |
| Semantic dementia | 0 | 1 | 0 |
| Progressive mixed (logopenic) aphasia | 0 | 1 | 2 |
| Social and executive disorder | 2 | 8 | 3 |
| Corticobasal syndrome | 7 | 0 | 4 |
| Alzheimer disease | 1 | 1 | 0 |
| Dementia with Lewy bodies | 1 | 0 | 0 |
| Pathologic diagnosis§ | |||
| Dementia with Pick bodies | 2 | 0 | 0 |
| Corticobasal degeneration | 11 | 0 | 0 |
| Progressive supranuclear palsy | 2 | 0 | 0 |
| Argyrophilic grain disease | 1 | 0 | 0 |
| FTD-P17 | 1 | 0 | 0 |
| Frontotemporal lobar degeneration with ubiquitin inclusions¶ | 0 | 9 | 0 |
| Motor neuron disease with dementia | 0 | 1 | 0 |
| Dementia lacking distinctive histopathology | 0 | 1 | 0 |
| Alzheimer disease | 0 | 0 | 10 |
| Lewy body variant | 0 | 0 | 2 |
We date onset from the initial persistent clinical complaint. We report median and interquartile range for survival. Patient groups differ in their survival, according to the Kruskal-Wallis test [χ2 (2) = 10.66; p< 0.01]. Tau-positive patients [z = 1.83; p< 0.01] have a shorter survival than patients with frontal-variant Alzheimer disease while tau-negative patients [z = 1.79; p< 0.07] approached significance.
n = 16.
Number of patients assigned a clinical syndrome at presentation.
Number of patients with a pathologic diagnosis assigned at autopsy. Five patients had evidence for multiple histopathologic abnormalities, and patients were assigned to the group based on the dominant pathology. Multiple pathologies included one case of progressive supranuclear palsy (also with features of Parkinson disease and Alzheimer disease); one case with corticobasal degeneration (also with features of Alzheimer disease); one case of motor neuron disease with dementia (also with features of Alzheimer disease); and two cases of Lewy body variant of Alzheimer disease (both with features of Parkinson disease and one with features of argyrophilic grain disease).
One FTLD-U case had a progranulin mutation.
MMSE = Mini-Mental State Examination.
Cases were assigned to three groups on the basis of the pathologic diagnosis at autopsy.1,6 These groups included tau-positive disease, tau-negative disease, and frontal-variant AD (fvAD),11 that is, patients with a clinical diagnosis of an FTLD spectrum disorder who had histopathologic evidence of AD as the primary diagnosis at autopsy. The specific pathologic diagnoses are provided in table 1. There was no difference among tau-positive, tau-negative, and fvAD groups in age at onset, education, duration of illness at the time of initial testing, or severity of dementia (as assessed with the MMSE) at the time of the initial neuropsychological assessment (all p values > 0.2, according to analyses of variance).
A consensus mechanism assigned patients to a clinically defined syndromic subgroup when first seen, based on a modification of published criteria.12,13 At least two experienced individuals independently examined the clinical record, including a detailed history, a mental status examination (this did not include any of the reported neuropsychological measures), and a neurologic examination, but were blinded to the neuropsychological evaluation and imaging data. Open discussion resolved differences. These clinical diagnoses are also summarized in table 1. Briefly, patients with primary progressive aphasia were subdivided into those with a nonfluent variant (progressive nonfluent aphasia) due to effortful speech with grammatic limitations, a semantic dementia variant due to difficulty understanding single words and objects, and a mixed (logopenic) form of primary progressive aphasia involving impairments of both single word processing and slowed speech. Patients with a disorder of social and executive functioning exhibited bizarre behavioral changes such as disinhibition, hyperoral behavior, and apathy. Patients with corticobasal syndrome (CBS) demonstrated difficulty with visual-spatial, apractic, and executive functioning and an asymmetric extrapyramidal disorder. Other available clinical diagnoses included AD, presenting with episodic memory difficulty as well as deficits in language, visual-spatial, and executive domains; and Lewy body variant of AD, with additional attentional deficits an extrapyramidal disorder.
Clinical and neuropsychological protocol
Patients were assessed regularly with portions of a published neuropsychological protocol.14 The frequency of evaluation, the amount of time between evaluations, and the duration of protocol participation are summarized in table 1. Briefly:
Wechsler Adult Intelligence Scale-Revised Digit Span subtest15: Repeat a sequence of numbers in a forward order and then in a backwards order
Letter Fluency16: Generate different words in 60 seconds, excluding proper nouns and numbers, beginning with a specified letter (FAS)
Animal Fluency17: Produce as many names of different animals as possible in 60 seconds
Visual Confrontation Naming18: name line drawings
Semantic Memory19,20: Judge the membership of color photos and words in a familiar semantic category (vegetables, tools)
Verbal Serial List Learning Test–recall and recognition21: Free recall of a 10-word list following three learning trials and a filled delay, followed by a recognition test where the 10 original words were intermixed with 10 novel words
Visual Construction17: copy four geometric designs.
