Abstract
The Nottingham Health Profile (NHP [1]) is a widely used instrument to measure subjective health in clinical research. However, there are no age-specific norms for older adults in Germany. The present study was conducted to analyze the psychometric properties of the German version of the Nottingham Health Profile (NHP) in older people. Age-specific reference values for the elderly are presented. Subjects were drawn from the general population of older German people aged 61 to 95 years (n=630; mean age 69.5 years; 55.7% female). Five of the six NHP scales revealed a good internal consistency (.70≤α≤.92). The subscales (with the exception of the subscale social isolation) showed moderate relations with instruments measuring somatization disorders and subjective body complaints (Screening for Somatoform Disorders SOMS [2]); Giessen Subjective Complaints List GBB-24 [3]). Compared to younger subjects, subjective health decreases with age. Therefore age-specific reference data for older people are necessary. Differential reference data are reported for four age groups above 60 years of age and for male and female older people. The outcome confirms that the NHP is a reliable, valid instrument to measure subjective health in older people.
Keywords: older people, subjective health, Nottingham Health Profile
Abstract
Das Nottingham Health Profile (NHP) ist ein weit verbreitetes Verfahren zur Erfassung subjektiver Gesundheit in der klinischen Forschung. Für den deutschsprachigen Bereich liegen aber bislang noch keine altersspezifischen Normwerte für die ältere Bevölkerung vor.
Die vorliegende Studie prüft die psychometrische Qualität der deutschsprachigen Version des Nottingham Health Profile (NHP) in der Anwendung bei älteren Menschen und präsentiert altersspezifische Referenzwerte. Die Stichprobe stammt aus der deutschen Allgemeinbevölkerung und umfasst Personen im Alter von 61 bis 95 Jahre (n=630; Durchschnittsalter 69,5 Jahre, 55,7% weiblich).
Fünf der sechs NHP-Skalen weisen eine gute interne Konsistenz auf (,70≤α≤,92). Die Subskalen (mit Ausnahme der Subskala Soziale Isolation) zeigen mittlere Zusammenhänge mit Instrumenten zur Erfassung somatoformer Störungen und subjektiver Körperbeschwerden (Sreening für Somatoforme Störungen SOMS; Giessener Beschwerdebogen GBB-24). Im Vergleich mit jüngeren Menschen nimmt die subjektive Gesundheit im höheren Lebensalter ab. Dies bestätigt die Notwendigkeit altersspezifischer Referenzwerte für Ältere. Für vier Altersgruppen über 60 Jahre sowie für Frauen und Männer werden differenzierte Referenzwerte dargestellt. Die Ergebnisse bestätigen, dass der NHP ein reliables, valides Instrument zur Erfassung subjektiver Gesundheit bei Älteren ist.
Introduction
In medical treatment, subjective health is a relevant indicator of therapeutic success [4], [5]. This is in line with the conception of health of the World Health Organization, which understands health as more than the absence of illness and which implies also subjective ratings of health, mental wellbeing and social relations. Consequently, subjective health concerns an important question in gerontological research and in clinical diagnostics of healthy and ill older people or in older people with functional limitations [6], [7], [8], [9]. Empirical research revealed that subjective ratings of health are as relevant for independent living in older people as the objective medical status [10], [11]. Furthermore, subjective health is a significant predictor for depression, hospitalization and mortality in the older people [12], [13], [14], [15], [16], [17], [18], [19]. Several questionnaires have been developed to measure subjective health (e.g. Short Form General Health Survey SF-36 [20]; Nottingham Health Profile NHP [1]).
Not all current instruments are concerned with subjects over 60 years. However, there are age-related somatic, mental or social changes that might reduce subjective health in older people. On the other hand, gerontological research on resilience shows that older people are able to accommodate to age-related changes and thus preserve quality of life despite of those changes [21]. Therefore it seems not to be appropriate to relate ratings of subjective health of older people to reference values of younger people. Rather, age-specific reference values are necessary.
For the SF-36, one of the internationally most often used instruments for measuring subjective health and health-related quality of life, there are some age-specific reference values for older patients [22], [23], [24], [25] or for older people from the general population from epidemiological studies and population surveys in different countries [26], [27], [28].
