Abstract
Study Objectives:
To investigate prevalence, incidence, and persistence of insomnia, and their bidirectional longitudinal associations with depression and physical disorders.
Design:
A community based longitudinal study.
Setting:
Elders living in private households in South Korea.
Participants:
1204 people ≥ 65 years of age were evaluated at baseline; 909 of them (75%) were re-interviewed after 2 years.
Measurements and Results:
Insomnia was defined as difficulty in initiation or maintenance of sleep ≥ 3 nights per week over the last month. Diagnosis of depression (Geriatric Mental State) and number of physical disorders were ascertained. Sociodemographic and clinical covariates included age, gender, education, housing, past occupation, current employment, living area, life events, social deficit, physical activity, cognitive impairment, anxiety, and daily drinking. Of those (27%) with insomnia at baseline, 40% had insomnia at follow-up. Of those without insomnia at baseline, 23% had insomnia at follow-up. Baseline depression was significantly associated with prevalence and incidence of insomnia. Baseline number of physical disorders was significantly associated with prevalence, incidence, and persistence of insomnia. Baseline insomnia was independently associated with incident depression and an increase in reported physical disorders.
Conclusions:
Insomnia was common and often persistent in this population. Insomnia was closely and reciprocally related to depression and physical disorders.
Citation:
Kim JM; Stewart R; Kim SW; Yang SJ; Shin IS; Yoon JS. Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans. SLEEP 2009;32(9):1221-1228.
Keywords: Aging, depression, epidemiology, incidence, longitudinal studies, physical disease, prevalence, sleep initiation and maintenance disorders
INSOMNIA IS A COMMON SYMPTOM IN OLDER ADULTS. PREVALENCE ESTIMATES FROM EPIDEMIOLOGICAL RESEARCH HAVE RANGED FROM 20% TO 40% in elders.1–8 Insomnia prevalence has been found to be associated with measures of worse physical and mental health: for example, a higher number of medical conditions including respiratory symptoms and angina, increased physical disability, worse perceived health, and depressive symptoms.2–5,8–10 Insomnia in elders has also been found to be associated with increased age, female sex, unmarried status, lower education and lower income,3,8,11,12 although these have not been replicated in all studies.13
Cross-sectional research is limited in terms of inferring direction of cause and effect and distinguishing the extent to which associations with prevalence are accounted for by those with incidence and/or persistence of the outcome. Prospective studies of insomnia in older people have been less common, but have suggested annual incidence rate ranging from 3% to 15%,9,14,15 and annual persistence rate ranges from 5% to 30%.14–17 In one large study, incidence and persistence of insomnia in elders were found to be predicted by previous chronic disease, depressive symptoms, poor perceived health, and use of sedatives.14 Other longitudinal studies in older populations have reported similar findings.9,15
The consequences of insomnia have not often been investigated. Insomnia increased the risk of developing new major depression in the Epidemiologic Catchment Areas (ECA) study in adults aged 18 years and over.18 In 12-year and 20-year longitudinal studies in young adults, insomnia predicted subsequent depression.17,19 A recent study from the United Kingdom in adults aged 18 and over reported that insomnia at baseline was significantly associated with incidence of anxiety, depression, and widespread pain at 12-month follow-up.20 With respect to older populations, baseline insomnia has been found to be associated with future depressive episode and persistent insomnia has been suggested as a perpetuating factor for depression.21,22
Overall, longitudinal studies of insomnia in elderly populations are sparse, particularly with respect to its natural history and its associations with other psychiatric or physical conditions. In an analysis of data obtained from a longitudinal community study of an older Korean population, we investigated the epidemiology of insomnia in elders. The objectives of this analysis were: to estimate the prevalence, incidence, and persistence of insomnia over a 2-year period; and to investigate bidirectional longitudinal associations with depression and physical disorders.
METHODS
Study Population
This analysis was carried out on data from a prospective community-based study of late-life psychiatric morbidity carried out in Kwangju, South Korea from 2001 to 2003, in collaboration with the 10/66 International Research Program on dementia and late-life mental disorder in low and middle income nations.23 The study has been described in detail in several previous publications.24,25 In brief, all community residents ≥ 65 years of age within 2 geographic catchment areas (one urban, one rural) were systematically identified from national registration lists and were approached to participate at baseline. Attempts were made to follow up all participants 2 years later (mean [SD] interval 2.4 [0.3] years). All contact was made by home visits by a team of bachelor's degree-level research staff, trained and supervised by the project psychiatrist throughout the survey period. All participants gave formal informed consent at each examination. This study was approved by the Chonnam National University Hospital Institutional Review Board.
Measurements
Data on insomnia, depression, and physical disorders were obtained both at baseline and follow-up. Information on sociodemographic and other clinical factors was gathered at baseline. All data were gathered using a structured questionnaire developed by the 10/66 Dementia in Developing Countries Research Group.23
In the course of the interview, all participants were asked the following four questions: i) Do you have trouble going to sleep?; ii) Do you have trouble in staying asleep including awakening early?; iii) How often does the problem occur per week?; and iv) How long has the problem been present? Insomnia questions had a time frame of one month. Therefore, symptoms were required to be present for at least the previous month. Based on the answers to these questions, insomnia was defined as difficulty in initiation or maintenance of sleep with a frequency of 3 nights or more per week over at least the last month. In addition, sub-threshold insomnia was defined as difficulty in initiation or maintenance of sleep with a frequency of 1 or 2 nights per week over at least the last month.
