Abstract
Background
Burkholderia pseudomallei is intrinsically resistant to aminoglycosides and macrolides, mostly due to AmrAB-OprA efflux pump expression. We investigated the molecular mechanisms of aminoglycoside susceptibility exhibited by Thai strains 708a, 2188a, and 3799a.
Methodology/Principal Findings
qRT-PCR revealed absence of amrB transcripts in 708a and greatly reduced levels in 2188a and 3799a. Serial passage on increasing gentamicin concentrations yielded 2188a and 3799a mutants that became simultaneously resistant to other aminoglycosides and macrolides, whereas such mutants could not be obtained with 708a. Transcript analysis showed that the resistance of the 2188a and 3799a mutants was due to upregulation of amrAB-oprA expression by unknown mechanism(s). Use of a PCR walking strategy revealed that the amrAB-oprA operon was missing in 708a and that this loss was associated with deletion of more than 70 kb of genetic material. Rescue of the amrAB-oprB region from a 708a fosmid library and sequencing showed the presence of a large chromosome 1 deletion (131 kb and 141 kb compared to strains K96243 and 1710b, respectively). This deletion not only removed the amrAB-oprA operon, but also the entire gene clusters for malleobactin and cobalamin synthesis. Other genes deleted included the anaerobic arginine deiminase pathway, putative type 1 fimbriae and secreted chitinase. Whole genome sequencing and PCR analysis confirmed absence of these genes from 708a. Despite missing several putative virulence genes, 708a was fully virulent in a murine melioidosis model.
Conclusions/Significance
Strain 708a may be a natural candidate for genetic manipulation experiments that use Select Agent compliant antibiotics for selection and validates the use of laboratory-constructed Δ(amrAB-oprA) mutants in such experiments.
Author Summary
Burkholderia pseudomallei is the etiologic agent of melioidosis, an emerging tropical disease. Because of low infectious dose, broad-host-range infectivity, intrinsic antibiotic resistance and historic precedent as a bioweapon, B. pseudomallei was listed in the United States as a Select Agent and Priority Pathogen of biodefense concern by the US Centers for Disease Control and Prevention and the National Institute of Allergy and Infectious Diseases. The mechanisms governing antibiotic resistance and/or susceptibility and virulence in this bacterium are not well understood. Most clinical and environmental B. pseudomallei isolates are highly resistant to aminoglycosides, but susceptible variants do exist. The results of our studies with three such variants from Thailand reveal that lack of expression or deletion of an efflux pump is responsible for this susceptibility. The large deletion present in one strain not only removes an efflux pump but also several putative virulence genes, including an entire siderophore gene cluster. Despite this deletion, the strain is fully virulent in an acute mouse melioidosis model. In summary, our findings shed light on mechanisms of antibiotic resistance and pathogenesis. They also validate the previously advocated use of laboratory-constructed, aminoglycoside susceptible efflux pump mutants in genetic manipulation experiments.
Introduction
Melioidosis is a disease caused by Burkholderia pseudomallei [1],[2]. Melioidosis is endemic to tropical and subtropical regions of the world [3] and is considered an emerging disease (e.g. NE Thailand [4]) as well as a disease of biodefense importance [4]. Melioidosis has received worldwide popular attention in the wake of the 2004 SE Asia Tsunami disaster [5],[6],[7],[8]. Treatment of melioidosis is complicated by the intrinsic resistance of B. pseudomallei to many antibiotics, including aminoglycosides, macrolides, several penicillins, and first and second generation cephalosporins [1],[2],[9]. Factors complicating drug therapy are the ability of B. pseudomallei to form biofilms [10] and to enter into prolonged, presumably intracellular, latency periods of up to six decades in a human host [11].
Genome sequence analysis has provided an indication of possible mechanisms of resistance to antimicrobial compounds, but less than a handful of resistance genes have been experimentally confirmed to date [12]. The K96243 and other B. pseudomallei genomes encode an arsenal of efflux pumps, including 10 pumps belonging to the resistance nodulation cell division (RND) family, which play major roles in clinically significant antibiotic resistance in Gram-negative bacteria. Two of these, AmrAB-OprA [13] and BpeAB-OprB [14] were reported to play major roles in high-level resistance to aminoglycosides and macrolides, but our unpublished results with strain 1026b indicate that BpeAB-OprB does not efflux aminoglycosides. Using a surrogate Pseudomonas aeruginosa strain we recently showed that BpeEF-OprC extrudes chloramphenicol and trimethoprim [15]. While the majority of clinical B. pseudomallei isolates exhibit high levels of aminoglycoside and macrolide resistance, rare (∼1∶1000) isolates are susceptible to these antibiotics. It has been noted that the resistance profile of these isolates matches that of amrAB-oprA mutants suggesting possible involvement of AmrAB-OprA in intrinsic aminoglycoside and macrolide resistance or lack thereof [16], but this has not yet been experimentally demonstrated. In this report we provide evidence that the susceptibility of three isolates from NE Thailand is indeed due to lack of, or greatly reduced, AmrAB-OprA expression, either due to deletion or as to as yet unknown mechanisms. Furthermore, deletion of an ∼131 kb region of chromosome 1 in one strain not only removed amrAB-OprA, but also genes encoding several putative virulence factors and other functions implicated in bacterial pathogenesis and physiology.
Materials and Methods
Bacterial strains, media and growth conditions
B. pseudomallei strains used in this study are listed in Table 1 . Escherichia coli strains used for cloning experiments were DH5α [17] or DH5α(λpir) (laboratory strain). All bacteria were routinely grown with aeration at 37°C. Low salt (5 g/L NaCl) Lennox LB broth (LSLB) and agar (MO BIO Laboratories, Carlsbad, CA) were used as rich media. M9 medium [18] with 10 mM glucose was used as the minimal medium. Unless otherwise noted, antibiotics were added at the following concentrations: 100 µg/ml ampicillin (Ap), 12.5 µg/ml chloramphenicol (Cm), 15 µg/ml gentamicin (Gm), 35 µg/ml kanamycin (Km) and 25 µg/ml zeocin (Zeo) for E. coli; 1,000 µg/ml Km and 2,000 µg/ml Zeo for wild-type B. pseudomallei and 50 µg/ml for Gm susceptible B. pseudomallei strains. Antibiotics were either purchased from Sigma, St. Louis, MO (ampicillin, chloramphenicol, erythromycin, kanamycin, polymyxin B and streptomycin), EMD Biosciences, San Diego, CA (gentamicin), Invitrogen, Carlsbad, CA (zeocin) or Biomol via VWR International, West Chester, PA (spectinomycin).
Table 1. Strains, plasmids and primers used in this study.
