Abstract
Recent advances in placebo research have demonstrated the mind’s power to alter physiology. In this study, we combined an expectancy manipulation model with both verum and sham acupuncture treatments to address: 1) how and to what extent treatment and expectancy effects --including both subjective pain intensity levels (pain sensory ratings) and objective physiological activations (fMRI) -- interact; and 2) if the underlying mechanism of expectancy remains the same whether placebo treatment is given alone or in conjunction with active treatment. The results indicate that although verum acupuncture + high expectation and sham acupuncture + high expectation induced subjective reports of analgesia of equal magnitude, fMRI analysis showed that verum acupuncture produced greater fMRI signal decrease in pain related brain regions during application of calibrated heat pain stimuli on the right arm. We believe our study provides brain imaging evidence for the existence of different mechanisms underlying acupuncture analgesia and expectancy evoked placebo analgesia. Our results also suggest that the brain network involved in expectancy may vary under different treatment situations (verum and sham acupuncture treatment).
Keywords: acupuncture, acupuncture analgesia, placebo, placebo analgesia, expectancy, expectancy manipulation, conditioning, pain, sham acupuncture needle
Introduction
Embedded in biomedical science are many sets of related dichotomies: body or mind, objective or subjective, biology or belief, specific or non-specific, and pharmacology or placebo (Kirmayer, 1988). In treatment, these effects are generally considered additive (Kirsch, 2000; Kleijnen et al., 1994). In fact, the fundamental assumption of the randomized controlled trial is that a medication or procedure demonstrates efficacy by producing a statistically significant additive value above a placebo effect (Kaptchuk, 1998). Taking pain relief as an example, it is believed that analgesic treatments consist of two components: the treatment specific effect from the physical or pharmacological interventions, and the non-specific, or placebo, component. The latter is believed to be induced by the psychosocial context in which the treatment is given including expectations of therapeutic benefit (Colloca and Benedetti, 2005; Kleijnen et al., 1994).
Acupuncture has been studied in almost one thousand different randomized controlled trials (RCTs) (Ernst, 2006; Kaptchuk, 2000; Linde et al., 2001). The results of these trials have been contradictory or equivocal. In these trials, it is not uncommon for “placebo/sham acupuncture/minimal acupuncture” controls to induce positive therapeutic effects on the same order of magnitude as verum (genuine) acupuncture. In other studies, verum and sham groups often demonstrate superiority and clinical benefits over waiting list of conventional therapies controls (Brinkhaus et al., 2006; Haake et al., 2007; Kaptchuk, 2000,, 2002a; Leibing et al., 2002; Linde et al., 2005; Melchart et al., 2005).
Acupuncture RCTs also suggest that expectancy, a crucial component of placebo (Benedetti, 2008; Kirsch, 1985; Montgomery and Kirsch, 1997), plays an important role in acupuncture treatment efficacy (Kaptchuk, 2002b; Kaptchuk et al., 2006; Linde et al., 2007). Importantly, basic science research investigating acupuncture analgesia on experimental pain, (which has produced more consistently positive results for acupuncture than clinical trials), has implicated overlapping mechanisms involving endogenous opioids and CCK for example, in both acupuncture (Han, 2003; Mayer et al., 1977) and placebo analgesia (Benedetti et al., 1999; Levine et al., 1978). This information suggests that the clinical practice of acupuncture may utilize some of the same endogenous analgesic mechanisms elicited by placebo treatments. Taken together, these findings beg the question–do the same mechanisms underlie acupuncture and placebo analgesia?
In parallel, advances in brain imaging provide scientists with new tools for investigating the neurobiological mechanisms underlying both placebo/nocebo and acupuncture treatment. Studies in placebo and nocebo research have shown the dramatic power of the mind to alter physiology and underlying brain circuitry (Bingel et al., 2006; Colloca et al., 2008b; Craggs et al., 2007; Kong et al., 2008; Kong et al., 2006a; Lieberman et al., 2004; Petrovic et al., 2002; Price et al., 2007; Scott et al., 2007,, 2008; Wager et al., 2004; Wager et al., 2007; Zubieta et al., 2005). Investigations of acupuncture also demonstrate complicated brain networks involved in acupuncture stimulation (Dougherty et al., 2008; Fang et al., 2008; Fang et al., 2004; Hui et al., 2000; Hui et al., 2005; Kong et al., 2007b; Kong et al., 2007d; Kong et al., 2002; Li et al., 2004; Li et al., 2006; Napadow et al., 2007; Napadow et al., 2006; Napadow et al., 2004; Pariente et al., 2005; Wu et al., 1999; Wu et al., 2002; Yoo et al., 2004) and acupuncture analgesia (Zhang et al., 2003a; Zhang et al., 2003b). In contrast, little empirical work has directly examined the interactions between the physiological components of interventions and such non-specific factors as expectancy. For example, do acupuncture analgesia and placebo analgesia work through the same brain networks? Is the underlying mechanism of expectancy the same whether placebo treatment is given alone or in conjunction with active treatment?
One difficulty in studying placebo analgesia using healthy volunteers and experimentally-induced pain is that the placebo effects are fewer and smaller than those in genuine clinical pain studies (Beecher, 1959; Charron et al., 2006; Shapiro and Shapiro, 1997). In a previous study (Kong et al., 2006a), using a well-established expectancy/conditioning manipulation to increase expectation of analgesia, we found that placebo analgesia evoked by sham acupuncture, as indicated by subjective pain rating reductions, was significantly greater on placebo sites than on the control sites on the same right arm where subjects were not expecting an analgesic effect. The magnitude of this analgesia effect is comparable with the magnitude of the verum acupuncture analgesia effect observed in another study from our group (Kong et al., 2005).
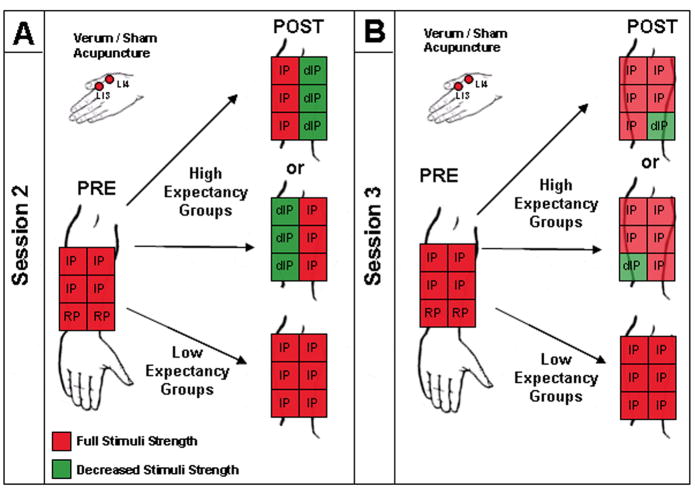
In this current study, we combined the same expectancy/conditioning manipulation model to investigate whether the patterns of neural activation underlying the modulation of pain perception by verum acupuncture analgesia and expectancy evoked placebo analgesia can be distinguished using fMRI. In this experiment, subjects were randomized into four groups, receiving verum or sham acupuncture paired with either high or low expectancy/conditioning manipulation. Then analgesic response to experimental heat pain applied on the right forearm was tested. In each group, we also included a within-subject control. Subjects were told that if they responded to the acupuncture treatment they would experience analgesia only on the treated side of their arm, but not on the untreated side of their arm (Figure 1). Forty-eight subjects (12 in each group) completed the experiment. In this manuscript, we present the data from two high expectancy groups (real and sham acupuncture) to investigate the underlying mechanisms of verum acupuncture and expectancy/conditioning induced placebo analgesia. Data from the low expectancy groups will be presented in a separate manuscript.
Figure 1. Details of experimental procedure.
In Session 2, we used a marker to draw a numbered 2 × 3 grid on the medial aspect of the right forearm and placed the thermal probe in one box of the grid for each of the stimulus sequences (e.g. random pain (RP) and identical sequence (IP)). After treatment in high expectancy groups, decreased stimulus temperatures (dIP) indicated by green color were applied on the meridian side (HE side), but not on the non-meridian side (Control side) to give each subject an unmistakable experience of analgesia. After treatment in low expectancy groups, the same temperature pre-treatment IP stimuli were applied. In Session 3, subjects were told that Session 2 procedures would be repeated during the fMRI scan. However, only one dIP was decreased (green color) on the HE side in high expectancy groups. The other spots were delivered at original temperatures on the remaining regions of the forearm, thus the pre-post treatment contrast is a subtraction of identical stimuli. The pre- and post- treatment pain rating and fMRI signal change differences between the HE and Control sides were the primary outcomes of this study.
Material and Methods
Subjects
Seventy-seven healthy, right-handed subjects enrolled in this experiment, which was said to be a study of acupuncture analgesia. All subjects were naive to acupuncture. Experiments were conducted with the written consent of each subject and approval by the Massachusetts General Hospital’s Institutional Review Board. All subjects were debriefed at the end of the experiment.
