Abstract
Background: While there is an increasing emphasis on patient empowerment and shared decision making, patients’ preferences for attributes associated with their treatment still need to be measured and considered. In the present study, patients' preferences regarding treatment of multiple myeloma (MM) were explored using direct assessment and a Discrete-Choice-Experiment (DCE).
Patients and methods: After reviewing the literature about preferences of myeloma patients we conducted a qualitative study with three focus groups consisting of six to eight MM-patients each. In order to achieve content validity, we aimed at collecting all relevant factors for an ideal MM-treatment. In a subsequent quantitative study phase, data was collected in an online or paper-pencil self-completed questionnaire. It included sociodemographic data, self-rated health (SF12v2 variation) and patients preferences of therapy characteristics using direct measurement (16 items on a five-point Likert-scale) as well as a Discrete-Choice-Experiment (DCE, eight pairs with eight characteristics).
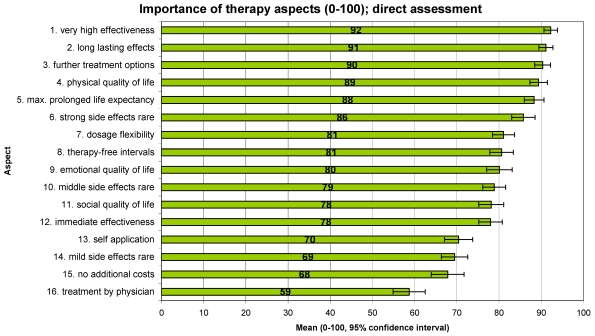
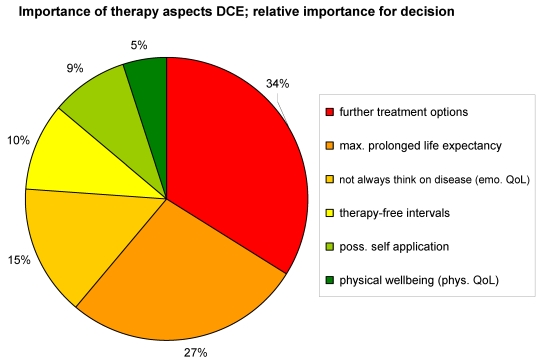
Results: 282 patients answered the questionnaire; 46% female, age: mean 62 yrs (SD=10 years), duration of MM: 5 yrs (SD=3.8 years). Direct measurement showed effectiveness aspects (i.e. high effectiveness, long lasting effects, max. prolonged life expectancy) and further treatment options in the first places, followed by maximal prolonged life expectancy, minor side effects and therapy-free-intervals. In the DCE, alternatives with further treatment options, longer life expectancy, "not always think of the disease" and therapy-free-intervals were more likely to be chosen, giving thus similar results.
Conclusion: Besides prolongation of life expectancy and effectiveness of treatment, further treatment options are of foremost importance to multiple myeloma patients. In addition, therapy-free intervals as well as an improved emotional quality of life (“Not always think of the disease”) are valued as very important.
The combination of direct assessment of importance and DCE is a valid combined survey technique for eliciting preferences of patients with multiple myeloma. The former ensures content validity (the possibility to measure a longer list of potentially important aspects), the latter has the advantage to combine positive and negative therapy characteristics and to avoid the problem of ceiling effects and “all-is-important” results.
Keywords: multiple myeloma, patient preference, Discrete-Choice-Experiment (DCE), direct assessment
Abstract
Hintergrund: Mit dem wachsenden Fokus auf die Beteilung von Patienten an Therapieentscheidungen im Sinne des „Shared decision making“ ist es wichtig, die Patientenpräferenzen hinsichtlich von Therapieeigenschaften zu erfassen und zu berücksichtigen. Ziel der vorliegenden Studie war es, mittels direkter Bewertung und Discrete-Choice-Experiments (DCE) diejenigen Parameter der Therapie zu erfassen, die Patienten mit Multiplem Myelom (MM) am wichtigsten sind.