Depression was assessed using the community version of the Geriatric Mental State diagnostic schedule (GMS B3).26 This is a fully structured diagnostic instrument with an accompanying computerized algorithm (AGECAT) and has been widely used in international epidemiological research for depression in older people. The instrument and algorithm are designed to diagnose depression in the last month ‘of clinical significance' – i.e. levels of psychopathology which would warrant clinical intervention. With typical community prevalence rates between 10%–20%, the GMS-AGECAT depression criterion encompasses a broader spectrum than DSM-IV major depression including both moderate and severe manifestations of the disorder as defined in ICD or DSM diagnostic systems. The GMS B3 was translated into Korean according to a formal standardized process.27 The κ value for interrater reliability was 0.84 for depression in Korea.27 As in other studies, participants rated as AGECAT 3, 4, and 5 are considered to be likely depression cases, those rated as 1 and 2 to be depression sub-cases, and those rated as 0 to have no relevant symptomatology.
General physical health was quantified by measuring the number of self-reported disorders reported in response to a structured questionnaire which enquired about the presence of 11 common and generally chronic health problems: arthritis or rheumatism; eyesight problems; hearing difficulty or deafness; persistent cough; breathlessness, difficulty breathing or asthma; high blood pressure; heart disease or angina; gastric or intestinal problems; faints or blackouts; paralysis, weakness, or loss of power in one leg or arm; and skin disorders such as pressure sores, leg ulcers, or severe burns. The questionnaire was specifically developed for evaluating global physical health in older people28 and has been used widely in previous research.29 Corroboration was sought with family informants where possible. Positive responses were totalled to generate a summary scale which was, because of the skewed distribution, divided into 4 groups (0, 1, 2∼3, 4+).
Sociodemographic data on age, gender, duration of formal education, housing (owned or rented), and past principal occupation (manual or non-manual) were obtained. Current employment was also ascertained, as there is no statutory retirement requirement in this setting and many elders continue to work. Living area was coded (rural or urban) by the address recorded in the national registration list. Life events were measured by the List of Threatening Events (LTE),30 whose validity in old age has been previously established.31 Nine life events over the previous year are enquired about: serious illness (self), serious illness (close relative), bereavement (immediate family), bereavement (other relative or close friend), marital separation, end of relationship, problem with close friend or relative, and theft or loss. Positive responses were totalled to generate a summary scale and were divided into no (0) or any (1+) recent life events. As previously applied in community research,31 six social support deficits were defined as: living alone, seeing a relative less often than once a month, seeing a friend less often than once a month, having no close friends, seeing a neighbor less often than once a month, and having no close neighbors. Individual yes/no responses were then totalled to generate a summary scale which was categorized into no (0) or any (1+) deficit. Daily physical activity, taking into account both work and leisure activity, was ascertained and sedentary lifestyle was defined as a binary variable (active or inactive).23 The “brain organicity” (cognitive impairment) output from the GMS AGECAT was included as a covariate applying the conventional confidence level ≥ 3 in the stage two algorithm to define organic disorder “caseness.”26 Anxiety caseness was defined from the GMS AGECAT anxiety score in an identical manner.26 Daily alcohol intake was estimated using a single GMS item where participants are asked whether they have a drink more or less every day, and a binary variable was generated.
Statistical Analysis
Prevalence of insomnia at baseline was measured. For analysis of insomnia incidence, the sample was restricted to those without insomnia at baseline and insomnia at follow-up was treated as a binary dependent variable. For analysis of insomnia persistence, the same analyses were carried out in those with insomnia at baseline. For cross-sectional associations, unadjusted analyses (χ2 tests) of prevalent insomnia with baseline characteristics (depression, number of physical disorder, age, gender, education, housing, past occupation, current employment, living area, life events, social deficit, physical activity, GMS organicity, GMS anxiety, and daily drinking) were carried out. For investigating predictors of incident and persistent insomnia, analyses were repeated with these baseline measures as independent variables, insomnia at follow-up as the dependent variable and stratifying according to the presence or not of baseline insomnia. Factors potentially associated with insomnia on the 3 unadjusted analyses (P < 0.10) were then entered into logistic regression models separately to investigate independence. In addition, prevalence of sub-threshold insomnia was estimated both at baseline and at follow-up. The proportions of changes in insomnia symptoms, i.e., insomnia, sub-threshold insomnia, and no insomnia, from baseline to follow-up were calculated. Any increase in insomnia symptoms was considered as another dependent variable, and the same unadjusted and adjusted analyses were repeated.
To investigate associations of insomnia with depression and physical disorders as outcomes, similar analyses were carried out. Prevalence, incidence, and persistence of depression were measured and increase in depression symptoms was considered as another dependent variable. In addition, any increase between baseline and follow-up in the number of physical disorders from the 11-point scale were identified. Associations of baseline insomnia with depression physical disorder outcomes were analyzed using χ2 tests. In previous analyses from the same sample, depression and disability were associated with all baseline sociodemographic and clinical characteristics.32,33 Therefore, logistic regression models for depression and physical disorder outcomes included all these characteristics as covariates. Statistical analyses were carried out using SPSS 12.0 software.