The NHP is another frequently used international questionnaire that can be considered as one of the standard methods for measuring subjective health and distress in clinical studies. In gerontological research, the NHP is often used in clinical studies, e.g. regarding patients with heart failure [29] or after coronary artery bypass grafting [30], Parkinson patients [31], dementia patients [32], patients after hip fracture [33], older people at risk of malnutrition [34], [35] or patients in orthopaedic practice [36].
In a recent study conducted by McQueen, Long and Schurman [36], the SF-36 and the NHP were compared regarding the evaluation of therapeutic effects for older orthopaedic patients. The authors state that there are some advantages of the NHP compared to the SF-36 in older people. The NHP seems to be appropriate for older people because the items are easy to answer with "yes" or "no", whereas the items of the SF-36 are to be answered in a more complex way using two to six different categories.
The internal consistency of the SF-36 and the NHP can be compared in clinical populations. The German version of the NHP was evaluated based on a sample which was representative for the German population [37]. From this evaluation it can be concluded that the NHP cannot differentiate between subjects in the range of low and medium levels of complaints. However, there was a significant age-related decline of subjective health above the age of 60 years and older. Therefore it can be assumed that the NHP-items are more appropriate to assess subjective health in older people experiencing an age-associated decline of physiological and psychological functioning and consequently a higher degree of health-related complaints. Therefore the NHP should be considered as an alternative to the more widely used SF-36 in research regarding older people. For the NHP, however, there are only few age-specific reference values for the non-clinical population of older people [31], although, in terms of health deficits, the older people constitute the most important group in medical care.
This study was carried out to determine whether the NHP is a suitable instrument to measure subjective health in older people, based on data of the above mentioned survey on the general German population [37].
The aim of the present study is to analyze the psychometric properties of the NHP in older people (internal consistency, concurrent validity). Age-related differences between older and younger people (18 to 60 years) will be presented because the results of Hinz et al. [37] are not available in English. Furthermore, age-specific reference data for older people over 60 years of age will be given. Finally, relations between health-related quality of life, subjective body complaints and somatoform disorders in older people will be analyzed.
Methods
Sample
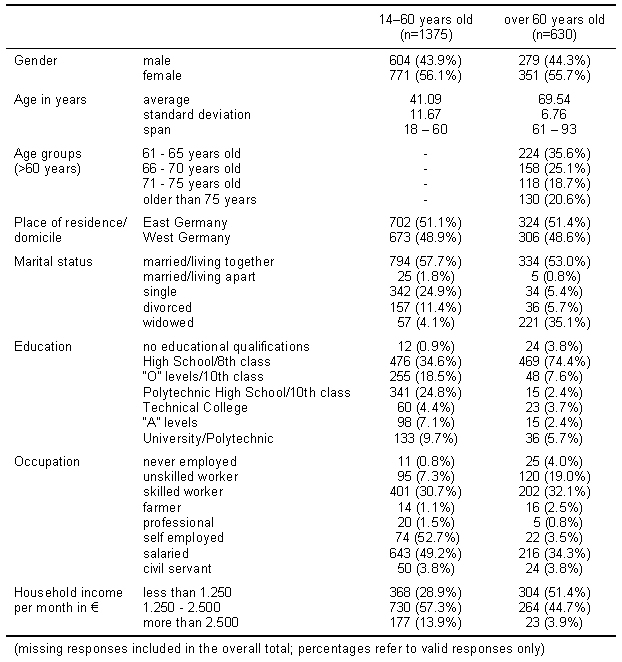
For the current study, a random sample from the general population was examined. The sample consisted of 2005 people aged between 18 and 92 years. The response rate was 69.2%, and finally the sample included 630 people over 60 years old (average age 69.5 years; 55.7% female) of whom complete data from the NHP were available. Further socio-economic and socio-demographic details can be found in Table 1 (Tab. 1). The interviewed elderly were living independently. There were no older people living in institutions in the sample.
Table 1. Socio-demographic characteristics of the general population sample.
The research data were obtained by a public opinion institute by means of multiple topic questionnaires. The subjects were interviewed at home. The households were selected from 201 sample points in Germany. Each household was selected by chance. Interviewees from each of the households were also selected randomly. Subjects participated voluntarily after informed consent had been obtained.