Patienten und Methoden: Nach Durchsicht der relevanten Literatur führten wir eine qualitative Vorstudie auf Basis dreier Fokus-Gruppen mit jeweils sechs bis acht MM-Patienten durch. Um die Inhaltsvalidität des Fragebogens für die quantitative Hauptstudie abzusichern, zielten wir darauf ab, alle relevanten Faktoren einer idealen MM-Behandlung aus Patientensicht zu erfassen. Der Fragebogen (online sowie Papierversion) der Hauptstudie beinhaltete soziodemographische Angaben, Fragen zum Gesundheitszustand (SF12v2 SOEP Variante) und Fragen zur direkten Messung der Präferenzen (16 Items, fünfstufig Likert-skaliert) sowie ein Discrete-Choice-Experiment mit acht Paaren mit je acht Therapieeigenschaften.
Ergebnisse: Die Auswertung basiert auf 282 Patienten; 46% weiblich, Durchschnittsalter 62 Jahre (SD=10 Jahre), mittlere Erkrankungsdauer fünf Jahre (SD=3,8). In der direkten Präferenzabfrage erachteten die Befragten die Parameter Wirksamkeit und weitere Behandlungsoptionen als am wichtigsten, gefolgt von verlängerter Lebenserwartung, geringen Nebenwirkungen und therapiefreien Intervallen. Im DCE bevorzugten Patienten Behandlungsalternativen signifikant, die eine oder mehrere der folgenden Eigenschaften beinhalteten: weitere Behandlungsoptionen, verlängerte Lebensdauer, "nicht immer an die Krankheit denken müssen“ sowie therapiefreie Intervalle. Damit ergeben sich ähnliche Präferenzen wie in der direkten Messung.
Schlussfolgerung: Neben einer Verlängerung der Lebenserwartung und der Wirksamkeit der Behandlung ist es MM-Patienten besonders wichtig, dass eine Therapie weitere Behandlungsoptionen im Verlauf der Erkrankung offen hält. Darüber hinaus sind Therapiepausen und eine verbesserte emotionale Lebensqualität („Nicht immer an die Krankheit denken müssen“) von Bedeutung. Methodisch ist die Kombination der direkten Bewertung mit einer wahlbasierten Messung wie dem DCE für die Erhebung der Präferenzen von MM-Patienten bezüglich der Therapie nach unseren Ergebnissen sinnvoll und fruchtbar. Die direkte Methode kann mehr Aspekte berücksichtigen (Inhaltsvalidität), während das DCE durch Vorlage von Kombinationen positiver wie negativer Eigenschaften eine klarere Abstufung der Präferenzen erzeugt und Deckeneffekte sowie „alles-ist-wichtig“-Ergebnisse vermeidet.
Introduction
Multiple myeloma (MM) is a B-cell malignancy affecting immunoglobulin-producing plasma cells and accounts for approximately 15% of lymphato-hematopoietic cancers (LHC) [1]. The disease is a subtype of the heterogeneous group of lymphoma (ICD C.90). The major clinical features of this relatively rare cancer result from the abnormal accumulation of malignant plasma cells within the bone marrow and other tissues. Multiple myeloma primarily affects older adults with the median age at diagnosis of 65 years [2].
In the European Union, the incidence of multiple myeloma is 5.72 per 100,000 people, about 27,500 new patients develop the disease each year in Europe and 3500 in Germany [3]. Currently, around 70,000 patients are living with multiple myeloma in the European Union and 12,000 in Germany. Multiple myeloma is slightly more common in men than women [4].
Despite advances in systemic and supportive therapies, multiple myeloma has remained an incurable disease. The present study assesses the therapy-related expectations and perceptions of MM-patients. Contrary to clinical trials concerning mainly efficacy, the primary goal of this study was the comprehensive evaluation of preferably all relevant aspects of treatment quality from the patients’ perspective such as effectiveness, quality of life, further treatment options and therapy-free intervals. Secondary, we were interested how the study participants would judge the relevance of these criteria.