Procedures for the Delivery and Assessment of Noxious Thermal Stimuli
Subjects were recruited to participate in two behavioral testing sessions and one fMRI scanning session. Each session was separated by a minimum of three days.
Calibrated thermal pain stimuli were delivered to the right medial aspect of the forearm using a TSA-2001 Thermal Sensory Analyzer with a 3 cm × 3 cm probe (Medoc Advanced Medical Systems, Rimat Yishai, Israel) running computerized visual analog scale software (COVAS). All stimuli were initiated from a baseline resting temperature of 32 °C and increased to a target temperature (determination of the target temperature is described below). Each stimulus was presented for 12 seconds, including a 2.5 second ramp up and ramp down, and the inter-stimulus interval ranged from 24–30 seconds.
Gracely Sensory and Affective scales (Gracely et al., 1978a; Gracely et al., 1978b) were used to measure subjective pain ratings. To ensure consistent pain administration, a 2×3 grid was drawn in marker along the palmar side of the forearm, with three boxes each on radial and ulnar sides. We placed the thermal probe in one box of the grid for each stimulus sequence (Figure 1).
Session 1
We used the first behavioral session to familiarize subjects with the rating scales and determine appropriate stimulus intensities using methods employed in our previous studies (Kong et al., 2008; Kong et al., 2006a; Kong et al., 2006b). In summary, temperatures eliciting subjective intensity ratings in the LOW pain range (~ 5; which indicates weak on the 0–20 Sensory Scale) and HIGH pain range (~ 15; strong) were selected for each individual using an ascending series of noxious stimuli (increasing by 1 °C per stimulus). We then applied a series of 8 noxious stimuli, 4 HIGH and 4 LOW pain stimuli, presented in random order, (Random Pain sequence indicated by the abbreviation RP) and a series of 6 identical HIGH pain noxious stimuli (Identical Pain sequence, indicated by IP) to the right arm. Temperatures were adjusted when necessary to ensure that each subject’s subjective ratings of HIGH and LOW remained in the desired range and the final temperature settings were used in the following sessions.
Session 2
We used Session 2 to manipulate subjects’ expectancy to acupuncture treatment using a method modified from previous studies (De Pascalis et al., 2002; Kong et al., 2006a; Montgomery and Kirsch, 1997; Price et al., 1999; Voudouris et al., 1990; Wager et al., 2004).
At the start of Session 2, subjects were randomized into one of four arms of a 2×2 factorial design: verum or sham acupuncture paired with either high or low expectation manipulation.
At the beginning of Session 2, subjects were told that responses to acupuncture can be variable and that a given subject’s response tends to remain consistent across sessions. Subjects then viewed a Traditional Chinese Medicine meridian diagram and were falsely told that, according to previous literature, acupuncture could only produce analgesia on the side of the arm where the meridian passed through but not on the other side of the arm. To balance the design, half the subjects were then shown accurate diagrams (real diagram) of the large intestine (LI) Meridian passing through the radial side of the right arm, while the other half viewed a modified diagram (fake diagram) showing the LI Meridian passing through the ulnar side of the arm. (For clarity, we use the terms meridian (real and fake) side and non-meridian (real and fake) side in the following.)
Next, RP sequences were administered to the bottom two boxes of the 2×3 grid and IP sequences were applied to the top four. To proceed in the study, subjects had to consistently rate the HIGH pain stimuli as being more painful (indicated by a high score on the Sensory scale) than the LOW pain stimuli when RP stimuli were applied to the right forearm. Additionally, subjects had to report approximately equivalent ratings (average pain rating difference less than 1.5) to IP stimuli on both the radial and ulnar sides of their arm.
Then, according to their randomization, subjects received either verum or sham electroacupuncture (see below). After treatment, subjects were told they would be receiving the same pre-treatment IP stimuli to test the analgesic effect of acupuncture. Subjects then completed an expectancy form indicating the maximum pain they had experienced during IP application and their expectations regarding how this pain level would change after receiving acupuncture treatment.
In actuality, we repeated pre-treatment IP sequences on both meridian and non-meridian sides only in low expectancy groups. In high expectancy groups, we surreptitiously decreased temperatures (delineated by decreased IP (dIP) on Figure 1) on the “meridian” side of the arm to elicit “faint to weak” (~5) ratings and give subjects an unmistakable experience of analgesia. On the “non-meridian” side, IP temperatures remained at pre-treatment HIGH levels to further impress the “good effect” of acupuncture treatment. Subjects once again completed the expectancy form at the end of this session.
Session 3
Session 3 was performed in the fMRI scanner and subjects were told that Session 2 procedures would be repeated. In actuality, the same Session 2 procedures were performed only for the low expectancy groups. For high expectancy groups, however, only one dIP was administered on the bottom of the meridian side of the right forearm arm to remind subjects’ of the analgesia they experienced in Session 2. Noxious stimuli for the remaining other 5 boxes, (top four boxes and one bottom box on the non-meridian side that received RP before treatment) were all delivered at the original IP.
The differences between pre- and post-treatment pain ratings and brain activation during these final IP sequences on the top four boxes were the primary outcomes of this study.
Additionally, at the beginning of Session 3 and after the expectancy boost (reminder), subjects were again required to complete the expectancy forms.
During the scanning of pain sequences, subjects were instructed to focus on a small black fixation cross in the center of a screen in front of them. The cross turned red to cue the onset and duration of each stimulus (12 seconds) and after a delay of 4, 6, or 8 seconds, turned black again. Next, the Sensory Box Scale was displayed on the screen for 8 seconds and subjects used a pointer to indicate their subjective ratings.
Acupuncture administration
Identical verum or sham acupuncture was performed at Large Intestine 3 and 4 (LI 3 & 4) on the right hand by a licensed acupuncturist in Sessions 2 and 3.
For verum electroacupuncture, needles were inserted into the skin about 1.5 cm and adjusted until subjective deqi (Kong et al., 2007b), but no sharp pain, was evoked. Needles were then connected to an electro acupuncture device passing a 2 Hz current (OMS Medical Supplies IC-1107) (Kong et al., 2005); the intensity was gradually increased to the highest level subjects could tolerate without the sensation of sharp pain.
For sham electroacupuncture, specially-designed Streiberger sham acupuncture needles were placed on the surface of the skin and connected to a de-activated electroacupuncture device. The Streiberger needle has been validated and used in many studies (Kleinhenz et al., 1999; Kong et al., 2005; Kong et al., 2006a; McManus et al., 2007; Streitberger and Kleinhenz, 1998; White et al., 2003)
In total, verum or sham acupuncture treatment lasted approximately 25 minutes. Verum treatments were further broken down into three 6.5-minute (current ON), 1.5-minute (current OFF) blocks. After treatment, sensations evoked by verum and sham acupuncture were measured with the MGH (Massachusetts General Hospital) Acupuncture Sensation Scale (MASS), a rubric created by acupuncture researchers at MGH (Kong et al., 2005; Kong et al., 2007a; Kong et al., 2007b).
Behavioral Data Analysis
This manuscript focuses on the interaction between expectancy for pain relief and treatment mode (verum and sham acupuncture), using data from the two high expectancy groups, including the within-subject control (“non-meridian” side). Data from the two low expectancy groups, for which we believe that nocebo effects may be involved, (Benedetti et al., 1997; Benedetti et al., 2006; Colloca et al., 2008a; Kong et al., 2008) will be reported in a future paper. In the two high expectancy groups, meridian sides are always manipulated to make subjects expect acupuncture analgesia, and so we refer to the meridian side (real or fake) as the High Expectancy (HE) side. Because subjects were told acupuncture would not produce any effects on the non-meridian side, we refer to this side as the Control side.
To test the main effect of treatment mode and expectancy level, a mixed-model ANOVA was performed on pre- and post- treatment subjective pain sensory rating differences across the two groups (verum and sham groups) and two sides of the arm (HE and Control side). To test the influence of expectancy on acupuncture analgesia, we used a t-test to compare HE pre- and post-treatment subjective pain ratings between real and sham acupuncture groups. To test expectancy under verum and sham treatment conditions, we compared HE and Control sides across treatment group.
fMRI Data Acquisition and Analysis
Brain imaging was performed with a 3-axis gradient head coil in a 3 Tesla Siemens MRI System equipped for echo planar imaging (At the midpoint of the study, an MRI scanner upgrade replaced the 3 Tesla head-only Siemens Allegra MRI System with a 3 Tesla whole-body Siemens TIM Trio MRI System, but scanning parameters remained consistent across the two systems. Comparable numbers of subjects from each group were distributed across the two scanner systems: 7–8 subjects per group were tested on the old scanner, 5–6 subjects per group were tested on the new scanner.)
Thirty axial slices (4 mm thick with 1 mm skip) parallel to the anterior and posterior commissure covering the whole brain were imaged with 2000 ms TR, 40 ms TE, 90° flip angle and 3.13 × 3.13 mm in-plane spatial resolution. A high-resolution 3D MPRAGE sequence for anatomic localization was also collected.