Neuropathologic assessment
Detailed description of the pathology protocol is described elsewhere.1 Briefly, representative tissue obtained at the time of autopsy was fixed in both neutral-buffered formalin and 70% ethanol in 150 mmol/L NaCl, pH 7.4, paraffin-embedded, and cut into 6- to 10-µm-thick sections. Sections were stained with hematoxylin and eosin and Thioflavin S. Immunohistochemistry was performed on sections of neocortex (anterior cingulate gyrus, mid-frontal gyrus, superior temporal gyrus, angular gyrus), hippocampus, putamen, globus pallidus, cerebellum, and midbrain including substantia nigra pars compacta. Immunohistochemistry was performed with antibodies to tau, α-synuclein, ubiquitin, TDP-43, β-amyloid, and other proteins as required to complete the diagnostic workup of atypical cases. The avidin-biotin-peroxidase method with 3,3′-diaminobenzidine for color development was used for all immunostaining. The neuropathologic diagnosis of FTLD was made using criteria that emphasize tau-positive as well as tau-negative but TDP-43/ubiquitin-immunoreactive inclusions in cell bodies of neuronal and glial cells in gray matter, white matter, and subcortical regions.1,22,23 Cases with AD were diagnosed on the basis of histopathology and immunohistochemistry performed with standard and previously published protocols using antibodies that detect phosphorylated tau (PHF124 [provided by Dr. Peter Davies]) and β-amyloid (i.e., 4G8 [Senetek, MD Heights, MO]). Several of these cases were included in previously published clinical-pathologic series.1,23,25
Statistics
Raw scores of neuropsychological data were converted to z-scores based on the performance of 25 age-matched [mean (±SD) = 66.68 (±9.48) years] and education-matched [mean (±SD) = 15.36 (±1.93) years] healthy seniors. Analyses of variance indicated that the age and education of these healthy controls does not differ from the patient groups. A threshold of z = −2.32 (equivalent to a p value of 0.01) was used to identify abnormal performance in patient groups relative to controls when first seen.
A mixed-effect model (Proc Mixed program, SAS v9.1, SAS Institute, Cary, NC) was used to examine longitudinal cognitive decline over 100 months from disease onset in the three pathologically defined groups of patients.26 This statistical procedure accounts for within-subject correlations due to repeated measurement of cognitive variables in the same subjects and for missing data points. Follow-up time was treated as both a random effect and a fixed effect, and a random intercept was also included in the mixed-effect model. Demographic variables and disease diagnosis were treated as fixed effects. The coefficient for the fixed effect estimating monthly change for each neuropsychological measure was used to illustrate longitudinal decline in the figures. For between-group longitudinal analysis using the mixed-effect model, F-statistics were computed for the overall effect of covariates, and t statistics were reported for any two disease group comparisons that were significant. For within-group longitudinal analyses using the mixed effect model, t statistics were reported for any two tasks differing within each disease group. Longitudinal decline may be linear or curvilinear, and we examined both longitudinal effects in the statistical models. Since longitudinal change was rarely curvilinear in this dataset, we report linear effects except where otherwise indicated. Statistical significance was set at the p < 0.05 level (two-tailed) unless otherwise indicated.
RESULTS
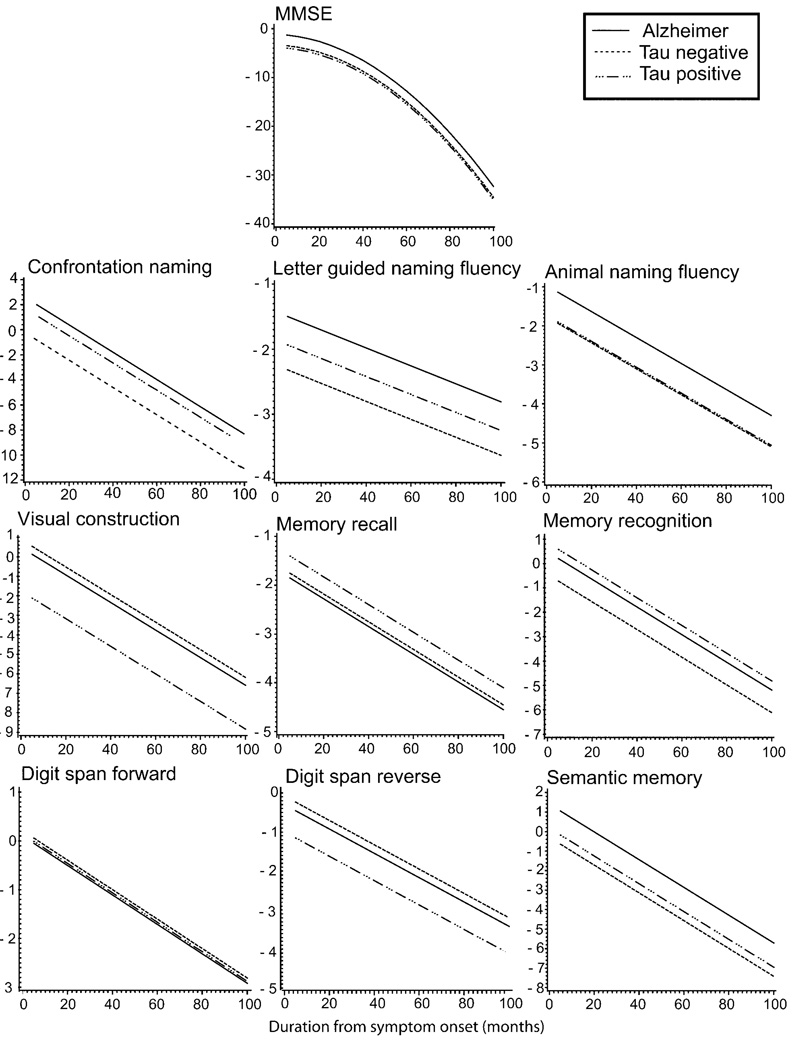
The patient groups did not differ from each other in MMSE scores when first seen. Longitudinal observations of these groups of patients revealed a significant effect of curvilinear decline over time on MMSE performance (F = 20.45; p < 0.0001). The absence of a difference between groups in the MMSE scores was sustained over time. This is illustrated in the figure.
