Abstract
Indolmycin, a potential antibacterial drug, competitively inhibits bacterial tryptophanyl-tRNA synthetases. An effort to identify indolmycin resistance genes led to the discovery of a gene encoding an indolmycin-resistant isoform of tryptophanyl-tRNA synthetase. Overexpression of this gene in an indolmycin-sensitive strain increased the indolmycin MIC 60-fold. Its transcription and distribution in various bacterial genera were assessed. The level of resistance conferred by this gene was compared to that of a known indolmycin resistance gene and to those of genes with resistance-conferring point mutations.
Aminoacyl-tRNA synthetases frequently have been mentioned as targets for a new class of antimicrobial drugs (17, 21, 25, 28, 34). Much of the interest in these enzymes as drug targets is based on the efficacy of mupirocin, an isoleucyl-tRNA synthetase inhibitor that is clinically used as a topical antibacterial agent. Two well-characterized inhibitors of bacterial tryptophanyl-tRNA synthetase are the naturally occurring antibiotics chuangxinmycin and indolmycin (Fig. 1). Indolmycin is produced by Streptomyces griseus ATCC 12648 (23, 29), and Actinoplanes tsinanensis produces chuangxinmycin (3). Indolmycin is of particular interest because it is active against human pathogens, including methicillin-resistant Staphylococcus aureus and Helicobacter pylori (16, 19). The indolmycin MICs for methicillin-resistant Staphylococcus aureus and H. pylori are 0.5 and 0.016 μg/ml, respectively (16, 19).
FIG. 1.
Indolmycin, tryptophan, and chuangxinmycin. As structural analogs of tryptophan, indolmycin and chuangxinmycin competitively inhibit bacterial tryptophanyl-tRNA synthetases (3, 38). Chuangxinmycin was provided as a gift from GlaxoSmithKline. The indolmycin used in these studies was chemically synthesized (see Materials and Methods).
A concern in the development of any antimicrobial drug is the emergence of resistance (5). The efficacy of mupirocin has been compromised by the distribution of mupA and mupM, two genes that encode isoleucyl-tRNA synthetase isoforms that are resistant to mupirocin (4, 8, 15, 32). mupM is a resistance gene from the mupirocin producer Pseudomonas fluorescens, and mupA has been observed in Staphylococcus aureus, but its origins are unknown (7, 35, 39). Bacteria that have acquired mupA or mupM retain their chromosomal copy of mupirocin-sensitive isoleucyl-tRNA synthetase. Thus, auxiliary aminoacyl-tRNA synthetase genes are highly correlated with antibiotic resistance. Another example is the auxiliary tryptophanyl-tRNA synthetase gene (trpRS1) in Streptomyces coelicolor that confers high-level resistance to indolmycin (22, 36). The horizontal transfer of antibiotic-resistant aminoacyl-tRNA synthetase genes could negatively impact the clinical development and use of antibacterials that inhibit aminoacyl-tRNA synthetases (2, 9). Given the pharmacological potential of indolmycin, the identification of native resistance genes is of interest. In efforts to identify additional indolmycin-resistant synthetases, we performed a bioinformatic search and discovered a novel auxiliary tryptophanyl-tRNA synthetase gene (SGR3809) in Streptomyces griseus NBRC 13350, which is best known as the producer of streptomycin (26). This gene is distinct in sequence from trpRS1, yet it also confers high-level resistance to indolmycin. Homologs of this gene were found in several other bacterial species, including the indolmycin producer Streptomyces griseus ATCC 12648. The level of resistance conferred by this gene was compared to those of trpRS1 and tryptophanyl-tRNA synthetase genes with resistance-conferring point mutations.
MATERIALS AND METHODS
Bacterial strains and culture conditions.
