Abstract
In this article we review findings from the World Trade Center Disaster (WTCD) Outcomes Study, a prospective cohort study of 2,368 New York City (NYC) adults funded by the National Institutes of Health after the September 11 attacks. The findings reported were based on a baseline survey conducted one year after the disaster and a follow-up conducted two years post-disaster. One of the goals of this research was to assess the effectiveness of post-disaster treatments received by NYC residents following the attacks. Among the major findings of this study were the relatively small increase in mental health service utilization and the fact that only brief worksite interventions seemed to be an effective post-disaster treatment intervention. Specifically, those who received more conventional post-disaster interventions, such as formal psychotherapy sessions and/or psychotropic medicines, seemed to have poorer outcomes. Since this study was designed to assess treatment outcomes, use advanced measurement techniques, and incorporate propensity score matching to control for bias, these treatment findings were unexpected and raised clinical questions. Additional findings were also discussed related to minority group members, alcohol abuse, the onset and course of posttraumatic stress disorder post-disaster, and other findings. Future research is recommended to resolve the issues raised by this important study, especially as this relates to treatment outcomes.
Keywords: Posttraumatic stress disorder, PTSD, disaster, mental health, alcohol abuse, treatment, effectiveness, outcomes, barriers to care, brief interventions, World Trade Center Disaster, September 11
Following the September 11 terrorist attacks in New York City (NYC), several large-scale epidemiologic studies were funded by the National Institutes of Health to examine the impact of this event on area residents. The study, Impact of Mental Health Services in NY after WTC Disaster (Research Grant R01# MH-66403, Boscarino PI), was one of these investigations. It's primary purpose was to assess the impact of post-event treatments received by NYC residents following the World Trade Center Disaster (WTCD). The secondary purpose was to describe the prevalence of PTSD and related mental disorders among area residents and to identify risk and protective factors for such outcomes. The WTCD was a unique event in US history and represented the largest war-related loss of life on US soil since the American Civil War (Centers for Disease Control, 2002). In response to this disaster, NYC agencies and institutions, as well as those in surrounding communities, provided an extensive array of mental health treatment services for area residents. In NYC, these services were made available to the public through the federally-funded “Project Liberty” program, which offered mental health services to the general public at no or little cost (Felton, 2002). Our study offered a unique health services research opportunity and was specifically designed to assess mental health outcomes associated with this service delivery effort (Boscarino, Adams, & Figley, 2004).
STUDY OVERVIEW AND METHOD
The data for this study come from a prospective cohort study of adults who were living in NYC on the day of the disaster. Detailed information on the basic study design has been published elsewhere (Adams & Boscarino, 2005a; Adams & Boscarino, 2005b; Adams & Boscarino, 2006; Adams, Boscarino, & Galea, 2006a; Adams, Boscarino, & Galea, 2006b; Boscarino, Figley, Adams, Galea, Resnick, et al., 2004; Boscarino, Galea, Ahern, Resnick, & Vlahov, 2002; Boscarino & Adams, 2008; Boscarino, Galea, Ahern, Resnick, &Vlahov, 2003; Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2004; Boscarino, Adams, & Figley, 2005; Boscarino, Adams, Foa, et. al., 2006; Boscarino, Adams, Figley, Galea, et al., 2006; Boscarino, Adams, Stuber, & Galea, 2005; Boscarino, Adams, & Galea, 2006; Galea, Boscarino, Resnick, & Vlahov, 2003; Vlahov et al., 2004; Vlahov et al., 2002). Briefly, using random-digit dialing, a baseline telephone survey was conducted a year after the WTCD attack. As part of the overall study design, residents who reported receiving mental health treatment a year after the attack were “over-sampled” by use of screener questions at the beginning of the survey. The baseline population was also stratified by the 5 NYC boroughs and gender, and was sampled proportionately. Questionnaires were translated into Spanish and then back-translated by bilingual Americans to ensure linguistic and cultural appropriateness. Approximately 7% of these interviews were conducted in Spanish. The baseline survey occurred between October and December 2002 and a follow-up survey occurred one-year later, between October 2003 and February 2004. The data collection procedures were the same for both surveys. Trained interviewers using computer-assisted telephone interviewing (CATI) conducted all interviews. All interviewers were supervised and monitored by the survey contractor in collaboration with the investigative staff. The mean duration of the interview was 45 minutes for the baseline and 35 minutes for the follow-up survey. The Institutional Review Board (IRB) of The New York Academy of Medicine (NYAM) reviewed and approved the study's original protocol. The Geisinger Health System (GHS) IRB subsequently approved the analyses related to the current study.
For the baseline study, 2,368 individuals completed the survey. We were able to re-interview 1,681 of these respondents in the follow-up survey. Using industry-standard survey definitions, the baseline cooperation rate was 63% and the re-interview rate for the follow-up study was 71% (Adams, Boscarino, & Galea, 2006b), consistent with previous epidemiological investigations (Galea et al., 2002). Sampling weights were developed for each wave to correct for potential selection bias related to the number of telephone numbers and persons per household and for the over-sampling of treatment-seeking respondents (Boscarino, Adams, & Figley, 2004). Demographic weights also were used with the follow-up data, to adjust for slight differences in response rates by different demographic groups, a common practice in panel surveys (Groves et al., 2004). With these survey adjustments, the study database is considered representative of adults who were living in NYC on the day of the WTCD attack (Boscarino, Adams, & Figley, 2004).
The basic data analyses in our study focused on answering the following specific research questions.
Who sought mental health treatment after this event?
What were the barriers encountered to seeking treatment after this event?
What were the mental health outcomes among those who received treatment?
What types of post-disaster interventions were the most effective?
What were the risk and protective factors for experiencing adverse mental health outcomes after this event?
Earlier research regarding the health consequences of disasters and other traumatic events guided our original study. The post-disaster literature relevant to the WTCD at the time related to the survivors of the Oklahoma City bombing. Among direct survivors of that incident, 45% had post-disaster psychiatric disorders and 34% had PTSD (North et al., 1999). Another study of the same event found that 62% of residents of the Oklahoma City metropolitan area experienced at least one direct stress-related outcome due to the bombing (Smith, Christiansen, Vincent, & Hann, 1999). In addition, a comparison of Oklahoma City area residents to Indianapolis area residents, used as a control group, suggested that Oklahoma residents reported about twice the psychological distress, PTSD, increased alcohol use, and increased smoking behavior, compared to persons in the Indianapolis area (Smith et al., 1999). Although some investigators have contended that persons recover quickly from these experiences (e.g., McFarlane, 1988; McFarlane, 1989), others suggested that large-scale community disasters could result in significant psychological problems and poorer health outcomes post-disaster (Brewin, Andrews, & Valentine, 2000; Bromet & Dew, 1995: Rubonis & Bickman, 1991). Thus, the research literature at the time suggested that the psychological impact of the WTCD event would be significant. In addition, previous studies of the consequences of PTSD suggested that the impact of this disorder could be substantial (Kessler, 2000; Kulka et al., 1990). Other research suggests that PTSD was not only associated with mental health problems but also with alterations in physical health status (Boscarino, 1996; Boscarino, 1997; Boscarino & Chang, 1999a; Boscarino & Chang, 1999b; Boscarino, 2004; Boscarino, 2006; Boscarino, 2008; McFarlane, Atchison, Rafalowicz, & Papay, 1994; Schnurr & Green, 2004). Furthermore, other research has suggested that survivors of these events have increased psychological difficulties, chronic problems in living, and significant psychosocial resource loss (Adams et al., 2002; Bromet & Dew, 1995; Norris et al., 2002), possibly amplifying adverse health outcomes (Adams & Boscarino, 2006; Boscarino, 1995).