Pre-processing and statistical analysis were performed using SPM2 software (Wellcome Department of Cognitive Neurology). Pre-processing included motion correction, normalization to the MNI stereotactic space, and spatial smoothing with an 8 mm Gaussian kernel. Then, for each individual, the HIGH pain minus LOW pain in RP sequence, and the fMRI signal difference between pre- and post-treatment (pre- minus post-treatment) during IP administration on the HE side and Control side was calculated for each subject using a general linear model (GLM). Low-frequency noise was removed with a high-pass filter applied with default values (128s) to the fMRI time series at each voxel.
Group analysis was performed using a random-effects model. We first compared all pre-treatment HIGH pain with LOW pain on both HE and Control sides when the RP were applied as outlined previously (Kong et al., 2006a; Wager et al., 2004). This yielded a mask of pain-intensity associated brain regions with which we could test for the acupuncture and placebo effects in the following analysis. According to previous imaging studies on placebo analgesia and pain modulation (Benedetti et al., 2005; Kong et al., 2006a; Kong et al., 2007c; Petrovic and Ingvar, 2002; Wager et al., 2004), brain regions such as rostral ACC (rACC), dorsal lateral prefrontal cortex (DLPFC) and orbital prefrontal cortex (OPFC) play an important role in pain modulation. We added these to our a priori regions of interest (ROIs).
Similar to the behavioral analysis, to investigate the effects produced by treatment modes (verum and sham acupuncture) and expectancy-related brain regions, we performed the following calculations with and without the mask described above, by: 1) comparing pre- and post-treatment fMRI signal change (pre- minus post-treatment) differences between verum and sham acupuncture groups on HE and Control sides separately using a t-test; 2) comparing pre-and post- fMRI signal change differences between the HE and Control sides within the same groups with a paired t-test.
Finally, the interaction between treatment modes (verum vs sham) and expectancy level (HE vs Control sides) was estimated. This interaction was calculated by comparing fMRI signal changes during the pain administration between verum acupuncture on HE side and sham acupuncture on the Control side, and verum acupuncture on the Control side and placebo on the HE side.
The threshold of activation within the mask (pre-treatment HIGH pain > LOW pain) and the pre-defined ROIs (rACC, DLPFC and orbital prefrontal cortex) were set at voxel-wise p<0.005 uncorrected with 20 contiguous voxels. A threshold of voxel-wise p<0.001 uncorrected with 20 contiguous voxels and cluster p<0.05 corrected was used to detect activation in other regions.
Results
Subjects
Forty-eight of seventy-seven consenting volunteers completed the study and were used for data analysis (average age 26.4 ± 4.9; 24 males). Twelve subjects did not fit the criteria for continued inclusion in the study (average ratings for HIGH pain were not greater than average ratings for LOW pain, or IP ratings on the radial and ulnar sides of their right arm were not approximately equivalent), eleven voluntarily withdrew, two could not tolerate the heat pain in Session 1, one could not tolerate electroacupuncture, and one could not tolerate the scanning session. Data from two subjects completing the study was also excluded because of poor quality (head movement within each functional run exceeded 2 mm). Again, in this manuscript, only the data from two groups, HIGH expectancy with verum or sham acupuncture (each with 12 subjects, balanced for male and female), are presented.
Subjective Ratings of Pain and Expectancy
The average rating for the pain
We used Session 3 pre- and post- treatment pain sensory intensity rating differences in response to administration of the IP sequence to test our hypothesis. Table 1 presents subjects’ pre- and post-treatment IP ratings on the HE and Control sides across the two groups. A mixed-model ANOVA showed a significant main effect for side, F (1, 22) = 19.04, p = .0002, with more pain reduction reported for the HE side than the Control side. The effect of real versus sham acupuncture was not significant, F (1, 22) = 1.52, p = 0.23, nor was the interaction, F (1, 22) = 0.002, p = 0.97.
Table 1.
Average pain sensory ratings of IP stimuli on HE side and Control side in Session 3 for the verum (VH) and sham placebo (PH) high expectancy groups (mean ± SE).
| VH | PH | |||
|---|---|---|---|---|
| HE | CONTROL | HE | CONTROL | |
| Pre | 13.8±0.7 | 13.8±0.7 | 13.4±0.7 | 13.1±0.8 |
| Post | 12.3±0.8 | 14.2±0.5 | 12.6±0.9 | 14.0±0.6 |
| Difference | 1.5±0.7 | −0.4±0.3 | 0.9±0.5 | −1.0±0.2 |
Paired t-tests on the pre- and post-treatment pain rating changes on the HE and Control sides within each group indicated that there was a significant pain rating reduction in both verum and sham groups (p < 0.011 in verum acupuncture group; and p < 0.007 in sham acupuncture group) (Figure 2). Two sample t-tests comparing the pre- and post-treatment pain rating changes on HE side and Control side between the two groups showed that there was no significant difference (p = 0.5 on HE side, p = 0.1 on control side) due to treatment group.
Figure 2.
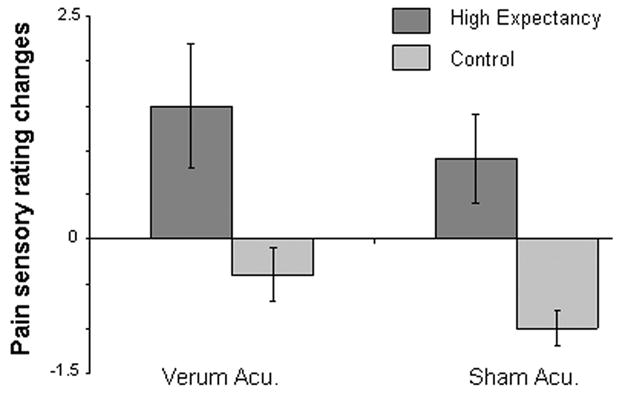
Subjective sensory pain rating changes (Pre–Post) on high expectancy side (HE) and Control side in verum and placebo acupuncture groups.
In Sessions 2 and 3, subjects were periodically asked to rate the highest pain level they had experienced during the IP sequences and then predict how intense this pain would be after acupuncture treatment. The difference between these two ratings, reported in Table 2, comprised subjects’ expectancy of pain relief. Overall, there were no significant expectancy differences between the two groups at the beginning of Session 2. At the end of Session 2, subjects in both high expectancy groups indicated significantly greater levels of expected pain relief than before manipulation, and this was maintained for the remainder of the experiment.
Table 2.
Subjects’ expected pain reduction in Session 2 and Session 3 for the verum (VH) and sham placebo (PH) high expectancy groups (n=12 in each group, mean ± SE).
| Expectancy | VH | PH |
|---|---|---|
| Session 2 pre-treatment | 3.3±0.5 | 5.1±0.7 |
| Session 2 post-treatment | 9.8±1.4 | 9.1±1.3 |
| Session 3 pre-treatment | 10.1±1.5 | 7.7±1.1 |
| Session 3 post-expectancy boost | 11.7±1.7 | 8.7±1.3 |
For the 24 subjects whose data are presented in this manuscript, the stimulus temperatures and the corresponding subjective sensory ratings (mean ± SD) were 48.1±1.1 °C and 14.5 ± 1.6 for HIGH pain; 45.1±1.6 °C and 5.0 ± 2.7 for LOW pain. As expected, temperature (p=5.5E-15) and pain intensity ratings (p = 1.4E-19) differ significantly between the two stimulus intensity levels. Two sample t-tests comparing the stimulus temperatures used to elicit HIGH and LOW pain showed there is no significant difference between the two groups (p = 0.3 for HIGH pain, and p = 0.95 for LOW pain). A Pearson correlation between the analgesia effect and temperatures used in verum and placebo group showed no significant correlations (p = 0.99 for verum acupuncture and p = 0.47 for sham acupuncture).
Subjective acupuncture sensation evoked by verum and sham acupuncture
Subjects in both groups endorsed multiple descriptors to characterize their experience of acupuncture. Results are shown in Table 3. Consistent with previous studies (Kong et al., 2005), average MASS ratings for all 12 descriptors showed subjects in the verum group experiencing significantly more intense sensations than subjects in the sham group (p < 0.002).
Table 3.
