Abstract
The prevalence of somatoform pain complaints was assessed in a representative sample of 2050 persons in Germany in the age range from 18 to 92 years by the Screening for Somatoform Symptoms questionnaire [57]. A high percentage of the study participants turned out to complain of serious somatoform pains. Most frequently, back pain (30.5%), joint pain, pain in the arms and/or legs (19.9%) and headache or facial pain (19.5%) were reported. Women complained of more somatoform pain symptoms than men. Pain was higher with an increasing age, lower education, lower income, rural residency, and residency in Eastern Germany. While the prevalence of somatoform pain is high, the majority of patients does not receive adequate psychotherapeutic care but is inadequately treated by somatic treatments.
Keywords: somatoform complaints, pain, community survey
Abstract
Im Rahmen einer bevölkerungsrepräsentativen Befragung wurden 2050 in Deutschland lebende Personen im Alter von 18 bis 92 Jahren mittels des Fragebogens „Screening für Somatoforme Störungen" [57] zur Prävalenz somatoformer Schmerzbeschwerden befragt. Es zeigte sich, dass ein hoher Prozentsatz der Befragten das Bestehen somatoformer Schmerzbeschwerden äußert. Am häufigsten werden Rückenschmerzen (30,2% der Untersuchungspersonen), Gelenkschmerzen (25,1%), Schmerzen in den Armen oder Beinen (19,9%) und Kopf- oder Gesichtsschmerzen (19,5%) angegeben. Dabei berichten Frauen mehr somatoforme Schmerzbeschwerden als Männer, mit steigendem Alter werden mehr somatoforme Schmerzen geäußert, und mit geringerem Bildungsgrad, geringerem Haushaltseinkommen, ländlichem Wohnsitz und Wohnsitz in Ostdeutschland erhöht sich die Häufigkeit von Schmerzbeschwerden. Die ermittelte hohe Prävalenz somatoformer Schmerzen steht im deutlichen Widerspruch zur Versorgungsrealität, in der der überwiegende Teil dieser Patienten keine adäquate psychotherapeutische Behandlung erhält, sondern störungsinadäquat im somatischen Gesundheitssystem gebunden ist.
Introduction
Somatic complaints have a high prevalence in the population. Between 80% [34], [35] and 95% [59] of the population reported bodily sensations at least once per week, and during a period of two weeks an average of four different body complaints was reported [18]. Only 5% to 14% of the adults had no symptoms during this time period [65]. Schumacher and Brähler [60] studied a representative sample of the German population by a short form of the Giessen Complaint List (2182 persons aged 18 to 60 years). Most frequently headaches (67.4%), back pain (61.9%), neck pain (57.2%), tiredness (54%) and exhaustion (50.8%) were reported.
Pain symptoms constitute the most significant cluster among physical complaints. Thus in Sweden, 66% of the persons studied between 18 and 84 years reported current or recent pain symptoms [8] while other Swedish studies reported a prevalence for persistent pain of 55% (three months period), or of 49% (six months period), respectively [3], [2]. In a representative American study, a six month prevalence of about 45% was determined for recurrent and persistent pains of different locations [40] and 16% of the subjects in a Canadian study reported that they had suffered from pain in the last two weeks [13]. In a recent Spanish telephone survey 43.2% out of a community telephone sample of 5000 reported having had pain in the previous week [11]. A multinational WHO-study reported an average prevalence of persistent pain (at least six months duration) of 22% (5.5% to 35%) [24].
Back pain, head and facial pain, muscle and joint pain as well as neck and shoulder pain are among the most frequent chronic pain symptoms [2], [8], [13], [31], [67], [39].
A series of epidemiological studies has dealt with the prevalence of back pain ("lower back pain"). In North America, a point prevalence of 5.6% was reported [47], while two German studies found considerably higher point prevalences of 37% to 40% or more [14], [38], [55]. The one year prevalence in the German studies was 73% to 75%. In the general population and for patients in primary medical care in England, prevalence rates of about 36% (referring to an interval of one month to one year) were reported [51], [68]. In a Canadian study with 2000 representative inhabitants of a province, 28.4% of participants reported suffering from back pain at the time of the survey, and 84.1% had already suffered from back pain in the course of their lives [10]. Comparatively stable one month prevalence rates for back pain between 46% and 51% were assessed in large scale studies in Finland which were conducted between 1972 and 1992 with an interval of 5 years [26]. As in other Scandinavian studies, a comparable prevalence of about 50% was shown, however, referring to a one-year period [45], [46]. Further epidemiological studies deal with the prevalence of headaches. Thus Goebel et al. [22] investigated 4061 representative persons and found that 71.4% of participants suffered from headaches at least occasionally. In a representative Norwegian study, 6% of the men and 30.1% of the women reported at least weekly occurring headaches [4].
Neck and shoulder pain are also frequent; however, due to limited space findings cannot be reported in detail [4], [12], [25], [47], [53].