RESEARCH FOCUS
Psychobiological-Stressor Model
Although level of exposure and disaster-related loss are commonly associated with the impact of these events on well-being (Caldera, Palma, Penayo, & Kullgren, 2001; Galea et al., 2002; Geonjian et al., 2001; Mecocci et al., 2000), there are other risk factors involved. Research suggests that increased PTSD vulnerability often occurs among those with a history of mental health disorders, child abuse, or a history of previous traumas (Boscarino, Adams, & Figley, 2004; Breslau, Chilcoat, Kessler, & Davis, 1999; Shalev, 1996). Demographic and socioeconomic factors also are known to affect these experiences (Adams & Boscarino, 2005a). In addition, research has identified the role of social support among those exposed to traumatic stress, both in terms of protecting individuals from PTSD onset (Adams & Boscarino, 2006), and in terms of influencing effective treatments (Boscarino, 1995; van der Kolk, McFarlane, & van der Hart, 1996). In summary, the degree of exposure, social/cultural variables, and other factors, such as self-esteem and other character traits, are known to enhance or reduce the impact of traumatic stress exposures on mental health (Boscarino, Adams, & Figley, 2004). In addition, while many psychosocial components of traumatic stress exposures are now recognized (Adams, Figley, & Boscarino. 2008), the underlying biological bases of these syndromes have also become apparent (Boscarino, 1996; Boscarino & Chang, 1999a; Boscarino & Chang 1999b; Boscarino, 2004; Boscarino, 2008; van der Kolk, 1996; Chrousos, 1995). Thus, we would expect long-term health issues to emerge in traumatized populations, including increases in substance use, changes in help-seeking behaviors, and the onset of chronic health conditions (Boscarino, 2004; Boscarino, 2008). This psychobiological-stressor model guided the original study design.
Outcomes Research Design
As we note below, our WTCD sample represents one of the limited number of population-based studies that prospectively examined post-disaster mental health services and health outcomes for these interventions following a major traumatic event (Boscarino et al., 2002; Boscarino et al., 2003; Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2004; Boscarino, Figley, Adams, et al., 2004; Boscarino, Adams, & Figley, 2005; Boscarino, Adams, Foa, et. al., 2005; Boscarino, Adams, Stuber, et. al., 2005). In addition to descriptive research, our data enabled us to test specific hypotheses about the relationships between trauma experiences, the impact of different interventions, risk and protective factors, and long-term mental health outcomes. We note that our study was specifically designed as an outcomes study and was implemented to answer these kinds of research questions using a cohort study design (Boscarino and Chang 1999c; Figley, Carbonell, Boscarino, & Chang, 1999; Hulley, Cummings, Browner, Grady, & Newman, 2007; Rogers et al. 2000; Rosenheck, Stolar, & Fontana, 2000).
The survey instruments used in this research included reliable scales and health services research measures that had been used and validated in previous research (Freedy, Kilpatrick & Resnick., 1993; Kilpatrick, Acierno, Resnick, & Sanders, 1997; Kilpatrick et al., 2000; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993) and recent traumatic stressor research (Adams & Boscarino, 2005a; Adams & Boscarino, 2005b; Adams & Boscarino, 2006; Adams, Boscarino, & Galea, 2006a; Adams, Boscarino, & Galea, 2006b; Boscarino et al., 2002; Boscarino, Adams, & Figley, 2004; Boscarino, Galea, et al., 2003; Boscarino, Galea, et al., 2004; Boscarino, Figley, Adams, et al., 2004; Boscarino, Adams, & Figley, 2005; Boscarino, Adams, Foa, et al., 2006; Boscarino, Adams, Stuber, et. al., 2005; Boscarino, Adams, & Galea, 2006; Boscarino & Adams, 2008; Galea, Boscarino, et al., 2003). A summary of these scales and measures is presented below in Table 1. Briefly, most of these data were prospectively collected and included the following core measures: (1) demographic characteristics; (2) WTCD exposure variables; (3) exposure to other traumatic events; (4) WTCD rescue and recovery involvement; (5) stressful life experiences; (6) mental health, medical, and other services received pre- and post-disaster; (7) prescription medication use pre- and post-disaster; (8) use of alternative health services pre- and post-disaster; (9) substance use pre- and post-disaster; (10) barriers to care; (11) self-esteem, social support, functional health status and work productivity; (12) post-traumatic stress disorder; (13) major depressive disorder; (14) psychological symptoms in past 30 days; and (15) community-level indicator data (see Table 1).
Table1.
Core Measurement Instruments in WTCD Outcome Study*
| Measurement Area | Measure 1 | Measure 2 | Measure 3 | Measure 4 |
|---|---|---|---|---|
| 1. Mental health status | DSM-IV PTSD for lifetime, past 12 months/30 days | DSM-IV major depression for lifetime, past 12 months/30 days | BSI-18 Psychological symptom scale past 30 days | |
| 2. Substance use | Q-F of tobacco use | Q-F of alcohol use | Binge drinking | CAGE alcohol dependence scale |
| 3. Care visits, treatments & interventions | Outpatient visits & hospitalizations | Outpatient mental health visits & hospitalizations | Psychotropic medication use | Mental health interventions & access to care |
| 4. Stress exposures | Level of exposure to WTC disaster events | Traumatic exposures in lifetime & past 12 months. | Stressful life events in the past 12 months | |
| 5. Social/community resources | Social support in past 12 months | NORC Social capital scale | Assistance from friends & neighbors | Zip code-level census & NYC health data |
| 6. Psychological resources | Rosenberg self-esteem scale | Anomie hostility scale | ||
| 7. Functional status | SF-12: mental & physical functioning past 30 days | Reported work productivity past 30 days | ||
| 8. Demographic measures | Age, gender, income, education, ethnicity, race | Work status, immigration status, language spoken | Religion, church attendance | Household composition |
| 9. Other measures | Use of Alternative services | Disaster rescue & recovery involvement | Reported medical history |
WTCD = World Trade Center Disaster
For more detailed discussion of measures used, see: Boscarino, JA, Adams, RE, Figley, CR. (2004). Mental health service use 1-year after the World Trade Center disaster: implications for medical care. General Hospital Psychiatry, 26, 346−358.