Average MASS ratings for the verum (VH) and sham placebo (PH) high expectancy groups (mean ± SE)
| Soreness | aching | deep-pressure | heaviness | fullness | tingling | numbness | dull-pain | sharp-pain | warm | cold | throbbing | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VH | 2.4±0.5 | 2.8±0.5 | 2.6±0.6 | 1.3±0.4 | 1.3±0.5 | 2.0±0.5 | 2.0±0.5 | 3.7±0.7 | 0.8±0.2 | 0.7±0.2 | 0.2±0.2 | 2.4±0.7 |
| PH | 0.4±0.2 | 0.1±0.1 | 0.5±0.4 | 1.3±0.7 | 1.2±0.6 | 1.3±0.4 | 1.3±0.6 | 0.1±0.1 | 0.1±0.1 | 0.3±0.3 | 0.2±0.2 | 0.0±0.0 |
fMRI Results
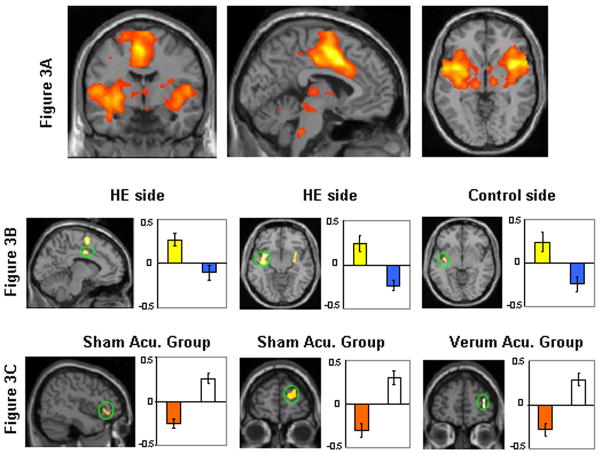
To elucidate the brain regions correlating with pain intensity and generate the mask of pain intensity used to measure the acupuncture and placebo effects, we first calculated a contrast between all pre-treatment HIGH and LOW pain (HIGH pain > LOW pain) when RP were applied pre-treatment in Session 3. The comparison yielded significant activations (voxel-wise p<0.001 corrected with 20 contiguous voxels) in the entire predicted network of pain intensity sensitive regions, including bilateral insular/opercular cortices/superior temporal gyrus, dorsal anterior cingulate cortex/medial prefrontal cortex (dACC/MPFC), secondary somatosensory cortex (SII), thalamus, putamen, periaquiductal grey (PAG), medulla, cerebellum, and left SI/M1 (contralateral) (Figure 2). These results are consistent with previous studies (Kong et al., 2006a; Kong et al., 2006b; Wager et al., 2004) and they comprised the mask for the following analysis.
Second, we compared pre- and post-treatment fMRI signal differences between verum acupuncture and sham acupuncture (verum > sham) on HE and Control sides separately (Table 4 and Figure 3B). The results showed that, for the comparison of verum > sham, on both HE side and Control side, verum acupuncture produced greater fMRI signal decreases than sham acupuncture in brain regions including left insula/putamen/claustrum/superior temporal gyrus and left inferior frontal gyrus; however, the fMRI signal decrease was even more extensive for stimuli delivered on HE side than Control side. Additional brain regions that exhibited significant fMRI signal decreases in response to stimuli delivered to the HE side include bilateral medial frontal gyrus, inferior parietal lobule, left dACC, rACC, and right inferior, middle and superior frontal gyrus. The only additional region that showed a differential fMRI decrease in response to stimuli delivered to the Control side after treatment was the left middle frontal gyrus. No brain regions were above the threshold when the opposite comparison (sham > verum) was performed.
Table 4.
Comparison results of fMRI signal change differences (pre-treatment pain > post-treatment pain) between HE side and Control side across the verum (Acu) and sham (Pla) treatment groups.
| Comparisons | Area (Brodmann Area) | Z score | Number of voxels in cluster | Peak coordinate (x,y,z) | ||
|---|---|---|---|---|---|---|
| Effect of treatment (HE side) | Left insula/putemen/claustrum/superior temporal gyrus (38) | 3.59 | 518 | −36 −8 −12 | ||
| Left medial frontal gyrus (6) | 3.4 | 105 | −80 58 | |||
| Left supramarginal gyrus (40) | 3.31 | 26 | −64 −50 26 | |||
| Right medial frontal gyrus (6) | 3.25 | 51 | 10 0 70 | |||
| Left dACC (24) | 3.19 | 33 | −8 −2 36 | |||
| Acu > Pla | ROI | Right putamen/claustrum/insula/superior temporal gyrus (38) | 3.14 | 160 | 28 6 −16 | |
| Right inferior parietal lobule (40) | 3.01 | 63 | 52 −36 28 | |||
| Right inferior frontal gyrus/insula (47) | 3.55 | 116 | 48 36 −2 | |||
| Right middle/superior frontal gyrus (6/8) | 3.52 | 130 | 18 18 58 | |||
| Left inferior frontal gyrus (47) | 3.11 | 25 | −50 28 −12 | |||
| Left medial frontal gyrus/rACC (10/32) | 2.85 | 20 | −12 60 8 | |||
| Others | No regions above threshold | |||||
| Pla > Acu | No regions above threshold | |||||
| Effect of treatment (Control side) | Left claustrum/insula | 3.56 | 27 | −28 −16 16 | ||
| Left superior temporal gyrus/insula (38) | 3.04 | 51 | −48 8 −16 | |||
| Acu > Pla | ROI | Left superior temporal gyrus/putamen/claustrum/insula (38) | 3.00 | 75 | −46−10−10 | |
| Left inferior frontal gyrus (47) | 3.26 | 28 | −42 32 0 | |||
| Left inferior frontal gyrus/insula (47) | 2.98 | 32 | −44 16 8 | |||
| Left middle frontal gyrus (46) | 2.98 | 33 | −24 36 26 | |||
| others | No regions above threshold | |||||
| Pla > Acu | No regions above threshold | |||||
| Effect of Expect. in VH group | HE > Con | ROI | Left M1 (4) | 2.88 | 79 | −26 −22 70 |
| others | No regions above threshold | |||||
| Con > HE | ROI | Right middle frontal gyrus (10) | 3.06 | 53 | 36 52 6 | |
| others | No regions above threshold | |||||
| Effect of Expect. in PH group | HE > Con | ROI | Left operculum | 2.97 | 21 | −58 −6 8 |
| Others | No regions above threshold | |||||
| Right inferior frontal gyrus (47)/insula | 3.29 | 63 | 32 18 −16 | |||
| Right inferior frontal gyrus (47)/insula | 3.78 | 64 | 50 34 −12 | |||
| Con > HE | ROI | Right superior frontal gyrus (8) | 3.55 | 124 | 34 32 54 | |
| Right inferior frontal gyrus (44) | 3.31 | 38 | 34 6 32 | |||
| Right superior frontal gyrus (10) | 3.16 | 75 | 24 62 22 | |||
| Right medial frontal gyrus (10) | 3.08 | 14 62 14 | ||||
| Others | No regions above threshold | |||||
| Interaction between treatment mode and expectancy level | ROI | Right superior frontal gyrus (8) | 3.56 | 82 | 16 34 54 | |
| Right inferior frontal gyrus (47) | 2.89 | 31 | 26 10 −16 | |||
| Others | No region above threshold | |||||
Note: VH indicates verum acupuncture with high expectancy, PH indicates sham acupuncture with high expectancy, HE side indicates meridian side where subjects were manipulated to expect good analgesia effect, Control side (Con) indicates non-meridian side where subjects were told acupuncture can not produce any effect. ROIs include the brain regions within the mask of HIGH pain > LOW pain and additional a priori regions in the DLPFC and OPFC and rACC/MPFC. Italics indicate regions within the HIGH pain minus LOW pain mask. The threshold is set to voxel-wise p<0.005 with 20 continuous voxels for predefined ROIs. The threshold for other regions (Others), were set to voxel-wise p<0.001 uncorrected with 20 contiguous voxels and cluster p<0.05 corrected for other regions. Peak coordinates refer to the MNI atlas.
Figure 3.
A) fMRI signal changes invoked by all RP pre-treatment HIGH pain stimuli minus all pre-treatment LOW pain stimuli. B) Representative brain regions showing significantly greater fMRI signal decrease after verum acupuncture treatment compared with sham acupuncture treatment (verum > sham). The bars indicate cluster beta values of pre- and post-treatment difference (pre- minus post-) in verum acupuncture group (yellow) and sham acupuncture group (blue) for both HE and Control sides (average ± SE). C) Representative regions showing significantly more brain activations on HE side compared with Control side after treatment in both sham and verum acupuncture groups. The bar indicates cluster beta values of pre- and post-treatment difference (pre- minus post-) on HE side (orange) and Control side (white).
The result of HE side and Control side comparisons within the verum acupuncture group and the sham acupuncture group are shown in Table 4 and Figure 3C. In the verum acupuncture group, identical noxious stimuli delivered to the HE side produced more signal decreases after treatment than those delivered to the Control side in M1, while noxious stimuli delivered to the Control side produced a greater signal decrease in right middle frontal gyrus than stimuli delivered to the HE side. For the sham acupuncture group, left operculum signal decrease was greater on the HE side than Control side, and right insula, inferior frontal gyrus, superior frontal gyrus and medial frontal gyrus signal decreases were greater on the Control side than HE side.