Figure 1. Longitudinal decline on neuropsychological tests.
The slope indicates the rate of monthly decline (x-axis) as reflected by z-score performance on each task (y-axis). Note that the y-axis scale differs from task to task.
Between-group effects at the initial assessment
Table 2 summarizes patient neuropsychological performance at the initial testing session. Differences between groups were found for two tasks: FAS letter fluency [F(2,17) = 18.45; p < 0.001] and visual constructions [F(2,37) = 5.83; p < 0.01]. For letter fluency, fvAD patients were less impaired than tau-positive patients [t(13) = 5.46; p < 0.001] and tau-negative patients [t(5) = 4.52; p < 0.01]. For visual constructions, tau-positive patients were more impaired than tau-negative patients [t(20) = 2.18; p < 0.05].
Table 2.
Mean ± SD neuropsychological test performance at onset*
| Tau-positive |
Tau-negative |
Frontal-variant Alzheimer disease |
||||
|---|---|---|---|---|---|---|
| Raw scores | z-Scores† | Raw scores | z-Scores† | Raw scores | z-Scores† | |
| Visual constructions | 6.13 ± 3.93 (16) | −3.92 ± 3.64 | 10.10 ± 1.45 (10) | −0.24 ± 1.34 | 8.33 ± 2.19 (12) | −1.88 ± 2.03 |
| Confrontation naming | 12.59 ± 2.32 (17) | −1.17 ± 1.73 | 10.50 ± 4.43 (10) | −2.73 ± 3.30 | 11.92 ± 2.75 (13) | −1.67 ± 2.05 |
| Semantic memory | 39.40 ± 7.12 (15) | −2.78 ± 3.69 | 39.00 ± 5.97 (7) | −2.98 ± 3.09 | 39.00 ± 12.66 (13) | −2.98 ± 6.56 |
| Animal naming fluency | 7.13 ± 3.54 (15) | −2.64 ± 0.67 | 8.50 ± 5.76 (10) | −2.38 ± 1.09 | 10.08 ± 4.91 (12) | −2.08 ± 0.93 |
| FAS naming fluency | 9.55 ± 7.46 (11) | −2.41 ± 0.57 | 4.67 ± 6.43 (3) | −2.79 ± 0.49 | 35.75 ± 10.37 (4) | −0.40 ± 0.80 |
| Digits forward | 5.63 ± 1.46 (16) | −0.62 ± 0.97 | 5.78 ± 1.20 (9) | −0.52 ± 0.80 | 5.60 ± 2.01 (10) | −0.64 ± 1.34 |
| Digits reverse | 2.40 ± 1.50 (15) | −1.77 ± 1.15 | 3.75 ± 1.49 (8) | −0.74 ± 1.14 | 3.00 ± 1.12 (9) | −1.31 ± 0.85 |
| Memory recall | 2.94 ± 1.91 (16) | −2.27 ± 1.08 | 3.00 ± 2.79 (10) | −2.24 ± 1.58 | 1.69 ± 2.14 (13) | −2.98 ± 1.21 |
| Memory recognition | 16.19 ± 5.36 (16) | −1.40 ± 2.56 | 15.30 ± 6.17 (10) | −1.83 ± 2.95 | 15.58 ± 2.50 (12) | −1.69 ± 1.98 |
Numbers in parentheses indicate the number of participants who were able to complete each test at the initial evaluation.
Performance relative to 25 age- and education-matched healthy seniors.
Between-group effects assessed longitudinally
Statistical analyses of longitudinal decline are summarized in table 3, and the slopes illustrating longitudinal decline are provided in the figure. Performance on each of the tasks declined over time in all three groups. Several of these measures also showed a difference between groups that was maintained longitudinally. However, we did not observe an interaction of group × neuropsychological decline.
Table 3.