| Strain or Plasmid | Relevant Propertiesa | Reference or Source |
| B. pseudomallei | ||
| 1026b | AG and ML resistant wild-type strain; clinical isolate | [45] |
| DD503 | AG and ML susceptible Δ(amrR-amrAB-oprA)1026b derivative | [13] |
| 708a | AG and ML susceptible clinical isolate | [16] |
| 2188a | AG and ML susceptible clinical isolate | [16] |
| 3799a | AG and ML susceptible clinical isolate | [16] |
| Bp24 | Spontaneous AG and ML resistant derivative of 3799a | This study |
| Bp35 | Spontaneous AG and ML resistant derivative of 2188a | This study |
| Bp50 | 1026b with Δ(amrR-amrAB-oprA) | [20] |
| Bp66 | Low level Gmr derivative of 708a | This study |
| Bp187 | Bp24 with Δ(amrR-amrRAB-oprA) | This study |
| Bp202 | Bp187::mini-Tn7T-LAC | This study |
| Bp194 | Bp187::mini-Tn7T-LAC-amrA + B +-oprA + | This study |
| Bp192 | Bp35 with Δ(amrR-amrAB-oprA) | This study |
| Bp201 | Bp192::mini-Tn7T-LAC | This study |
| Bp200 | Bp192::mini-Tn7T-LAC-amrA + B +-oprA + | This study |
| Plasmids | ||
| pEX-S12pheS | Gmr; gene replacement vector | Lopez and Schweizer, unpublished |
| pUC18T-mini-Tn7T-LAC | Apr, Gmr; mini-Tn7 cloning and delivery vector | [46] |
| pPS2142 | Apr, Gmr; pUC18T-miniTn7T-LAC with amrA+B+-oprA+; amrAB-oprA expression under Ptac b control | [20] |
| pTNS3 | Apr; source of Tn7 transposase components TnsABCD | [20] |
| pFKM2 | Apr Kmr; source of FRT-nptII-FRT cassette | [20] |
| pFLPe2b | Zeor; source of Flpe recombinase | [20] |
| pPS1927 | Apr; pWSK29 [47] with ∼15 kb strain 1026b chromosomal EcoRI fragment containing amrA+B+-oprA+ | This study |
| pPS2282 | Apr; pGEM-T Easy (Novagen) with ∼3.1 kb PCR fragment containing Δ(amrAB-OprA)::FRT-nptII-FRT t | This Study |
| pPS2354 | Gmr Kmr; pEX-S12pheS with ∼3.1 kb blunt-ended EcoRI fragment of pPS2282 cloned into the SmaI site | This Study |
| Primers c | ||
| 597 | 5′-CGAATTGGGGATCTTGAAGTTCCT | This study |
| 1546 | 5′-TACATGGCGATAGCTAGACTGG | This study |
| 1599 | 5′-CGCGCGCAATTGTTCCTC | This study |
| 1600 | 5′-TCGTAAGAAAGCGACACGCA | This study |
| 1601 | 5′-CGATTCTTCGCGCGTCTTG | This study |
| 1602 | 5′-CGCGTGCGTGCCCATTCG | This study |
| 1742 | 5′-AAGACCGCGCTCTATTACGA | This study |
| 1743 | 5′-TCGTCACCGTATCAGTGCAT | This study |
| 1756 | 5′-ATCTTGCCGTTGAAGTGTCC | This study |
| 1757 | 5′-ATCGCTGAACACGAAGAACC | This study |
| 1774 | 5′-ACTAGTAGTGAGCGCAACGCAATTA | This study |
| 1779 | 5′-GCCTCTTCGCTATTACGC | This study |
| 1797 | 5′-GTTCGTCGCCGAGGAGT | This study |
| 1801 | 5′-GAAGCCGGTGAAATCGACG | This study |
| 1954 | 5′-CTCAAGTCGGTGTCCATTCC | This study |
| 1955 | 5′-ACGTTATCCGGCGTGATCT | This study |
| 2031 | 5′-CCTGGTTCACCTGCTCGATG | This study |
| 2032 | 5′-CTTCGTCGCTGCAAGAAACG | This study |
| 2033 | 5′-CGATCGACCTGCCTGAAACC | This study |
| 2034 | 5′-AGCTCGTCGTGAACACGGC | This study |
| 2035 | 5′-GACGTAATGGAACGACGCGC | This study |
| 2036 | 5′-CGTCGGCGCATTGAACGACA | This study |
| 2037 | 5′-CGATTCGTACATCGCGGCGA | This study |
| 2038 | 5′-CTCAACTTCACGGGCGAGAT | This study |
Abbreviations: AG, aminoglycosides; Ap, ampicillin; Gm, gentamicin; Km, kanamycin; ML, macrolides; r, resistance; Zeo, zeocin.
Ptac, E. coli lac/trp operon hybrid promoter.
Only selected primers are shown; other primer sequences are available from the authors upon request. Oligonucleotides were purchased from IDT, Coralville, IA.
DNA and genetic methods
Published procedures were employed for manipulation of DNA, and transformation of E. coli and B. pseudomallei [19],[20],[21]. Plasmid DNAs were isolated from E. coli and B. pseudomallei using the QIAprep Mini-spin kit (Qiagen, Valencia, CA). Colony PCR with B. pseudomallei was performed as previously described [20]. B. pseudomallei chromosomal DNA was isolated using the Gentra Puregene DNA purification kit (Qiagen). Custom oligonucleotides were synthesized by Integrated DNA Technologies (Coralville, IA). Isolation of chromosomally-integrated mini-Tn7 elements followed by Flp-mediated selection marker excision was performed using recently published procedures [20]. Quantitative real-time PCR was performed using the methods and primer sets described by Kumar et al. [22]. Other primer sequences are shown in Table 1 . Total RNA was extracted from cells grown to late log phase (optical density at 600 nm ∼0.7) in LSLB medium without antibiotics using the RNeasy Mini Kit (Qiagen).
Mutant construction
For isolation of Δ(amrR-amrAB-oprA) mutants, three partially overlapping DNA fragments representing flanking DNA segments and the Kmr marker were PCR-amplified from 50 ng pPS1927 and pFKM2 [20] DNA templates and then spliced together by an overlap extension PCR. To do this, the following fragments were amplified in a first-round PCR using Platinum Taq HiFi DNA polymerase (Invitrogen, Carlsbad, CA) and the following primers: a 892-bp amrR upstream fragment using primers 1581 (5′- agggtgtccacatccttgaa) and 1582 (5′- TCAGAGCGCTTTTGAAGCTAATTCGggacacttcaacggcaagat), a 828-bp oprA downstream fragment using primers 1583 (5′- AGGAACTTCAAGATCCCCAATTCGgtcgccgaatacgagaagac) and 1584 (5′- gaaatacgccttgacgcact), and a 1382-bp FRT-nptII-FRT fragment using primers 596 (5′-CGAATTAGCTTCAAAAGCGCTCTGA) and 597 (5′-CGAATTGGGGATCTTGAAGTTCCT)(Lowercase letters denote chromosome-specific sequences and uppercase letters FRT cassette-specific sequences.) These fragments were combined in a second PCR and, after gel purification, the resulting recombinant ∼3.1-kb DNA fragment was cloned into pGEM-T Easy (Novagen), which yielded pPS2282. The Δ(amrR-amrAB-oprA::FRT-nptII-FRT) cassette was excised from pPS2282 with EcoRI, blunted ended with T4 DNA polymerase (NEB) and ligated into the SmaI site of pEX-S12pheS (C. Lopez and H. Schweizer, unpublished) yielding pPS2354. Gene replacement using PheS-mediated counter-selection on M9-glucose supplemented with 0.15% p-chlorophenylalanine was performed as previously described [23] except that E. coli strains SM10(λpir) or RHO1 (a Km susceptible derivative of SM10[λpir] [24]; D. Rholl and H. Schweizer, unpublished) were used for conjugation experiments. The recipient strain was either Bp24 or Bp35 and merodiploids were selected on LSLB medium supplemented with 1000 µg/ml Km (to select for the Δ[amrR-amrAB-oprA::FRT-nptII-FRT] cassette cloned in pEX-S12pheS) and 100 µg/ml polymyxin B (to counterselect against RHO1). p-chlorophenylalanine resistant colonies were then obtained and screened for the presence of the correct deletion alleles by colony PCR [20] and primers 597 and 1546 for Δ(amrR-amrAB-oprA)::FRT-nptII-FRT. An unmarked Δ(amrR-amrAB-oprA) mutation was obtained after Flp recombinase- mediated excision of the nptII marker using pFlpe2 [20]. The presence of the deletion allele was verified by phenotypic (Gm susceptibility) and genotypic (PCR with primers 1581 and 1584) analyses.