Frequently, no physical causes could be found for the physical complaints. In the literature, some major studies examined persons with frequent physical complaints (including numerous pain symptoms) in order to determine if a physical cause underlies these symptoms. Thus Kroenke and Price [44] could only find physical causes of serious physical symptoms in 31% of 13,538 adults. Myrtek and Fahrenberg [49] found no coronary stenosis in one fourth of those undergoing angiography. Kroenke and Mangelsdorf [43] studied 1000 internal medicine patients with frequent general symptoms and could only determine a significant organic pathology in 16% of the cases. Only in 11% of patients with chest pain an organic cause was found. The same was true in 10% of back pain and abdominal pain cases, respectively. Based on a literature review, Kellner [33] concluded that 20% to 84% of the patients who consulted a physician reported physical complaints without an organic basis. While an unrecognised organic disorder cannot be excluded, these patients were more likely suffering from somatoform disorders. They are treated, however, by somatic treatments, which is known to contribute to chronicity of the somatoform symptoms and cause enormous costs to the health systems [58]. Studies showed that more than six times more money was spent for inpatient treatments of patients with physical complaints without adequate organic explanation than for the average patient; for ambulatory care even 14 times more was spent than for the average patient [62]. According to studies of Escobar et al. [17] these patients utilised medical services three times more frequently than others and in severe cases up to ten times more frequently. Zielke [69] reported 140.3 average work disability days in the last three years for these patients, and a mean of 70.4 hospital days and 32.4 ambulatory physician consultations. Fink [19], [20], [21] found no organic cause among 19% of the "high utilizers" of the Danish health care system. Katon et al. [32] came to similar conclusions in their study of two American hospitals.
Meanwhile, there have been some studies on the epidemiology of pain (e.g. [11]). However, usually they did not differentiate if the pain symptoms were based on an organic cause or not and if they were of a somatoform nature. This discrimination is highly relevant considering the reported frequency of somatoform complaints and the resulting health costs. In order to contribute to empirical knowledge, this paper therefore presents data on the prevalence of explicit somatoform pain complaints.
Methods
Sample and data collection
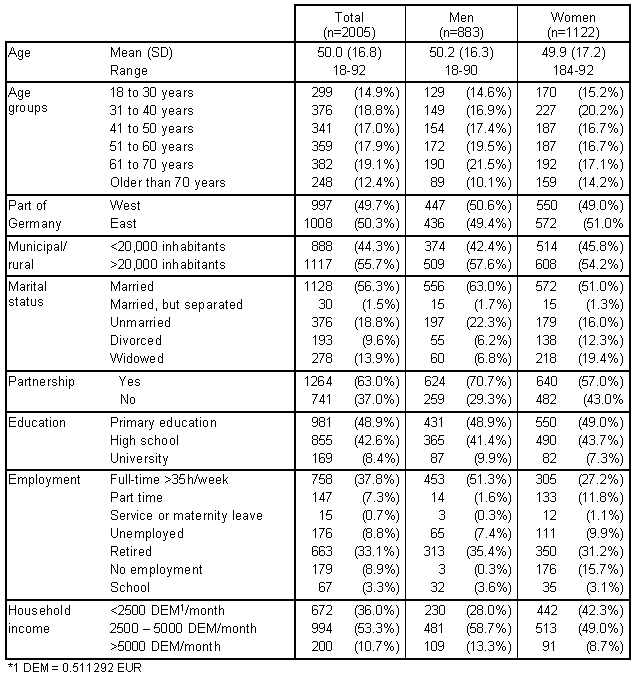
In November/December 1998, 2050 persons were surveyed who were representative for the German population according to age, sex and education. The population of the survey comprised the German speaking inhabitants living in private households with an age of 14 years and higher. Data collection was done as a survey by trained interviewers of a survey institute. The survey was based on the ADM sample system (ADM=Arbeitskreis Deutscher Marktforschungsinstitute) which assured the representativity of the survey. The system was based on the register of the Federal Elections in 1994 from which 96 Eastern and 105 Western German sample points were chosen. Based on these 201 sample points, according to a specific scheme, a street, a house, a floor, an apartment and finally the target person were selected (random-root-procedure). Two call-backs were done before one address was considered a failure. Quality neutral failures (e.g. apartment not inhabited) amounted to 3.8%, systematic failure (target persons refused interview) was 30.6% (total number of addresses=3125). Table 1 (Tab. 1) shows the sample of the participants of 18 years and above according to various sociodemographic parameters.
Table 1. Sociodemographic characteristics of the sample.
Measures
The SOMS 2 (Screening for Somatoform Symptoms, [57]) was used. This questionnaire is a screening instrument for identification of persons with somatoform disorders. It is strictly based on the criteria of the classification systems DSM-IV [1] and ICD-10 [15] which specified symptom lists for the diagnosis of somatoform disorders. A certain number of symptoms is required along with various inclusion and exclusion criteria.
The questionnaire covered the following contents:
· 53 items addressed all physical symptoms which are relevant for the diagnosis of a somatization disorder according to DSM-IV (33 symptoms), and, according to ICD-10, for the diagnosis somatization disorder (14 symptoms) and for the diagnosis of somatoform autonomic disorder (12 symptoms). Symptoms are rated as applicable or not applicable for the period of the last two years. Only those complaints were to be reported for which physicians found no causes and which strongly impaired the well-being of the respondents. Among these items were 10 items measuring the prevalence of somatoform pain symptoms: "head or facial pain", "abdominal or epigastric pain", "back pain", "joint pain", "pain in the legs and/or arms", "chest pain", "rectal pain ", "painful intercourse", "pain during urination", "painful menstruation". Reports of the study participants on these items are the content of the paper presented.