Significant between-group differences in longitudinal neuropsychological test performance
| Main effect for pathology group | Tau-positive vs tau-negative | Tau-positive vs fv-AD | Tau-negative vs fv-AD | Main effect for duration | |
|---|---|---|---|---|---|
| Visual constructions | F = 2.75; p = 0.06 | t = 2.06; p = 0.04* | t = 1.85; p = 0.06† | — | F = 16.96; p = 0.0003 |
| Confrontation naming | F = 4.48; p = 0.01 | t = 2.17; p = 0.03‡ | — | t = 2.93; p = 0.004§ | F = 53.88; p< 0.0001 |
| Semantic memory | F = 1.86; NS | — | — | — | F = 25.50; p< 0.0001 |
| Animal naming fluency | F = 4.00; p = 0.02 | — | t = 2.52; p = 0.01† | t = 2.36; p = 0.02§ | F = 70.26; p< 0.0001 |
| FAS naming fluency | F = 2.86; p = 0.07 | — | — | t = 2.36; p = 0.02§ | F = 4.57; p = 0.05 |
| Digits forward | F = 0.02; NS | — | — | — | F = 17.01; p = 0.0003 |
| Digits reverse | F = 2.27; NS | t = 1.95; p = 0.05* | — | — | F = 18.15; p = 0.0003 |
| Memory recall | F = 1.33; NS | — | — | — | F = 62.54; p = 0.0001 |
| Memory recognition | F = 3.17; p = 0.04 | t = 2.49; p = 0.01‡ | — | — | F = 24.75; p < 0.0001 |
Tau-positive patients more impaired than tau-negative patients.
Tau-positive patients more impaired than fvAD patients.
Tau-negative patients more impaired than tau-positive patients.
Tau-negative patients more impaired than fvAD patients.
fvAD = frontal-variant Alzheimer disease.
On the visual construction measure, we observed significantly worse performance in tau-positive patients relative to tau-negative patients and fvAD patients throughout the course of disease. On measures of language functioning, the tau-negative group had significantly worse visual confrontation naming than the tau-positive group and the fvAD group during the disease course. On language-mediated executive measures, we found significantly poorer longitudinal performance on the animal fluency task in tau-positive patients and tau-negative patients relative to fvAD patients. On the FAS letter fluency task, we observed significantly worse performance in tau-negative patients relative to fvAD patients throughout the course of disease. There was a borderline effect for worse longitudinal performance on the reverse digit span task in tau-positive patients relative to tau-negative patients. Finally, there was a significant difference in longitudinal decline in verbal recognition memory due to the worse performance of tau-negative patients relative to patients with tau-positive disease. To determine whether the observed neuropsychological difficulties were biased in part by the relatively large number of CBD patients in the tau-positive subgroup, we directly contrasted performance in CBD patients with the other tau-positive patients. No significant group differences were found.
Within-group longitudinal effects
Within-group assessments were largely consistent with the profiles emerging from the between-group analyses, as summarized in table 4. Tau-positive patients showed significantly worse performance on visual constructions, letter-guided naming fluency, and semantically guided naming fluency that is sustained throughout the disease course relative to their performance on other neuropsychological measures. Tau-negative patients showed significantly worse performance during the course of the disease on language measures such as visual confrontation naming and semantic memory, verbally mediated executive measures such as animal fluency and FAS letter fluency, and verbal memory recall. Patients with frontal-variant AD showed significant difficulty longitudinally on verbal memory recall, recognition memory, semantic memory, visual confrontation naming, and animal naming fluency relative to other measures.
Table 4.
Significant within-group differences in longitudinal neuropsychological test performance*
| Less impaired task | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visual constructions |
Confrontation naming |
Semantic memory |
Animal naming fluency |
FAS naming fluency |
Digits forward |
Digits reverse |
Memory recall |
Memory recognition |
|
| More impaired task | |||||||||
| Visual constructions | TP | TP | TP | TP | TP | TP | |||
| Confrontation naming | TN | AD | TN, AD | AD | |||||
| Semantic memory | AD | TN | AD | TN | |||||
| Animal naming fluency | TN | TP | TP | TP, AD | TP, TN, AD | TP, TN, AD | TP | TP | |
| FAS naming fluency | TP | TP | TP, TN | TP, TN | TP | ||||
| Digits forward | |||||||||
| Digits reverse | |||||||||
| Memory recall | TN | AD | AD | TN, AD | TN, AD | ||||
| Memory recognition | AD | AD | AD | ||||||
A patient group in a cell indicates significantly worse performance on the task in the left column relative to the task in the top row. All differences are significant at the p < 0.05 level.
TP = tau-positive; TN = tau-negative; AD = frontal-variant Alzheimer disease.
DISCUSSION
Patients with pathologically confirmed FTLD and fvAD decline over time in their performance on measures of language, executive, and visual functioning. Moreover, profiles of longitudinal cognitive decline appear to differ across pathologically defined groups. These observations begin to clarify neurobiological inferences that are supported by clinical-pathologic studies of early onset neurodegenerative diseases, and emphasize important practical implications for differential diagnosis and the identification of measures useful for clinical trials.