Further analysis of the interaction (e.g. HE side verum acupuncture and Control side placebo acupuncture (pre-post)–Control side verum acupuncture and HE side placebo acupuncture (pre-post)) showed significant fMRI signal change in right superior and inferior frontal gyrus.
Discussion
In this study, we combined an expectancy manipulation procedure with both verum and sham acupuncture to investigate the brain networks involved in acupuncture analgesia, expectancy/conditioning induced placebo analgesia and their interrelationship. Our results showed that, although acupuncture analgesia and placebo analgesia show comparable magnitudes of behavioral efficacy, each has a different pattern of associated brain activation. Our results show that relatively different brain networks can be involved in the expectancy effect in verum acupuncture as compared with sham acupuncture. For the verum acupuncture group, there were only a few small differences between the high expectancy side and control side. For the sham acupuncture group, however, a more complicated network, particularly involving a number of areas in the frontal gyrus, was significantly involved. These results suggest that expectancy may involve distinct mechanisms under different circumstances.
In this experiment, we found that the verum and sham acupuncture treatments yielded comparable magnitudes of reported analgesia. This finding is consistent with previous RCTs (Brinkhaus et al., 2006; Haake et al., 2007; Kaptchuk, 2000,, 2002a; Leibing et al., 2002; Linde et al., 2005; Melchart et al., 2005) reporting no significant differences between verum and sham acupuncture treatment, but significant positive clinical effects beyond no treatment controls.
To investigate the role of expectancy in acupuncture, Linde and colleagues (Linde et al., 2007) recently reviewed four acupuncture RCTs of 864 patients with migraine, tension-type headache, chronic low back pain, and knee osteoarthritis. Their results showed positive expectations and attitudes towards acupuncture treatment predicted positive outcomes independent of whether or not the treatments were real or sham. Consistent with this finding, we found that, even within the same verum acupuncture group on the same right forearm, if subjects were manipulated to expect that acupuncture could only work for him or her on a particular side of the arm (HE side) but not on the other side (Control side), verum acupuncture’s analgesia effect on reported pain rating changes could be significantly different, indicating the power of expectancy on acupuncture efficacy reports.
However, contrary to the behavioral subjective pain rating reports, fMRI analysis showed that, compared with sham treatment, verum acupuncture could significantly inhibit the brain response to calibrated pain stimuli, as indicated by fMRI signal decreases in left insula, putamen, and superior temporal gyrus, regardless of where the pain was applied (HE or Control side). This brain response reduction is consistent with the interpretation that acupuncture treatment suppresses pain perception not only by cognitive modulation but also by a more peripheral site of action involving inhibition of ascending nociceptive information (Han, 2003; Melzack, 1989; Pomeranz, 1997).
For instance, in a previous study, Zhang and colleagues (Zhang et al., 2003b) found that after 2 Hz electric acupoint stimulation (EAS), brain activation to calibrated cold pain was reduced in brain regions including contralateral SI, LPFC, and inferior temporal (BA20, 37) cortices; bilateral caudal ACC (BA24), parietal (BA7) cortex, medial cuneus, midbrain, pons, and cerebellum; and ipsilateral parietal (BA 39) cortex. In another study (Zhang et al., 2003a), this same group found that, after 2 Hz electrical acupoint stimulation, positive correlations could be observed in contralateral primary motor area, supplementary motor area, and ipsilateral superior temporal gyrus. Although the experimental paradigm and treatment modality of these studies are not exactly the same as ours, (for example, a differential use of superficial electric acupoint stimulation vs electroacupuncture stimulation with needle insertion), results are partly consistent.
More interestingly in this study, we also found that on the HE side, where subjects expected that acupuncture would produce an analgesic effect, more extensive fMRI signal decreases were observed in brain regions including right insula, putamen, claustrum and superior temporal gyrus, bilateral medial frontal gyrus, inferior parietal lobule, left dACC, and rACC when we compared the fMRI signal change differences between verum and sham acupuncture groups. This result suggests that expectancy is able to enhance acupuncture analgesia initiated by an inhibited brain response to calibrated pain stimuli. Given the roles of dACC in affective components of pain (Price, 2000) and rACC in emotional modulation (Bush et al., 2000; Vogt, 2005), we speculate that positive expectancy may enhance acupuncture analgesia efficacy through the emotional modulation pathway. We believe this is the first brain imaging study to elucidate the brain mechanisms behind how positive expectancy can influence the therapeutic effect of verum acupuncture treatment.
As another interesting finding, we observed that the brain network involved in expectancy modulation can vary under different situations. In the verum acupuncture group, when we compared the HE side with the Control side, only minimal differences were observed in left M1 (HE > Control) and right middle frontal gyrus (BA 10) (Control > HE). While in the sham acupuncture group, when we calculated the contrast of HE minus Control (HE > Control), significant fMRI signal changes were observed in in left operculum. The opposite comparison (Control > HE) showed fMRI signal change in right insula, right inferior frontal gyrus (BA 47, 44), medial frontal gyrus and superior frontal gyrus (BA 10). This result is partly consistent with our previous placebo analgesia study using a similar expectancy manipulation (we used RP in that study to test placebo analgesia while we use IP in this experiment), in which we found a greater fMRI signal increase in response to calibrated noxious stimuli after sham acupuncture treatment in brain regions such as anterior insula and dACC/medial frontal gyrus, lateral and orbital prefrontal cortex on HE side. It is also partly consistent with other studies (Price et al., 2007) that observed fMRI signal decreases after placebo treatment in brain regions such as bilateral insula/operculum.
A remaining question considers why different networks are involved when the same expectancy manipulation is used in different treatment groups. One speculation could contend that verum acupuncture treatment actually inhibits incoming noxious information similarly on HE and Control sides of the right forearm, thus ceiling effects denies sufficient room for an expectancy effect; while for the sham acupuncture group, more potential remains for expectancy effects. Another possibility suggested by prior research demonstrates that in different circumstances, variation between specific and non-specific effects can change (Kirsch, 2000; Kleijnen et al., 1994). This avenue of research has demonstrated that depending on environmental cues and the information/misinformation provided to subjects (expectancy), pharmacologically active substances such as buprenorphine, tramadol, ketorolac and metamizol (Amanzio et al., 2001), diazepam (Colloca et al., 2004), alcohol (McKay and Schare, 1999), caffeine (Flaten and Blumenthal, 1999; Kirsch and Rosadino, 1993), oxprenolol (Landauer and Pocock, 1984), tetrahydrocannabionol (Curran et al., 2002), nicotine (Perkins et al., 2003), cocaine (Muntaner et al., 1989), phenmetrazine (Penick and Hinkle, 1964), epinephrine (Penick and Fisher, 1965), amphetamine (Lyerly et al., 1964)--- or their matching placebo controls -- can have different objective and subjective effects, and that the pharmacological-placebo difference can shift indicating that pharmacological effects and their matching placebo effects interact with expectancy.
In this experiment, we have demonstrated different patterns of brain activation in response to calibrated noxious stimuli when a positive expectancy of analgesia is induced under different treatment circumstances, even when the subjective self-reported analgesia in the two conditions are comparable. We believe what we uniquely showed here is that equivalent subjective effects can be dissociated from objective functional neuroanatomical activations using brain imaging tools. To our knowledge our study is the first to examine the interaction of active treatment and expectancy on both subjective outcomes and objective neuroanatomical correlates and to show dissociation between the two effects.
A final question considers why we did not observe differences in reported pain rating between the two groups on either HE or Control sides, if verum acupuncture is supposed to inhibit incoming noxious stimulation information equally on both the HE and Control sides. Were subjects actually objectively experiencing less pain or merely reporting analgesia? We speculate some level of bias in subjective pain ratings to account for this outcome (Kong et al., 2007c; Montgomery and Kirsch, 1997; Price et al., 1999). From the point of view of cognitive neuroscience, subjective pain rating is a complicated decision making process, which can be significantly biased by previous experience and expectation (Mesulam, 1998; Miller and Cohen, 2001). For this reason, we believe as a more objective means to study a subjective phenomenon, brain imaging can enhance our understanding of pain and pain modulation processes.
It is worth noting that such dissociation between a subjective impression and independent corroboration has also been observed in other studies. Kelly and colleagues (Kelly et al., 2008) investigated the efficacy of a light therapy device intended to rejuvenate facial skin in 36 patients. They found that after an 8-week treatment as well as 1-month follow up, patients reported robust and statistically significant improvements in seven facial features. In sharp contrast, both the treating physician and blinded expert raters were unable to detect any improvement. Moreover, effect sizes were close to zero and in the opposite direction from improvement. Fregni and colleagues (Fregni et al., 2006) showed similar dissociation in a acute model of Parkinson’s disease when they gave 10 patients on three different occasions either levodopa, placebo pill or sham transcranial magnetic stimulation. On objective outcomes, only the levodopa group improved, but on subjective outcomes, patients in the two different controls reported improvement equal to the levodopa.