MAIN STUDY FINDINGS
Mental Health Service Use – Baseline (Year 1)
The demographic profile for our study population is presented in Table 2. As reported previously, our weighted final sample closely matched the demographic profile of adult NYC residents (Adams et al., 2006b). As can be seen in Table 2, more than half of our population was a member of a minority group, 57% were female, and about 30% had high exposure to the WTCD event, meaning that they had fairly extensive exposure to the attack and its aftermath (Boscarino, Adams, & Figley, 2004). Analyses from one year post-disaster showed that prevalence of current PTSD was about 5% and the prevalence of current major depression was about 12% (Table 3). Furthermore, 20% of New Yorkers had had mental health visits in the past 12 months and 12.9% reported one or more of these mental health visits was related to the WTCD event. Compared to the year before the attacks, 8.6% of New Yorkers had increased post-disaster mental health visits and 5.3% had a new post-disaster treatment episode in the 12 months post-disaster (Table 3). In terms of medications, 8.1% used psychotropic drugs (Boscarino, Adams, & Figley, 2004). Post-disaster psychotropic medication use related to the WTCD event was 4.5%. Increased post-disaster medication use, compared to the year before the disaster, was 4.1% and new medication episodes occurred among 3% of New Yorkers (Boscarino, Adams, & Figley, 2004). As with outpatient visits, post-disaster medication usage was lower than expected (Boscarino, Adams, & Figley, 2004).
Table 2.
Demographic Profile for Baseline (Year 1) and Follow-up (Year 2) for WTCD Outcome Study*
| 1 Year Post Disaster (N=2368) | 2 Years Post Disaster (N=1681) | |||
|---|---|---|---|---|
| Demographics | Percent (N) | 95% CI | Percent (N) | 95% CI |
| Age | ||||
| 18−29 | 27.2 (483) | 24.8−29.7 | 22.7 (284) | 20.1−25.6 |
| 30−44 | 34.2 (866) | 31.8−36.7 | 32.9 (596) | 30.1−35.8 |
| 45−64 | 28.8 (726) | 26.5−31.1 | 32.5 (586) | 29.8−35.4 |
| 65+ |
9.8 (248) |
8.5−11.4 |
11.9 (215) |
10.1−13.9 |
| Gender | ||||
| Male | 46.2 (1016) | 43.6−48.8 | 46.2 (693) | 43.2−49.3 |
| Female |
53.8 (1352) |
51.2−56.4 |
53.8 (988) |
50.7−56.9 |
| Race | ||||
| White | 39.3 (1015) | 36.9−41.7 | 43.0 (782) | 40.1−45.9 |
| African American | 26.3 (606) | 24.2−28.6 | 26.0 (422) | 23.4−28.7 |
| Hispanic/Latino | 25.7 (559) | 23.5−28.1 | 24.1 (367) | 21.5−26.9 |
| Asian | 5.2 (99) | 4.1−6.6 | 4.6 (62) | 3.4− 6.1 |
| Other |
3.5 (89) |
2.7−4.5 |
2.4 (48) |
1.7− 3.4 |
| Borough of Residence | ||||
| Manhattan | 21.1 (555) | 19.8−22.5 | 21.0 (411) | 19.5 −22.6 |
| Bronx | 15.6 (373) | 14.4−16.8 | 15.5 (252) | 14.1−17.0 |
| Brooklyn | 30.1 (707) | 28.5−31.7 | 30.3 (490) | 28.4−32.2 |
| Queens | 27.9 (594) | 26.4−29.4 | 27.7 (423) | 26.0−29.5 |
| Staten Island |
5.4 (139) |
4.7− 6.2 |
5.5 (105) |
4.65 −6.3 |
| Exposure to WTCD | ||||
| Low Exposures | 26.5 (510) | 24.2−28.9 | 26.7 (362) | 24.0−29.6 |
| Moderate Exposures | 44.0 (1003) | 41.4−46.6 | 43.9 (719) | 40.9−47.0 |
| High Exposures | 22.0 (594) | 20.0−24.2 | 21.8 (416) | 19.4−24.4 |
| Very High Exposures | 7.5 (261) | 6.4− 8.8 | 7.6 (184) | 6.3− 9.1 |
Note: All N's are unweighted. Percentages and confidence intervals shown represent the weighted data (i.e., adjustments to the sample for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification). CI = Confidence interval; WTCD = World Trade Center Disaster.
Table 3.
Baseline Psychological Disorders and Mental Health Service Utilization Following the World Trade Center Disaster in New York City (N = 2,368)
| Outcomes | Unweighted N† | Weighted % | 95%CI* |
|---|---|---|---|
| Mental Health Status | |||
| PTSD Ever | 284 | 8.15 | 6.87−9.42 |
| PTSD since WTCD | 196 | 5.25 | 4.23−6.26 |
| Depression Ever | 621 | 19.00 | 17.11−20.83 |
| Depression since WTCD |
416 |
11.76 |
10.29−13.22 |
| Mental Health Visits | |||
| Any Mental Health Treatment Visits Ever | 1242 | 38.98 | 36.56−41.39 |
| Any Mental Health Treatment Visits since WTCD | 766 | 19.99 | 18.20−21.77 |
| Any Mental Health Treatment Visits related to WTCD | 547 | 12.88 | 11.51−14.25 |
| Increased Mental Health Treatment Visits since WTCD | 332 | 8.57 | 7.36−9.79 |
| New Mental Health Treatment Visit since WTCD | 189 | 5.28 | 4.32−6.25 |
CI = Confidence interval; WTCD = World Trade Center Disaster.
All N's are unweighted. Percentages and confidence intervals shown represent the weighted data (i.e., adjustments to the sample for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification).
For additional information, see: Boscarino, JA, Adams, RE, Figley, CR. (2004). Mental health service use 1-year after the World Trade Center disaster: Implications for medical care. General Hospital Psychiatry, 26, 346−358.
In multivariate logistic regression analyses, increased mental health visits were associated with younger age, peri-event panic attack, negative life events, and depression. In addition, WTCD-related visits had a positive “dose-response” association with level of WTCD exposure (p < 0.0001 for trend). WTCD-related visits also were positively associated with peri-event panic, anxiety, lower self-esteem, PTSD, and depression. Increased post-disaster medication use was positively related to PTSD and depression, and negatively associated with African American status. WTCD-related medication use also was positively related to younger age, female gender, WTCD exposure level, negative life events, PTSD, anxiety, and lower self-esteem.
In summary, while the percentage of New Yorkers seeking post-disaster treatment did not increase substantially from the pre-disaster period, the volume of visits among existing patients apparently increased. We concluded that exposure to WTCD events was related to post-disaster PTSD and depression, as well as WTCD-related mental health service use in New York. However, contrary to expectations, although the WTCD did have an impact on treatment seeking among existing patients, it did not substantially increase mental health treatment seeking among the general NYC population (Boscarino, Adams, & Figley, 2004). Given the availability of post-disaster mental health services (Felton, 2002), it was thought that services use would be much higher.