RESULTS
Sample Recruitment and Identification of Insomnia
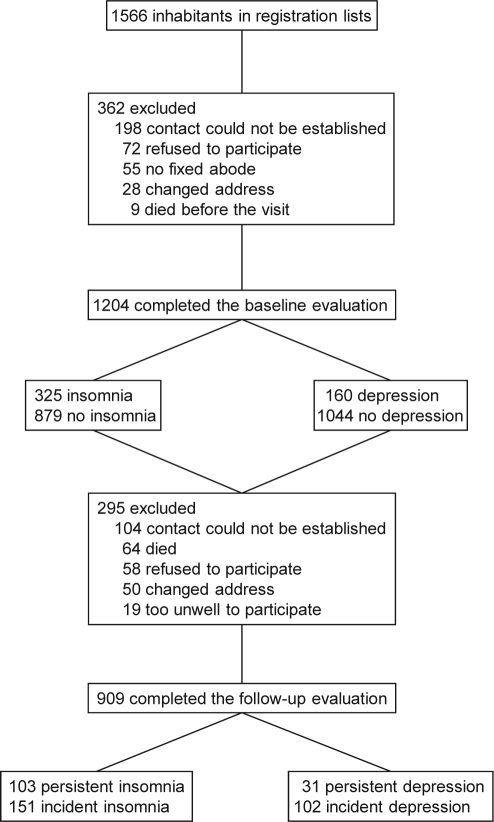
The recruitment process at baseline and sample follow-up are described in Figure 1. At baseline, participants (N = 1204) and non-participants (N = 362) did not differ significantly with respect to age (mean [SD] ages, 72.2 (5.9) and 72.4 (6.6), respectively) or gender (58% and 62% female, respectively) (all P-values > 0.1). Prevalence, incidence, and persistence of insomnia are designated in the left part of Figure 1. Insomnia was present in 325 (27%) of these 1204 participants. At follow-up, 909 (75%) were re-examined. Those present (N = 909) or not (N = 295) at follow-up were not significantly different at baseline with respect to age (mean [SD] 72.4 [5.7] and 73.0 [6.9] years, respectively), gender (58% and 59% female, respectively), or prevalence of insomnia at baseline (28% and 23%, respectively) (all P-values > 0.06). Insomnia was present in 254 (28%) of all 909 followed-up participants. Incidence of insomnia was defined in 151 (23%) of the 651 followed-up participants without baseline insomnia; and persistence of insomnia in 103 (40%) of the 258 followed-up participants with baseline insomnia.
Figure 1.
Flow diagram for baseline recruitment and sample follow-up.
Changes in insomnia symptoms from baseline to follow-up are summarized in Table 1. For the 909 participants who were successfully followed, the overall prevalence of insomnia (not including sub-threshold level) was similar at baseline (N = 258, 28%) and at follow-up (N = 254, 28%). Of 909 followed participants, insomnia symptoms were unchanged in 378 (42%), had improved in 245 (27%), and had worsened in 286 (31%).
Table 1.
Changes in Insomnia Symptoms from Baseline to Follow-Up
| Symptoms at baseline | Symptoms at follow-up (number, %) |
||
|---|---|---|---|
| No insomnia (N = 285) | Sub-threshold insomnia (N = 370) | Insomnia (N = 254) | |
| No insomnia (N = 321) | 134 (47) | 135 (37) | 52 (20) |
| Sub-threshold insomnia (N = 330) | 90 (32) | 141 (38) | 99 (39) |
| Insomnia (N = 258) | 61 (21) | 94 (25) | 103 (41) |
Unadjusted Associations with Insomnia
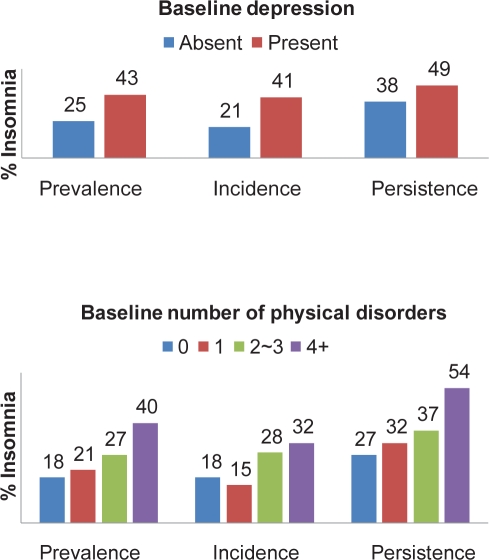
Unadjusted associations between baseline characteristics and insomnia are summarized in Figure 2 and Table 2. Prevalent insomnia was significantly associated with depression (OR [95% CI]: 2.3 [1.6–3.2]), increased number of physical disorders (OR [95% CI] per unit increase: 1.5 [1.3–1.7]), rented housing, having no current employment, urban residence, presence of social support deficits, physical inactivity, and GMS anxiety. Baseline factors significantly associated with incident insomnia (i.e. in participants without insomnia at baseline) were depression (OR [95% CI]: 2.6 [1.5–4.4]), increased number of physical disorders (OR [95% CI] per unit increase: 1.4 [1.2–1.7]), previous manual occupation, and physical inactivity. Persistence of insomnia (i.e., for participants with insomnia at baseline) was only significantly associated with increased number of physical disorders (OR [95% CI] per unit increase: 1.5 [1.2–2.0]); associations with baseline depression (OR [95% CI]: 1.6 [0.9–2.9]), previous education, and rented housing were of borderline significance (P < 0.1). Additionally, an increase in insomnia symptoms was associated with depression (OR [95% CI]: 1.8 [1.2–2.6]), increased number of physical disorders (OR [95% CI] per unit increase: 1.2 [1.0–1.4]), female sex (OR [95% CI]: 1.3 [1.0–1.8]), and previous manual occupation (OR [95% CI]: 1.7 [1.0–2.9]).