Fosmid library construction and screening
Genomic DNA was extracted from strain 708a using the QiAmpDNA Mini Kit (Qiagen, Valencia, CA). Fosmids containing ∼40 kb inserts were isolated using the CopyControl Fosmid Library Production Kit following manufacturer's instructions (Epicentre, Madison, WI). Approximately 1,200 Cmr resistant colonies were pooled in groups of 30 (designated pools A–Z and 1–11), grown overnight in Cm containing medium, induced to high copy number and fosmid DNA was extracted using the QIAprep Mini-spin kit (Qiagen). Fosmid DNA from the 30 pools were screened by PCR using primers 1742 and 1743, and PCR products were obtained from 5 pools. DNA from these pools was transformed into E. coli DH5α and single colonies were screened for the presence of the correct clones by PCR using primers 1742 and 1743. DNA was extracted from these clones and sequenced with primers 1774 and 1779 which anneal in the fosmid backbone, as well as 1742 which anneals in the insert. Sequences obtained with primers 1774 and 1779 were BLAST searched against genome sequences of B. pseudomallei strains K96243, 1710b, 1106a and 668.
Next Gen Sequencing and data analysis
The genome of strain 708a was sequenced using a short “read” technology to detect missing genes relative to reference genomes. Five µg of DNA from B. pseudomallei strain 708a was sheared into approximately 175 bp fragments using air nebulization. A genomic library was then constructed following standard protocols from Illumina, Inc. (San Diego, CA). The library was sequenced on an Illumina Genome Analyzer (GA) using a single read sequencing method. Image analysis for base calling and alignments followed protocols of Craig et al. [25]. Genomic sequencing data (42 bp reads) for strain 708a were aligned against the K96243 and MSHR668 (data not presented) reference genomes using the Illumina GA software. The aligned reads were then visualized using the software program SolScape (Beckstrom-Sternberg et al., manuscript in preparation). Genomic regions with no reads were interpreted as missing from the sequenced genome.
Isolation of gentamicin resistant mutants
Gentamicin resistant derivatives of strains 2188a and 3799a were isolated in several steps. First, the strains were grown overnight at 37°C in LSLB medium containing 8 µg/ml Gm. The bacteria were then diluted into fresh LSLB medium containing 16 µg/ml Gm, followed by outgrowth at 37°C. The selection steps were repeated using LSLB medium containing 32, 64 and 128 µg/ml Gm. Similar selection steps were performed with 708a except that lower Gm concentrations of 2, 4, 8 and 16 µg/ml were employed.
Antimicrobial susceptibility testing
Minimal inhibitory concentrations (MICs) were determined in Mueller-Hinton broth from Becton Dickinson (Franklin Lakes, NJ) by the two-fold broth microdilution technique following Clinical and Laboratory Standards Institute guidelines [26]. The MICs were recorded after incubation at 37°C for 15 to 16 h.
Animal infection experiments
Ethics Statement: All animal procedures were performed using standard protocols and according to guidelines approved by the Colorado State University BioSafety Committee and the Colorado State University Animal Care and Use Committee. For animal infection experiments, B. pseudomallei strains were grown in LB medium to saturation by overnight incubation at 37°C with aeration. Glycerol was added to a final concentration of 15% and cell suspensions were stored at −80°C until ready for use. Inocula for in vivo infections were prepared by thawing and diluting the frozen bacterial stocks in sterile phosphate buffered saline (Sigma-Aldrich). Female BALB/c mice between 6–8 weeks of age were used for infection studies (Jackson Laboratories, Bar Harbor, ME). Mice were housed under pathogen-free conditions, and provided sterile water and food ad libitum. All animal infections were done using intranasal (i.n.) inoculation. Mice were anesthetized by intraperitoneal injection of 100 µg/g body weight of ketamine (Fort Dodge Animal Health, Overland Park, KS) and 10 µg/g body weight of xylazine (Ben Venue Laboratories, Bedord, OH). For all infections, the desired inoculum of B. pseudomallei was suspended in phosphate buffered saline. The 20 µl inoculum volume was delivered i.n, with the dose split evenly between both nostrils. At the completion of challenge studies, animals were humanely euthanized, according to study endpoints approved by the Animal Care and Use Committee at Colorado State University.
Results and Discussion
Aminoglycoside and macrolide susceptible isolates show reduced or absent AmrAB-OprA expression
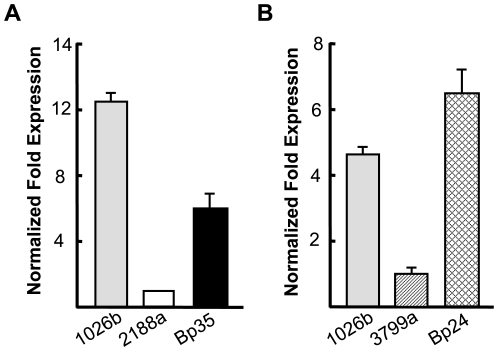
In agreement with previously published results, the aminoglycoside and macrolide susceptibility patterns of strains 708a, 2188a and 3799a isolated from human patients with various disease manifestations and clinical outcome ( Table 2 ) were similar to those observed with the AmrAB-OprA deficient strain DD503 ( Table 3 ). Quantitative real-time PCR was therefore used to assess amrAB-oprA expression relative to strain 1026b, which is known to constitutively express this efflux pump. No amrB transcripts were detected in strains 708a and Δ(amrAB-oprA) strain DD503, and amrB transcript levels were significantly lower in 2188a and 3799a than those measured in 1026b ( Fig. 1 ). As in our hands 2 to 3 fold differences in mRNA levels determined by qRT-PCR make the difference between low- and high-level RND pump-mediated resistance, these data support the notion that the aminoglycoside and macrolide susceptibilities of strains 708a, 2188a and 3799a are due to reduced or lack of AmrAB-OprA efflux pump expression.
Table 2. B. pseudomallei strains: origins, properties and clinical details.
| Strain | Isolation Date | Clinical Details | Gentamicin MICa |
| 708a | 30.8.90 | 32 year old male; 21 days fever and 14 days abdominal pain. No risk factors for melioidosis. Splenic abscess as single infectious site. Splenectomy required to control infection. Treated with intravenous ceftazidime followed by oral doxycycline. Survived. | 0.5 µg/ml |
| 2188a | 18.12.98 | 22 year old male rice farmer; 14 days fever, cough, sputum, swollen left knee. Known diabetic. Bacteremic with lung and joint involvement. Treated with joint washout and intravenous amoxicillin/clavulanic acid. Developed respiratory failure and died the day after admission. | 0.5 µg/ml |
| 3799a | 12.12.05 | 66 year old female rice farmer; 15 days cough, breathlessness, sputum. History of chronic renal failure. Bacteremic with lung and renal involvement. Treated with ceftazidime. Died from septic shock 4 days after admission. | 1 µg/ml |
MIC determinations were performed in Thailand using the E-test.