· 10 additional items assessed the inclusion and exclusion criteria of somatoform disorder studied according to the classification systems.
· In addition, another five items were provided for screening of other somatoform disorders.
· The questionnaire has been shown to be psychometrically sound. Norms have been defined based on a representative community sample of 2050 persons in the age of 14 - 92 years [29].
Statistical analysis
Relative frequencies were computed as measures for the prevalence of somatoform complaints. Associations of these complaints with a number of sociodemographic parameters were tested by Kruskal-Wallis.
Results
1. Prevalence of somatoform pain complaints
Table 2 (Tab. 2) shows the frequencies of the somatoform pain complaints studied (manifested in the past two years, no organic causes found by physicians, strongly compromising well-being) for the total sample and according to sex.
Table 2. Percentage of somatoform pain symptoms in the German population (%).
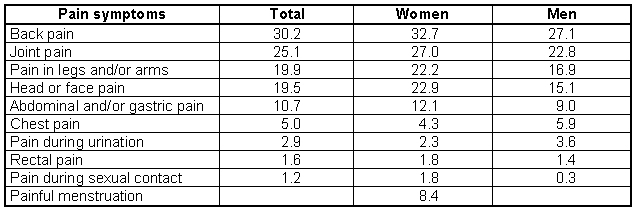
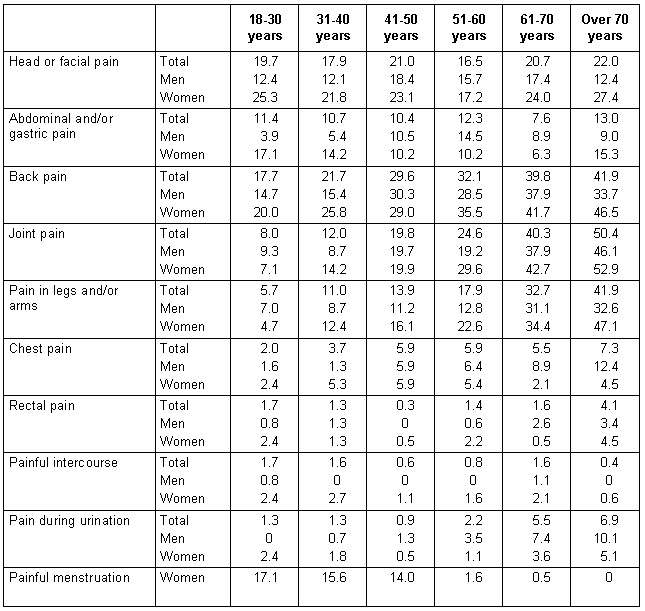
Table 3 (Tab. 3) presents the frequencies of the somatoform pain complaints in relation to age.
Table 3. Percentage of somatoform pain symptoms in the German population according to age and sex (%).
Most frequently, study participants complained of "back pain" (30.2% of the total sample, 32.7% of the women, 27.1% of the men), "joint pain" (25.1% total, 27% of the women, 22.8% of the men), "pain in the arms and/or legs" (19.9% total, 22.2% of the women, 16.9% of the men) and "head or facial pain" (19.5% total, 22.9% of the women, 15.1% of the men).
Table 4 (Tab. 4) presents the most frequent somatoform complaints assessed by the SOMS.
Table 4. The 10 most frequent somatoform complaints in persons of 18 years and above in Germany 1998 (SOMS, [57]).
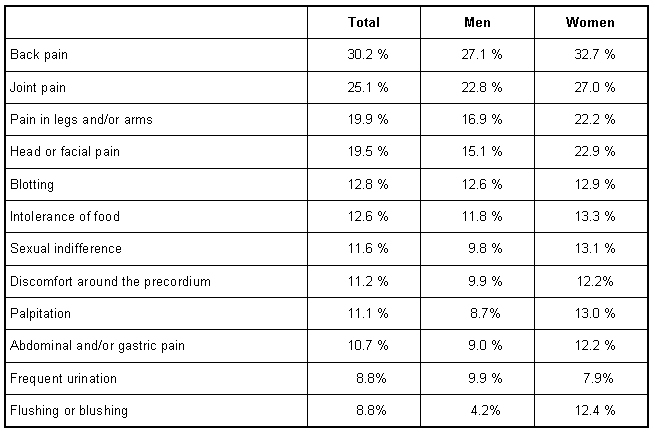
Clearly, pain played a special role among somatoform complaints. Thus, among the 10 most frequent complaints, five referred to pain symptoms and the highest four ranks were also taken by pain.
Figure 1 (Fig. 1) shows the average number of somatoform pain complaints reported depending on age. The presentation discards the item "painful menstruation", as this pain quality is not relevant for all age groups.
Figure 1. Fig. 1: Average somatoform pain symptoms according to age groups (maximum score possible = 9).