Methods
The study was divided into two parts:
a qualitative part to elicit and collect relevant attributes
a quantitative main study to assess the patients' preferences
Qualitative study
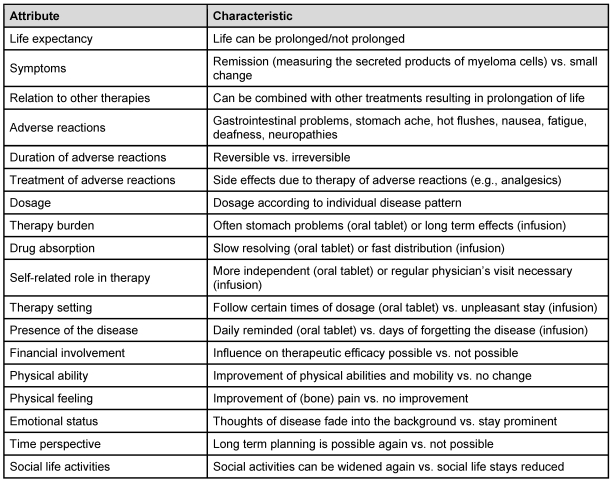
Prior to the main study, we performed a qualitative study to identify important aspects of an ideal multiple myeloma treatment. Patient advocacy groups „Arbeitsgemeinschaft Plasmozytom/Multiples Myelom (APMM)“ and „Deutsche Leukämie-Hilfe (DLH)“ asked patients to participate. They were interviewed in three focus groups (six to eight patients each). Study goals were explained to all participants and all gave written informed consent for their participation. On the basis of literature research and the results of these focus groups 18 MM-therapy aspects were selected for the main study (Table 1 (Tab. 1)). Using this material, we developed a questionnaire, which was administered to 25 patients in a pretest. Based on the results of the pretest we finalised the questionnaire.
Table 1. Items of patients' assessment.
Main study
The main study was performed as an anonymous survey from mid of May until end of July 2007 using either online or paper questionnaires. Patients were contacted either in writing and distributing the paper-based questionnaire version with stamped addressed envelopes, or via email/internet. Both methods were used since older patients might not want to use the online version. Patient advocacy groups helped in distributing paper-based questionnaires and the link to the online version among their regional affiliations. No personal data such as addresses, names or phone numbers were collected.
The questionnaire encompassed three main domains:
Part A: Sociodemographic characteristics: age, gender, educational level, household type (living alone or together with someone), duration of previous therapy, member of patient advocacy group (Table 2 (Tab. 2))
Part B: Current health status (Health related Quality of Life (QoL), SF12v2, German version of the SOEP, SozioOekonomisches Panel) [5], several questions concerning utilization of medical care (medical treatment in last three months, nights in hospital in last 12 months; Table 2 (Tab. 2))
Part C: assessment of importance of MM-therapy characteristics
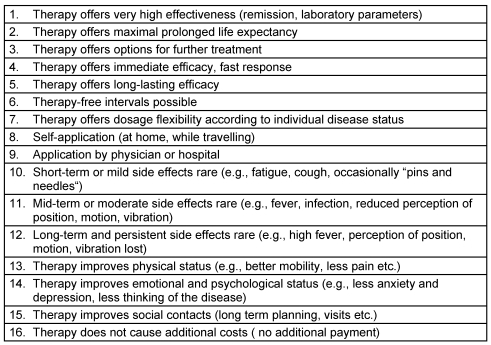
C1: Direct assessment of importance of 16 items (five-point Likert scale; Table 3 (Tab. 3))
Table 2. Patients characteristics (N=282).
Table 3. Direct assessment preferences/importance (5-point Likert-Scale, ranging from „very important“ (100 points) to „not important“ (0 points)). “How important do you consider (aspect)?” .