In patients with FTLD, tau-positive disease is associated with significantly greater difficulty on a measure of visual constructions than tau-negative disease throughout the course of the condition, while tau-negative disease is associated with significantly greater difficulty longitudinally than tau-positive disease on language measures such as visual confrontation naming. This pattern is confirmed in within-group assessments. Double dissociations such as this have been reported in cross-sectional studies.1,4,27 The basis for this double dissociation, however, is unclear. One contributing factor may be the distinct anatomic distributions of disease in tau-positive and tau-negative patients. This has been shown on MRI studies directly comparing cortical atrophy in tau-positive and tau-negative patients with autopsy-proven disease,28 distinct correlative patterns relating cortical atrophy on MRI in autopsy-proven disease with performance on measures such as confrontation naming and visual construction,7 and different cognitive performance profiles that depend on distinct anatomic distributions of histopathologic abnormalities in autopsy specimens.7,25 Another contributing factor may be related to the cytoarchitectonic distribution of pathology in these conditions.29–31 Some early-onset dementias such as FTLD-U may disproportionately affect superficial layers, thereby interfering with local neuronal processes that support specific cognitive measures. Other diseases such as PiD may compromise neuronal integrity in both superficial and deep layers. Since these conditions compromise pyramidal neurons in deeper layers that are crucial for inter-region connectivity, complex cognitive processes supported by these large-scale neural networks may be selectively more vulnerable in these conditions. Additional work is needed to assess clinical-pathologic hypotheses such as these in cases with tau-positive and tau-negative disease.
These findings also appear to distinguish FTLD from AD. Several clinical-pathologic reports find that patients with an unusual presentation of AD can mimic the clinical phenotype of an FTLD spectrum disorder, resulting in a misdiagnosis.1–3 fvAD patients may present with a social disorder and limited executive resources due to frontal pathology,11 and FTLD-like patients with autopsy-proven AD may have a “logopenic” form of primary progressive aphasia. 32,33 These patients have significant cortical atrophy on MRI in posterior peri-Sylvian regions bilaterally,27 and autopsy-confirmed cases of AD have been described with this “logopenic” clinical presentation.34 Autopsy-confirmed fvAD patients also have impaired episodic memory relative to FTLD patients,1,4,27 and this correlates with MRI cortical volume in medial and lateral temporal regions, and with the histopathologic burden of amyloid in the medial temporal lobe.27
In the present study, we find that patients with a clinical presentation of FTLD that is due to pathologically proven AD differ longitudinally from tau-positive patients and tau-negative patients. Tau-positive patients thus have significantly greater difficulty on a measure of visual constructions than fvAD patients throughout the course of the disease; tau-negative patients are significantly more impaired than fvAD patients on measures of visual confrontation naming and FAS naming fluency; and both tau-positive patients and tau-negative patients are more impaired than fvAD patients on animal naming fluency. Within-patient analyses likewise show significant difficulty in tau-positive patients and tau-negative patients on animal naming fluency and FAS naming fluency. Relative difficulty on measures of animal and FAS naming fluency have been shown previously in cross-sectional studies of pathologically confirmed patients with FTLD compared to patients with AD.1,4,27 Category naming fluency measures such as these are complex, and difficulty on these measures may be due to several different reasons. While it is beyond the scope of this study to establish the basis for a category naming fluency impairment, the deficit in tau-positive patients may be related in part to a limitation of executive resources rather than a disorder of language because of their relatively preserved visual confrontation naming. In the tau-negative patients, the category naming fluency impairment may be due to their difficulty with the language component of these tasks, as suggested by their concurrent confrontation naming impairment. Within-group analyses show that episodic memory is the most impaired measure in fvAD, although between-group longitudinal measures show that tau-negative patients are impaired longitudinally in their verbal recognition memory relative to tau-positive patients, and that fvAD patients differ from neither tau-positive nor tau-negative patients. The longitudinal verbal memory deficit in tau-negative patients also may be related in part to their language difficulties. Memory may not be distinctly impaired longitudinally in fvAD because the hippocampus and medial temporal structures are not as severely impaired in these patients as in patients with the clinical diagnosis of AD.11
We find double dissociations such as these despite observing that subgroups of pathologically defined patients do not differ in overall dementia severity as measured by MMSE at their initial evaluation, and these subgroups maintain similar levels of relative overall dementia severity throughout the course of disease. The MMSE is not very sensitive to overall dementia severity in non-Alzheimer forms of dementia. Recent work attempts to deal with this problem by modifying the MMSE or developing a new instrument,35–37 but these instruments were not available during the early course of these longitudinal data. The double dissociation we observed nevertheless emphasizes that factors like overall dementia severity and disease duration cannot easily account for these neuropsychological differences. The relatively large number of patients with CBD in this cohort may account in part for the visual construction deficit in tau-positive patients. CBD is associated with parietal and frontal disease,25 and direct correlations of cognitive performance with MR imaging and histopathologically defined disease burden in a cross-sectional study relate visual constructional accuracy to tau-positive disease in frontal and parietal cortices.27 Direct comparisons between CBD and other tau-positive conditions do not confirm this possibility, although these results must be interpreted cautiously because of the small numbers of patients in these subgroups. Likewise, the relatively large number of patients with FTLD-U may account in part for the difficulty of tau-negative patients on a language measure such as visual confrontation naming, 1 since naming impairment is a prominent characteristic of semantic dementia14,38 and this syndrome is often associated with FTLD-U.39 Despite the power of such a double dissociation, these observations must be interpreted with some caution. Confirmation with other language, visual construction, executive, and memory measures is needed in a larger cohort of autopsy-proven cases. These findings nevertheless suggest that some consistent diagnostic information may be derived throughout the course of the disease from these simple, noninvasive neuropsychological observations.