Mental Health Service Use – Follow-up (Year 2)
Analysis of treatment seeking at follow-up (i.e., year 2 post-disaster) revealed that there were some increases in obtaining treatment in comparison to before the WTCD. The most noteworthy increase was for psychotropic medication use, which went from 8.5% before the WTCD to 12% two years after the attack (p < .001). Two years after the WTCD, 24% of NYC adults had received some type of mental health treatment in the form of therapy or medication in the past 12 months. This was an increase from the baseline survey (i.e., year 1 post-disaster), which was 20%. In addition, at follow-up, the majority of the time NYC residents reported that their post-disaster treatment was related to the WTCD, which was not the case one-year post-disaster. Detailed multivariate analyses for those who sought treatment after the WTCD in the year 2 follow-up survey suggested that those who experienced negative life events were more likely to seek counseling and those with low self-esteem were more likely to take psychotropic medications. Finally, those who reported that their counseling or medication use was related to the WTCD, were more likely to report greater exposure to the WTCD event. (Results available on request.)
Treatment Barriers
A second focus of the original study was to examine potential barriers related to using mental health services in NYC after the WTCD. When we examined at baseline those who met criteria for PTSD or major depression post-disaster, only 45% reported using post-disaster mental health services and only 33% indicated that they sought these services for WTCD-related problems (Boscarino, Adams, Stuber, et al., 2005). In a multivariate logistic model, only WTCD exposure was significant in predicting post-disaster service use among persons with these psychological disorders. For service utilization related to the WTCD, results indicated that African Americans were less likely to have had mental health visits compared to Whites, while those who had a regular doctor, had greater exposure to WTCD events, and those who had a peri-event panic attack were more likely to have such visits. In terms of medication use, 26% of these PTSD-depression cases used psychotropic drugs in the year after the WTCD and 16% reported that this use was related to the disaster. Multivariate results, again, suggested that African Americans were less likely to use post-disaster medications, whereas persons 45+ years old, those with a regular doctor, those exposed to more WTCD events, and those who had a peri-event panic attack were more likely to have taken medications related to the disaster (Boscarino, Adams, Stuber, et al., 2005). When we asked this group of respondents at baseline why they did not seek help, many indicated that they did not think that they had a problem, that they had the help of family and friends, or that they tried to solve these problems on their own (Boscarino, Adams, Stuber, et al., 2005).
Racial and Ethnic Group Results
The discovery of racial/ethnic disparities in seeking treatment led us to assess the association between race/ethnicity and psychological health status in more detail at baseline (Adams & Boscarino, 2005a). When we did this, there was no evidence of racial/ethnic differences for PTSD, PTSD symptom severity, or the likelihood of being classified in poor physical health on the SF-12 physical health scale, once other risk factors were controlled. In fact, African Americans were less likely to meet criteria for major depression or to be classified as unhealthy on the SF-12 mental health scale (Adams & Boscarino, 2005a). Only for peri-event panic attack were there significant differences by ethnicity, with both African Americans and Puerto Ricans more likely to meet criteria for this mental disorder relative to Whites (Adams & Boscarino, 2005a).
Functional Health Status Outcomes
Using baseline data, we also examined the relationship between exposure to the WTCD and functional health status following the attacks based on the SF-12 scale. Overall — the greater the exposure to WTCD events, the poorer psychological well-being — even after controlling for demographic characteristics, other stressors, and social psychological resources (Adams & Boscarino, 2005b). Exposure was only weakly related to physical well-being, however, once other factors were controlled.
We also examined the consequences of the WTCD longitudinally. In ordinary least-squares regression models that contained demographic characteristics, stress risk factors, and stress moderators as independent variables, level of exposure to the disaster was associated with follow-up (i.e., year 2 post-disaster) physical and psychological well-being. However, we found that level of exposure was not related to these outcomes, once the baseline (year 1) measure of the follow-up dependent variable was controlled in these models. This suggested that disaster exposure did not continue to have a lasting negative impact on physical or psychological health status (Adams, Boscarino, & Galea, 2006a).
Our results did indicate that experiencing a WTCD-related peri-traumatic panic attack was related to poorer physical health status post-disaster at baseline, while meeting the criteria for alcohol dependence post-disaster was associated with poorer mental health status at baseline (Adams, Boscarino, & Galea, 2006a). At follow-up, however, and contrary to expectations, WTCD-related peri-traumatic panic attack did not have an adverse impact on health, once other risk factors were controlled (Boscarino & Adams, 2008).
Results Related to PTSD Onset and Course
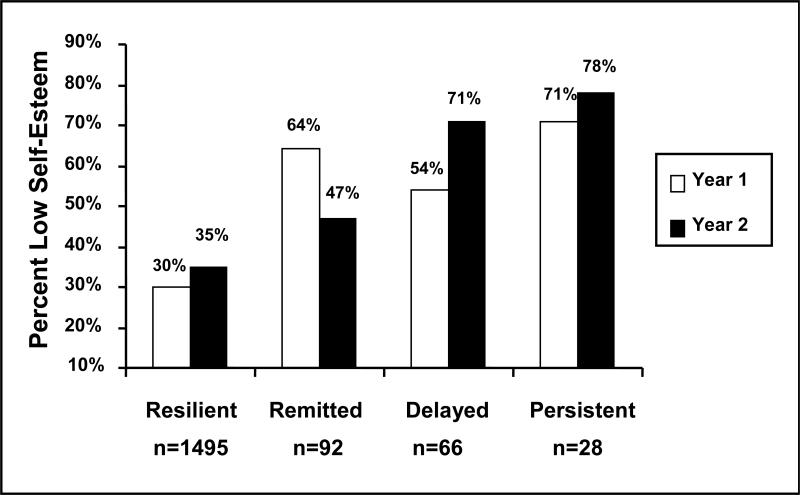
As noted, our results suggested that the prevalence of PTSD 12 months post-disaster was about 5% (Boscarino, Adams, & Figley, 2004). Further analyses suggested that there were significant associations between PTSD at baseline and being female, being younger, having lower self-esteem, having lower social support, having greater WTCD event exposures, having greater lifetime traumatic events, and having a history of depression (all p-values < 0.05; Adams & Boscarino, 2006). However, the results were different for PTSD at follow-up (year 2 post-disaster). At follow-up, being middle-aged, being Latino, having lower self-esteem, having more negative life events, and having higher traumatic life events were now significant predictors of PTSD (Adams & Boscarino, 2006). Noteworthy was that WTCD event exposure now was not significant at follow-up. Further analyses suggested that the onset of “delayed PTSD” at follow-up tended to be associated with the onset of negative life events and decreases in self-esteem, not with previous WTCD event exposure, per se. (Adams & Boscarino, 2006). The finding for self-esteem and PTSD outcomes are shown in Figure 1. As can be seen, increased self-esteem is associated with remitted PTSD at follow-up (i.e., PTSD at baseline, but not at follow-up) and decreased self-esteem is associated with delayed PTSD at follow-up (i.e., no PTSD at baseline, but PTSD at follow-up). Also noteworthy is that the resilient PTSD cases (i.e., no PTSD at baseline or follow-up) have the lowest levels of low self-esteem of any of the PTSD groups studied (see Figure 1).