Data analysis
Reliability (internal consistency, split-half reliability) and concurrent validity of the NHP were analyzed. Furthermore, the inter-correlations of the scales are reported. In order to test differences between younger and older subjects regarding health-related quality of life, the whole sample was divided into three age groups (18-40 years, 41-60 years and over 60 years). The possible effect of age and gender in the older people over 60 years of age was investigated by means of a multi-factorial ANOVA with four age groups (61-65 years, 66-70 years, 71-75 years and over 75 years) and sex. Because of the large sample size, only differences with an error probability of p<.001 were taken into account. Relationships between subjective perceptions of health, body complaints and somatoform disorders were tested by means of correlation analysis, in which, due to sample size, coefficients with a level of p<.001 were regarded as relevant.
The statistical analysis was carried out by means of SPSS for Windows, version 8.0.
Questionnaires
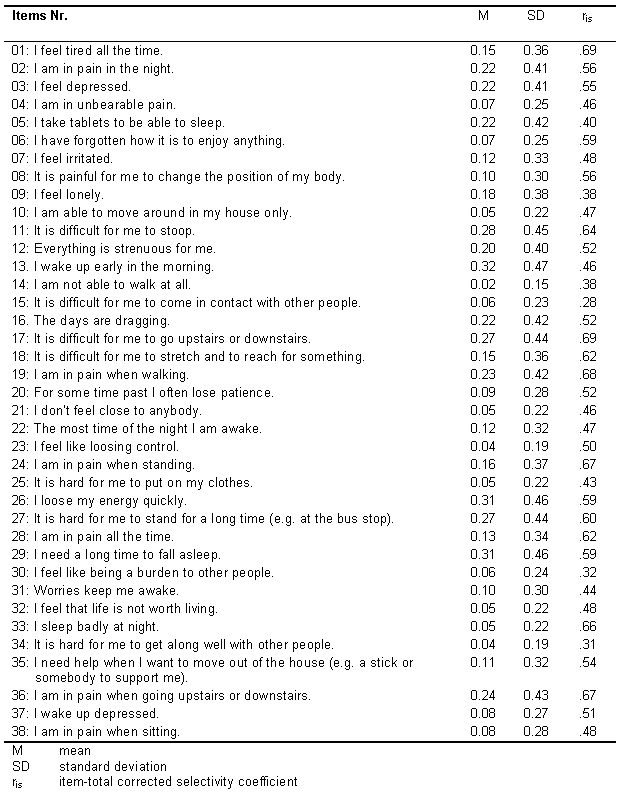
The Nottingham Health Profile [1] was used in a German version, developed by Kohlmann, Bullinger & Kirchberger-Blumstein [38]. It consists of 38 items (complaints) which the respondent has to evaluate as presently occuring or not ("yes", "no"; cf. Table 2(Tab. 2)). The items are assigned to one of the following categories: energy loss, pain, burdensome emotional reactions, sleeping problems, social isolation, and physical mobility. A higher value corresponds to a greater extent of disturbance.
Table 2. Psychometric data for the scales of the NHP for people over 60 years .
The validity of the NHP was evaluated with two measures for subjective body complaints and somatoform disorders. The Giessen Subjective Complaints List (GBB-24) by Brähler and Scheer [3] is an instrument to measure body complaints. It consists of 24 items. A set of 6 items each constitutes four factor-analytically derived scales: exhaustion, stomach complaints, limb complaints and heart complaints. Furthermore, the scores of the 24 single complaints are summed up to a total score ("complaints load"). The intensity of each complaint has to be rated according to a five point scale, ranging from 0 ("not existing") to 4 ("strong"); i.e. a higher score reflecting a higher degree of body complaint. Somatoform disorders were assessed by means of the Screening for Somatoform Disturbances (SOMS) by Rief, Hiller & Heuser [2], which is also a self-assessment method. This questionnaire lists all body symptoms relevant according to the classification and diagnostic systems DSM-IV and ICD-10 for both a somatization disorder and a somatoform autonomous function disorder. For the current study, a "complaint index of somatization" has been calculated, which consists of 47 sex-unspecific body complaints. A higher index score represents a higher degree of somatoform disorder.
Results
Reliability of the NHP in older people
Table 2 (Tab. 2) and 3(Tab. 3) show the item and scale coefficients of the NHP, respectively. The scales "pain", "physical mobility" and "emotional reaction" show a good internal consistency (.80≤α≤.85) and split half reliability (.77≤α≤.86). The corresponding results for "sleep" (α=.75, rtt=.77) and "energy loss" (α=.70, rtt=.71) can be regarded as sufficient, whereas the scale "social isolation" shows a relatively unsatisfactory reliability (α=.57; rtt=.55), suggesting to interpret this scale with caution.