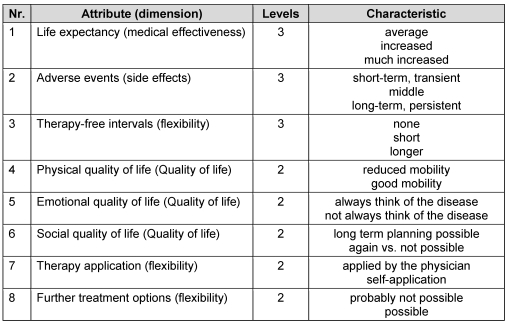
Table 4. Attributes (dimensions) and characteristics of the Discrete-Choice-Experiment (DCE).
Table 5. Example for Discrete-Choice-Experiment (DCE); pair comparison No. 3.
Discrete-Choice-Experiment (DCE)
Discrete-Choice-Experiments, also known as conjoint analysis [6], are an attribute-associated measure of benefit that is based on the assumptions that firstly, healthcare interventions, services, or policies can be described by their characteristics (or attributes) and secondly, an individuals’ valuation depends on the levels of these characteristics [7], [8]. In DCEs patients are asked several times to choose between the alternatives presented and described by their attributes; DCEs are therefore often called choice-based measures.
Since the questionnaire in this study was also distributed as a paper-based version, we conducted a relative simple DCE technique with eight pair decisions, each with eight attributes. Respondents had to choose eight times between alternative A or B. The attributes and their levels are given in Table 4 (Tab. 4), an example for a choice between two alternatives is given in Table 5 (Tab. 5).
Statistical analysis
For statistical data analysis, we used variance analysis, regression analysis, factor analysis, and random effect probit and logit models for the DCE. All statistical analyses were done by SPSS and STATA. The p-value <0.05 (two-sided) was considered as being statistically significant.
Results
Patients Characteristics (Part A)
Between May and June 2007, 282 patients completed the questionnaires. 54% answered via paper version and 46% online. We could not evaluate a participation rate, since the invitation to participation was widely spread via internet and email and therefore, the number of patients reached is unknown. 46% of the study participants were female, 54% male; the huge majority is living together with another person, only 16% live alone. Compared with external data from cancer registries, the patients in our study were younger: age at diagnosis (ICD: C.90) in registry Rhineland-Palatinate = 67 years (median) vs. first therapy in this study = 62 years (median) [9]. 16% of the patients were treatment-naive. Only patients, who previously had received treatment, answered the questions about therapy, use of health care system and preferences (N=238). Approximately 75% of the respondents were currently members of patient advocacy groups. Other baseline characteristics are listed in Table 2 (Tab. 2).
Self-rated health and use of health care (Part B)
As expected, the MM-patients report a health status (assessed with SF12 v2, SOEP version) that is distinctly below the general population. The mean value of 41.6 points (±8.6 standard deviation) for the physical health scale (which is a mean value of 0.84 standard deviations below the German average) lies farther below the norm value fixed at a mean of 50 points (SD=10) than the value for the mental health scale (mean 46.2 points, ±11.0 standard deviation) compared to 50 (SD=10) in the norm population. Nearly all respondents have seen a physician within the last three months (N=229 out of 230 valid answers). The average number of disease-related visits was 9.2 (approx. three visits/months; SD=14.2; range 0–150; median five visits). 60% of the study participants stayed at least one night in hospital during the last year (approx. 1.5 nights/month; SD=27.0, range 0–150; mean 19.3 nights, median eight nights).
Relevance of therapy characteristics: Direct assessment and DCE (Part C)
Preferences in the direct assessment (Part C1)
In part C1, respondents had to rate the importance of 16 therapy characteristics using a five-point Likert-Scale, ranging from “very important“ (100 points) to “not important“ (0 points) (Table 3 (Tab. 3)).