Figure 1.
Percent of Respondents Having Low Self-Esteem by PTSD Status at Follow-up*
*PTSD groups were defined as follows: Resilient = no PTSD in year 1 or year 2; Remitted = PTSD in year 1 but not year 2; Delayed = no PTSD in year 1 but PTSD in year 2; Persist = PTSD in year 1 and year 2.
Figure adopted with permission from Lippincott Williams & Wilkins (copyright 2006): Adams, RE, Boscarino, JA. (2006). Predictors of PTSD and delayed-PTSD after disaster: The impact of exposure and psychosocial resources. Journal of Nervous and Mental Disease, 195, 485−493.
Alcohol Abuse
Since research has suggested that exposure to psychological trauma was associated with increased abuse of alcohol (Boscarino, Adams, & Galea, 2006), we analyzed alcohol consumption, binge drinking, and alcohol dependence among study participants at one year and two years post-disaster. In multivariate models controlling for demographic factors, other stressor exposures, psychological resources, and history of anti-social behavior, we found that greater exposure to the WTCD event was associated with greater alcohol consumption at one year and two years after this event (Boscarino, Adams, & Galea, 2006). In addition, our analyses indicated that exposure to the WTCD was associated with binge drinking at one year after but not two years after this event. Alcohol dependence, assessed as present in either year 1 or year 2, also was positively associated with greater WTCD exposure. Posttraumatic stress disorder was not associated with alcohol use, once WTCD exposure and other covariates were controlled. In addition, we found that our alcohol abuse measures were positively associated with most adverse mental health measures, including PTSD, depression, anxiety, and poor functional health status (Adams, Boscarino, & Galea, 2006a).
Treatment Effectiveness
Conventional Interventions
As noted above, a central focus of our study was to use our prospective, population-based research design to evaluate intervention outcomes among those who obtained post-disaster mental health services, which were made widely available in NYC post-disaster (Felton, 2002). This basic prospective evaluation design was used successfully in past mental health effectiveness studies (Bovasso, Eaton, & Armenian, 1999). To assess the effectiveness of various psychotherapy treatments, we identified individuals who either had PTSD or subsyndromal PTSD (Galea et al., 2003) at baseline and who were re-interviewed at follow-up (n = 490). Using a propensity score method (Rosenbaum & Rubin, 1983), we then matched cases that received different types of post-disaster interventions to comparable cases that did not. For these analyses we compared outcomes at follow-up for several standards of treatment that patients received (e.g., those receiving 3−6 psychotherapy sessions for 30 minutes or more post-disaster vs. those that did not, etc.).
The health outcomes examined included alcohol dependence, binge drinking, mental health symptoms, SF-12 physical and mental health status, and PTSD. For these analyses, propensity scores were used to match treated cases to untreated controls. These results, based on conditional logistic regression, suggested that conventional post-disaster interventions for traumatic stress exposures appeared to be ineffective. That is, participants in our study who received traditional psychotherapy at baseline were not less symptomatic based on our outcome measures at follow-up, compared to those individuals with baseline PTSD who did not receive these interventions. In fact, our results suggested, paradoxically, that the treated cases often had worse outcomes than the untreated cases. In addition, this treatment exposure revealed a negative dose-response effect, whereby the more treatment a patient received, the worse his or her mental health outcomes at follow-up. When we examined outcomes for all respondents, regardless of whether they met the case definition or not for PTSD or depression, these results were basically the same. In other words, those who received psychotherapy, regardless of their level of psychological impairment at baseline, had worse outcomes at follow-up. (Results available upon request.)
Brief Interventions
When we assessed the effects of brief emergency mental health counseling post-disaster, the results were different. Although there has been controversy associated with this modality (Gist & Devilly, 2002; Kaplan, Iancu & Bodner, 2001; van Emmerik, Kamphuis, Hulsbosch, & Emmelkamp, 2002), consistent with some reports (e.g., Basoglu, Salcioglu, Livanou, & Kalender, 2005), we found that brief post-disaster interventions significantly reduced mental health problems and symptoms up to two years after these interventions (Boscarino, Adams, & Figley, 2005; Boscarino, Adams, Foa, et al., 2006). In our study, about 10% of NYC adults reported receiving some type of crisis interventions conducted by mental health professionals within a year after the attacks (Table 3). Based on our sample, approximately 7% of NYC adults (∼ 425,000 persons) reported receiving employer-sponsored, worksite crisis interventions related to the WTCD. These interventions were delivered at the worksite and were defined as a brief session related to coping with the World Trade Center disaster shortly after this event, directed by a mental health professional and arranged by area employers for their employees. Crisis interventions following traumatic events have been utilized for a number of years (Gist & Devilly, 2002; Kaplan, Iancu, & Bodner, 2001; van Emmerik et al., 2002).
However, the effectiveness and safety of these interventions have been challenged (Boscarino, Adams, Foa, et al., 2006; Gist & Devilly, 2002).
In the past, evaluation of these interventions has been hampered by limited research designs (Boscarino, Adams, Foa et al., 2006). The purpose of our recent study was to conduct a more advanced and focused analysis of preliminary findings reported elsewhere based on a multivariate covariate model (Boscarino, Adams, & Figley, 2005). Our initial analysis, which examined both mental health and alcohol abuse outcomes, suggested that those who attended 1−3 brief sessions had significantly better outcomes 2 years post-disaster (Boscarino, Adams, & Figley, 2005). Based on these initial findings we refined our analysis and expanded the number of covariates to control for potential bias and confounding. The latter was achieved through use of more advanced propensity score matching to assess the “average treatment” effect of worksite interventions (Boscarino, Adams, Foa, et al., 2006).
A description of the services received by employees at the worksite and the patient's rating of these services are shown in Table 4. The data for this analysis was based on a subset of 1,121 employed adults interviewed by telephone in our household WTCD survey at baseline and at follow-up. For the current study, we used propensity scores to match worksite intervention cases (n = 150) to worksite nonintervention controls (n = 971) using a 1:5 matching ratio based on a bias-corrected, nearest-neighbor algorithm (Boscarino, Adams, Foa, et al., 2006). Unlike more conventional mental health treatments, these worksite interventions appeared to be effective across a spectrum of outcomes, including reduced alcohol dependence, binge drinking, depression, PTSD severity, and reduced anxiety symptoms (Table 5; Boscarino, Adams, Foa, et al., 2006). While this propensity study had limitations, it suggested that brief post-disaster crisis interventions may be effective for employees following mass exposure to psychologically traumatic events. None of the other interventions that we studied came close to achieving these results. The reasons for the effectiveness of the brief worksite interventions were unclear and warrant further investigations. Other than for the outcome of alcohol dependence and binge drinking, those who received conventional therapy sessions tended to do worse after these interventions. In addition, the more conventional sessions they received, the worse they did in terms of PTSD, depression, anxiety, and global severity, a worrisome finding. As discussed previously, our study included extensive risk factor data (see Table 1); we used these data to “risk adjust” our treatment models. For conventional treatments, this risk adjustment made little difference.