Figure 2.
Prevalence, incidence, and persistence of insomnia by baseline depression and number of physical disorders.
Table 2.
Univariate Associations of Baseline Demographic Characteristics with Prevalent, Incident, and Persistent Insomnia
| Source | Prevalence analysis |
Incidence analysis* |
Persistence analysis** |
||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % insomnia | OR (95% CI) | N | % insomnia | OR (95% CI) | N | % insomnia | OR (95% CI) | |
| All participants | 1204 | 27.0 | - | 651 | 23.2 | - | 258 | 39.9 | - |
| Age | |||||||||
| 65-74 | 800 | 26.1 | 1.0 | 443 | 21.9 | 1.0 | 167 | 43.1 | 1.0 |
| 75+ | 404 | 28.7 | 1.1 (0.9–1.5) | 208 | 26.0 | 1.3 (0.9–1.8) | 91 | 34.1 | 0.7 (0.4–1.2) |
| Gender | |||||||||
| Male | 505 | 25.3 | 1.0 | 285 | 20.7 | 1.0 | 99 | 35.4 | 1.0 |
| Female | 699 | 28.2 | 1.2 (0.9–1.5) | 366 | 25.1 | 1.3 (0.9–1.9) | 159 | 42.8 | 1.4 (0.8–2.3) |
| Duration of formal education | |||||||||
| 1+ year | 630 | 26.5 | 1.0 | 338 | 21.0 | 1.0 | 131 | 45.8 | 1.0 |
| 0 year | 574 | 27.5 | 1.1 (0.8–1.4) | 313 | 25.6 | 1.3 (0.9–1.9) | 127 | 33.9 | 0.6 (0.4–1.1) |
| Housing | |||||||||
| Owned | 1096 | 26.2 | 1.0 | 604 | 22.5 | 1.0 | 231 | 38.1 | 1.0 |
| Rented | 108 | 35.2 | 1.5 (1.0–2.3) | 47 | 31.9 | 1.6 (0.9–3.1) | 27 | 55.6 | 2.0 (0.9–4.5) |
| Past occupation | |||||||||
| Non-manual | 121 | 24.0 | 1.0 | 61 | 9.8 | 1.0 | 20 | 30.0 | 1.0 |
| Manual | 1083 | 27.3 | 1.2 (0.8–1.9) | 590 | 24.6 | 3.0 (1.3–7.1) | 238 | 40.8 | 1.6 (0.6–4.3) |
| Current employment | |||||||||
| Yes | 542 | 23.8 | 1.0 | 322 | 21.1 | 1.0 | 107 | 44.9 | 1.0 |
| No | 662 | 29.6 | 1.4 (1.0–1.7) | 329 | 25.2 | 1.3 (0.9–1.8) | 151 | 36.4 | 0.7 (0.4–1.2) |
| Living area | |||||||||
| Rural | 746 | 23.7 | 1.0 | 445 | 21.6 | 1.0 | 147 | 40.8 | 1.0 |
| Urban | 458 | 32.3 | 1.5 (1.2–2.0) | 206 | 25.8 | 1.3 (0.9–1.7) | 111 | 38.7 | 0.9 (0.6–1.5) |
| Recent life events | |||||||||
| No | 303 | 25.0 | 1.0 | 175 | 21.5 | 1.0 | 55 | 34.1 | 1.0 |
| Yes | 901 | 31.2 | 1.4 (0.9–1.8) | 476 | 23.0 | 1.1 (0.7–1.7) | 203 | 40.8 | 1.3 (0.6–2.7) |
| Social support deficit | |||||||||
| No | 363 | 21.2 | 1.0 | 219 | 20.1 | 1.0 | 67 | 35.8 | 1.0 |
| Yes | 841 | 29.0 | 1.5 (1.1–2.0) | 432 | 24.9 | 1.3 (0.9–2.0) | 191 | 42.2 | 1.3 (0.7–2.3) |
| Physical activity | |||||||||
| Active | 852 | 22.7 | 1.0 | 488 | 21.3 | 1.0 | 165 | 37.3 | 1.0 |
| Inactive | 352 | 34.4 | 1.8 (1.4–2.3) | 163 | 30.1 | 1.6 (1.1–2.4) | 93 | 45.2 | 1.4 (0.9–2.3) |
| GMS organicity | |||||||||
| No | 811 | 25.8 | 1.0 | 448 | 22.1 | 1.0 | 166 | 39.8 | 1.0 |
| Yes | 393 | 29.5 | 1.2 (0.9–1.6) | 203 | 25.6 | 1.2 (0.8–1.8) | 92 | 40.2 | 1.0 (0.6–1.7) |
| GMS anxiety | |||||||||
| No | 1180 | 26.5 | 1.0 | 642 | 23.1 | 1.0 | 248 | 39.1 | 1.0 |
| Yes | 24 | 50.0 | 2.8 (1.2–6.2) | 9 | 33.3 | 1.7 (0.4–6.8) | 10 | 60.0 | 2.3 (0.6–8.5) |
| Daily drinking | |||||||||
| No | 946 | 24.6 | 1.0 | 505 | 23.0 | 1.0 | 199 | 40.3 | 1.0 |
| Yes | 258 | 28.3 | 1.2 (0.9–1.6) | 146 | 24.7 | 1.1 (0.7–1.7) | 59 | 42.4 | 1.1 (0.6–2.0) |
Sample restricted to participants with no insomnia at baseline.