As demonstrated in Figure 1 (Fig. 1), all items concerning quality of treatment are of relatively high importance for the patients (given is the mean and the 95% confidence interval). This is not surprising, since only aspects were presented, that were rated as important according to the literature and the qualitative study/focus groups. The most relevant aspects have mean values ≥ 90 points.
Figure 1. Direct assessment: Importance of 16 therapy aspects (mean values; 95% CI).
Preferences in the Discrete-Choice-Experiment (DCE) (Part C2)
DCEs are limited to the use of only a few characteristics. It is very important to cover all the relevant fields when selecting the items for the DCE. From the literature review and the focus groups we learned that four major preference dimensions from myeloma patients' perspective are:
Medical effectiveness aspects (like prolonged life expectancy, effectiveness and long duration of effect)
Side effects
Quality of life (in the three subdimensions social, physical and emotional)
Flexibility in the sense of breaks in therapy and further treatment options
Upon this basis, we aggregated the patients’ preferences from part C1 into eight characteristics (as shown in Table 4 (Tab. 4) and Table 5 (Tab. 5)) trying to cover all relevant dimensions. 16 virtual therapies combining the eight characteristics were generated at random. These 16 therapies were then randomly combined to eight pairs with alternative A and B each. This approach created varying decision options: some choices were relatively simple because one alternative was in almost all aspects apparently better than the other. On the contrary, in difficult decisions the advantages and disadvantages were mostly equally distributed which made the alternatives more equivalent and the choice more difficult. As an example, Table 5 (Tab. 5) depicts pair 3 where advantages of alternative B in the attributes 1, 2 and 3 are facing disadvantages in the attributes 6 and 8; in the attributes 4, 5 and 7, both alternatives are equivalent (54% of patients chose alternative B, 46% alternative A).
The chosen attributes and their 2 or 3 levels were effect-coded for the overall analyses of all eight pair comparisons. In general, the level signing the positive pole of an attribute was coded positive (e.g. physical quality of life: positive pole characteristic “not limited“, negative pole “limited“). There was no a priori hypothesis concerning the evaluation of the poles at item 7 “Therapy applied by the physician or self-application”; here self-application was coded as plus, applied by the physician coded as minus.
In total, there were 1,797 valid observations. Some of the respondents did evaluate no or not all pairs. On average, out of 232 respondents who finished at least one pair comparison, 7.7 pairs were available (range 1–8).
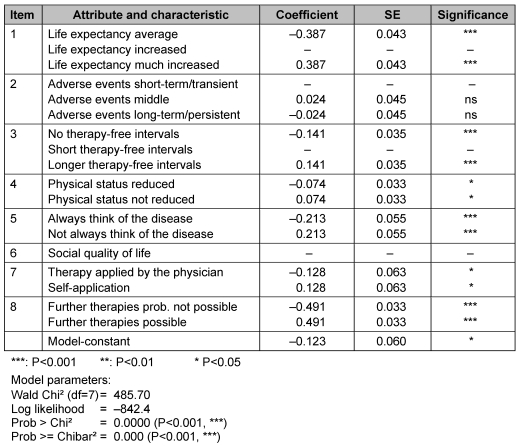
We created a random effects probit model which takes into account the partial dependency of observations from the same person concerning the parameter estimation (as shown in a highly significant chi bar test, this is advisable for our data).
For some levels and attributes the model does not give a valid estimator due to collinearity problems. This was true for the mid category of “Life expectancy” (item 1), the highest category of the parameter “Side effects“ (item 2), the mid category of the parameter “Therapy intervals“ as well as for the dichotomous attribute “Social quality of life” (item 6).
Asking for practicability approximately every 10th respondent rated the pair comparisons of the DCE as “very difficult“ to accomplish, 18% as “rather difficult“, 38% “partly difficult, partly not”, 28% “rather not difficult”, and 7% had no difficulties at all.