Table 3. Psychometric data for the items of the NHP (German version) for people over 60 years.
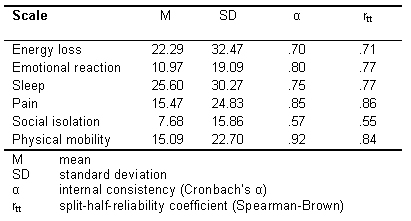
Scale inter-correlations are shown in Table 4 (Tab. 4).
Table 4. Intercorrelations of NHP scales.
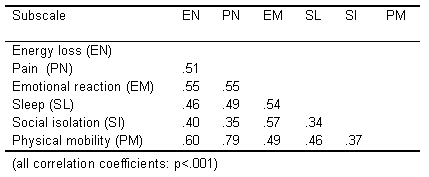
In general, medium size correlations appeared for the NHP scales. The highest inter-correlations were found between social isolation and emotional reactions and between energy loss and emotional reactions. Furthermore, positive correlations between energy loss, pain and physical mobility could be established.
Reference data for the NHP in subjects over 60 years
To test the assumption that subjective health differs between younger and older people, the scores of the subjects over 60 years were compared to those of the subjects aged 18-40 years and of the subjects aged 41-60 years, respectively. The results of these comparisons are shown in Table 5 (Tab. 5).
Table 5. Comparison of the NHP scores between age groups (18-40 years, 41-60 years, over 60 years).
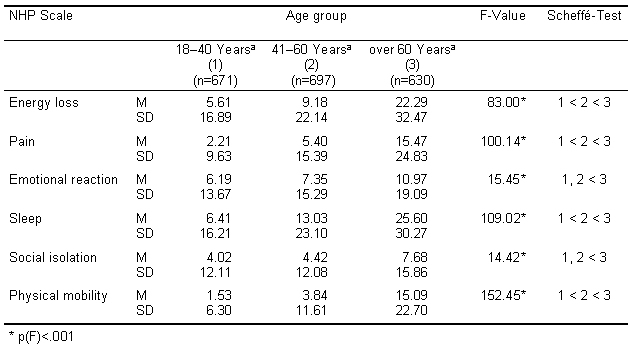
Our assumption of a decrease of subjective health with age, is confirmed for all scales. The results for the older people over 60 years of age differ in a highly significant way from the younger people (18-40 years and 41-60 years) as is evident from experienced energy loss, pain experience, negative emotional reactions, sleeping problems, social isolation and limitations of physical mobility. Moreover, when compared to their younger counterparts, the subjects aged 41 to 60 years already show a significant loss of subjectively experienced physical efficiency and mobility. For emotional reactions and social isolation, no difference occurred between these two age groups. Nonetheless, it is evident that there are age related limitations, especially in the area of functional capability.
Table 6 (Tab. 6) shows the NHP mean scores and the results of the two factor ANOVA for age and gender effects in the four age groups : 61-70 years , 71-75 years, 76-80 years and over 80 years.
Table 6. ANOVA results for the NHP scales with the factors age and gender for older people .
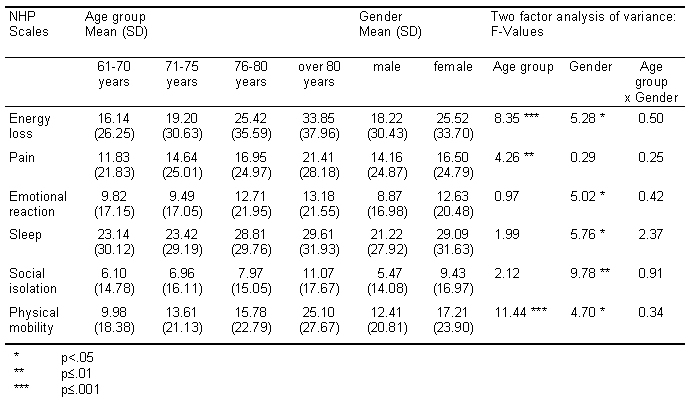
The ANOVA results confirm the relationship between age and decreasing physical efficiency (energy loss, physical mobility) and, to a lower extent, pain experience. However, there are no significant age effects concerning emotional or social aspects, nor do sleeping problems occur significantly more often in older age.