Also, one curious historical note might be in order, as our findings are consistent with a suggestion in the oldest canonical classic of Chinese medicine, the Yellow Emperor’s Inner Classic (Huang Di Nei Jing). Written in the first century BCE, the text states that “if a patient does not consent to therapy [acupuncture] with positive engagement, the physician should not proceed as the therapy will not succeed” (SuWen Chapter 11).
One potential limitation of our study is that the sham acupuncture used in this study could be regarded as another form of verum acupuncture. For instance, Japanese style acupuncture, as compared to Chinese style, tends to insert needles shallowly. Thus, our results may indicate a difference between acupuncture styles. In objection to this argument, we would argue that our sham acupuncture needle just touched, but did not penetrate into the skin, and did not involve any aspect of therapeutic contact. Previous studies indicate that connective tissue may play an important role in acupuncture treatment (Langevin et al., 2006a; Langevin et al., 2001; Langevin et al., 2002; Langevin et al., 2004; Langevin and Sherman, 2007; Langevin et al., 2006b); thus, our sham acupuncture that just touched the skin seems unlikely to produce the same effects of shallow needling. In addition, we did not manipulate the needles during the sham procedure. Thus, momentary sensation produced by sham acupuncture seems unlikely to explain analgesia effects comparable to verum acupuncture.
In summary, we found that, although acupuncture analgesia and expectancy induced placebo analgesia show comparable magnitudes of behavioral efficacy, each has a unique pattern of associated brain activation change. Objective fMRI signal changes show that expectancy can significantly enhance verum acupuncture’s analgesic effect, indicated by greater fMRI signal decrease compared with sham acupuncture. Also, the brain network involved in the expectancy can be different under different treatment conditions (verum vs sham). We believe our study provides the first brain imaging evidence on how expectancy can influence real (verum) acupuncture treatment and how different brain networks can be involved in this process.
Acknowledgments
This work was supported by PO1-AT002048 to Bruce Rosen from National Center for Complimentary and Alternative Medicine (NCCAM), R21AT00949 to Randy Gollub from NCCAM, KO1AT003883 to Jian Kong from NCCAM, K24AT004095 to Ted Kaptchuk from from NCCAM, M01-RR-01066 and UL1 RR025758-01 for Clinical Research Center Biomedical Imaging Core from National Center for Research Resources (NCRR), P41RR14075 for Center for Functional Neuroimaging Technologies from NCRR and the MIND Institute.
References
- Amanzio M, Pollo A, Maggi G, Benedetti F. Response variability to analgesics: a role for non-specific activation of endogenous opioids. Pain. 2001;90:205–215. doi: 10.1016/S0304-3959(00)00486-3. [DOI] [PubMed] [Google Scholar]
- Beecher HK. Measurement of Subjective Responses: Quantitative Effects of Drugs. Oxford, University Press; New York: 1959. [Google Scholar]
- Benedetti F. Mechanisms of placebo and placebo-related effects across diseases and treatments. Annu Rev Pharmacol Toxicol. 2008;48:33–60. doi: 10.1146/annurev.pharmtox.48.113006.094711. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Amanzio M, Casadio C, Oliaro A, Maggi G. Blockade of nocebo hyperalgesia by the cholecystokinin antagonist proglumide. Pain. 1997;71:135–140. doi: 10.1016/s0304-3959(97)03346-0. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Amanzio M, Vighetti S, Asteggiano G. The biochemical and neuroendocrine bases of the hyperalgesic nocebo effect. J Neurosci. 2006;26:12014–12022. doi: 10.1523/JNEUROSCI.2947-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedetti F, Arduino C, Amanzio M. Somatotopic activation of opioid systems by target-directed expectations of analgesia. J Neurosci. 1999;19:3639–3648. doi: 10.1523/JNEUROSCI.19-09-03639.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedetti F, Mayberg HS, Wager TD, Stohler CS, Zubieta JK. Neurobiological mechanisms of the placebo effect. J Neurosci. 2005;25:10390–10402. doi: 10.1523/JNEUROSCI.3458-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingel U, Lorenz J, Schoell E, Weiller C, Buchel C. Mechanisms of placebo analgesia: rACC recruitment of a subcortical antinociceptive network. Pain. 2006;120:8–15. doi: 10.1016/j.pain.2005.08.027. [DOI] [PubMed] [Google Scholar]
- Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, Irnich D, Walther HU, Melchart D, Willich SN. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4:215–222. doi: 10.1016/s1364-6613(00)01483-2. [DOI] [PubMed] [Google Scholar]
- Charron J, Rainville P, Marchand S. Direct comparison of placebo effects on clinical and experimental pain. Clin J Pain. 2006;22:204–211. doi: 10.1097/01.ajp.0000161526.25374.e5. [DOI] [PubMed] [Google Scholar]
- Colloca L, Benedetti F. Placebos and painkillers: is mind as real as matter? Nat Rev Neurosci. 2005;6:545–552. doi: 10.1038/nrn1705. [DOI] [PubMed] [Google Scholar]
- Colloca L, Lopiano L, Lanotte M, Benedetti F. Overt versus covert treatment for pain, anxiety, and Parkinson’s disease. Lancet Neurol. 2004;3:679–684. doi: 10.1016/S1474-4422(04)00908-1. [DOI] [PubMed] [Google Scholar]
- Colloca L, Sigaudo M, Benedetti F. The role of learning in nocebo and placebo effects. Pain. 2008a;136:211–218. doi: 10.1016/j.pain.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Colloca L, Tinazzi M, Recchia S, Le Pera D, Fiaschi A, Benedetti F, Valeriani M. Learning potentiates neurophysiological and behavioral placebo analgesic responses. Pain. 2008b;139:306–314. doi: 10.1016/j.pain.2008.04.021. [DOI] [PubMed] [Google Scholar]
- Craggs JG, Price DD, Verne GN, Perlstein WM, Robinson MM. Functional brain interactions that serve cognitive-affective processing during pain and placebo analgesia. Neuroimage. 2007;38:720–729. doi: 10.1016/j.neuroimage.2007.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran HV, Brignell C, Fletcher S, Middleton P, Henry J. Cognitive and subjective dose-response effects of acute oral Delta 9-tetrahydrocannabinol (THC) in infrequent cannabis users. Psychopharmacology (Berl) 2002;164:61–70. doi: 10.1007/s00213-002-1169-0. [DOI] [PubMed] [Google Scholar]
- De Pascalis V, Chiaradia C, Carotenuto E. The contribution of suggestibility and expectation to placebo analgesia phenomenon in an experimental setting. Pain. 2002;96:393–402. doi: 10.1016/S0304-3959(01)00485-7. [DOI] [PubMed] [Google Scholar]
- Dougherty DD, Kong J, Webb M, Bonab AA, Fischman AJ, Gollub RL. A combined [11C]diprenorphine PET study and fMRI study of acupuncture analgesia. Behav Brain Res. 2008;193:63–68. doi: 10.1016/j.bbr.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst E. Acupuncture--a critical analysis. J Intern Med. 2006;259:125–137. doi: 10.1111/j.1365-2796.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- Fang J, Jin Z, Wang Y, Li K, Kong J, Nixon EE, Zeng Y, Ren Y, Tong H, Wang Y, Wang P, Hui KK. The salient characteristics of the central effects of acupuncture needling: Limbic-paralimbic-neocortical network modulation. Hum Brain Mapp. 2008 doi: 10.1002/hbm.20583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang JL, Krings T, Weidemann J, Meister IG, Thron A. Functional MRI in healthy subjects during acupuncture: different effects of needle rotation in real and false acupoints. Neuroradiology. 2004;46:359–362. doi: 10.1007/s00234-003-1125-7. [DOI] [PubMed] [Google Scholar]
- Flaten MA, Blumenthal TD. Caffeine-associated stimuli elicit conditioned responses: an experimental model of the placebo effect. Psychopharmacology (Berl) 1999;145:105–112. doi: 10.1007/s002130051038. [DOI] [PubMed] [Google Scholar]
- Fregni F, Boggio PS, Bermpohl F, Maia F, Rigonatti SP, Barbosa ER, Pascual-Leone A. Immediate placebo effect in Parkinson’s disease--is the subjective relief accompanied by objective improvement? Eur Neurol. 2006;56:222–229. doi: 10.1159/000096490. [DOI] [PubMed] [Google Scholar]
- Gracely RH, McGrath PA, Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain. 1978a;5:5–18. doi: 10.1016/0304-3959(78)90020-9. [DOI] [PubMed] [Google Scholar]