While the measures presented above emphasize the differences between these patient subgroups, we also find longitudinal decline on several other neuropsychological measures that does not distinguish between groups. Previous reports of language and social measures that do not differentiate between subgroups of pathologically defined FTD subgroups longitudinally may be due in part to the complexity of survey measures such as these.9,10 In the present study, tau-positive, tau-negative, and fvAD groups are significantly impaired on a measure of semantic memory when first seen, and these groups subsequently appear to decline at the same rate in their performance on this task. Other work suggests that semantic memory is complex and involves multiple components, resulting in impairments in FTLD and AD groups of patients for different reasons.40–43 Likewise, episodic memory recall may not distinguish between groups in part because of the multiple ways in which verbal memory can be impaired,14 including the verbal modality, the representation of episodic memory information, and the executive resources supporting the strategic retrieval and recall of the targets.44,45 Finally, we find that these patient groups do not differ longitudinally on measures such as digit span forward and reverse. Performance on the digit span measures is not significantly impaired when these patients present, and these tasks may be too easy to be sensitive to longitudinal decline. Regardless of the basis for the impairment on these tests of semantic memory, episodic memory, and working memory, measures with a similar rate of decline across patient groups such as these may be useful for monitoring response to an intervention during treatment trials.
Several caveats should be kept in mind when considering our observations. Although we used a conservative statistical approach, a relatively small number of patients participated in this study, and tau subgroups were pathologically heterogeneous. Because these patients were recruited over several years from different clinics, we were able to examine only a restricted range of neuropsychological measures. Additional work is needed to confirm the group differences we observed with a more comprehensive neuropsychological battery examining larger numbers of patients. While we examined longitudinal performance for a longer duration and later in the course of disease than other work,9,10 it is possible that we did not examine patients sufficiently late in the disease process to demonstrate converging group profiles. Patient selection bias is likely to be minimal since we had little control over the particular histopathologic diseases contributing to the groups, although the pathologically defined groups are heterogeneous and therefore limit the generalizability of our observations. With these caveats in mind, our findings suggest different patterns of longitudinal decline in patients with distinct histopathologic diseases. Patients with tau-positive disease are significantly more impaired on a measure of visual construction than tau-negative patients, while patients with tau-negative disease are significantly more compromised than tau-positive patients on a measure of confrontation naming. Longitudinal measures of FAS naming fluency and animal naming fluency also distinguish tau-positive patients and tau-negative patients from patients with a frontal variant of AD. Since these impairment profiles are maintained over time, patients with different neurodegenerative conditions do not necessarily converge on a single, common phenotype as their disease progresses.
Acknowledgments
Supported by the NIH (AG17586, AG15116, AG44266, AG10124) and the Dana Foundation.
GLOSSARY
- AD
Alzheimer disease
- CBD
corticobasal degeneration
- FTLD
frontotemporal lobar degeneration
- FTLD-U
frontotemporal lobar degeneration with tau-negative but ubiquitin/TDP-43 immunoreactive-positive inclusions
- fvAD
frontal variant-Alzheimer disease
- MMSE
Mini-Mental State Examination
- PiD
Pick bodies
Footnotes
Disclosure: The authors report no disclosures.
REFERENCES
- 1.Forman MS, Farmer J, Johnson JK, et al. Frontotemporal dementia: clinicopathological correlations. Ann Neurol. 2006;59:952–962. doi: 10.1002/ana.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodges JR, Davies RR, Xuereb J, et al. Clinicopathological correlates in frontotemporal dementia. Ann Neurol. 2004;56:399–406. doi: 10.1002/ana.20203. [DOI] [PubMed] [Google Scholar]
- 3.Knopman DS, Boeve BF, Parisi JE, et al. Antemortem diagnosis of frontotemporal lobar degeneration. Ann Neurol. 2004;57:480–488. doi: 10.1002/ana.20425. [DOI] [PubMed] [Google Scholar]