Table 3. Antibiotic susceptibilities of B. pseudomallei strains.
| Strain | Known Genotype | MIC (µg/ml) for: | |||||
| Gma | Str | Spc | Ery | Cla | Cli | ||
| 1026b | Wild-type | 256 | 1024 | 512 | 128 | 64 | >1024 |
| DD503 | 1026b with Δ(amrR-amrAB-oprA) | 2 | NDb | 64 | 8 | 4 | >1024 |
| 708a | 1 | 8 | 32 | 16 | 16 | >1024 | |
| 2188a | 1 | 8 | 32 | 16 | 32 | >1024 | |
| 3799a | 2 | 8 | 64 | 16 | 16 | >1024 | |
| Bp24 | Gmr derivative of 3799a | >1024 | 1024 | 256 | 64 | 16 | >1024 |
| Bp35 | Gmr derivative of 2188a | >1024 | >1024 | >1024 | 256 | 512 | >1024 |
| Bp66 | Low level Gmr derivative of 708a | 32 | 8 | 16 | 4 | 16 | >1024 |
| Bp187 | Bp24 with Δ(amrR-amrAB-oprA) | 2 | 16 | 128 | 16 | 16 | >1024 |
| Bp202 | Bp187::mini-Tn7T-LACc | 4 | 32 | 128 | 8 | 16 | >1024 |
| Bp194 | Bp187::mini-Tn7T-LAC-amrA + B +-oprA +c | >1024 | >1024 | >1024 | 256 | 512 | >1024 |
| Bp192 | Bp35 with Δ(amrR-amrAB-oprA) | 2 | 16 | 128 | 16 | 16 | >1024 |
| Bp201 | Bp192::mini-Tn7T-LACc | 4 | 32 | 128 | 8 | 16 | >1024 |
| Bp200 | Bp192::mini-Tn7T-LAC-amrA + B +-oprA +c | >1024 | >1024 | >1024 | 256 | 256 | >1024 |
Cla, clarithromycin; Cli, clindamycin; Ery, erythromycin; Gm, gentamicin; Spc, spectinomycin; Str, streptomycin.
ND, not done; DD503 is streptomycin resistant because of a chromosomal rpsL mutation.
The mini-Tn7 elements are integrated at the glmS2-associated Tn7 attachment site [20]. MIC values were determined in cells grown in the presence of 1 mM isopropyl-β-D-thiogalactopyranoside.
Figure 1. amrB transcript levels in gentamicin susceptible and resistant strains.
mRNA levels in LSLB without antibiotics-grown late-log cultures of the indicated strains were determined with an amrB-specific primer set. Data were normalized using the 23S rRNA gene as the housekeeping control. amrB transcript levels were determined A in strain 2188a and its gentamicin resistant derivative Bp35 and B in strain 3799a and its gentamicin resistant derivative Bp24. Relative quantifications were performed using 2188a and 3799a, respectively.
Gentamicin resistant derivatives of 2188a and 3799a, but not 708a, express AmrAB-OprA
As we were able to PCR amplify the 5′ and 3′ regions of the amrAB-oprA operon from strains 2188a and 3799a, but not 708a (data not shown), we suspected that this operon was absent from 708a and present but expressed at low levels 2188a and 3799a. To test this notion, we attempted to isolate Gm resistant derivatives of these strains. Highly (MIC>1024 µg/ml) Gmr derivatives, e.g. Bp35 and Bp24, were readily obtained with strains 2188a and 3799a, but not with 708a (e.g. Bp66) ( Table 3 ). Moreover, the Gmr 2188a and 3799a derivatives Bp35 and Bp24 became simultaneously resistant to other aminoglycosides and macrolides and their antibiotic susceptibility profiles resembled that of AmrAB-OprA expressing strain 1026b ( Table 3 ). In contrast, the moderately (MIC 32 µg/ml) Gmr derivative of 708a (Bp66) did not simultaneously become resistant to other aminoglycosides and erythromycin. None of the strains tested exhibited altered clindamycin resistance. Clindamycin is a good substrate of BpeAB-OprB but not AmrAB-OprA (T. Mima and H. Schweizer, unpublished data). Consistent with these observations, significantly increased amrB transcript levels were detected in Bp24 and Bp35 ( Fig. 1 , panels A and B), but not Bp66 (not shown). Deletion of amrAB-oprA from Bp24 and Bp35 resulted in loss of aminoglycoside and macrolide resistance which could be complemented back to wild-type levels by a chromosomally integrated mini-Tn7 expressing amrA+B+-oprA+ ( Table 3 ). Together, these results indicate that the amrAB-oprA operon is absent from 708a and present, but not expressed in sufficient levels in strains 2188a and 3799a to confer aminoglycoside and macrolide resistance.
Lack of AmrAB-OprA expression in 2188a and 3799a is not due to mutations in the amrAB-oprA regulatory region
To assess whether lack of amrAB-oprA expression in strains 2188a and 3799a is due to mutations in the operon's regulatory region, the amrR-amrA intergenic region was amplified with primers 1601 and 1602 and sequenced. These analyses revealed that the sequence of the amrR-amrA intergenic regions of strains 2188a and 3799a and their Gmr derivatives Bp35 and Bp24 were identical (data not shown). Furthermore, amplification of the amrR coding sequences from 2188a and 3799a and their Gmr derivatives Bp35 and Bp24 with primers 1599 and 1600 did not reveal any mutations in amrR. In summary, these data revealed that i) lack of AmrAB-OprA expression in 2188a and 3799a was not caused by mutations in the amrAB-oprA regulatory region and ii) increased amrAB-oprA expression in Gmr derivatives Bp24 and Bp35 was not due to promoter-up mutations or other amrR mutations. Rather, the data suggest that AmrAB-OprA expression is governed by a yet unidentified transcription factor or other positive regulatory mechanism(s). It is well known that efflux pump operon expression in other bacteria is governed by local as well as global mechanisms (reviewed in [27]). For instance, mexAB-oprM operon expression in P. aeruginosa is under control of the local MexR repressor [28], as well as other mechanisms including the ArmR anti-repressor encoded by a gene elsewhere on the chromosome [29].
Strain 708a contains a large deletion on chromosome 1
Results of PCR and qRT-PCR analysis were consistent with the notion that the amrAB-oprA operon was missing from strain 708a. Using the 1710b chromosome 1 sequence as a guide, primer sets were designed to amplify ∼500 bp fragments in the amrAB-oprA containing region of chromosome 1. Results of this primer walking strategy identified a correct PCR product obtained with primer set 1742 and 1743 designed to amplify sequences located ∼5 kb upstream of amrR. However, no PCR products were obtained with primers designed to sequences located up to 65 kb downstream of oprA. These data were consistent with the presence of a large (>70 kb) deletion on chromosome 1 encompassing amrAB-oprA. To determine the deletion boundaries, a fosmid library was constructed using 708a chromosomal DNA. By PCR amplification, several fosmids containing DNA previously located ∼5 kb upstream of amrR were identified. Sequence analyses of both fosmid-chromosomal DNA boundaries and BLAST analyses using four B. pseudomallei genomes revealed the same open reading frames (ORFs) at the respective junctions, BURPPS1710b_2037 (or its respective homolog in other genomes) and BURPPS1710b_2160 (or its respective homolog in other genomes). A series of primers was designed to determine the sequence adjacent to the primer 1742 binding site. The sequence was aligned to that of 1710b and revealed a fusion of ORFs BURPPS1710b_2155 and BURPPS1710b_2054. We interpreted this to mean that compared to 1710b, the 708a sequence was missing nucleotides 2,219,259–2,359,936 (or ∼141 kb) from chromosome 1, including amrAB-oprA.
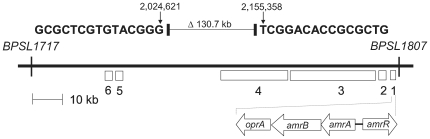
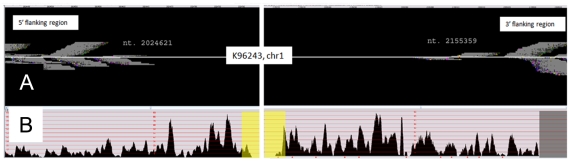
When compared to other strains, the extent of the deletion varied by approximately ±10 kb based on sequence from strains used as comparators. For example, when compared to K96243 the deletion is ∼131 kb ( Fig. 2 ). The deletion was further confirmed by: i) PCR amplification using primers 1797 and 1801 and DNA sequence analysis of a 1.1 kb chromosomal DNA fragment from 708a genomic DNA containing the predicted deletion junction; and ii) short read whole genome sequencing of the 708a genome ( Fig. 3 ).
Figure 2. Extent of chromosome 1 deletion in strain 708a compared to K96243.