Gender has a very distinct effect on all scales with the exception of pain experience. Throughout the study, the assessment of older women yields more negative results than that of older men. These differences become highly significant on the scale "social isolation" (p≤.001), which could be explained by a higher proportion of widows among the women (48.4%) compared to men (18.3%).
Correlations with body complaints and somatoform symptoms
The scores of the NHP scales were correlated with those of the Giessen Subjective Complaints List (GBB) and the Screening for Somatoform Disorders (SOMS). This provided an opportunity to test how loss of functional capacity and mental and social deprivation are related to subjective body complaints. The results are shown in Table 7 (Tab. 7).
Table 7. Correlations between NHP scales, body complaints and somatoform symptoms.
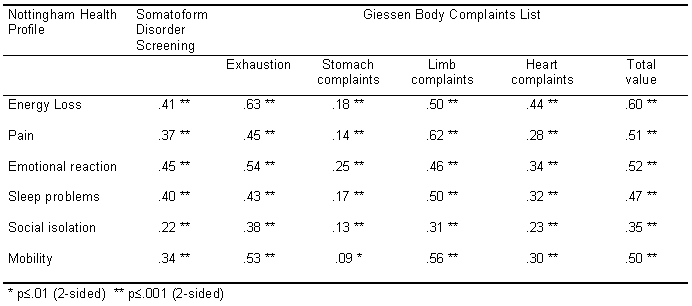
Overall, there were significant positive correlations between NHP scores and GBB scores and the somatization index regarding the physical dimensions of the NHP. This shows the validity of the NHP as a method for assessing the subjective evaluation of physical symptoms of older people as energy loss, pain and mobility. Significant correlations between body complaints and emotional reactions may reflect either the emotional reaction to physical decrease or the physical symptom of depressive complaints. However, the correlations were only of moderate magnitude, in particular in the case of somatization disorders.
Discussion
Subjective health, complementing objective medical data, is an important criterion for independent living and for the evaluation of the effects of geriatric therapy and rehabilitation. Appropriate procedures for the assessment of subjective perceptions of health are therefore necessary, especially in health-related research on older people, who are subject to increased chronic health limitations. The Nottingham Health Profile [1] is one of the most frequently used instruments in the area of subjective health in medical treatment. In particular, it seems to be appropriate for older people, because the items are short and easy to answer, and because the NHP covers areas of special importance to health limitations in older people, especially loss of energy, pain, sleeping disorders, social isolation, mobility and emotional states. However, there are nearly no age specific reference data for older people in Germany. Despite the lack of reference data for older people, the NHP is often used in gerontological and geriatric research. The current study presents results of a population survey, on which the NHP was evaluated in independent living older people from the non-clinical population.
The split-half-reliability and the internal consistency of the NHP-scales were satisfactory with exception of the social isolation subscale. This is consistent with findings of other studies that the psychometric quality of scales representing social isolation lacks sufficient precision [36]. The significant correlation coefficients of the NHP scales with subjective body complaints and somatoform disorders support the validity of the NHP for recording health-related limitations in older people.
There was a relatively high correlation between physical mobility and pain. This may be due to the fact that the pain-subscale reflects in particular limb complaints, as the pain-subscale of the NHP and the subscale "limb complaints" of the Giessen Subjective Complaints List [3] are highly inter-correlated. Furthermore, significant correlations could be found between emotional reactions, social isolation and energy loss, so that energy loss seems not only to be a consequence of physiological aging, but also a symptom of depressive complaints as a consequence of social isolation.
As was to be expected, older people, compared with those below 60 years of age, show an increased loss in subjective health. The largest differences are in those areas that deal with functional capacity in relation to the management of everyday life. This result supports the use of age specific reference data of the NHP. Reference data from younger people are not suitable to evaluate the health-related quality of the older people.
Significant age-specific differences in people over 60 years of age were found concerning energy loss, pain, and physical mobility. Therefore it may be supposed that limitations in subjective health are in particular experienced by older people when variations of physical capacity lead to limitations in everyday management. This area is highly significant for quality of life because the reduction of physical capability in old age is a general condition and is associated with the risk of losing independence. This result is confirmed by the study of Schneider et al. [19] who found that subjective health correlates to functional impairment in everyday life. No age-specific differences in the elderly above 60 years of age could be found for social isolation, sleeping disorders and emotional reactions. Following the concept of resilience [21], the low age-specific effects in the older people over 60 years of age may reflect the ability of older people to adjust emotionally to age-related changes of physical health status and social losses. Jang, Poon and Martin [18] found that individuals with advanced old age are more resilient to the effects of disabilities than the younger despite of higher levels of health problems. Because of their lifetime experiences of dealing with life events, the very old may be more able to cope with disease and functional decline [18], [39]. As Jang, Poon and Martin [18] suppose, compared to younger people the older people have different values and expectations regarding health because of the higher prevalence rates of health problems in age peers. Furthermore, by older people disease is considered more likely as a normative age-related change than as a health problem. Longitudinal studies would be necessary to further detect the conditions under which subjective ratings of health deteriorates and how a substantial proportion of older people is able to manage physical and functional decline and to preserve good subjective health.