- 4.Rascovsky K, Salmon DP, Ho GJ, et al. Cognitive profiles differ in autopsy-confirmed frontotemporal dementia and AD. Neurology. 2002;58:1801–1808. doi: 10.1212/wnl.58.12.1801. [DOI] [PubMed] [Google Scholar]
- 5.Rascovsky K, Salmon D, Hansen LA, Thal LJ, Galasko D. Disparate letter and semantic category fluency deficits in autopsy-confirmed frontotemporal dementia and Alzheimer’s disease. Neuropsychology. 2007;21:20–30. doi: 10.1037/0894-4105.21.1.20. [DOI] [PubMed] [Google Scholar]
- 6.McKhann G, Trojanowski JQ, Grossman M, Miller BL, Dickson D, Albert M. Clinical and pathological diagnosis of frontotemporal dementia: report of a work group on frontotemporal dementia and Pick’s disease. Arch Neurol. 2001;58:1803–1809. doi: 10.1001/archneur.58.11.1803. [DOI] [PubMed] [Google Scholar]
- 7.Grossman M, Libon DJ, Forman MS, et al. Distinct antemortem profiles in pathologically defined patients with frontotemporal dementia. Arch Neurol. 2008 doi: 10.1001/archneur.64.11.1601. (in press) [DOI] [PubMed] [Google Scholar]
- 8.Kertesz A, McMonagle P, Blair M, Davidson W, Munoz DG. The evolution and pathology of frontotemporal dementia. Brain. 2005;128:1996–2005. doi: 10.1093/brain/awh598. [DOI] [PubMed] [Google Scholar]
- 9.Blair M, Marczinski CA, Davis-Faroque N, Kertesz A. A longitudinal study of language decline in Alzheimer’s disease and frontotemporal dementia. J Int Neuropsychol Soc. 2007;13:237–245. doi: 10.1017/S1355617707070269. [DOI] [PubMed] [Google Scholar]
- 10.Marczinski CA, Davidson W, Kertesz A. A longitudinal study of behavior in frontotemporal dementia and primary progressive aphasia. Cogn Behav Neurol. 2004;17:185–190. [PubMed] [Google Scholar]
- 11.Johnson JK, Head E, Kim R, Starr A, Cotman CW. Clinical and pathological evidence for a frontal variant of Alzheimer disease. Arch Neurol. 1999;56:1233–1239. doi: 10.1001/archneur.56.10.1233. [DOI] [PubMed] [Google Scholar]
- 12.Grossman M. Frontotemporal dementia: a review. J Int Neuropsychol Soc. 2002;8:564–583. doi: 10.1017/s1355617702814357. [DOI] [PubMed] [Google Scholar]
- 13.Neary D. Frontotemporal degeneration, Pick’s disease, and corticobasal degeneration. Arch Neurol. 1997;54:1425–1427. doi: 10.1001/archneur.1997.00550230088023. [DOI] [PubMed] [Google Scholar]
- 14.Libon DJ, Xie SX, Moore P, et al. Patterns of neuropsychological impairment in frontotemporal dementia. Neurology. 2007;68:369–375. doi: 10.1212/01.wnl.0000252820.81313.9b. [DOI] [PubMed] [Google Scholar]
- 15.Wechsler D. Wechsler Adult Intelligence Scale. San Antonio: Psychological Press; 1995. [Google Scholar]
- 16.Mickanin J, Grossman M, Onishi K, Auriacombe S, Clark C. Verbal and non-verbal fluency in patients with probable Alzheimer’s disease. Neuropsychology. 1994;8:385–394. [Google Scholar]
- 17.Morris JC, Heyman A, Mohs RC. The consortium to establish a registry for Alzheimer’s disease (CERAD): part I: clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39:1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan E, Goodglass H, Weintraub S. The BOSTON NAMING TEST. Philadelphia: Lea and Febiger; 1983. [Google Scholar]
- 19.Grossman M, D’Esposito M, Hughes E, et al. Language comprehension difficulty in Alzheimer’s disease, vascular dementia, and fronto-temporal degeneration. Neurology. 1996;47:183–189. doi: 10.1212/wnl.47.1.183. [DOI] [PubMed] [Google Scholar]
- 20.Grossman M, White-Devine T, Payer F, et al. Constraints on the cerebral basis for semantic processing from neuroimaging studies of Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1997;63:152–158. doi: 10.1136/jnnp.63.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welsh KA, Butters N, Hughes J, Mohs R, Heyman A. Detection of abnormal memory decline in mild cases of Alzheimer’s disease using CERAD neuropsychological measures. Arch Neurol. 1991;48:278–281. doi: 10.1001/archneur.1991.00530150046016. [DOI] [PubMed] [Google Scholar]
- 22.Dickson DW, Bergeron C, Chin SS, et al. Office of rare diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol. 2002;61:935–946. doi: 10.1093/jnen/61.11.935. [DOI] [PubMed] [Google Scholar]
- 23.Neumann M, Sampathu DM, Kwong LK, et al. Ubiquinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 24.Greenberg SG, Davies P. A preparation of Alzheimer paired helical filaments that displays distinct tau proteins by polyacrylamide gel electrophoresis. Proc Natl Acad Sci USA. 1990;87:5827–5831. doi: 10.1073/pnas.87.15.5827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray RC, Neumann M, Farmer J, et al. Cognitive and motor assessment in autopsy-proven corticobasal degeneration. Neurology. 2007;68:1274–1283. doi: 10.1212/01.wnl.0000259519.78480.c3. [DOI] [PubMed] [Google Scholar]