Estimated coefficients and their standard errors are shown in Table 6 (Tab. 6). All but one of the attributes were statistically significant predictors of the model of patient preference. The attribute “Further treatment options” (item 8) was the most important, closely followed by “maximal prolonged life expectancy” (item 1). Items of the psychological quality of life as “Not always think of the disease” (item 5) and “Therapy-free intervals possible” (item 3) were also relevant aspects for preferring a treatment. Less important but still statistically significant were the items “Self-application of the treatment” (item 7) and “Physical well-being” (item 4). Characteristics of side effects (item 2) did not play a significant role.
Table 6. Results of Discrete-Choice-Experiment (DCE) .
Based on the proportional distribution of the items’ importance, and distributing the preference scores to sum of a total of 100%, the relative importance of different treatment attributes is shown in Figure 2 (Fig. 2) (item 2 is omitted since not significant).
Figure 2. DCE: Importance of therapy aspects; relative importance for decision.
In additional evaluations, socio-demographic and structural parameters (age, gender, type of questionnaire) were analysed. They influenced the preferences only slightly. Therefore, the present model can be seen as a general preference model for patients with Multiple Myeloma independently from sociodemographic factors.
Discussion
The patients' view and desires in healthcare decisions (e.g. attributes of therapies) are often not sufficiently considered. However, in times of limited healthcare resources, shared decision making as patients involvement in treatment decisions have been encouraged in recent years. This requires an understanding of patients’ priorities concerning treatment decision making.
The present study collects and depicts the preferences of German MM-patients regarding their therapy. Based on a qualitative study to ensure content validity, a quantitative preference measurement was performed including a direct assessment and a choice-based measurement of patients’ preferences (DCE). This latter technique allows the estimation of the relative importance of different aspects of care and the trade-offs between these aspects, while the direct assessment allows the inclusion of more aspects. Hence, both methods should be used in a combined way.
For practicability DCE needs to be performed with preferably the least number of parameter and pairs. The level of complexity of our study turned out to manageable for the participants.
The study population comprised 282 myeloma patients, who completed paper-based and online-questionnaires. The intense usage of the paper version shows that offering the paper copy is important and useful – at least in this patient population.
Since the questionnaire was widely spread (paper and pencil version and online version) the number of patients got into contact with the questionnaire is unknown – therefore, response rates cannot be calculated. Study participants are probably more committed and well-informed than the average of MM-patients, because most of the respondents were therapy-experienced and members of patient advocacy groups. Furthermore study participants are younger than the average MM-patients in cancer registries. We do not know, if this selection could have potentially biased the preference assessments. However, the age of the patients was not associated with the preference-model in our study.
As expected, the health status of the respondents in the present trial was clearly under the average of the German general population. The analysis revealed the greatest differences concerning physical health aspects, the discrepancies regarding mental health factors were less pronounced. Obviously, patients with multiple myeloma feel particularly limited in their physical abilities.
In the direct measurement of preferences, the study participants prioritized 16 treatment aspects. Effectiveness aspects including duration of effect and further treatment options as “must haves” for registered compounds are ranked highest by the patients. Maximal prolonged life expectancy, minor side effects as well as therapy-free intervals were also very important. Social quality of life, cost aspects and the mode of application (by the physician or self-application) were less important.
In the simultaneous measurement of preferences (DCE; eight pairs with eight aspects) “further treatment options” ranked highest, followed by “maximal prolongation of life expectancy”. Provided that these two attributes were given, patients clearly preferred the respective alternatives. These findings are congruent with the direct preference evaluation, showing a high score for life expectancy and further treatment options.
Furthermore, a good emotional quality of life (“Not always think of the disease”) and intervals between the treatments – relieving the patients to some extent at least temporarily – were also relevant for the decision. Self-application of the treatment as well as physical quality of life had an additional but minor influence. In the DCE side effects did not reveal a significant impact and the attribute “Social quality of life” could not be estimated.
Except the low rating of the aspects “Physical quality of life” and “Side effects” in the DCE compared to the direct assessment, the results of the two techniques were widely congruent.