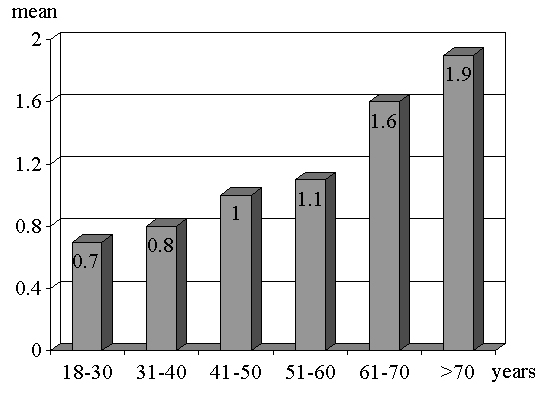
The figure shows that even younger adults reported an average of one somatoform pain symptom, and those aged over 70 years reported an average of two somatoform pain symptoms, i.e. somatoform pain is a ubiquitous common every-day phenomenon.
2. Somatoform pain complaints determined by sociodemographic parameters
As Table 5 (Tab. 5) shows, the sociodemographic parameters "age", "sex", "partnership", "education", "household income", "rural/municipal" and East/West" had an impact on the prevalence of somatoform pain complaints (Kruskal-Wallis test).
Table 5. Impact of sociodemographic characteristics on somatoform pain symptoms (Kruskal-Wallis-Tests χ2).
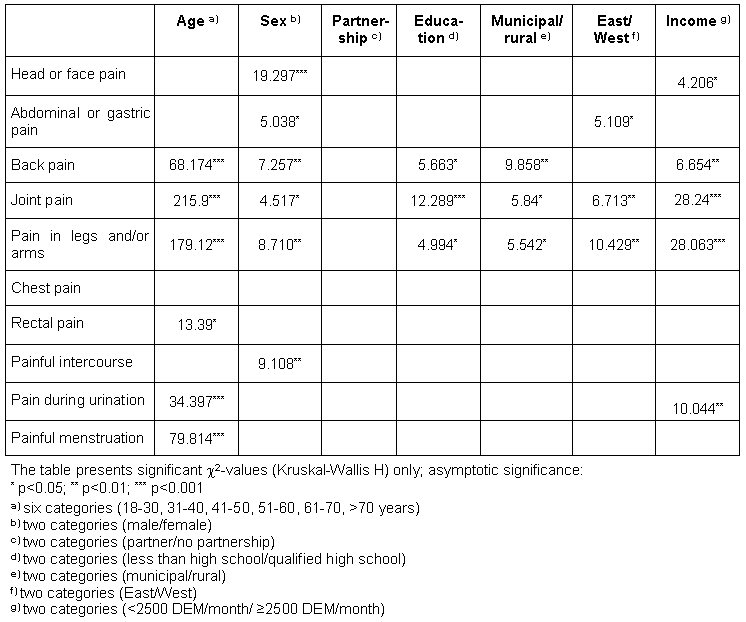
The close relationship between an increasing age and the increase of "back pain", "joint pain" and "pain in the legs and/or arms" was very impressive. Only "painful menstruation" decreased with an increasing age according to expectations.
Women reported "head or facial pain", "back pain", "joint pain", "pain in the legs and/or arms" and "painful intercourse" significantly more frequently than men. "Abdominal or epigastric pain" was also more frequent in women than in men.
More "back pain", "joint pain" and "pain in the legs and/or arms" were associated with a lower degree of education, and a lower degree of household income was associated with more "head or facial pain", "back pain", "joint pain", "pain in the legs and/or arms" and "pain during urination".
Inhabitants of small towns (size <20,000) complained more frequently of "back pain", "joint pain" and "pain in the legs and/or arms" than inhabitants of larger cities, and East Germans more frequently reported "pain in the abdomen", "joint pain" and "pain in the legs and/or arms" than West Germans.
The presence of a partnership, according to this survey, showed no relationship to the intensity of pain complaints.
Discussion
Somatoform pain complaints are very frequent in the general population. Thus 30.2% of the participants reported "back pain" which occurred in the last two years, significantly compromised well-being and lead to ambulatory physician consultations without resulting in the specification of an organic cause. 25.1% of the population reported "joint pain", 19.9% "pain in the legs and/or arms" and 19.5% "headaches".
These findings are very impressive as they only came from persons who reported that their pain had no organic correlate. It is to be conjectured, however, that another significant proportion of persons with somatoform pain did not report the symptoms as fixation on an organic symptom is characteristic for somatoform disorders. The neglect of this organic fixation in somatoform disorders is a significant criticism of the SOMS-2 questionnaire [29], because the insistence on the organogenesis of complaints represents an obligatory diagnostic criterion of somatoform disorders. Careful clinical interviews are therefore necessary for the diagnosis of somatoform disorders in the clinical sector. However, such a procedure is not practicable within a frame representative for the whole population and thus an approach towards diagnostic findings is aimed, using the described questionnaire.
Further, these reports are descriptive and do not allow conclusions regarding etiologic or pathogenic mechanisms of somatization. In its descriptive orientation the SOMS-2 follows the classification systems DSM-IV and ICD-10 which both defined somatoform complaints by counting symptoms based on symptom lists taking inclusion and exclusion criteria (particularly the demand for a lack of the defined physical disorder) into account. These diagnostic algorithms by the classification systems have been questioned repeatedly. Particularly the disregard of significant etiologic and pathogenic aspects of somatoform disorders (e.g. parameters regarding psychopathology, prognosis and cause, relations to psychosocial conditions, integration of emotional aspects) were criticised [30], [42]. The diagnostic procedures of the diagnosis systems imply that somatoform disorders are not diagnosed according to positive characteristics, but rather by negative characteristics (lack of an organic finding). In addition, this procedure subsumes a heterogeneous, only superficially similar collection of disorders [42].