Table 4.
Descriptive Statistics for Brief Intervention Exposures in Baseline Survey (N = 2,368)*
| Intervention Characteristics |
% (Weighted) |
95% CI |
N (Unweighted) |
|---|---|---|---|
| Number of Brief Crisis Sessions | |||
| None | 89.9 | 88.4−91.3 | 2012 |
| One | 4.4 | 3.4−5.6 | 123 |
| Two to Three | 3.6 | 2.9−4.5 | 134 |
| Four or more |
2.1 |
1.7−2.8 |
89 |
| Percent any Brief Crisis Sessions |
10.2 |
8.9−11.8 |
356 |
| Number of Brief Crisis Sessions at Worksite | |||
| None | 93.5 | 92.4−94.5 | 2124 |
| One | 3.4 | 2.6−4.4 | 103 |
| Two to Three | 2.3 | 1.8−2.8 | 99 |
| Four or more |
0.9 |
0.6−1.3 |
42 |
| Percent any Brief Crisis Sessions at Worksite |
6.5 |
5.5−7.6 |
244 |
| Content of Brief Sessions, among those having any sessions (n = 356) | |||
| Educated about Stress Symptoms | 63.7 | 56.2−70.7 | 244 |
| Talked about Experiences | 62.9 | 55.0−70.1 | 264 |
| Taught to Cope with Things | 65.1 | 57.8−71.7 | 246 |
| Taught to Think Positively | 64.1 | 56.8−70.8 | 238 |
| Taught to Evaluate Thoughts | 57.7 | 50.4−64.6 | 206 |
| Taught to Deal with Emotions | 69.1 | 61.8−75.5 | 255 |
| Taught to Relax |
65.9 |
58.6−72.4 |
245 |
| Reported Helpfulness of Crisis Intervention Sessions, among those having any sessions (n=356) | |||
| Not at All Helpful | 17.7 | 12.0−25.4 | 47 |
| Helped a Little | 24.5 | 18.9−31.1 | 84 |
| Helped Some | 25.4 | 20.2−31.6 | 101 |
| Helped a Lot | 32.4 | 26.0−39.5 | 124 |
All N's are unweighted. Percentages and confidence intervals shown represent the weighted data (i.e., adjustments to the sample for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification). CI = Confidence interval; WTCD = World Trade Center Disaster.
Table adopted with permission from Lippincott Williams & Wilkins (copyright 2006): Boscarino, JA, Adams, RE, Foa, EB, Landrigan, PJ. (2006). A propensity score analysis of brief worksite crisis interventions after the World Trade Center disaster: Implications for intervention and research. Medical Care, 44, 454−462.
Table 5.
Summary Results for Brief Worksite Interventions for 7 Outcomes at Follow-up*
| |
PTSD Diagnosis |
Depression Diagnosis |
Alcohol Dependence |
Binge Drinking |
Mean PTSD Symptom Level |
Mean Depression Symptom Level |
Mean Anxiety Symptom Level |
|---|---|---|---|---|---|---|---|
| |
|
|
|
|
|
|
|
| Significance level | NS | p < .05 | p < .01 | p < .05 | p < .05 | p < .05 | p < .10 |
|
Impact of treatment vs. no treatment** |
- |
7.2% |
4.8% |
5.5% |
.8 |
1.8 |
1.4 |
For additional information, see: Boscarino, JA, Adams, RE, Foa, EB, Landrigan, PJ. (2006). A propensity score analysis of brief worksite crisis interventions after the World Trade Center disaster: Implications for intervention and research. Medical Care, 44, 454−462.
As an example of the brief treatment outcome impact, the results for depression suggest that the prevalence of depression was about 7% lower among treated cases at follow-up compared to matched untreated cases. Likewise, treated cases had lower mean depression symptom scores by about 2 points compared to matched untreated cases.
CONCLUSION
As noted, following exposure to the WTCD, the majority of individuals exposed to these events generally did not seek mental health treatment, even though some clearly experienced mental problems (Boscarino, Adams, Stuber, et al., 2005). In addition, some persons experienced delayed mental health problems two years after the initial exposure (Adams & Boscarino, 2006). Our main study objective was to undertake analyses that could provide insight related to the impact of treatment-seeking and the onset of mental health problems following a major traumatic event exposure — information that could inform health professionals about the consequences of exposure to psychological trauma and the impact of treatment interventions following such events. Our study's main findings are as follows:
Generally, those who sought mental health treatment after the WTCD tended to be individuals who sought treatment before this event. They also tended to be individuals highly exposed to the WTCD event. Conversely, symptomatic individuals who did not seek treatment tended to be members of minority groups, did not have health insurance coverage, and tended to have sought informal support from friends and neighbors.
Those who experienced “delayed” PTSD after the WTCD event (i.e., no PTSD at baseline, but PTSD at follow-up), tended to be Hispanic, non-native born, to have recently experienced lower self-esteem and/or negative life events. Contrary to expectations, the degree of WTCD exposure did not predict delayed PTSD. Persistent PTSD cases (i.e., had PTSD at baseline and at follow-up) were similar to delayed cases, except that these cases had higher exposure to the WTCD events and they had a history of mental health disorders before the WTCD event.
The outcomes of mental health treatment after the WTCD attack and what types of interventions were the most beneficial were a major focus of our research. Our findings suggested that early brief interventions at the worksite were the most effective post-disaster treatment. In addition, informal support seeking from friends, neighbors, and from spiritual communities also appeared beneficial. Conversely, those who received more extensive post-disaster interventions (e.g., formal psychotherapy sessions for 30 minutes or more) did not benefit and, in fact, they appeared to have worse outcomes. The reasons for the latter finding were unclear, since we controlled for an extensive number of risk factors in these analysis, presumably controlling for selection bias and confounding.
In terms of those who were the most resilient to mental health problems following the WTCD event, they tended to be males, older persons, those with higher self-esteem and stronger social support. They also tended to be persons without a history of mental health problems before the WTCD event. Finally, they tended to be persons with fewer lifetime traumatic events and those with fewer stressful life events in the past year.
Our study suggests that exposure to psychological trauma is associated with increases in problem drinking and alcohol abuse long after exposure and that these substance use outcomes tend to be associated with other adverse mental health outcomes post-exposure.
RECOMMENDATIONS
Based on our study findings, our recommendations for future post-trauma research include the following:
Additional research is needed related to why receiving brief post-disaster treatment interventions were effective.
Conversely, research is needed to confirm that those who received conventional post-disaster treatments actually did worse, and if so, why this may have been the case.
Additional research is needed to determine why clearly symptomatic members of minority groups tended not to seek post-disaster treatment. For example, was this because of differences in perceived stigma, because of informal or alternative treatment-seeking, or some other reason?
Further research is needed to determine the effectiveness and nature of informal social support and alternative interventions in protecting individuals from post-disaster mental health problems.