Sample restricted to participants with insomnia at baseline.
GMS: Geriatric Mental State schedule.
Adjusted Associations with Insomnia
Adjusted associations from logistic regression models between baseline characteristics (simultaneously entered into regression models) and insomnia are summarized in Table 3. Prevalent insomnia was independently associated with depression, four or more number of physical disorders, and social support deficit. Incident insomnia was independently associated with depression, four or more physical disorders, and previous manual occupation. Persistent insomnia was independently associated with ≥ 4 physical disorders even after adjustment for depression. The association with depression appeared stronger for incidence compared to persistence of insomnia. An increase in insomnia symptoms was independently associated with depression and ≥ 4 physical disorders. With respect to the 11 individual physical disorders, all reported disorders apart from skin disorders were significantly and independently associated with prevalent insomnia; eyesight problems and hearing difficulty were independently associated with insomnia incidence; and heart disease and gastrointestinal problems were independently associated with insomnia persistence.
Table 3.
Multivariate Associations of Baseline Characteristics with Prevalent, Incident, and Persistent Insomnia
| Independent variable | Associations with insomnia outcomes (OR, 95% CI) |
|||
|---|---|---|---|---|
| Prevalence | Incidence | Persistence | Symptom increase | |
| Depression (present) | 1.7 (1.1–2.4) | 2.4 (1.4–4.2) | 1.2 (0.6–2.4) | 1.6 (1.0–2.4) |
| Number of physical disorders | ||||
| 0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 1 | 1.0 (0.7–1.7) | 0.7 (0.4–1.4) | 1.5 (0.5–4.1) | 1.1 (0.7–1.8) |
| 2-3 | 1.5 (0.9–2.3) | 1.7 (0.9–3.0) | 1.6 (0.6–4.1) | 1.2 (0.8–1.9) |
| 4+ | 2.3 (1.4–3.6) | 1.8 (1.0–3.5) | 3.1 (1.2–8.1) | 1.6 (1.0–2.5) |
| Gender (female) | - | - | - | 1.2 (0.9–1.6) |
| Previous education (absent) | - | - | 0.6 (0.4–1.1) | - |
| Housing (rented) | 1.1 (0.7–1.7) | - | 1.6 (0.7–3.6) | - |
| Past occupation (manual) | - | 2.9 (1.2–6.9) | - | 1.5 (0.9–2.7) |
| Current employment (not employed) | 1.1 (0.8–1.5) | - | - | - |
| Living area (urban) | 1.2 (0.9–1.7) | - | - | - |
| Social support deficit (present) | 1.5 (1.1–2.0) | - | - | - |
| Physical activity (inactive) | 1.2 (0.9–1.6) | 1.1 (0.7–1.8) | - | - |
| GMS anxiety (present) | 1.4 (0.6–3.4) | - | - | - |
GMS: Geriatric Mental State Schedule.
Associations of Insomnia with Depression and Physical Disorders
Prevalence, incidence, and persistence of depression are described in the right part of Figure 1. Depression was present in 160 (13%) of 1204 participants at baseline. Incident depression was present in 102 (13%) of 792 followed-up participants without baseline depression; and persistent depression was present in 31 (26%) of the 117 followed-up participants with baseline depression. Depression sub-caseness were present 245 (20%) of 1204 baseline participants, and 208 (23%) of 909 followed-up participants. Of 909 followed-up participants, depression symptom scores were unchanged in 340 (38%), had improved in 240 (26%), and had worsened in 286 (36%). An increase in the number of reported physical disorders was present in 241 (27%) of 909 total followed-up participants (with complete data on physical health status at both baseline and follow-up). Associations of baseline insomnia with depression outcomes and increased physical disorders are summarized in Table 4. Baseline insomnia was significantly associated with prevalent and incident depression, with an increase in number of depression symptoms, and an increase in number of reported physical disorders before and after adjustment for sociodemographic and clinical characteristics. In addition, persistence of insomnia was strongly associated with incidence of depression over the same period (OR [95% CI] = 2.4 [1.3–4.2]) after adjustment.
Table 4.
Associations of Baseline Insomnia with Depression Outcomes and an Increase in Reported Physical Disorders
| Outcome (sample size of analysis) | Association of insomnia with specified outcome* |
|
|---|---|---|
| (odds ratio, 95% CI) | ||
| Unadjusted | Adjusted | |
| Prevalent depression (N = 1204) | 2.3 (1.6–3.2) | 2.1 (1.5–3.0) |
| Incident depression (N = 792) | 1.7 (1.1–2.7) | 1.8 (1.2–2.9) |
| Persistent depression (N = 117) | 1.6 (0.7–3.5) | 1.5 (0.6–3.7) |
| Increase in depression symptoms (N = 909) | 1.4 (1.0–1.8) | 1.4 (1.0–1.9) |
| Increase in reported physical disorders (N = 909) | 1.4 (1.0–1.9) | 1.4 (1.0–2.0) |
Adjusted for age, gender, education, housing, past occupation, current employment, living area, life events, social deficit, physical activity, GMS organicity, GMS anxiety, and daily drinking.