- Gracely RH, McGrath PA, Dubner R. Validity and sensitivity of ratio scales of sensory and affective verbal pain descriptors: manipulation of affect by diazepam. Pain. 1978b;5:19–29. doi: 10.1016/0304-3959(78)90021-0. [DOI] [PubMed] [Google Scholar]
- Haake M, Muller HH, Schade-Brittinger C, Basler HD, Schafer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26:17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- Hui KK, Liu J, Makris N, Gollub RL, Chen AJ, Moore CI, Kennedy DN, Rosen BR, Kwong KK. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp. 2000;9:13–25. doi: 10.1002/(SICI)1097-0193(2000)9:1<13::AID-HBM2>3.0.CO;2-F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui KK, Liu J, Marina O, Napadow V, Haselgrove C, Kwong KK, Kennedy DN, Makris N. The integrated response of the human cerebro-cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. Neuroimage. 2005;27:479–496. doi: 10.1016/j.neuroimage.2005.04.037. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet. 1998;351:1722–1725. doi: 10.1016/S0140-6736(97)10111-8. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ. The Web That Has No Weaver: Understanding Chinese Medicine. Contemporary Books (McGraw-Hill); Chicago: 2000. [Google Scholar]
- Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002a;136:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. 2002b;136:817–825. doi: 10.7326/0003-4819-136-11-200206040-00011. [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ, Stason WB, Davis RB, Legedza AR, Schnyer RN, Kerr CE, Stone DA, Nam BH, Kirsch I, Goldman RH. Sham device v inert pill: randomised controlled trial of two placebo treatments. Bmj. 2006;332:391–397. doi: 10.1136/bmj.38726.603310.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JM, Boulos PR, Kaptchuk TJ, Rubin PAD. Mirror, mirror on the wall: Placebo effects that exist only in the eye of the beholder. Journal of Evaluation in Clinical Practice. 2008 doi: 10.1111/j.1365-2753.2008.00999.x. in press. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ. In: Mind and body as metaphors: hidden values in biomedicine. Lock M, Gordon D, editors. Biomedicine Examined Klumer Academic; Boston: 1988. [Google Scholar]
- Kirsch I. Response expectancy as a determinant of experience and behavior. Am Psychol. 1985;40:1189–1202. [Google Scholar]
- Kirsch I. Are drug and placebo effects in depression additive? Biol Psychiatry. 2000;47:733–735. doi: 10.1016/s0006-3223(00)00832-5. [DOI] [PubMed] [Google Scholar]
- Kirsch I, Rosadino MJ. Do double-blind studies with informed consent yield externally valid results? An empirical test. Psychopharmacology (Berl) 1993;110:437–442. doi: 10.1007/BF02244650. [DOI] [PubMed] [Google Scholar]
- Kleijnen J, de Craen AJ, van Everdingen J, Krol L. Placebo effect in double-blind clinical trials: a review of interactions with medications. Lancet. 1994;344:1347–1349. doi: 10.1016/s0140-6736(94)90699-8. [DOI] [PubMed] [Google Scholar]
- Kleinhenz J, Streitberger K, Windeler J, Gussbacher A, Mavridis G, Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- Kong J, Fufa DT, Gerber AJ, Rosman IS, Vangel MG, Gracely RH, Gollub RL. Psychophysical outcomes from a randomized pilot study of manual, electro, and sham acupuncture treatment on experimentally induced thermal pain. J Pain. 2005;6:55–64. doi: 10.1016/j.jpain.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, Vangel M, Rosen B, Kaptchuk TJ. Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med. 2007a;13:1059–1070. doi: 10.1089/acm.2007.0524. [DOI] [PubMed] [Google Scholar]
- Kong J, Gollub RL, Polich G, Kirsch I, Vangel MG, LaViolette P, Rosen BTJK. An fMRI study on the neural mechanisms of hyperalgesic nocebo effect. Journal of Neuroscience. 2008;28:13354–13362. doi: 10.1523/JNEUROSCI.2944-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Gollub RL, Rosman IS, Webb JM, Vangel MG, Kirsch I, Kaptchuk TJ. Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. J Neurosci. 2006a;26:381–388. doi: 10.1523/JNEUROSCI.3556-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Gollub RL, Webb JM, Kong JT, Vangel MG, Kwong K. Test-retest study of fMRI signal change evoked by electro-acupuncture stimulation. Neuroimage. 2007b:1171–1181. doi: 10.1016/j.neuroimage.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Kaptchuk TJ, Polich G, Kirsch I, Gollub RL. Placebo analgesia: findings from brain imaging studies and emerging hypotheses. Rev Neurosci. 2007c;18:173–190. doi: 10.1515/revneuro.2007.18.3-4.173. [DOI] [PubMed] [Google Scholar]
- Kong J, Kaptchuk TJ, Webb JM, Kong JT, Sasaki Y, Polich GR, Vangel MG, Kwong K, Rosen B, Gollub RL. Functional neuroanatomical investigation of vision-related acupuncture point specificity-A multisession fMRI study. Hum Brain Mapp. 2007d doi: 10.1002/hbm.20481. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J, Ma L, Gollub RL, Wei J, Yang X, Li D, Weng X, Jia F, Wang C, Li F, Li R, Zhuang D. A pilot study of functional magnetic resonance imaging of the brain during manual and electroacupuncture stimulation of acupuncture point (LI-4 Hegu) in normal subjects reveals differential brain activation between methods. J Altern Complement Med. 2002;8:411–419. doi: 10.1089/107555302760253603. [DOI] [PubMed] [Google Scholar]
- Kong J, White NS, Kwong KK, Vangel MG, Rosman IS, Gracely RH, Gollub RL. Using fMRI to dissociate sensory encoding from cognitive evaluation of heat pain intensity. Hum Brain Mapp. 2006b;27:715–721. doi: 10.1002/hbm.20213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landauer AA, Pocock DA. Stress reduction by oxprenolol and placebo: controlled investigation of the pharmacological and non-specific effects. Br Med J (Clin Res Ed) 1984;289:592. doi: 10.1136/bmj.289.6445.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langevin HM, Bouffard NA, Badger GJ, Churchill DL, Howe AK. Subcutaneous tissue fibroblast cytoskeletal remodeling induced by acupuncture: evidence for a mechanotransduction-based mechanism. J Cell Physiol. 2006a;207:767–774. doi: 10.1002/jcp.20623. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol. 2001;91:2471–2478. doi: 10.1152/jappl.2001.91.6.2471. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Churchill DL, Wu J, Badger GJ, Yandow JA, Fox JR, Krag MH. Evidence of connective tissue involvement in acupuncture. Faseb J. 2002;16:872–874. doi: 10.1096/fj.01-0925fje. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Konofagou EE, Badger GJ, Churchill DL, Fox JR, Ophir J, Garra BS. Tissue displacements during acupuncture using ultrasound elastography techniques. Ultrasound Med Biol. 2004;30:1173–1183. doi: 10.1016/j.ultrasmedbio.2004.07.010. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Sherman KJ. Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Med Hypotheses. 2007;68:74–80. doi: 10.1016/j.mehy.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Langevin HM, Storch KN, Cipolla MJ, White SL, Buttolph TR, Taatjes DJ. Fibroblast spreading induced by connective tissue stretch involves intracellular redistribution of alpha- and beta-actin. Histochem Cell Biol. 2006b;125:487–495. doi: 10.1007/s00418-005-0138-1. [DOI] [PubMed] [Google Scholar]
- Leibing E, Leonhardt U, Koster G, Goerlitz A, Rosenfeldt JA, Hilgers R, Ramadori G. Acupuncture treatment of chronic low-back pain -- a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002;96:189–196. doi: 10.1016/s0304-3959(01)00444-4. [DOI] [PubMed] [Google Scholar]
- Levine JD, Gordon NC, Fields HL. The mechanism of placebo analgesia. Lancet. 1978;2:654–657. doi: 10.1016/s0140-6736(78)92762-9. [DOI] [PubMed] [Google Scholar]
- Li G, Huang L, Cheung RT, Liu SR, Ma QY, Yang ES. Cortical activations upon stimulation of the sensorimotor-implicated acupoints. Magn Reson Imaging. 2004;22:639–644. doi: 10.1016/j.mri.2004.01.074. [DOI] [PubMed] [Google Scholar]
- Li G, Jack CR, Jr, Yang ES. An fMRI study of somatosensory-implicated acupuncture points in stable somatosensory stroke patients. J Magn Reson Imaging. 2006;24:1018–1024. doi: 10.1002/jmri.20702. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Jarcho JM, Berman S, Naliboff BD, Suyenobu BY, Mandelkern M, Mayer EA. The neural correlates of placebo effects: a disruption account. Neuroimage. 2004;22:447–455. doi: 10.1016/j.neuroimage.2004.01.037. [DOI] [PubMed] [Google Scholar]