Research is recommended related to factors that affect post-disaster resiliency. For example, persons with higher self-esteem post-disaster tended to be protected from future mental health problems. Some research questions are: Why were these persons protected from mental health problems? Should self-esteem be a focus of post-event interventions in the future? In the past, post-disaster interventions have usually focused on psychopathology, rather than on wellness and positive psychological factors. Our research suggests that this clinical focus might be misplaced.
Our study suggests that exposure to psychological trauma may be associated with increases in problem drinking and alcohol abuse after these exposures and deserves further investigation.
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health (Grant # R01 MH-66403) and the Pennsylvania Department of Health (Grant # 4100042573). Joseph A. Boscarino, PhD, MPH serves as the Senior Investigator, Center for Health Research at the Geisinger Clinic. He is also an Asscoiate Professor in the Depts. of Medicine and Pediatrics at Mount Sinai School of Medicine. Richard E. Adams, PhD serves with the Dept. of Sociology at Kent State University. The authors have no conflict of interest related to the current research.
Contributor Information
Joseph A. Boscarino, Geisinger Clinic, Danville, PA Mount Sinai School of Medicine, New York, NY
Richard E. Adams, Kent State University, Kent, OH
REFERENCES
- Adams RE, Boscarino JA. Differences in mental health outcomes among Whites, African Americans, and Hispanics following the September 11 attacks. Psychiatry. 2005a;68:250–265. doi: 10.1521/psyc.2005.68.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Stress and well-being in the aftermath of the World Trade Center attack: the continuing effects of a community-wide disaster. Journal of Community Psychology. 2005b;33:175–190. doi: 10.1002/jcop.20030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Predictors of PTSD and delayed-PTSD after disaster: the impact of exposure and psychosocial resources. Journal of Nervous and Mental Disease. 2006;195:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. Alcohol use, mental health status and psychological well-being 2 years after the World Trade Center attacks in New York City. American Journal of Drug and Alcohol Abuse. 2006a;32:203–224. doi: 10.1080/00952990500479522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. Social and psychological resources and health outcomes after World Trade Center disaster. Social Science and Medicine. 2006b;62:176–188. doi: 10.1016/j.socscimed.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Bromet EJ, Panina N, Golovakha E, Goldgaber D, Bluzman S. Stress and well-being in mothers of young children 11 years after Chornobyl nuclear power plant accident. Psychological Medicine. 2002;32:143–156. doi: 10.1017/s0033291701004676. [DOI] [PubMed] [Google Scholar]
- Adams RE, Figley CR, Boscarino JA. The compassion fagtigue scale: Its use with social workers following urban disaster. Research in Social Work Practice. 2008;18:238–250. doi: 10.1177/1049731507310190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basoglu M, Salcioglu E, Livanou M, Kalender D, Acar G. Single-session behavioral treatment of earthquake-related posttraumatic stress disorder: a randomized waiting list controlled trial. Journal of Trauma Stress. 2005;8:1–11. doi: 10.1002/jts.20011. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Post-traumatic stress and associated disorders among Vietnam veterans: the significance of combat exposure and social support. Journal of Traumatic Stress. 1995;8:317–336. doi: 10.1007/BF02109567. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Post-traumatic stress disorder, exposure to combat, and lower plasma cortisol among Vietnam veterans: findings and clinical implications. Journal of Consulting and Clinical Psychology. 1996;64:191–201. doi: 10.1037//0022-006x.64.1.191. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Diseases among men 20 years after exposure to severe stress: implications for clinical research and medical care. Psychosomatic Medicine. 1997;59:605–614. doi: 10.1097/00006842-199711000-00008. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Association between posttraumatic stress disorder and physical illness: results and implications from clinical and epidemiologic studies. Annals of New York Academy of Sciences. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. PTSD and mortality among US Army veterans: A 30-year follow-up. Annals of Epidemiolgy. 2006;16:248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. A Prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosomatic Medicine. 2008;70:668–676. doi: 10.1097/PSY.0b013e31817bccaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE. Peritraumatic panic attacks and health outcomes two years after psychological trauma: implications for intervention and research. Psychiatry Research. 2008;160 doi: 10.1016/j.psychres.2008.03.019. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Mental health service use 1-year after the World Trade Center disaster: implications for medical care. General Hospital Psychiatry. 2004;26:346–358. doi: 10.1016/j.genhosppsych.2004.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. A prospective cohort study of the effectiveness of employer-sponsored crisis interventions after a major disaster. International Journal of Emergency Mental Health. 2005;7:9–22. [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Worker productivity and outpatient service use after the September 11th attacks: Results from the New York City terrorism outcome study. American Journal of Industrial Medicine. 2006;49:670–682. doi: 10.1002/ajim.20340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR, Galea S, Foa EB. Fear of terrorism and preparedness in New York City 2 years after the attacks: implications for disaster planning and research. Journal of Public Health Management and Practice. 2006;12:505–513. doi: 10.1097/00124784-200611000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Foa EB, Landrigan PJ. A propensity score analysis of brief worksite crisis interventions after the World Trade Center disaster: Implications for intervention and research. Medical Care. 2006;44:454–462. doi: 10.1097/01.mlr.0000207435.10138.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Galea S. Alcohol use in NY after the terrorist attacks: a study of the effects of psychological trauma on drinking behavior. Addictive Behaviors. 2006;31:606–621. doi: 10.1016/j.addbeh.2005.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Stuber J, Galea S. Disparities in mental health treatment following the World Trade Center disaster: Implication for mental health care and health services research. Journal of Traumatic Stress. 2005;18:287–297. doi: 10.1002/jts.20039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Chang J. Higher abnormal leukocyte and lymphocyte counts 20 years after exposure to severe stress: Research and clinical implications. Psychosomatic Medicine. 1999a;61:378–386. doi: 10.1097/00006842-199905000-00019. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Chang J. Electrocardiogram abnormalities among men with stress-related psychiatric disorders: Implications for coronary heart disease and clinical research. Annals of Behavioral Medicine. 1999b;21:227–234. doi: 10.1007/BF02884839. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Chang J. Survival after coronary artery bypass graft surgery and community socioeconomic status: Clinical and research implications. Medical Care. 1999c;37:210–216. doi: 10.1097/00005650-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Figley CR, Adams RE, Galea S, Resnick H, Fleischman AR, et al. Adverse reactions of study persons recently exposed to mass urban disaster. Journal of Nervous and Mental Disease. 2004;192:515–524. doi: 10.1097/01.nmd.0000135476.20580.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Resnick H, Vlahov D. Mental health service and psychiatric medication use following the terrorist attacks in New York City. Psychiatric Services. 2004;55:274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Utilization of mental health services following the September 11th terrorist attacks in Manhattan, New York City. International Journal of Emergency Mental Health. 2002;4:143–155. [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Psychiatric medication use following the September 11th terrorist attacks in Manhattan, New York City. Journal of Traumatic Stress. 2003;16:301–306. doi: 10.1023/A:1023708410513. [DOI] [PubMed] [Google Scholar]
- Bovasso GB, Eaton WW, Armenian HK. The long-term outcomes of mental health treatment in a population-based study. Journal of Consulting and Clinical Psychology. 1999;67:529–38. doi: 10.1037//0022-006x.67.4.529. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit area survey of trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Dew MA. Review of psychiatric epidemiologic research on disasters. Epidemiologic Reviews. 1995;17:113–119. doi: 10.1093/oxfordjournals.epirev.a036166. [DOI] [PubMed] [Google Scholar]
- Caldera T, Palma L, Penayo U, Kullgren G. Psychological impact of the hurricane Mitch in Nicaragua in a one-year perspective. Social Psychiatry and Psychiatric Epidemiology. 2001;36:108–114. doi: 10.1007/s001270050298. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control Community needs assessment of lower Manhattan residents following the World Trade Center attacks - Manhattan, New York, 2001. Morbidity and Mortality Weekly Report. 2002;288(10):1227–1228. [Google Scholar]
- Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. New England Journal of Medicine. 1995;332:1351–1362. doi: 10.1056/NEJM199505183322008. [DOI] [PubMed] [Google Scholar]
- Felton CJ. Project Liberty: A public health response to New Yorkers’ mental health needs arising from the World Trade Center terrorist attacks. Journal of Urban Health. 2002;79:429–433. doi: 10.1093/jurban/79.3.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figley CR, Carbonell JL, Boscarino JA, Chang J. A clinical demonstration model for assessing the effectiveness of therapeutic interventions: An expanded clinical trials methodology. International Journal of Emergency Mental Health. 1999;1:155–164. [PubMed] [Google Scholar]
- Freedy JR, Kilpatrick DG, Resnick HS. Allen R, editor. Natural disasters and mental health: Theory, assessment, and intervention. Journal of Social Behavior and Personality. 1993;8:49–103. Handbook of post-disaster interventions. [special issue].