708a contains a deletion fusing the bold sequences of BPSL1717 and BPSL1807, respectively. Some notable genes and gene clusters present in K96243 but missing from 708a are: 1 amrR-amrAB-oprA; 2 a three gene operon (BPSL1801-BPSL1800-BPSL1799) encoding a putative type-1 fimbrial protein along with its outer membrane usher protein and chaperone; 3 the 13 gene malleobactin biosynthetic gene cluster and its extracytoplasmic sigma factor MbaS defined by mbaF-fmtA-mbaA-mbaI-mbaJ-mbaE-BPSL1781-BPSL1782-BPSL1783-BPSL1784-BPSL1785-BPSL1786-mbaS; 4 a cluster of 18 genes (BPSL1755-BPSL1773) encoding a putative aerobic (or late cobalt insertion) vitamin B12 biosynthetic pathway with an embedded gene (BPSL1763) encoding a putative exported chitinase; 5 arcD (BPSL1742) and arcABC (BPSL1743-BPSL1744-BPSL1745) coding for the arginine deiminase pathway; and 6 a two gene cluster (BPSL1732-BPSL1731) coding for a putative methyl-accepting chemotaxis citrate transducer and chemotaxis protein CheW2, respectively. Strain 1710b contains an additional 10 kb of DNA in this region.
Figure 3. Large deletion verification in chromosome 1 of strain 708a by whole genome sequencing.
Genomic sequencing data from strain 708a were aligned against the K96243 reference genome. Panel A shows the read density near positions 2,024,621 and 2,155,359 on chromosome 1. Panel B shows the 708a read density across the ∼4.5 Kb flanking the deletion in chromosome 1 of strain K96243. The yellow highlighted region in panel B marks a ∼130.7 Kb region with a near-zero read coverage, which correspond to the panel A coordinates. This lack of reads is strong evidence for deletion of the entire region in strain 708a.
Genes contained within the large deletion present in 708a chromosome 1
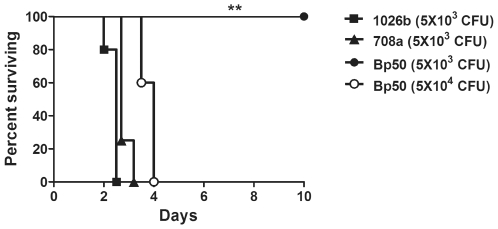
Because of the more thorough and detailed annotation of the published K96243 genome we decided to use it to assess key genes missing from B. pseudomallei strain 708a. According to K96243 coordinates, 708a is missing nucleotides 2,024,622 to 2,155,357 fusing the BURPPS1710b_2155 and BURPPS1710b_2054 equivalents BPSL1717 and BPSL1807 ( Fig. 2 ). In K96243, as well as 1710b and other B. pseudomallei strains, this >90 gene region not only contains amrAB-oprA but several other genes that may be pertinent to this bacterium's physiology and pathogenesis ( Table 4 ). First, this deleted region contains the 13 gene malleobactin biosynthetic gene cluster and its extracytoplasmic sigma factor MbaS defined by mbaF-fmtA-mbaA-mbaI-mbaJ-mbaE-BPSL1781-BPSL1782-BPSL1783-BPSL1784-BPSL1785-BPSL1786-mbaS [30]. Malleobactin is a hydroxamate siderophore that is analogous to the same genes in Pseudomonas aeruginosa pyoverdine [31] and B. cepacia ornibactin [32]. Pyoverdine is essential for infection and full virulence of P. aeruginosa, as assessed in several different experimental models [33], along with biofilm formation [34]. Similarly, B. cepacia mutants defective in ornibactin synthesis showed significantly reduced virulence [32]. However, in the case of 708a, despite missing the entire malleobactin biosynthetic gene cluster and exhibiting overall greatly reduced siderophore synthesis (as assessed by growth on Chrome azurol S plates) [30],[35] (data not shown), the 708a stain was still able to cause severe illness in the infected human from which it was isolated ( Table 2 ). Moreover, strain 708a was also fully virulent in our acute inhalational challenge model in mice ( Fig. 4 ). Thus, it is possible that malleobactin may not play the same crucial role in infection and virulence that the P. aeruginosa pyoverdine siderophore does. Alternatively, B. pseudomallei is known to synthesize other iron transport systems, including a pyochelin siderophore and heme-hemin receptor and transporter [30],[36], and thus 708a may utilize these alternative pathways for iron transport. Second, immediately adjacent to the malleobactin biosynthetic genes is a cluster of 18 genes (BPSL1755-BPSL1773) encoding a putative aerobic (or late cobalt insertion) vitamin B12 biosynthetic pathway [37]. Vitamin B12 is a known cofactor for numerous enzymes mediating methylation, reduction and intramolecular rearrangements. Why this pathway is dispensable for growth in 708a is not known. However, some bacteria are known to possess an alternative anaerobic (or early cobalt insertion) pathway [37]. Third, the deletion in 708a encompasses the genes arcD (BPSL1742) and arcABC (BPSL1743-BPSL1745) coding for the arginine deiminase pathway. In P. aeruginosa, this pathway provides for ATP synthesis under anaerobic conditions in the absence of exogenous electron acceptors provided that arginine is present in the growth medium [38]. In this context it is worthy of note that 708a was isolated from a splenic abscess and abscesses are generally considered to provide a mixed aerobic-anaerobic environment [39],[40]. If 708a was truly able to grow under anaerobic conditions, then 708a must be capable of utilizing alternative pathways for energy generation under anaerobic conditions. This alternate pathway presumably would require nitrate as B. pseudomallei was shown to be capable of growing anaerobically only in the presence of arginine and nitrate [41].
Table 4. K96243 gene equivalents contained within the 708a chromosome 1 deletion.