There were gender differences in subjective health which showed women partly to be disadvantaged. The differences regarding energy loss and sleep might be explained by the fact that men who have survived into advanced age belong to a selected part of the population that has particularly good health, because they have lived beyond the statistical life expectancy for men ("surviving of the fittest"). Furthermore, older men of this age cohort usually have a higher educational level than women and more often live with a partner, whereas older women are more often widowed. The proportion of men who were married was 75.3% compared to only 35.3% of the women. These factors seem to be relevant for subjective health life ratings. Jang, Poon and Martin [18] found that there are more negative perceptions of health status in those individuals with higher age and fewer years of education, and in unmarried women.
With the exception of the subscale social isolation, which should be interpreted cautiously because of the relatively low internal consistency, the results of the current study show that the NHP is suitable for assessing subjective health in older people. This corresponds to the findings of McQueen, Long and Schurman [36]. According to McQueen, Long and Schurman [36] who evaluated the NHP in an English speaking, clinical population, the NHP should also be considered as a reliable, valid and useful alternative to the SF-36 in older people of the general population. Whereas the NHP cannot differentiate in the range of low and medium health-related complaints [37], in people over 60 years of age with an age-associated decline of physiological functioning the NHP may be recommended as a suitable instrument to assess subjective health. However, there are some limitations of the instrument that have to be held in mind. The concept of the NHP focuses on the negative aspects of subjective health, whereas positive aspects are underscored which are seen to be important in a holistic view on subjective health.
The availability of reference data specific to older people makes it possible to discover deviations from these norms when comparing subjective health of an older patient with that of older people from the general population. Even if age-specific and sex-specific reference data should be used because there were age-related and sex-related differences in subjective health in the present study, due to small sample sizes the reference data for the whole sample of the elderly over 60 years of age should be used temporarily. Further studies should follow to establish age-specific and sex-specific reference data for older people based on larger samples.
References
- 1.Hunt SM, McEwen J. The development of a subjective health indicator. Sociol Health Illn. 1980;2:231–246. doi: 10.1111/1467-9566.ep11340686. [DOI] [PubMed] [Google Scholar]
- 2.Rief W, Hiller W, Heuser J. Screening für Somatoforme Störungen [Screening for Somatoform Disorders] Göttingen, Bern: Testzentrale; 1997. [Google Scholar]
- 3.Brähler E, Scheer JW. Der Giessener Beschwerdebogen GBB. Testhandbuch [The Giessen Subjective Complaints List. Manual] Bern: Huber Verlag; 1995. [Google Scholar]
- 4.Metcalve D, et al. The measurements of outcomes in general practice. In: Stewart M, et al., editors. Tools for primary care research. Newbury Park, Londony: SAGE; 1992. pp. 14–27. [Google Scholar]
- 5.WHOQOL Group. Development of the WHOQOL: Rationale and current status. Int J Ment Health. 1994;23:24– 56. [Google Scholar]
- 6.Paterson DH, Stathokostas L. Physical activity, fitness, and gender in relation to morbidity, survival, quality of life, and independence in older age. In: Shepard RJ, editor. Gender, physical activity, and aging. Boca Raton: CRC Press; 2002. pp. 99–120. [Google Scholar]
- 7.Ahern FM, Gold CH, Heller DA, Dominick KL. Health-related quality of life among older adults with activity-limiting health conditions. J Ment Health Aging. 2003;9:43–53. [Google Scholar]