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in Manhattan, New York City. New England Journal of Medicine. 2002;346:982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Galea S, Boscarino JA, Resnick H, Vlahov D. Mental health in New York City after the September 11 terrorist attacks: Results from two population surveys. In: Manderscheid RW, Henderson MJ, editors. Mental Health, United States, 2001. US Government Printing Office; Washington, DC: 2003. pp. 83–91. [Google Scholar]
- Gist R, Devilly GJ. Post-trauma debriefing: The road too frequently travelled. Lancet. 2002;360:741–742. doi: 10.1016/S0140-6736(02)09947-6. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Molina L, Steinberg AM, Fairbanks LA, alvarez ML, Goenjian HA, Pynoos RS. Post-traumatic stress and depressive reactions among Nicaraguan adolescents after Hurricane Mitch. American Journal of Psychiatry. 2001;158(5):788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey methodology. Wiley; New York, NY: 2004. [Google Scholar]
- Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing clinical research: An epidemiologic approach. Third Edition Lippincott Williams & Wilkins; Baltimore, MD: 2007. [Google Scholar]
- Kaplan Z, Iancu I, Bodner E. A review of psychological debriefing after extreme stress. Psychiatric Services. 2001;52:824–827. doi: 10.1176/appi.ps.52.6.824. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61(suppl 5):4–12. [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Sanders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam generation: Report of findings from the National Vietnam Readjustment Study. Brunner/Mazel; New York: 1990. [Google Scholar]
- McFarlane AC. Aetiology of posttraumatic stress disorders following a natural disaster. British Journal of Psychiatry. 1988;152:116–121. doi: 10.1192/bjp.152.1.116. [DOI] [PubMed] [Google Scholar]
- McFarlane AC. The aetiology of posttraumatic morbidity: Predisposing, precipitating and perpetuating factors. British Journal of Psychiatry. 1989;154:221–228. doi: 10.1192/bjp.154.2.221. [DOI] [PubMed] [Google Scholar]
- McFarlane AC, Atchison M, Rafalowicz E, Papay P. Physical symptoms in posttraumatic stress disorder. Journal of Psychosomatic Research. 1994;38:715–726. doi: 10.1016/0022-3999(94)90024-8. [DOI] [PubMed] [Google Scholar]
- Mecocci P, Di Torio AD, Pezzuto S, Rinaldi P, Simonelli G, Maggio D, et al. Impact of the earthquake of September 26,1997 in Umbria, Italy on the socioenvironmental and psychophysical conditions of an elderly population. Aging (Milano) 2000;12:281–286. doi: 10.1007/BF03339848. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981−2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, Smith EM. Psychiatric disorders among survivors of the Oklahoma City bombing. Journal of the American Medical Association. 1999;282:755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and PTSD in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rogers WJ, Canto JG, Barron HV, Boscarino JA, Shoult DA, Every NR. Treatment and outcome of myocardial infarction in hospitals with and without invasive capability. Journal of the American College of Cardiology. 2000;35:371–379. doi: 10.1016/s0735-1097(99)00505-7. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DR. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Rosenheck R, Stolar M, Fontana A. Outcomes monitoring and the testing of new psychiatric treatments: work therapy in the treatment of chronic posttraumatic stress disorder. Health Services Research. 2000;35(1 Pt 1):133–151. [PMC free article] [PubMed] [Google Scholar]
- Rubonis AV, Bickman L. Psychological impairment in the wake of disaster: The disaster-psychopathology relationship. Psychological Bulletin. 1991;109:384–399. doi: 10.1037/0033-2909.109.3.384. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of extreme stress. American Psychological Association; Washington, DC: 2004. [Google Scholar]
- Shalev AY. Stress versus traumatic stress: from acute homeostatic reactions to chronic psychopathology. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic stress: The effects of overwhelming experience on mind, body, and society. Guilford Press; New York: 1996. pp. 77–101. [Google Scholar]
- Smith DW, Christiansen EH, Vincent R, Hann NE. Population effects of the bombing of Oklahoma City. Journal of Oklahoma State Medical Association. 1999;92:193–198. [PubMed] [Google Scholar]
- van der Kolk BA. The body keeps the score: Approaches to the psychobiology of posttraumatic stress disorder. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic stress: The effects of overwhelming experience on mind, body, and society. Guilford Press; New York, NY: 1996. pp. 214–241. [Google Scholar]
- van der Kolk BA, McFarlane AC, van der Hart O. A general approach to treatment of posttraumatic stress disorder. In: van der Kolk BA, McFarlane AC, Weisaeth L, editors. Traumatic stress: The effects of overwhelming experience on mind, body, and society. Guilford Press; New York: 1996. pp. 417–440. [Google Scholar]
- van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PM. Single session debriefing after psychological trauma: A meta-analysis. Lancet. 2002;360:766–71. doi: 10.1016/S0140-6736(02)09897-5. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, et al. Increased consumption of cigarettes, alcohol, and marijuana among New York City residents six to nine months after the September 11th terrorists attacks. American Journal of Drug and Alcohol Abuse. 2004;30:385–407. doi: 10.1081/ada-120037384. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, et al. Increased use of cigarettes, alcohol, and marijuana among Manhattan residents after September 11 terrorist attacks. American Journal of Epidemiology. 2002;155:988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]