| Locus Tag or Gene | Putative or Known Function |
| BPSL1717 | Hypothetical protein |
| BPSL1718 | Hypothetical protein |
| BPSL1719 | Putative kinase |
| BPSL1720 | Putative argininosuccinate lyase |
| BPSL1721 | Putative argininosuccinate synthase |
| BPSL1722 | Putative formyl transferase |
| BPSL1723 | Hypothetical protein |
| BPSL1724 | Putative histidinol-phosphate aminotransferase |
| BPSL1725 | Hypothetical protein |
| BPSL1726 | Hypothetical protein |
| BPSL1727 | Putative non-ribosomal peptide synthase (thioesterase domain) |
| BPSL1727 | Putative non-ribosomal peptide synthase (thioesterase domain) |
| BPSL1728 | Putative exported porin |
| BPSL1729 | Putative AraC-family transcriptional regulator |
| BPSL1730 | Putative transmembrane protein |
| BPSL1731 | Chemotaxis protein CheW2 |
| BPSL1732 | Putative methyl-accepting chemotaxis citrate transducer |
| BPSL1733 | Hypothetical protein |
| BPSL1734 | Acyl-CoA synthase |
| BPSL1735 | Putative transport system membrane protein |
| BPSL1736 | Putative methyltransferase |
| BPSL1737 | Putative ABC transport system, exported protein |
| BPSL1738 | Putative ABC transport system, membrane protein |
| BPSL1739 | Putative ABC transport system, ATP-binding protein |
| BPSL1740 | Putative ABC transport system, membrane protein |
| BPSL1741 | Hypothetical protein |
| arcD | Arginine/ornithine antiporter |
| arcA | Arginine deiminase |
| arcB | Ornithine carbamoyltransferase |
| arcC | Carbamate kinase |
| BPSL1746 | Short chain dehydrogenase |
| BPSL1747 | Hypothetical protein |
| BPSL1748 | Putative LysR-family transcriptional regulator |
| BPSL1749 | Putative glutathione S-transferase |
| BPSL1750 | Putative MarR-family transcriptional regulator |
| BPSL1751 | Putative amino-acid transport-related exported protein |
| BPSL1752 | Putative MarR-family regulatory protein |
| BPSL1753 | Putative transport-related membrane protein |
| BPSL1754 | Putative lipoprotein |
| BPSL1755 | Precorrin-4 C11-methyltransferase |
| BPSL1756 | Precorrin-6× reductase |
| BPSL1757 | Cobalt-precorrin-6A synthase |
| BPSL1758 | Precorrin-6Y C5,15-methyltransferase |
| BPSL1759 | Putative oxidoreductase |
| BPSL1760 | Precorrin-8× methylmutase |
| BPSL1761 | Precorrin-2 methyltransferase |
| BPSL1762 | Precorrin-3b C17-methyltransferase |
| BPSL1763 | Putative exported chitinase |
| BPSL1764 | Hypothetical protein |
| BPSL1765 | Putative carboxylesterase |
| BPSL1766 | Hypothetical protein |
| BPSL1767 | Putative magnesium chelatase protein |
| BPSL1768 | Cobaltochelatase |
| BPSL1769 | Putative cobalamin biosynthesis-related protein |
| BPSL1770 | High-affinity nickel transport protein |
| BPSL1771 | Cobalamin biosynthesis protein CbiG |
| BPSL1772 | Cob(I)yrinic acid a,c-diamide adenosyltransferase |
| BPSL1773 | Cobyrinic acid A,C-diamide synthase |
| mbaF | Putative N5-hydroxyornithine transformylase1 |
| fmtA | Malleobactin receptor |
| mbaA | Putative L-ornithine-N5-oxygenase |
| mbaI | Putative non-ribosomal peptide synthase |
| mbaJ | Putative non-ribosomal peptide synthase |
| mbaE | Similar to P. aeruginosa pvdE (ABC transporter) |
| BPSL1780 | Hypothetical protein |
| BPSL1781 | Putative periplasmic iron-binding protein |
| BPSL1782 | Putative ferric iron reductase |
| BPSL1783 | Putative iron transport-related membrane protein |
| BPSL1784 | Putative iron transport-related ATP-binding protein |
| BPSL1785 | Hypothetical protein (similar to syrP from Streptomyces verticillus) |
| BPSL1786 | Hypothetical protein (similar to mbtH from Mycobacterium tuberculosis) |
| mbaS | MbaS, extracytoplasmic sigma factor |
| BPSL1788 | Pseudogene |
| BPSL1789 | Short chain dehydrogenase |
| BPSL1790 | Putative zinc-binding dehydrogenase |
| BPSL1791 | Hypothetical protein |
| BPSL1792 | Hypothetical protein |
| BPSL1793 | Putative sugar-binding exported protein |
| BPSL1794 | Putative AraC-family transcriptional regulator |
| BPSL1795 | Hypothetical protein |
| BPSL1796 | Hypothetical protein |
| BPSL1797 | Putative ABC transport system, membrane protein |
| BPSL1798 | Hypothetical protein |
| BPSL1799 | Putative fimbrial chaperone |
| BPSL1800 | Putative outer membrane usher protein precursor |
| BPSL1801 | Putative type-1 fimbrial protein |
| BPSL1802 | OprA multidrug efflux outer membrane channel protein |
| BPSL1803 | AmrB multidrug efflux system transporter protein |
| BPSL1804 | AmrA multidrug efflux system membrane fusion protein |
| BPSL1805 | AmrR TetR family regulatory protein |
| BPSL1806 | Subfamily M23B unassigned peptidase |
| BPSL1807 | Putative amino acid transport system, membrane protein |
Annotation of BPSL1774 (mbaF) through BPSL1787 (mbaS) according to Alice et al. [30].
Figure 4. Strain 708a is fully virulent in an acute murine melioidosis infection model.
BALB/c mice (n = 4–5 mice) were infected intranasally with 5×103 CFUs of 1026b ▪, 5×103 CFUs of strain 708a ▴, and 5×103 • or 5×104 ○ colony forming units of the isogenetic Δ(amrRAB-oprA) 1026b derivative Bp50. Statistical differences in survival times were determined by Kaplan-Meier curves followed by log-rank test. The Bonferroni corrected threshold was applied and comparisons with p <0.017 were considered significant. (**, p <0.01 for strain 1026b vs. Bp50 (5,000 CFU) and 708a vs. Bp50 (5,000 CFU). Data are representative of 2 independent experiments.
Fourth, other noteworthy genes covered by the deletion include i) a three gene operon (BPSL1801-BPSL1799) encoding a putative type-1 fimbrial protein along with its outer membrane usher protein and chaperone; ii) a two gene cluster (BPSL1732-BPSL1731) coding for a putative methyl-accepting chemotaxis citrate transducer and chemotaxis protein CheW2, respectively; and iii) a putative exported chitinase (BPSL1763).
Genes missing from the 131 kb deletion are not present elsewhere on the chromosome
To assess whether the aforementioned genes were indeed absent from the chromosome we performed i) whole genome sequencing and ii) PCR analysis of selected genes.
Genomic alignments were performed to compare 708a data with two B. pseudomallei reference genomes: strains K96243 and MSHR668. The 42 bp reads had an average density of 24× and covered 93.3% (chromosome 1) and 96.9% (chromosome 2) of the reference genomes. The notable exception to this coverage was a ∼130.7 Kb region corresponding to positions 2,024,621 and 2,155,359 in chromosome 1 of the K96243 genome ( Fig. 3 ). Nearly zero reads aligned to this region indicating that the 708a strain does not contain any of these genes. While these data do not discern gene order or chromosomal linearity between 708a and the reference genomes, this does represent a comprehensive query and argues that the genes in this region are not present anywhere in the 708a genome. If homologous genes existed elsewhere in the 708a genome, they would have generated short reads that would have aligned with this region. The short read data are available online at http://www.mggen.nau.edu/MGGen_research.html.
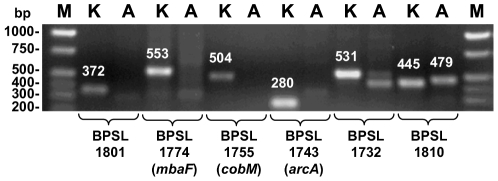
Because whole genome sequence coverage was not 100% for both chromosomes, we performed PCR analysis for selected genes using gene-specific primers designed for amplification of the corresponding K96243 sequences ( Fig. 5 ). PCR analysis showed the expected DNA fragments with genomic DNA templates from K96243 but not with 708a templates. The identities of the amplified DNA fragments were verified by DNA sequence analyses which also confirmed minor bands visible in some PCR reactions from 708a templates as non-specific amplification products. As a positive control, we amplified a fragment from the BPSL1809-BPSL1810 region using primers 1742 and 1743. This region is present in both 708a and K96243. The 445 bp amplicon derived from K96243 DNA consists of 243 bp from BPSL1810 and 202 bp from the BPSL1809-BPSL1810 intergenic region. The corresponding fragment obtained with 708a DNA is slightly larger (479 bp) because of several insertions in the BPSL1809-BPSL1810 intergenic region.
Figure 5. Deleted genes are absent from the 708a genome.
PCR was performed with genomic DNA isolated from K strain K96243 or A strain 708a with gene-specific primers. These included 2037 & 2038 for BPSL1801, 2035 & 2036 for BPSL1774, 2033 & 2034 for BPSL1755, 1954 & 1955 for BPSL1743, 2031 & 2032 for BPSL1732, and 1742 & 1743 for BPSL1810. PCR products were separated on a 1% agarose gel and stained with ethidium bromide. Sizes of the expected PCR fragments (in bp and based on K96243 genomic sequence) are indicated above the respective bands. Gene annotations are according to K96243 and gene names, where known, are in parentheses. Lanes M contained the Hi-Lo DNA ladder (Minnesota Molecular, Minneapolis, MN) and the sizes of pertinent fragments are indicated on the left.