- 8.Cipher DJ, Clifford PA. Dementia, pain, depression, behavioural disturbances, and ADLs. Toward a comprehensive conceptualization of quality of life in long-term care. Int J Geriatr Psychiatry. 2004;19:741–748. doi: 10.1002/gps.1155. [DOI] [PubMed] [Google Scholar]
- 9.Gabriel Z, Bowling A. Quality of life from the perspectives of older people. Ageing Soc. 2004;24:675–691. [Google Scholar]
- 10.Baltes PB, Mayer KU. The Berlin Aging Study: Aging from 70 to 100. New York: Cambridge University Press; 2001. [Google Scholar]
- 11.Pinquart M. Correlates of subjective health in older adults: A meta-analysis. Psychol Aging. 2001;16:414–426. doi: 10.1037//0882-7974.16.3.414. [DOI] [PubMed] [Google Scholar]
- 12.Benjamin-Coleman R, Alexy B. Use of the SF-36 to identify community dwelling rural elderly at risk for hospitalization. Public Health Nurs. 1999;16:223–227. doi: 10.1046/j.1525-1446.1999.00223.x. [DOI] [PubMed] [Google Scholar]
- 13.Idler EL, Kasl S, Lemke J. Self-evaluated health and mortality among the elderly in New Haven, Connecticut, and Iowa and Washington counties, Iowa, 1982 - 1986. Am J Epidemiol. 1990;131:91–103. doi: 10.1093/oxfordjournals.aje.a115489. [DOI] [PubMed] [Google Scholar]
- 14.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 15.Helmer C, Barberger-Gateau P, Letenneur L, Dartigues JF. Subjective health and mortality in French elderly women and men. J Gerontol B Psychol Sci Soc Sci. 1999;54(2):S84–S92. doi: 10.1093/geronb/54b.2.s84. [DOI] [PubMed] [Google Scholar]
- 16.Nybo H, Petersen HC, Gaist D. Predictors of mortality in 2,249 Nonagenarians-the Danish 1905-cohort survey. J Am Geriatr Soc. 2003;51:1365–1373. doi: 10.1046/j.1532-5415.2003.51453.x. [DOI] [PubMed] [Google Scholar]
- 17.Baron-Epel O, Shemy G, Carmel S. Prediction of survival: a comparison between two subjective health measures in an elderly population. Soc Sci Med. 2004;58:2035–2043. doi: 10.1016/S0277-9536(03)00412-X. [DOI] [PubMed] [Google Scholar]
- 18.Jang Y, Poon LW, Martin P. Individual differences in the effects of disease and disability on depressive symptoms: The role of age and subjective health. Int J Aging Hum Dev. 2004;59:125–137. doi: 10.2190/RT1W-2HD7-KG5X-K1FB. [DOI] [PubMed] [Google Scholar]
- 19.Schneider G, Driesch G, Kruse A, Wachter M, Nehen HG, Heuft G. What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence. Arch Gerontol Geriatr. 2004;39:227–237. doi: 10.1016/j.archger.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Stewart AL, Hays RD, Ware JE. The MOS Short-Form General Health Survey: reliability and validity in a patient population. Med Care. 1988;26:724. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Staudinger UM, Marsiske M, Baltes PB. Resilience and reserve capacity in later adulthood: Potentials and limits of development across the life span. In: Cicchetti D, Cohen D, editors. Developmental psychopathology. Volume 2. New York: Wiley; 1995. pp. 801–847. [Google Scholar]
- 22.Williams JW, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, Cornell J, Sengupta A. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. J Am Med Assoc. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 23.Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA. Deterioration in quality of life following hip fracture: a prospective study. Osteoporos Int. 2000;11:460–466. doi: 10.1007/s001980070115. [DOI] [PubMed] [Google Scholar]
- 24.Pupello DF, Bessone LN, Lopez E, Brock JC, Alkire MJ, Izzo EG, Sanabria G, Sims DP, Ebra G. Long-term results of the bioprosthesis in elderly patients: impact on quality of life. Ann Thorac Surg. 2001:244–248. doi: 10.1016/s0003-4975(01)02515-2. [DOI] [PubMed] [Google Scholar]
- 25.Seymour DG, Ball AE, Russell EM, Primrose WR, Garratt AM, Crawford JR. Problems in using health survey questionnaires in older patients with physical disabilities. The reliability and validity of the SF-36 and the effect of cognitive impairment. J Eval Clin Pract. 2001;7:411–418. doi: 10.1046/j.1365-2753.2001.00296.x. [DOI] [PubMed] [Google Scholar]