In spite of these critical aspects, the SOMS-2 has been proved as a suitable screening procedure for assessing prevalence data. The etiologic and pathogenic aspects of somatoform disorders, however, can only be determined by more detailed inquiry (interviews).
The high prevalence of somatoform pain disorders is known to be reflected in the high prevalence of the consumption of pain medication. Thus in the federal health survey in 1998, 0.6% to 2.1% (depending on residency and sex) of the 18 to 45 year olds and 2.6% to 7.7% of the 46 to 79 year old reported the daily intake of "medication against rheumatic and vertebral disk complaints" [37]. Analgesics/antirheumatics were the most frequently prescribed medications with a total of 116,000,000 prescriptions (in the year 1995) in Germany [9]. In the East German medication survey, in the state of Sachsen (1991/1992) 10.4% of the women reported having taken analgesics in the previous week [41]. It can be assumed that there is a direct relationship between the high prevalence of somatoform pain disorders in the general population and a high utilisation of somatic treatments [27] as well as a strong consumption of pain medication. The treatment of patients with a somatoform pain disorder in a somatically oriented health system is clearly inadequate. It becomes a major cause for the chronic course of this disease and results in a strong financial demand on the health system. Still psychotherapeutic procedures are only utilised in a small proportion of the general population, which has a high proportion of persons with somatoform pains. According to our representative survey of 2179 persons in 2000 [27], psychosocial professionals (psychiatrists, psychotherapists, psychologists) have only been consulted by a small segment of the population, with about the same frequency as nonmedical (naturopathic) practitioners, community nurses and clergy. Only 1.2% of the survey participants reported having utilised a psychotherapeutic treatment of at least 10 sessions.
Women reported more somatoform pain than men. This corresponds to estimates from the literature showing a clearly higher prevalence for women, particularly for back and head pains than for men. In addition, women complained about stronger and more enduring pain [7]. This sex difference also corresponded to other studies showing that women reported more psychological and body complaints than men and described themselves as sicker [6], [28], [36], [48], [56], [63]. The sex difference we found also corresponded to studies on the prevalence of somatoform complaints. Thus, Kroenke and Price [44] using the diagnostic interview schedules with 13,538 persons showed that 20 out of 32 somatoform complaints (without gynaecological symptoms) were stronger in women than in men. Neumer et al. [50] in their analysis of the literature also confirmed the higher prevalence of somatization disorders in women for the American population.
With an increasing age there was a strong increase of somatoform pain symptoms. The high frequency of somatoform pain complaints in the ageing population has been supported by other studies on the prevalence of pains of different aetiologies. Thus, Gunzelmann et al. [23] studied 593 representative persons over the age of 60 years with the short form of the Giessen complaint list (GBB-24, [5]). Of those, 23% reported strong back pain, 23% strong joint pain, and 18% strong neck pain. Other authors also reported prevalence rates, which differed considerably, however, depending on the assessment instrument and the pain quality (e.g. [16]: more than 22% back pain over 67 years; [54]: in 44% of the participants over 65 years tension headaches, in 11% migraine; [61]: in 63% of the males and 37% of the females over 57% muscle pain; [64]: in 71% of the over 65 year olds joint pain). The high prevalence of somatoform pain symptoms in the ageing population corresponds to the high utilisation of tranquilisers and analgesics in this age group. Thus, Stuck et al. [66] in Swiss citizens aged over 75 years reported an extreme frequency of consumption of benzodiazepines and non-steroidal analgesics. 29% of these aged 75 to 80 years olds and 33% over 80 years olds took benzodiazepines (women 36%, men 21%), and 70% of the participants 74 to 80 year old and 24% of the over 80 year olds consumed non-steroidal analgesics (women 24%, men 15%). The studies of Perrig and Stähelin [52] also showed a high frequency of the consumption of tranquillisers and analgesics in a community sample over 65 years. According to this study, one in ten consumed these medications. The high prevalence of somatoform pain disorders in higher age demonstrates the often underestimated significance of somatization in higher age and points to the importance of biopsychosocial perspective of ageing.
The significance of social and structural parameters for the somatoform pain complaints is underscored by a surplus of pain with low education, low household income, rural residency and residency in Eastern Germany.
To summarise, somatoform pain complaints are very frequent in the German population. The prevalence depends strongly on the age and the sex of the persons afflicted and on the pain localisation. Considering the strong utilisation of the somatic health system, due to the pathological illness behaviour ("doctor shopping") and the inadequate treatment of patients with somatization disorders, the high frequency of somatoform pain disorders has an enormous health, economic and political significance [29].