In summary, these findings provide some insight into the physiology and pathogenesis of B. pseudomallei. However, because 708a grows normally in rich and minimal laboratory media under aerobic conditions, is fully virulent in an acute murine melioidosis model and caused human melioidosis, the genes affected by the deletion must be dispensable at least under the in vitro and in vivo conditions encountered during laboratory studies and splenic abscess disease during human infection caused by lone presence of 708a. This scenario is likely as simultaneous infection with more than one strain is uncommon in human melioidosis [42].
Concluding remarks
The clinical diagnosis of Burkholderia pseudomallei still relies on culture which is most commonly performed using selective Ashdown's agar whose main selective ingredient is gentamicin. The majority of B. pseudomallei strains grow on this medium because of their intrinsic resistance to aminoglycosides mediated by the AmrAB-OprA efflux pump. At least 1 in 1,000 clinical isolates in NE Thailand are susceptible to aminoglycosides and such isolates are obviously missed by using Ashdown's diagnostic agar. The actual number of aminoglycoside susceptible strains may thus be higher. Our results confirm that the aminoglycoside and macrolide susceptibility of rare clinical isolates is indeed due to reduced or lack of expression of the amrAB-oprA efflux pump operon, as previously suggested but not proven [16]. Even though BpeAB-OprB was previously implicated to contribute to aminoglycoside and macrolide resistance in strain KHW [14], we now know that this pump does not confer aminoglycoside resistance in 1026b (T. Mima and H. Schweizer, unpublished observations), a strain isolated in the same hospital as 708a. BpeAB-OprB is only expressed at very low levels in wild-type strains which may explain the low levels of erythromycin resistance observed in 708a, 2188a and 3799a in the absence of AmrAB-OprB. This notion is supported by the observation that all strains analyzed in this study exhibit clindamycin resistance. Clindamycin is a good substrate of BpeAB-OprB but not AmrAB-OprA (T. Mima and H. Schweizer, unpublished data). As expected, qRT-PCR analyses showed only low-level BpeAB-OprB expression in these strains (data not shown). Though strain 708a contains a large deletion encompassing several gene clusters encoding potential virulence factors and genes required for growth under anaerobic conditions, these genes may either be dispensable for in vitro and in vivo growth or this strain compensates for them by expressing similar functions from another set of genes. The latter notion may be supported by the observation that the genetically engineered 1026b AmrAB-OprA mutant derivative Bp50 shows reduced virulence in the murine melioidosis model whereas 708a missing these genes is as virulent as 1026b ( Fig. 4 ). We do not know the factors, if any, that led to selection of strains missing or lacking expression of AmrAB-OprA. Further experiments aimed at addressing some of these issues at the molecular level are facilitated by availability of the nearly complete 708a sequence and tools that allow genetic manipulation of this strain. Lastly, because 708a is fully virulent in the murine melioidosis model, yet very susceptible to aminoglycosides, this strain may be a natural candidate for genetic manipulation experiments that use Select Agent compliant antibiotics for selection, such as gentamicin [20], kanamycin [20], spectinomycin/streptomycin [43] and nourseothricin [44] selection markers, and validates the use of laboratory-constructed Δ(amrAB-oprA) mutants in such experiments [13],[20].
Acknowledgments
We thank Ayush Kumar and Carolina Lopez for constructing and providing pPS1927 and pEX-S12pheS, respectively. We would also like to thank David Craig and John Pearson for their support of our sequencing efforts.
Footnotes
The authors have declared that no competing interests exist.
HPS was supported by NIH NIAID grant U54 AI065357. SJP and VW were supported by the Wellcome Trust. This work was supported in part by NIH NIAID grants U01 AI075568-01 and U54 AI065359 to PK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersinga WJ, van der Poll T, White NJ, Day NP, Peacock SJ. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat Rev Microbiol. 2006;4:272–282. doi: 10.1038/nrmicro1385. [DOI] [PubMed] [Google Scholar]
- 3.Currie BJ, Dance DAB, Cheng AC. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg. 2008;102/S1:S1–S4. doi: 10.1016/S0035-9203(08)70002-6. [DOI] [PubMed] [Google Scholar]
- 4.Stone R. Racing to defuse a bacterial time bomb. Science. 2007;317:1022–1024. doi: 10.1126/science.317.5841.1022. [DOI] [PubMed] [Google Scholar]
- 5.Ciervo A, Mattei R, Cassone A. Melioidosis in an Italian tourist injured by the tsunami in Thailand. J Chemother. 2006;18:443–444. doi: 10.1179/joc.2006.18.4.443. [DOI] [PubMed] [Google Scholar]
- 6.Athan E, Allworth AM, Engler C, Bastian I, Cheng AC. Melioidosis in tsunami survivors. Emerg Infect Dis. 2005;11:1638–1639. doi: 10.3201/eid1110.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Svensson E, Welinder-Olsson C, Claesson BA, Studahl M. Cutaneous melioidosis in a Swedish tourist after the tsunami in 2004. Scand J Infect Dis. 2006;38:71–74. doi: 10.1080/00365540500264738. [DOI] [PubMed] [Google Scholar]
- 8.Chierakul W, Winothai W, Wattanawaitunechai C, Wuthiekanun V, Rugtaengan T, et al. Melioidosis in 6 tsunami survivors in southern Thailand. Clin Infect Dis. 2005;41:982–990. doi: 10.1086/432942. [DOI] [PubMed] [Google Scholar]
- 9.Wuthiekanun V, Peacock SJ. Management of melioidosis. Expert Rev Anti Infect Ther. 2006;4:445–455. doi: 10.1586/14787210.4.3.445. [DOI] [PubMed] [Google Scholar]
- 10.Vorachit M, Lam K, Jayanetra P, Costerton JW. Resistance of Pseudomonas pseudomallei growing as a biofilm on silastic discs to ceftazidime and co-trimoxazole. Antimicrob Agents Chemother. 1993;37:2000–2002. doi: 10.1128/aac.37.9.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ngauy V, Lemeshev Y, Sadowski L, Crawford G. Cutaneous melioidosis in a man who was taken as a prisoner of war by the Japanese in World War II. J Clin Microbiol. 2005;43:970–972. doi: 10.1128/JCM.43.2.970-972.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holden MTG, Titball RW, Peacock SJ, Cerdeno-Tarraga AM, Atkins TP, et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci USA. 2004;101:14240–14245. doi: 10.1073/pnas.0403302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore RA, DeShazer D, Reckseidler S, Weissman A, Woods DE. Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob Agents Chemother. 1999;43:465–470. doi: 10.1128/aac.43.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan YY, Tan TMC, Ong YM, Chua KL. BpeAB-OprB, a multidrug efflux pump in Burkholderia pseudomallei. Antimicrob Agents Chemother. 2004;48:1128–1135. doi: 10.1128/AAC.48.4.1128-1135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar A, Chua K-L, Schweizer HP. Method for regulated expression of single-copy efflux pump genes in a surrogate Pseudomonas aeruginosa strain: identification of the BpeEF-OprC chloramphenicol and trimethoprim efflux pump of Burkholderia pseudomallei 1026b. Antimicrob Agents Chemother. 2006;50:3460–3463. doi: 10.1128/AAC.00440-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simpson AJ, White NJ, Wuthiekanun V. Aminoglycoside and macrolide resistance in Bukholderia pseudomallei. Antimicrob Agents Chemother. 1999;43:2332. doi: 10.1128/aac.43.9.2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liss L. New M13 host: DH5αF' competent cells. Focus. 1987;9:13. [Google Scholar]