- 26.Lyons RA, Perry HM, Littlepage BNC. Evidence for the validation of the Short-Form 36 Questionnaire (SF-36) in an elderly population. Age Ageing. 1994;23:182–184. doi: 10.1093/ageing/23.3.182. [DOI] [PubMed] [Google Scholar]
- 27.Jacoby F, Hoyer J, Wittchen HU. Seelische Gesundheit in Ost und West: Analysen auf der Grundlage des Bundesgesundheitssurveys [Mental health in eastern and western Germany: Analyzes of the German National Health Interview and Examination Survey] Z Klin Psychol Psychother. 2004;3:251–260. [Google Scholar]
- 28.Peek K, Ray L, Patel K, Stoebner-May D, et al. Reliability and validity of the SF-36 among older Mexican Americans. Gerontologist. 2004;44:418–425. doi: 10.1093/geront/44.3.418. [DOI] [PubMed] [Google Scholar]
- 29.Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY. Health-related quality of life in elderly patients with heart failure. Scand Cardiovasc J. 1999;33:278–285. doi: 10.1080/14017439950141524. [DOI] [PubMed] [Google Scholar]
- 30.Herlitz J, Wiklund I, Sjöland H, Karlson BW, Karlsson T, Haglid M, Hartford M, Caidahl K. Impact of age on improvement in health-related quality of life 5 years after coronary artery bypass grafting. Scand J Rehabil Med. 2000;32:41–48. doi: 10.1080/003655000750045730. [DOI] [PubMed] [Google Scholar]
- 31.Karlsen KH, Larsen JP, Tandberg E, Maeland JG. Influence of clinical and demographic variables on quality of life in patients with Parkinson disease. J Neurol Neurosurg Psychiatry. 1999;66:431–435. doi: 10.1136/jnnp.66.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bureau-Chalot F, Novella JL, Jolly D, Ankri J, Guillemin F, Blanchard F. Feasibility, acceptability and internal consistency reliability of the Nottingham Health Profile in dementia patients. Gerontology. 2002;48:220–225. doi: 10.1159/000058354. [DOI] [PubMed] [Google Scholar]
- 33.Van Balen R, Essink-Bot ML, Steyerberg E, Cools H, Habbema DF. Quality of life after hip fracture: a comparison of four health status measures in 208 patients. Disabil Rehabil. 2003;25:507–519. doi: 10.1080/0963828031000090443. [DOI] [PubMed] [Google Scholar]
- 34.Christensson L, Unossons M, Ek AC. Measurement of perceived health problems as a means of detecting elderly people at risk of malnutrition. J Nutr Health Aging. 2003;7:257–262. [PubMed] [Google Scholar]
- 35.Wouters-Wesseling W, Van Hooijdonk C, Wagenaar L, Bindels J, De Groot L, Van Staveren W. The effect of a liquid nutrition supplement on body composition and physical functioning in elderly people. Clin Nutr. 2003;22:371–377. doi: 10.1016/s0261-5614(03)00034-7. [DOI] [PubMed] [Google Scholar]
- 36.McQueen DA, Long MJ, Schurman JR., 2nd Selecting a subjective health status measure for optimum utility in everyday orthopaedic practice. J Eval Clin Pract. 2005;11:45–51. doi: 10.1111/j.1365-2753.2004.00493.x. [DOI] [PubMed] [Google Scholar]
- 37.Hinz A, Klaiberg A, Schumacher J, Brähler E. Zur psychometrischen Qualität des Lebensqualitäts-Fragebogens Nottingham Health Profile (NHP) in der Allgemeinbevölkerung [The psychometric properties of the Nottingham Health Profile [NHP] in the General Population] Psychother Psychosom Med Psychol. 2002;53:353–358. doi: 10.1055/s-2003-40948. [DOI] [PubMed] [Google Scholar]
- 38.Kohlmann T, Bullinger M, Kirchberger-Blumstein I. Die deutsche Version des Nottingham Health Profile (NHP). Übersetzungsmethodik und psychometrische Validierung [The German version of the Nottingham Health Profile [NHP]. Methodological issues of translation and psychometric validation] Soz Präventivmed. 1997;42:175–185. doi: 10.1007/BF01300568. [DOI] [PubMed] [Google Scholar]
- 39.Martin P, Rott C, Poon LW, Courtenay B, Lehr U. A molecular view of coping behavior in older adults. J Aging Health. 2001;13:72–91. doi: 10.1177/089826430101300104. [DOI] [PubMed] [Google Scholar]