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington DC: APA; 1994. [Google Scholar]
- 2.Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9:174–182. doi: 10.1097/00002508-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Andersson HI. The epidemiology of chronic pain in a Swedish rural area. Qual Life Res. 1994;3 Suppl 1:19–26. doi: 10.1007/BF00433371. [DOI] [PubMed] [Google Scholar]
- 4.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Brähler E, Scheer JW. Der Gießener Beschwerdebogen. Handbuch. 2. überarb. und ergänzt. Aufl. Bern: Huber; 1995. [Google Scholar]
- 6.Brähler E, Schumacher J, Felder H. Die Geschlechtsabhängigkeit von Körperbeschwerden im Wandel der Zeit. In: Brähler E, Felder H, editors. Weiblichkeit, Männlichkeit und Gesundheit. 2. Auflage. Opladen: Westdeutscher Verlag; 1999. pp. 171–185. [Google Scholar]
- 7.Brattberg G, Parker MG, Thorslund M. A longitudinal study of pain: reported pain from middle age to old age. Clin J Pain. 1997;13:144–149. doi: 10.1097/00002508-199706000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989;37:215–222. doi: 10.1016/0304-3959(89)90133-4. [DOI] [PubMed] [Google Scholar]
- 9.Bundesministerium für Gesundheit. Daten des Gesundheitswesens. Baden-Baden: Nomos Verlagsgesellschaft; 1997. [Google Scholar]
- 10.Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine. 1998;23:1860–1866. doi: 10.1097/00007632-199809010-00012. [DOI] [PubMed] [Google Scholar]
- 11.Catala E, Reig E, Artes M, Aliaga L, Lopez JS, Segu JL. Prevalence of pain in the Spanish population: telephone survey in 5000 homes. Eur J Pain. 2002;6:133–140. doi: 10.1053/eujp.2001.0310. [DOI] [PubMed] [Google Scholar]
- 12.Cote P, Cassidy JD, Carroll L. The Saskatchewan health and back pain survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 1998;23:1889–1898. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 13.Crook J, Rideout E, Browne G. The prevalence of pain complaints in a general population. Pain. 1985;18:299–314. doi: 10.1016/0304-3959(84)90824-8. [DOI] [PubMed] [Google Scholar]
- 14.Deck R, Kohlmann T, Raspe H. Zur Epidemiologie von Rückenschmerzen. Psychomed. 1993;5:164–168. [Google Scholar]
- 15.Dilling H, Mombour W, Schmidt MH. Internationale Klassifikation psychischer Störungen. ICD-10, Kapitel V (F). Klinisch-diagnostische Leitlinien. Bern: Huber; 1993. [Google Scholar]
- 16.Edmond SS, Felson DT. Prevalence of back symptoms in elders. J Rheumat. 2000;27:220. [PubMed] [Google Scholar]
- 17.Escobar JI, Golding JM, Hough RL, Karno M, Burnam MA, Wells KB. Somatization in the community: relationship to disability and use of services. Am J Pub Health. 1987;7:837–840. doi: 10.2105/ajph.77.7.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faller H. Somatisierung, Krankheitsattribution und Public Health. Z Klin Psychol Psychiat Psychother. 1998;46:193–214. [Google Scholar]
- 19.Fink P. Physical complaints and symptoms of somatizing patients. J Psychosom Res. 1992;36:125–136. doi: 10.1016/0022-3999(92)90021-s. [DOI] [PubMed] [Google Scholar]
- 20.Fink P. Surgery and medical treatment in persistent somatization patients. J Psychosom Res. 1992;36:439–447. doi: 10.1016/0022-3999(92)90004-l. [DOI] [PubMed] [Google Scholar]
- 21.Fink P. The use of hospitalization by persistent somatizing patients. Psychol Med. 1992;22:173–180. doi: 10.1017/s0033291700032827. [DOI] [PubMed] [Google Scholar]
- 22.Göbel H, Petersen-Braun M, Soyka D. Die Prävalenz von Kopfschmerzen in Deutschland. Eine Untersuchung an einer repräsentativen Stichprobe auf der Basis der Kopfschmerzklassifikation der Internationalen Headache Society. Schmerz. 1993;7:287–297. doi: 10.1007/BF02529865. [DOI] [PubMed] [Google Scholar]
- 23.Gunzelmann T, Schumacher J, Brähler E. Prävalenz von Schmerzen im Alter: Ergebnisse repräsentativer Befragungen der deutschen Altenbevölkerung mit dem Gießener Beschwerdebogen. Schmerz. 2002;16(4):249–254. doi: 10.1007/s00482-002-0136-3. [DOI] [PubMed] [Google Scholar]
- 24.Gureje O, Korff, Simon GE, Gater R. Persistent pain and well-being: A World Health Organization study in primary care. JAMA. 1998;280:147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 25.Hasvold T, Johnsen R. Headache and neck or shoulder pain - frequent and disabling complaints in the general population. Scand J Prim Health Care. 1993;11:219–224. doi: 10.3109/02813439308994834. [DOI] [PubMed] [Google Scholar]