DISCUSSION
The principal findings of this 2-year longitudinal study of community elders were that prevalence, incidence, and persistence of insomnia were 27%, 23%, and 40%, respectively; that baseline depression was associated with prevalent and incident insomnia; that baseline higher number of physical disorders was associated with prevalent, incident and persistent insomnia; and that baseline insomnia was an independent risk factor for incident depression and an increase in reported physical disorders.
A particular strength of the present study was the longitudinal design which made it possible to investigate both the course of insomnia (and factors predicting this) and longitudinal associations of insomnia with changes in mental and physical health. Although a large volume of research has described and investigated the prevalence and cross-sectional correlates of insomnia, such studies have limited ability to infer causal relationships between associated factors. To our knowledge, this is the first study in an older community population to report factors predicting the incidence and persistence of insomnia as well as insomnia as a risk factor for other health-related changes. In particular, the association between depression and insomnia has been reported repeatedly in cross-sectional studies of elders,2–5,9 but has received relatively little longitudinal research. The relationship between the two is complex because insomnia is considered to be a symptom contributing to a diagnosis of depression and contributes one or more items in many depression screening scales. However, some findings suggest that they may be considered as separate entities, for example, as predictors of disability pension award.34 Cross-sectional associations clearly cannot be used to infer the direction of cause and effect between them. An 8-year longitudinal study of 1042 elderly people found that depressed mood and worse physical health were major risk factors for incident insomnia.9 In a 3-year longitudinal study of 6800 elders, depression was found to be associated with both the development and remission of insomnia symptoms.14 Similarly, another 1∼4 year longitudinal study of 4467 US elders found that depression was the primary factor predicting the incidence of insomnia.15 In our study, baseline depression was a predictor of incidence, but its association with persistence was substantially weaker and not statistically significant. This finding is consistent with a recent study of 2363 adults aged 18 and over where baseline depression was also associated with incident but not with persistent insomnia.20
There have been relatively few studies on the consequences of insomnia in any population and, to our knowledge, no previous research specifically in an older sample. With respect to depression, insomnia predicted its incidence over a 2-year follow-up period. This finding was similar to those from younger adult populations,17–20 as well as from other older cohorts.21,22 Furthermore, persistence insomnia was strongly associated with incident depression, which also supports previous findings in younger and older adults.18,19,21,22
Other strengths were that this study was community-based with a reasonably large sample size and reasonable follow-up rate, that there was no substantial differential attrition with respect to risk factors of interest, and that data were derived from instruments proven to be valid in older populations. An important limitation was that physical disorders were identified through self-report or treatment history, so that reporting bias could have arisen. However, the participants were blind to the objectives of this analysis and the interviewers were blind to depression case status. Therefore we do not believe that misclassification bias, if present, would have substantially altered the principal findings of the study. Another limitation was that data on service utilization or treatment for the insomnia, depression, and physical disorders were not available, which may have been unmeasured confounding factors. The sample was drawn from a specific community, and representativeness with respect to other Korean populations or elder populations elsewhere cannot be assumed. However, we are not aware of any specific cultural factors which are likely to have a substantial influence on the outcomes or associations in question.
To compare the occurrence of insomnia between studies is difficult because of differences in definitions of insomnia and survey methodologies. For the purpose of this analysis, insomnia was defined as difficulty in initiation or maintenance of sleep with a frequency of three nights or more per week over the last month. A recent study of Chinese elderly with the same definition reported a prevalence of 33%.8 Studies with similar definitions (difficulty in initiation or maintenance of sleep most of the time) have reported 25∼33% prevalence rates in Caucasian and Asian populations.2,6,35 In our study, insomnia prevalence estimates were 27% and 28% at baseline and follow-up, respectively, which are therefore similar to those in other samples. Studies using a similar definition in general adult populations have reported 15∼22% prevalence,36–38 lower than findings from older populations. A previous study in 3719 Korean adults aged 15 or older (including 116 elders) employing a similar definition reported a prevalence of 17%,39 again supporting other findings of higher insomnia prevalence in elders.40–42 The incidence and persistence of insomnia were 27% and 23%, respectively over the 2.4 year period of our study. Overall, our findings support the notion that insomnia is a common and frequently chronic problem across a variety of populations. Incidence and persistence in studies of this sort are clearly only approximate concepts since participants' status in between examination points is not known. Because the study only measured the one-month period prevalence of insomnia at baseline and at follow-up, incidence is likely to be under-estimated since some new cases may have occurred during the 2.4-year interval which remitted before the follow-up examination. Persistence on the other hand may be over-estimated since some cases with insomnia at both baseline and follow-up may have remitted in between. As with depression in older people, there is a need for more in-depth examination with more frequent examinations to characterize better the course of this syndrome.
Epidemiological studies of older populations have repeatedly found both cross-sectional and longitudinal associations between worse general health and insomnia.2,10,14,15 In particular, two studies reported that increased number of physical conditions were associated with incident as well as persistent insomnia.14,15 In our study, a higher number of physical disorders was one of the predictors of incident insomnia, and was the only predictor of insomnia persistence. Older samples obviously contain high numbers of people with chronic physical disorders: for example, over 80% of persons aged 65 or over reported at least one chronic physical disorder in one study.43 In the Kwangju sample, this proportion was 82%. Therefore, the well-recognized associations between physical disorders and insomnia have particular public health relevance in the older age groups and our findings suggest that evaluation of interventions to improve physical health and its disabling consequences should be considered both to prevent the development of insomnia and reduce the risk of it persisting.