Conclusion
Besides prolongation of life expectancy and effectiveness of treatments, multiple myeloma patients are very concerned, that the chosen therapy does not affect further treatment options. In addition, therapy-free intervals as well as an improved emotional well-being are valued as very important, whereas no supplementary costs, treatment by physician and self-application were ranked comparatively low.
This study confirmed classical direct assessment of preferences as well as the DCE method as valid survey techniques for eliciting preferences of patients with multiple myeloma. Both methods should be used in a combined way, since the direct assessment is able to consider more potentially important aspects, and the DCE forces participants to rank these aspects in a complex decision, avoiding ceiling effects and “all-is-important” results.
Notes
Conflicts of interest
None declared.
Acknowledgments
Ortho Biotech, Division of Janssen-Cilag, Neuss, Germany supported this study financially.
The patient advocacy groups for MM Deutsche Leukämie- und Lymphom-Hilfe e.V. (DLH), Arbeitsgemeinschaft Plasmozytom/Multiples Myelom (APMM) supported the organisation of the qualitative and quantitative survey.
References
- 1.Deutsche Krebshilfe e.V. Plasmozytom/Multiples Myelom. Ein Ratgeber für Betroffene, Angehörige und Interessierte. Bonn: Deutsche Krebshilfe e.V.; 2005. [Google Scholar]
- 2.British Committe for Standardisation in Haematology. Guideline. Diagnosis and Management of Multiple Myeloma. Br J Haematol. 2001;115:522–540. doi: 10.1046/j.1365-2141.2001.03206.x. DOI: 10.1046/j.1365-2141.2001.03206.x. Available from: http://dx.doi.org/10.1046/j.1365-2141.2001.03206.x. [DOI] [PubMed] [Google Scholar]
- 3.Ferlay J, Bray F, Sankila R, Parkin DM. EUCAN: Cancer Incidence, Mortality and Prevalence in the European Union 1998, version 5.0. IARC CancerBase No.4. Lyon: IARCPress; 1999. [Last updated on 17/3/2003]. Limited version available from: http://www-dep.iarc.fr/eucan/eucan.htm. [Google Scholar]
- 4.Goldschmidt H. Multiples Myelom. Epidemiologie, Ätiologie und Pathogenese. Internist (Berl) 2006;47(2) [Google Scholar]
- 5.Nübling, M, Andersen H, Mühlbacher . Entwicklung eines Verfahrens zur Berechnung der körperlichen und psychischen Summenskalen auf Basis der SOEP - Version des SF 12 (Algorithmus). Data Documentation 16. Berlin: Deutsches Institut für Wirtschaftsforschung (DIW); 2006. Verfügbar unter: http://www.diw.de/deutsch/produkte/publikationen/datadoc/docs/diw_datadoc_2006-016.pdf. [Google Scholar]
- 6.Szeinbach S, Barnes J, McGhan W, et al. Using conjoint analysis to evaluate health state preferences. Drug Inf J. 1999;33:849–858. [Google Scholar]
- 7.Ryan M. Discrete choice experiments in health care. BMJ. 2004;328:360–361. doi: 10.1136/bmj.328.7436.360. DOI: 10.1136/bmj.328.7436.360. Available from: http://dx.doi.org/10.1136/bmj.328.7436.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan M, Farrar S. Eliciting preference for healthcare using conjoint analysis. BMJ. 2000;320:1530–1533. doi: 10.1136/bmj.320.7248.1530. DOI: 10.1136/bmj.320.7248.1530. Available from: http://dx.doi.org/10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidtmann I, Husmann G, Krtschil A. Krebs in Rheinland-Pfalz. Inzidenz und Mortalität im Jahr 2002. Bericht des Krebsregisters Rheinland-Plalz mit Schwerpunktauswertungen zum Malignen Melanom. Mainz: 2004. [Google Scholar]