- 26.Heistaro S, Vartiainen E, Heliovaara M, Puska P. Trends of back pain in eastern Finland, 1972-1992, in relation to socioeconomic status and behavioral risk factors. Am J Epidemiol. 1998;148:671–682. doi: 10.1093/aje/148.7.671. [DOI] [PubMed] [Google Scholar]
- 27.Hessel A, Geyer M, Brähler E. Inanspruchnahme des Gesundheitswesens und Akzeptanz psychosozialer Kompetenzen. Z. Psychosom. Psychother. 2000;46:226–241. [PubMed] [Google Scholar]
- 28.Hessel A, Geyer M, Plöttner G, Schmidt B, Brähler E. Subjektive Einschätzung der eigenen Gesundheit und subjektive Morbidität in Deutschland - Ergebnisse einer bevölkerungsrepräsentativen Befragung. Z Psychother Psychosom Med Psychol. 1999;49:264–274. [PubMed] [Google Scholar]
- 29.Hessel A, Geyer M, Schumacher J, Brähler E. Somatoforme Beschwerden in der Bevölkerung Deutschlands. Z Psychosom Psychother. 2002;48:38–58. doi: 10.13109/zptm.2002.48.1.38. [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann SO. Somatisierungsstörung und somatoforme Störungen - Herkunft der Konzepte und ihre Abbildung in den neuen diagnostischen Glossaren. In: Rudolf SO, Henningsen SO, editors. Somatoforme Störungen: Theoretisches Verständnis und therapeutische Praxis. Stuttgart: Schattauer; 1998. pp. 3–12. [Google Scholar]
- 31.James FR, Large RG, Bushnell JA, Wells JE. Epidemiology of pain in New Zealand. Pain. 1991;44:279–283. doi: 10.1016/0304-3959(91)90097-H. [DOI] [PubMed] [Google Scholar]
- 32.Katon WJ, Korff, Lin E. Panic disorders: Relationship to high medical utilization. Am J Med. 1992;92 (Suppl 1A:7–11. doi: 10.1016/0002-9343(92)90130-4. [DOI] [PubMed] [Google Scholar]
- 33.Kellner R. Functional somatic syndroms and hypochondriasis. Arch Gen Psychiat. 1985;42:821–833. doi: 10.1001/archpsyc.1985.01790310089012. [DOI] [PubMed] [Google Scholar]
- 34.Kellner R. Somatization and Hypochondriasis. New York: Praeger Publishers; 1986. [Google Scholar]
- 35.Kirmayer LJ, Robbins JM. Functional somatic syndromes. In: Kirmayer LJ, Robbins JM, editors. Current concepts of somatization: research and clinical perspectives. Washington: American Psychiatric Press; 1991. pp. 79–106. [Google Scholar]
- 36.Kirschner W, Radoschewski M, Kirschner R. § 20 SBG V Gesundheitsförderung, Krankheitsverhütung. Ursachen zur Umsetzung durch die Krankenkassen. St. Augustin: Asgard; 1995. [Google Scholar]
- 37.Knopf H, Melchert HU. Subjektive Angaben zur täglichen Anwendung ausgewählter Arzneimittelgruppen - Erste Ergebnisse des Bundes-Gesundheitssurveys 1998. Gesundheitswesen. 1999;61, Sonderheft 2:151–157. [PubMed] [Google Scholar]
- 38.Kohlmann T, Raspe HH. Deskriptive Epidemiologie chronischer Schmerzen. In: Geissner E, Jungnitsch G, editors. Psychologie des Schmerzes. Diagnose und Therapie. Weinheim: Psychologie Verlags Union; 1992. pp. 11–23. [Google Scholar]
- 39.Korff, Dworkin SF, Le Resche L, Kruger A. An epidemiological comparison of pain complaints. Pain. 1988;32:173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 40.Korff, Dworkin SF, Le Resche L. Graded chronic pain status: An epidemiological evaluation. Pain. 1990;40:279–291. doi: 10.1016/0304-3959(90)91125-3. [DOI] [PubMed] [Google Scholar]
- 41.Krappweis J, Schwarz U, Kirch W. Der Arzneimittelgebrauch bei Frauen im Bundesland Sachsen auf der Grundlage von Survey-Daten. Gesundheitswesen. 1996;58, Sonderheft 2:115–119. [PubMed] [Google Scholar]
- 42.Kriebel R, Paar G, Stäcker K-H. Somatisierung. Psychotherapeut. 1996;41:201–214. [Google Scholar]
- 43.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: Incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 44.Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Int Med. 1993;153:2474–2480. [PubMed] [Google Scholar]
- 45.Leboeuf-Yde C, Kloughart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine. 1996;21:1518–1525. doi: 10.1097/00007632-199607010-00005. [DOI] [PubMed] [Google Scholar]
- 46.Leboeuf-Yde C, Lauritsen JM. The prevalence of low back pain in the literature. A structured review of 26 Nordic studies from 1954 to 1993. Spine. 1995;20:2112–2118. doi: 10.1097/00007632-199510000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther. 1999;79:384–396. [PubMed] [Google Scholar]
- 48.Maschewski-Schneider U, Greiser E, Helmert U. Sind Frauen gesünder als Männer? Zur gesundheitlichen Lage der Frauen in der Bundesrepublik Deutschland. Soz Präv Med. 1998;33:173–180. doi: 10.1007/BF02078426. [DOI] [PubMed] [Google Scholar]