- 26.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 27.Grossman M, Libon DJ, Forman MS, et al. Distinct ante-mortem profiles in pathologically defined patients with frontotemporal dementia. Arch Neurol. 2008 doi: 10.1001/archneur.64.11.1601. (in press) [DOI] [PubMed] [Google Scholar]
- 28.Whitwell JL, Warren JD, Josephs KA, et al. Voxel-based morphometry in tau-positive and tau-negative frontotemporal lobar degenerations. Neurodegenerative Diseases. 2004;1:225–230. doi: 10.1159/000080990. [DOI] [PubMed] [Google Scholar]
- 29.Harasty JA, Halliday GM, Code C, Brooks WS. Quantification of cortical atrophy in a case of progressive fluent aphasia. Brain. 1996;119:181–190. doi: 10.1093/brain/119.1.181. [DOI] [PubMed] [Google Scholar]
- 30.Harasty JA, Halliday GM, Kril JJ, Code C. Specific temporoparietal gyral atrophy reflects the pattern of language dissolution in Alzheimer’s disease. Brain. 1999;122:675–686. doi: 10.1093/brain/122.4.675. [DOI] [PubMed] [Google Scholar]
- 31.Harasty JA, Halliday GM, Xuereb J, Croot K, Bennett H, Hodges JR. Cortical degeneration associated with phonologic and semantic language impairments in AD. Neurology. 2001;56:944–950. doi: 10.1212/wnl.56.7.944. [DOI] [PubMed] [Google Scholar]
- 32.Gorno-Tempini M, Dronkers NF, Rankin KP, et al. Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol. 2004;55:335–346. doi: 10.1002/ana.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grossman M, Ash S. Primary progressive aphasia: a review. Neurocase. 2004;10:3–18. doi: 10.1080/13554790490960440. [DOI] [PubMed] [Google Scholar]
- 34.Galton CJ, Patterson K, Xuereb J, Hodges JR. Atypical and typical presentations of Alzheimer’s disease: a clinical, neuropsychological, neuroimaging, and pathological study of 13 cases. Brain. 2000;123:484–498. doi: 10.1093/brain/123.3.484. [DOI] [PubMed] [Google Scholar]
- 35.Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a frontal assessment battery at bedside. Neurology. 2000;55:1621–1626. doi: 10.1212/wnl.55.11.1621. [DOI] [PubMed] [Google Scholar]
- 36.Mathuranath PS, Nestor PJ, Berrios GE, Rakowicz WP, Hodges JR. A brief cognitive test battery to differentiate Alzheimer’s disease and frontotemporal dementia. Neurology. 2000;55:1613–1620. doi: 10.1212/01.wnl.0000434309.85312.19. [DOI] [PubMed] [Google Scholar]
- 37.Libon DJ, Massimo L, Moore P, et al. Screening for frontotemporal dementias and Alzheimer’s disease with The Philadelphia Brief Assessment of Cognition: a preliminary analysis. Dement Geriatr Cogn Disord. 2007;24:441–447. doi: 10.1159/000110577. [DOI] [PubMed] [Google Scholar]
- 38.Grossman M, McMillan C, Moore P, et al. What’s in a name: Voxel-based morphometric analyses of MRI and naming difficulty in Alzheimer’s disease, frontotemporal dementia, and corticobasal degeneration. Brain. 2004;127:628–649. doi: 10.1093/brain/awh075. [DOI] [PubMed] [Google Scholar]
- 39.Davies RR, Hodges JR, Kril JJ, Patterson K, Halliday GM, Xuereb JH. The pathological basis of semantic dementia. Brain. 2005;128:1984–1995. doi: 10.1093/brain/awh582. [DOI] [PubMed] [Google Scholar]
- 40.Bozeat S, Lambon Ralph MA, Patterson K, Hodges JR. When objects lose their meaning: what happens to their use? Cogn Affective Behav Neurosci. 2002;2:236–251. doi: 10.3758/cabn.2.3.236. [DOI] [PubMed] [Google Scholar]
- 41.Lambon Ralph MA, McClelland JL, Patterson K, Galton CJ, Hodges JR. No right to speak? The relationship between object naming and semantic impairment: neuropsychological evidence and a computational model. J Cogn Neurosci. 2001;13:341–356. doi: 10.1162/08989290151137395. [DOI] [PubMed] [Google Scholar]
- 42.Koenig P, Smith EE, Grossman M. Semantic categorization of novel objects in frontotemporal dementia. Cogn Neuropsychol. 2006;23:541–562. doi: 10.1080/02643290542000094. [DOI] [PubMed] [Google Scholar]
- 43.Koenig P, Smith EE, Glosser G, et al. Categorization of novel animals by patients with Alzheimer’s disease and corticobasal degeneration. Neuropsychology. 2007;21:195–206. doi: 10.1037/0894-4105.21.2.193. [DOI] [PubMed] [Google Scholar]
- 44.Wagner AD, Schacter DL, Rotte M, et al. Building memories: remembering and forgetting of verbal experiences as predicted by brain activity. Science. 1998;281:1188–1191. doi: 10.1126/science.281.5380.1188. [DOI] [PubMed] [Google Scholar]
- 45.Lepage M, Ghaffar O, Nyberg L, Tulving E. Prefrontal cortex and episodic retrieval mode. Proc Natl Acad Sci USA. 2002;97:506–511. doi: 10.1073/pnas.97.1.506. [DOI] [PMC free article] [PubMed] [Google Scholar]