- Linde K, Streng A, Jurgens S, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes MG, Weidenhammer W, Willich SN, Melchart D. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293:2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- Linde K, Vickers A, Hondras M, ter Riet G, Thormahlen J, Berman B, Melchart D. Systematic reviews of complementary therapies - an annotated bibliography. Part 1: acupuncture. BMC Complement Altern Med. 2001;1:3. doi: 10.1186/1472-6882-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, Willich SN, Melchart D. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- Lyerly SB, Ross S, Krugman AD, Clyde DJ. Drugs and Placebos: the Effects of Instructions Upon Performance and Mood under Amphetamine Sulphate and Chloral Hydrate. J Abnorm Psychol. 1964;68:321–327. doi: 10.1037/h0044351. [DOI] [PubMed] [Google Scholar]
- Mayer DJ, Prince DD, Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Research. 1977;121:368–372. doi: 10.1016/0006-8993(77)90161-5. [DOI] [PubMed] [Google Scholar]
- McKay D, Schare ML. The effects of alcohol and alcohol expectancies on subjective reports and physiological reactivity: a meta-analysis. Addict Behav. 1999;24:633–647. doi: 10.1016/s0306-4603(99)00021-0. [DOI] [PubMed] [Google Scholar]
- McManus CA, Schnyer RN, Kong J, Nguyen LT, Hyun Nam B, Goldman R, Stason WB, Kaptchuk TJ. Sham acupuncture devices - practical advice for researchers. Acupunct Med. 2007;25:36–40. doi: 10.1136/aim.25.1-2.36. [DOI] [PubMed] [Google Scholar]
- Melchart D, Streng A, Hoppe A, Brinkhaus B, Witt C, Wagenpfeil S, Pfaffenrath V, Hammes M, Hummelsberger J, Irnich D, Weidenhammer W, Willich SN, Linde K. Acupuncture in patients with tension-type headache: randomised controlled trial. Bmj. 2005;331:376–382. doi: 10.1136/bmj.38512.405440.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzack R. Folk medicine and the sensory modulation of pain. In: Wall PD, Melzack R, editors. Textbook of Pain. Churchill Livingstone; Edinburgh: 1989. pp. 1209–1223. [Google Scholar]
- Mesulam MM. From sensation to cognition. Brain. 1998;121:1013–1052. doi: 10.1093/brain/121.6.1013. [DOI] [PubMed] [Google Scholar]
- Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. 2001;24:167–202. doi: 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Kirsch I. Classical conditioning and the placebo effect. Pain. 1997;72:107–113. doi: 10.1016/s0304-3959(97)00016-x. [DOI] [PubMed] [Google Scholar]
- Muntaner C, Cascella NG, Kumor KM, Nagoshi C, Herning R, Jaffe J. Placebo responses to cocaine administration in humans: effects of prior administrations and verbal instructions. Psychopharmacology (Berl) 1989;99:282–286. doi: 10.1007/BF00442823. [DOI] [PubMed] [Google Scholar]
- Napadow V, Kettner N, Liu J, Li M, Kwong KK, Vangel M, Makris N, Audette J, Hui KK. Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome. Pain. 2007 doi: 10.1016/j.pain.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napadow V, Kettner N, Ryan A, Kwong KK, Audette J, Hui KK. Somatosensory cortical plasticity in carpal tunnel syndrome--a cross-sectional fMRI evaluation. Neuroimage. 2006;31:520–530. doi: 10.1016/j.neuroimage.2005.12.017. [DOI] [PubMed] [Google Scholar]
- Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp. 2004;24:193–205. doi: 10.1002/hbm.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25:1161–1167. doi: 10.1016/j.neuroimage.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Penick SB, Fisher S. Drug-Set Interaction: Psychological and Physiological Effects of Epinephrine under Differential Expectations. Psychosom Med. 1965;27:177–182. doi: 10.1097/00006842-196503000-00010. [DOI] [PubMed] [Google Scholar]
- Penick SB, Hinkle LE., Jr The Effect of Expectation on Response to Phenmetrazine. Psychosom Med. 1964;26:369–373. doi: 10.1097/00006842-196407000-00006. [DOI] [PubMed] [Google Scholar]
- Perkins K, Sayette M, Conklin C, Caggiula A. Placebo effects of tobacco smoking and other nicotine intake. Nicotine Tob Res. 2003;5:695–709. doi: 10.1080/1462220031000158636. [DOI] [PubMed] [Google Scholar]
- Petrovic P, Ingvar M. Imaging cognitive modulation of pain processing. Pain. 2002;95:1–5. doi: 10.1016/s0304-3959(01)00467-5. [DOI] [PubMed] [Google Scholar]
- Petrovic P, Kalso E, Petersson KM, Ingvar M. Placebo and opioid analgesia--imaging a shared neuronal network. Science. 2002;295:1737–1740. doi: 10.1126/science.1067176. [DOI] [PubMed] [Google Scholar]
- Pomeranz B. Scientific basis of acupuncture. In: Stux G, Pomeranz B, editors. Basics of Acupuncture. Springer; Berlin: 1997. pp. 6–72. [Google Scholar]
- Price DD. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–1772. doi: 10.1126/science.288.5472.1769. [DOI] [PubMed] [Google Scholar]
- Price DD, Craggs J, Verne GN, Perlstein WM, Robinson ME. Placebo analgesia is accompanied by large reductions in pain-related brain activity in irritable bowel syndrome patients. Pain. 2007;127:63–72. doi: 10.1016/j.pain.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147–156. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- Scott DJ, Stohler CS, Egnatuk CM, Wang H, Koeppe RA, Zubieta JK. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron. 2007;55:325–336. doi: 10.1016/j.neuron.2007.06.028. [DOI] [PubMed] [Google Scholar]
- Scott DJ, Stohler CS, Egnatuk CM, Wang H, Koeppe RA, Zubieta JK. Placebo and nocebo effects are defined by opposite opioid and dopaminergic responses. Arch Gen Psychiatry. 2008;65:220–231. doi: 10.1001/archgenpsychiatry.2007.34. [DOI] [PubMed] [Google Scholar]
- Shapiro AK, Shapiro E. The Powerful Placebo: From Ancient Priest to Modern Physician. The Johns Hopkins University Press; Baltimore: 1997. [PMC free article] [PubMed] [Google Scholar]
- Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- Vogt BA. Pain and emotion interactions in subregions of the cingulate gyrus. Nat Rev Neurosci. 2005;6:533–544. doi: 10.1038/nrn1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voudouris NJ, Peck CL, Coleman G. The role of conditioning and verbal expectancy in the placebo response. Pain. 1990;43:121–128. doi: 10.1016/0304-3959(90)90057-K. [DOI] [PubMed] [Google Scholar]
- Wager TD, Rilling JK, Smith EE, Sokolik A, Casey KL, Davidson RJ, Kosslyn SM, Rose RM, Cohen JD. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162–1167. doi: 10.1126/science.1093065. [DOI] [PubMed] [Google Scholar]
- Wager TD, Scott DJ, Zubieta JK. Placebo effects on human mu-opioid activity during pain. Proc Natl Acad Sci U S A. 2007;104:11056–11061. doi: 10.1073/pnas.0702413104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White P, Lewith G, Hopwood V, Prescott P. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over pilot trial. Pain. 2003;106:401–409. doi: 10.1016/j.pain.2003.08.013. [DOI] [PubMed] [Google Scholar]
- Wu MT, Hsieh JC, Xiong J, Yang PC, Pan HB, Chen YCI, Tsai G, Rosen BR, Kwong KK. Central nervous pathway for acupuncture stimulation: localization of processing with functional MR imaging of the brain- preliminary experience. Radiology. 1999;212:133–141. doi: 10.1148/radiology.212.1.r99jl04133. [DOI] [PubMed] [Google Scholar]
- Wu MT, Sheen JM, Chuang KH, Yang P, Chin SL, Tsai CY, Chen CJ, Liao JR, Lai PH, Chu KA, Pan HB, Yang CF. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage. 2002;16:1028–1037. doi: 10.1006/nimg.2002.1145. [DOI] [PubMed] [Google Scholar]
- Yoo SS, Teh EK, Blinder RA, Jolesz FA. Modulation of cerebellar activities by acupuncture stimulation: evidence from fMRI study. Neuroimage. 2004;22:932–940. doi: 10.1016/j.neuroimage.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zhang WT, Jin Z, Cui GH, Zhang KL, Zhang L, Zeng YW, Luo F, Chen AC, Han JS. Relations between brain network activation and analgesic effect induced by low vs. high frequency electrical acupoint stimulation in different subjects: a functional magnetic resonance imaging study. Brain Res. 2003a;982:168–178. doi: 10.1016/s0006-8993(03)02983-4. [DOI] [PubMed] [Google Scholar]
- Zhang WT, Jin Z, Huang J, Zhang L, Zeng YW, Luo F, Chen AC, Han JS. Modulation of cold pain in human brain by electric acupoint stimulation: evidence from fMRI. Neuroreport. 2003b;14:1591–1596. doi: 10.1097/00001756-200308260-00010. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Bueller JA, Jackson LR, Scott DJ, Xu Y, Koeppe RA, Nichols TE, Stohler CS. Placebo effects mediated by endogenous opioid activity on mu-opioid receptors. J Neurosci. 2005;25:7754–7762. doi: 10.1523/JNEUROSCI.0439-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]