- 49.Myrtek M, Fahrenberg J. Somatoforme Störungen: Konzeptionelle und methodologische Kritik und ein Plädoyer für die funktionale Analyse des Krankheitsverhaltens. In: Margraf J, Neumer S, Rief W, editors. Somatoforme Störungen: Ätiologie, Diagnose und Therapie. Berlin: Springer; 1998. pp. 192–212. [Google Scholar]
- 50.Neumer S, Lieb R, Margraf J. Epidemiologie. In: Margraf J, Neumer S, Rief W, editors. Somatoforme Störungen: Ätiologie, Diagnose und Therapie. Berlin: Springer; 1998. pp. 37–49. [Google Scholar]
- 51.Papageorgiou AC, Croft PR, Ferry S, Jayson MI, Silman AJ. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine. 1995;20:1889–1894. doi: 10.1097/00007632-199509000-00009. [DOI] [PubMed] [Google Scholar]
- 52.Perrig P, Stähelin HB. Frauen und Gesundheit im Alter - Objektive und subjektive Gesundheit und Gesundheitsverhalten von pensionierten Arbeiterinnen und Angestellten. Z Gerontopsychol Gerontopsychiat. 1996;9:195–205. [Google Scholar]
- 53.Pope DP, Croft PR, Pritchard CM, Silman AJ. Prevalence of shoulder pain in the community: the influence of case definition. Ann Rheum Dis. 1997;30:3088–3012. doi: 10.1136/ard.56.5.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prencipe M, Casini AR, Ferretti C, Santini M, Pezzella F, Scaldaferri N, Culasso F. Prevalence of headache in an elderly population: attack frequency, disability, and use of medication. J Neurol Neurosurg Psychiat. 2001;70:377. doi: 10.1136/jnnp.70.3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Raspe HH, Wasmus A, Greif G, Kohlmann T, Kindel P, Mahrenholtz M. Rückenschmerzen in Hannover. Akt Rheumatol. 1990;15:32–37. [Google Scholar]
- 56.Riecher-Rössler A. Psychische Erkrankungen bei Frauen - einige Argumente für eine geschlechtersensible Psychiatrie und Psychotherapie. Z Psychosom Psychother. 2000;46:129–139. doi: 10.13109/zptm.2000.46.2.129. [DOI] [PubMed] [Google Scholar]
- 57.Rief W, Hiller W, Heuser J. SOMS - Das Screening für Somatoforme Störungen: Manual zum Fragebogen. Bern: Huber; 1997. [Google Scholar]
- 58.Rief W. Die somatoformen Störungen - Großes unbekanntes Land zwischen Psychologie und Medizin. Z Klin Psychol. 1996;25:173–189. [Google Scholar]
- 59.Schepank H. Psychogene Erkrankungen in der Stadtbevölkerung. Berlin: Springer; 1987. [Google Scholar]
- 60.Schumacher J, Brähler E. Prävalenz von Schmerzen in der deutschen Bevölkerung: Ergebnisse repräsentativer Erhebungen mit dem Gießener Beschwerdebogen. Schmerz. 1999;13:375–384. doi: 10.1007/s004829900046. [DOI] [PubMed] [Google Scholar]
- 61.Scudds RJ, Robertson JM. Pain factors associated with physical disability in a sample of community-dwelling senior citizens. J Gerontol A Biol Sci Med Sci. 2000;55(7):M393–M399. doi: 10.1093/gerona/55.7.m393. [DOI] [PubMed] [Google Scholar]
- 62.Smith GR, Monson RA, Ray DC. Patients with multiple unexplained symptoms. Their characteristics, functional health, and health care utilization. Arch Int Med. 1986;146:69–72. [PubMed] [Google Scholar]
- 63.Statistisches Bundesamt. Datenreport 1997. Zahlen und Fakten über die Bundesrepublik Deutschland. Bundeszentrale für politische Bildung; 1997. [Google Scholar]
- 64.Sternbach RA. Survey of pain in the United States: the Nuprin pain report. Clin J Pain. 1986;2:49–53. doi: 10.1016/0304-3959(86)90224-1. [DOI] [PubMed] [Google Scholar]
- 65.Stewart DE. Emotional disorders misdiagnosed as physical illness: Environmental hypersensitivity, candidiasis hypersensitivity, and chronic fatigue syndrome. Int J Ment Health. 1990;19:56–68. [Google Scholar]
- 66.Stuck AE, Gloor BD, Pfluger DH, Minder CE, Beck JC. Geschlechtsunterschiede im Medikamentenkonsum bei über 75jährigen Personen zu Hause: Eine epidemiologische Untersuchung in Bern. Z Geront Geriat. 1995;28:394–400. [PubMed] [Google Scholar]
- 67.Taylor H, Curran NM. The Nuprin Pain Report. New York: Louis & Harris; 1985. [Google Scholar]
- 68.Walsh K, Cruddas M, Coggon D. Low back pain in eight areas of Britain. J Epidemiol Community Health. 1992;46:227–230. doi: 10.1136/jech.46.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zielke M. Kosten-Nutzen-Aspekte somatoformer Störungen. In: Margraf J, Neumer S, Rief W, editors. Somatoforme Störungen: Ätiologie, Diagnose und Therapie. Berlin: Springer; 1998. pp. 69–94. [Google Scholar]