In this study, insomnia was also a predictor of worsening health. This was defined relatively crudely as an increase in the number of physical conditions reported and there was no information encompassing the severity or relative salience of individual conditions; there is also, to our knowledge, no research into the test-retest reliability of such a scale. However these sources of inaccuracy are unlikely to have been differential with respect to insomnia status and would therefore have obscured rather than exaggerated true associations. The associations persisted with little alteration in strength after adjustment for a variety of potential confounding factors.
In conclusion, the analysis of longitudinal data described here found two-way reciprocal relationships between insomnia, depression, and physical disorders in late-life. That is to say, both depression and physical disorders were predictors of insomnia, and insomnia was also found to predict incident depression and worsening physical health. These results support the hypothesis that insomnia is closely inter-related with mental as well as physical health in elders, and that appropriate and prompt management of one of the problems, or when one of them first presents, may reduce the onset and/or comorbidity of other problems. Further research in this area may be best focused on older people, because they are at particular high risk for all three disorder profiles.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Health 21 R&D, Ministry of Health and Welfare, Republic of Korea (A050047). RS is funded by NIHR Biomedical Research Centre for Mental Health, The South London and Maudsley NHS Foundation Trust – The Institute of Psychiatry, King's College London.
REFERENCES
- 1.Blazer DG, Hays JC, Foley DJ. Sleep complaints in older adults: a racial comparison. J Gerontol A Biol Sci Med Sci. 1995;50:M280–4. doi: 10.1093/gerona/50a.5.m280. [DOI] [PubMed] [Google Scholar]
- 2.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 3.Newman AB, Enright PL, Manolio TA, Haponik EF, Wahl PW. Sleep disturbance, psychosocial correlates, and cardiovascular disease in 5201 older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 1997;45:1–7. doi: 10.1111/j.1532-5415.1997.tb00970.x. [DOI] [PubMed] [Google Scholar]
- 4.Maggi S, Langlois JA, Minicuci N, et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc. 1998;46:161–8. doi: 10.1111/j.1532-5415.1998.tb02533.x. [DOI] [PubMed] [Google Scholar]
- 5.Chiu HF, Leung T, Lam LC, et al. Sleep problems in Chinese elderly in Hong Kong. Sleep. 1999;22:717–26. doi: 10.1093/sleep/22.6.717. [DOI] [PubMed] [Google Scholar]
- 6.Barbar SI, Enright PL, Boyle P, et al. Sleep disturbances and their correlates in elderly Japanese American men residing in Hawaii. J Gerontol A Biol Sci Med Sci. 2000;55:M406–11. doi: 10.1093/gerona/55.7.m406. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: consequences for older people. J Am Geriatr Soc. 2001;49:360–6. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- 8.Liu X, Liu L. Sleep habits and insomnia in a sample of elderly persons in China. Sleep. 2005;28:1579–87. [PubMed] [Google Scholar]
- 9.Morgan K, Clarke D. Risk factors for late-life insomnia in a representative general practice sample. Br J Gen Pract. 1997;47:166–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Morgan K, Dallosso H, Ebrahim S, Arie T, Fentem PH. Characteristics of subjective insomnia in the elderly living at home. Age Ageing. 1988;17:1–7. doi: 10.1093/ageing/17.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Habte-Gabr E, Wallace RB, Colsher PL, Hulbert JR, White LR, Smith IM. Sleep patterns in rural elders: demographic, health, and psychobehavioral correlates. J Clin Epidemiol. 1991;44:5–13. doi: 10.1016/0895-4356(91)90195-f. [DOI] [PubMed] [Google Scholar]
- 13.Henderson S, Jorm AF, Scott LR, Mackinnon AJ, Christensen H, Korten AE. Insomnia in the elderly: its prevalence and correlates in the general population. Med J Aust. 1995;162:22–4. doi: 10.5694/j.1326-5377.1995.tb138406.x. [DOI] [PubMed] [Google Scholar]
- 14.Foley DJ, Monjan AA, Izmirlian G, Hays JC, Blazer DG. Incidence and remission of insomnia among elderly adults in a biracial cohort. Sleep. 1999;22(Suppl 2):S373–8. [PubMed] [Google Scholar]
- 15.Quan SF, Katz R, Olson J, et al. Factors associated with incidence and persistence of symptoms of disturbed sleep in an elderly cohort: the Cardiovascular Health Study. Am J Med Sci. 2005;329:163–72. doi: 10.1097/00000441-200504000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Ganguli M, Reynolds CF, Gilby JE. Prevalence and persistence of sleep complaints in a rural older community sample: the MoVIES project. J Am Geriatr Soc. 1996;44:778–84. doi: 10.1111/j.1532-5415.1996.tb03733.x. [DOI] [PubMed] [Google Scholar]
- 17.Mallon L, Broman JE, Hetta J. Relationship between insomnia, depression, and mortality: a 12-year follow-up of older adults in the community. Int Psychogeriatr. 2000;12:295–306. doi: 10.1017/s1041610200006414. [DOI] [PubMed] [Google Scholar]