- 18.Miller JH. A Short Course in Bacterial Genetics. Cold Spring Harbor, N.Y.: Cold Spring Harbor Laboratory Press; 1992. [Google Scholar]
- 19.Sambrook J, Russell DW. Molecular Cloning. Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press; 2001. [Google Scholar]
- 20.Choi K-H, Mima T, Casart Y, Rholl D, Kumar A, et al. Genetic tools for select agent compliant manipulation of Burkholderia pseudomallei. Appl Env Microbiol. 2008;74:1064–1075. doi: 10.1128/AEM.02430-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rholl DA, Trunck LA, Schweizer HP. Himar1 in vivo Transposon Mutagenesis of Burkholderia pseudomallei. Appl Environ Microbiol. 2008;74:7529–7535. doi: 10.1128/AEM.01973-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar A, Mayo M, Trunck LA, Cheng AC, Currie BJ, et al. Expression of resistance-nodulation-cell division efflux pumps in commonly used Burkholderia pseudomallei strains and clinical isolates from Northern Australia. Trans Roy Soc Trop Med Hyg. 2008;102/S1:S145–S151. doi: 10.1016/S0035-9203(08)70032-4. [DOI] [PubMed] [Google Scholar]
- 23.Barrett AR, Kang Y, Inamasu KS, Son MS, Vukovich JM, et al. Genetic tools for allelic replacement in Burkholderia species. Appl Environ Microbiol. 2008;74:4498–4508. doi: 10.1128/AEM.00531-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller VL, Mekalanos JJ. A novel suicide vector and its use in construction of insertion mutations: osmoregulation of outer membrane proteins and virulence determinants in Vibrio cholerae requires toxR. J Bacteriol. 1988;170:2575–2583. doi: 10.1128/jb.170.6.2575-2583.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Craig DW, Pearson JV, Szelinger S, Sekar A, Redman M, et al. Identification of genetic variants using bar-coded multiplexed sequencing. Nat Methods. 2008;5:887–893. doi: 10.1038/nmeth.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clinical and Laboratory Standards Institute. M7-A7, Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard - seventh edition. Wayne, , PA.: 2006. [Google Scholar]
- 27.Kumar A, Schweizer HP. Bacterial resistance to antibiotics: active efflux and reduced uptake. Adv Drug Deliv Rev. 2005;57:1486–1513. doi: 10.1016/j.addr.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 28.Poole K, Tetro K, Zhao Q, Neshat S, Heinrichs D, et al. Expression of the multidrug resistance operon mexA-mexB-oprM in Pseudomonas aeruginosa: mexR encodes a regulator of operon expression. Antimicrob Agents Chemother. 1996;40:2021–2028. doi: 10.1128/aac.40.9.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilke MS, Heller M, Creagh AL, Haynes CA, McIntosh LP, et al. The crystal structure of MexR from Pseudomonas aeruginosa in complex with its antirepressor ArmR. Proc Natl Acad Sci USA. 2008;105:14832–14837. doi: 10.1073/pnas.0805489105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alice AF, Lopez CS, Lowe CA, Ledesma MA, Crosa JH. Genetic and transcriptional analysis of the siderophore malleobactin biosynthesis and transport genes in the human pathogen Burkholderia pseudomallei K96243. J Bacteriol. 2006;188:1551–1566. doi: 10.1128/JB.188.4.1551-1566.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Visca P, Imperi F, Lamont IL. Pyoverdine siderophores: from biogenesis to biosignificance. Trends Microbiol. 2007;15:22–30. doi: 10.1016/j.tim.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Sokol PA, Darling P, Woods DE, Mahenthiralingam E, Kooi C. Role of ornibactin biosynthesis in the virulence of Burkholderia cepacia: characterization of pvdA, the gene encoding L-ornithine N(5)-oxygenase. Infect Immun. 1999;67:4443–4455. doi: 10.1128/iai.67.9.4443-4455.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Visca P. Iron regulation and siderophore signalling in virulence by Pseudomonas aeruginosa. In: Ramos JL, editor. Pseudomonas. New York: Kluwer/Plenum; 2004. pp. 69–123. [Google Scholar]
- 34.Banin E, Vasil ML, Greenberg EP. Iron and Pseudomonas aeruginosa biofilm formation. Proc Natl Acad Sci USA. 2005;102:11076–11081. doi: 10.1073/pnas.0504266102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwyn B, Neilands JB. Universal chemical assay for the detection and determination of siderophores. Anal Biochem. 1987;160:47–56. doi: 10.1016/0003-2697(87)90612-9. [DOI] [PubMed] [Google Scholar]
- 36.Tuanyok A, Kim HS, Nierman WC, Yu Y, Dunbar J, et al. Genome-wide expression analysis of iron regulation in Burkholderia pseudomallei and Burkholderia mallei using DNA microarrays. FEMS Microbiol Lett. 2005;252:327–335. doi: 10.1016/j.femsle.2005.09.043. [DOI] [PubMed] [Google Scholar]
- 37.Warren MJ, Raux E, Schubert HL, Escalante-Semerena JC. The biosynthesis of adenosylcobalamin (vitamin B12). Nat Prod Rep. 2002;19:390–412. doi: 10.1039/b108967f. [DOI] [PubMed] [Google Scholar]
- 38.Vander Wauven C, Pierard A, Kley-Raymann M, Haas D. Pseudomonas aeruginosa mutants affected in anaerobic growth on arginine: evidence for a four-gene cluster encoding the arginine deiminase pathway. J Bacteriol. 1984;160:928–934. doi: 10.1128/jb.160.3.928-934.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brook I, Frazier EH. Microbiology of liver and spleen abscesses. J Med Microbiol. 1998;47:1075–1080. doi: 10.1099/00222615-47-12-1075. [DOI] [PubMed] [Google Scholar]
- 40.Brook I, Frazier EH. Aerobic and anaerobic microbiology of retroperitoneal abscesses. Clin Infect Dis. 1998;26:938–941. doi: 10.1086/513947. [DOI] [PubMed] [Google Scholar]
- 41.Yabuuchi E, Arakawa M. Burkholderia pseudomallei and melioidosis: be aware in temperate area. Microbiol Immunol. 1993;37:823–836. doi: 10.1111/j.1348-0421.1993.tb01712.x. [DOI] [PubMed] [Google Scholar]
- 42.Limmathurotsakul D, Wuthiekanun V, Chantratita N, Wongsuvan G, Thanwisai A, et al. Simultaneous infection with more than one strain of Burkholderia pseudomallei is uncommon in human melioidosis. J Clin Microbiol. 2007;45:3830–3832. doi: 10.1128/JCM.01297-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prentki P, Krisch H. In vitro insertional mutagenesis with a selectable DNA fragment. Gene. 1984;29:303–313. doi: 10.1016/0378-1119(84)90059-3. [DOI] [PubMed] [Google Scholar]
- 44.Maier TM, Pechous R, Casey M, Zahrt TC, Frank DW. In Vivo Himar1-based transposon mutagenesis of Francisella tularensis. Appl Environ Microbiol. 2006;72:1878–1885. doi: 10.1128/AEM.72.3.1878-1885.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DeShazer D, Brett P, Carlyon R, Woods D. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J Bacteriol. 1997;179:2116–2125. doi: 10.1128/jb.179.7.2116-2125.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi K-H, Schweizer HP. mini-Tn7 insertion in bacteria with single attTn7 sites: example Pseudomonas aeruginosa. Nat Protocols. 2006;1:153–161. doi: 10.1038/nprot.2006.24. [DOI] [PubMed] [Google Scholar]
- 47.Wang RF, Kushner SR. Construction of versatile low-copy-number vectors for cloning, sequencing and gene expression in Escherichia coli. Gene. 1991;100:195–199. [PubMed] [Google Scholar]