- 18.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 19.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Röossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 21.Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: a prospective perspective. Am J Psychiatry. 2000;157:81–8. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- 22.Pigeon WR, Hegel M, Unöutzer J, et al. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep. 2008;31:481–8. doi: 10.1093/sleep/31.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prince M, Acosta D, Chiu H, Scazufca M, Varghese M 10/66 Dementia Research Group. Dementia diagnosis in developing countries: a cross-cultural validation study. Lancet. 2003;361:909–17. doi: 10.1016/S0140-6736(03)12772-9. [DOI] [PubMed] [Google Scholar]
- 24.Kim JM, Stewart R, Shin IS, Yoon JS. Vascular disease / risk and late-life depression in a Korean community population. Br J Psychiatry. 2004;185:102–7. doi: 10.1192/bjp.185.2.102. [DOI] [PubMed] [Google Scholar]
- 25.Kim JM, Stewart R, Kim SW, Shin IS, Yang SJ, Yoon JS. Vascular risk factors and incident late-life depression in a Korean population. Br J Psychiatry. 2006;189:26–30. doi: 10.1192/bjp.bp.105.015032. [DOI] [PubMed] [Google Scholar]
- 26.Copeland JRM, Dewey ME, Griffiths-Jones HM. A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and AGECAT. Psychol Med. 1986;16:89–99. doi: 10.1017/s0033291700057779. [DOI] [PubMed] [Google Scholar]
- 27.Kim JM, Stewart R, Prince M, Shin IS, Yoon JS. Diagnosing dementia in a developing nation: an evaluation of the GMS-AGECAT algorithm in an older Korean population. Int J Geriatr Psychiatry. 2003;18:331–6. doi: 10.1002/gps.834. [DOI] [PubMed] [Google Scholar]
- 28.Lindesay J. The Guy's/Age Concern Survey: physical health and psychiatric disorder in an urban elderly community. Int J Geriatr Psychiatry. 1990;5:171–8. [Google Scholar]
- 29.Prince MJ, Harwood RH, Blizard RA, Thomas A, Mann AH. Impairment, disability and handicap as risk factors for depression in old age. The Gospel Oak Project V. Psychol Med. 1997;27:311–21. doi: 10.1017/s0033291796004473. [DOI] [PubMed] [Google Scholar]
- 30.Brugha TS, Bebbington P, Tennant C, Hurry J. The list of threatening experiences: a subset of 12 life events categories with considerable long-term contextual threat. Psychol Med. 1985;15:323–32. doi: 10.1017/s003329170002105x. [DOI] [PubMed] [Google Scholar]
- 31.Prince MJ, Harwood RH, Blizard RA, Thomas A, Mann AH. Social support deficits, loneliness and ife events as risk factors for depression in old age. The Gospel Oak Project VI. Psychol Med. 1997;27:323–32. doi: 10.1017/s0033291796004485. [DOI] [PubMed] [Google Scholar]
- 32.Kim JM, Stewart R, Shin IS, Yoon JS, Lee HY. Lifetime urban/rural residence, social support and late-life depression in Korea. Int J Geriatr Psychiatry. 2004;19:843–51. doi: 10.1002/gps.1175. [DOI] [PubMed] [Google Scholar]
- 33.Kim JM, Stewart R, Glozier N, et al. Physical health, depression and cognitive function as correlates of disability in an older Korean population. Int J Geriatr Psychiatry. 2005;20:160–7. doi: 10.1002/gps.1266. [DOI] [PubMed] [Google Scholar]
- 34.Overland S, Glozier N, Sivertsen B, et al. A comparison of insomnia and depression as predictors of disability pension. The HUNT Study. Sleep. 2008;31:875–80. doi: 10.1093/sleep/31.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cricco M, Simonsick EM, Foley DJ. The impact of insomnia on cognitive functioning in older adults. J Am Geriatr Soc. 2001;49:1185–9. doi: 10.1046/j.1532-5415.2001.49235.x. [DOI] [PubMed] [Google Scholar]
- 36.Janson C, Gislason T, De Backer W, et al. Prevalence of sleep disturbances among young adults in three European countries. Sleep. 1995;18:589–97. [PubMed] [Google Scholar]
- 37.Hetta J, Broman JE, Mallon L. Evaluation of severe insomnia in the general population--implications for the management of insomnia: insomnia, quality of life and healthcare consumption in Sweden. J Psychopharmacol. 1999;13(Suppl 1):S35–6. doi: 10.1177/026988119901304S10. [DOI] [PubMed] [Google Scholar]
- 38.Doi Y, Minowa M, Okawa M, Uchiyama M. Prevalence of sleep disturbance and hypnotic medication use in relation to sociodemographic factors in the general Japanese adult population. J Epidemiol. 2000;10:79–86. doi: 10.2188/jea.10.79. [DOI] [PubMed] [Google Scholar]
- 39.Ohayon M, Hong SC. Prevalence of insomnia and associated factors in South Korea. J Psychosom Res. 2002;53:593–600. doi: 10.1016/s0022-3999(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 40.Ohayon M. Epidemiological study on insomnia in the general population. Sleep. 1996;19(Suppl):S7–15. doi: 10.1093/sleep/19.suppl_3.s7. [DOI] [PubMed] [Google Scholar]
- 41.Leger D, Guilleminault C, Dreyfus JP, Delahaye C, Paillard M. Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res. 2000;9:35–42. doi: 10.1046/j.1365-2869.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 42.Stewart R, Besset A, Bebbington P, et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29:1391–7. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]
- 43.Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276:1473–9. [PubMed] [Google Scholar]