The strains used in this work are provided in Table 1. Escherichia coli strains DH5α and ET12567/pUZ8002 were grown in Luria-Bertani medium at 37°C for routine subcloning (30). Streptomyces species were grown at 30°C on mannitol soya flour medium (SFM), Difco nutrient agar medium, yeast extract-malt extract medium (YEME), or minimal liquid medium (NMMP) (20). SFM was used for conjugations between S. coelicolor and E. coli and for generating spore suspensions. For transcriptional analysis, S. coelicolor and Streptomyces avermitilis strains were grown in NMMP. The indolmycin producer S. griseus ATCC 12648 was grown in NMMP without polyethylene glycol (PEG) for transcriptional analysis and the liquid chromatography-mass spectrometry (LC-MS) analysis of culture supernatants. For selecting E. coli, ampicillin, apramycin, chloramphenicol, hygromycin, and kanamycin were employed at 100, 50, 25, 80, and 50 μg/ml, respectively. Nalidixic acid was used at 20 μg/ml to counterselect E. coli in conjugations with S. coelicolor. Apramycin and hygromycin were used at 50 μg/ml for selecting S. coelicolor.
TABLE 1.
Strains used in this study
| Strain | Genotype and/or description | Reference or source |
|---|---|---|
| S. avermitilis ATCC 31267 | 18, 27 | |
| S. coelicolor | ||
| M600 | Prototroph, SCP1− SCP2− | 1 |
| B725 | M600 trpRS1::apr; indolmycin sensitive | 20 |
| B730 | B725 trpRS2(L9F), spontaneous mutant selected at 1 μg/ml indolmycin (parent of B737) | 36 |
| B731 | B725, spontaneous mutant selected at 1 μg/ml indolmycin (unknown mutation[s], parent of B734) | This study |
| B732 | B725, spontaneous mutant selected at 1 μg/ml indolmycin (unknown mutation[s], parent of B735) | This study |
| B733 | B725, spontaneous mutant selected at 1 μg/ml indolmycin (unknown mutation[s], parent of B736) | This study |
| B734 | B725 TrpRS2(H48N), spontaneous mutant selected at 10 μg/ml indolmycin | This study |
| B735 | B725 TrpRS2(H48Q), spontaneous mutant selected at 10 μg/ml indolmycin | This study |
| B736 | B725 TrpRS2[G(−13)T], spontaneous mutant selected at 10 μg/ml indolmycin | This study |
| B737 | B725 TrpRS2[C(−17)A/L9F], spontaneous mutant selected at 10 μg/ml indolmycin | This study |
| B738 | B725 pJS310 | This study |
| B739 | B725 pJS311 | This study |
| B740 | B725 pJS312 | This study |
| B741 | B725 pJS313 | This study |
| B742 | B725 pJS314 | This study |
| B743 | B725 pJS315 | This study |
| B744 | B725 pJS316 | This study |
| B745 | B725 pJS317 | This study |
| B746 | B725 pJS318 | This study |
| B747 | B725 pJS319 | This study |
| B748 | B725 pJS320 | This study |
| B749 | B725 pJS321 | This study |
| B750 | B725 pJS322 | This study |
| B751 | B725 pJS323 | This study |
| B752 | B725 pJS324 | This study |
| B753 | B725 pJS325 | This study |
| S. griseus | ||
| NBRC 13350 | 26 | |
| ATCC 12648 | 28 | |
| S. lividans TK24 | ||
| S. venezuelae ATCC 10712 | ||
| E. coli | ||
| DH5α | F− φ80lacZΔM15 Δ(lacZYA-argF)U169 recA1 endA1 hsdR17 (rK− mK−) phoA supE44 thi-1 gyrA96 relA1 λ− | Invitrogen |
| ET12567 | dam dcm hsdS cat tet | 36 |
Plasmids and primers.
Standard cloning procedures were employed in generating the plasmids listed in Table 2 (30). The site-specific integrating vector pMS81 (10) was used for genetic complementation as previously described (36). pIJ10257 was used for overexpression in S. coelicolor (12). DNA sequencing was performed by Davis Sequencing (Davis, California). Table 3 shows the primers used in this work, all of which were synthesized by Invitrogen. PCR was performed with Taq (Invitrogen) and Pfu (Stratagene, Agilent Technologies). All PCRs were performed with 5% (vol/vol) dimethylsulfoxide (DMSO) (20).
TABLE 2.
Plasmids used in this study
| Plasmid | Description | Vector backbone | Reference or source |
|---|---|---|---|
| pUZ8002 | RP4 derivative, OriT, Kanr | 36 | |
| pGemT | pUC-derived, lacZ′, Ampr | Promega | |
| pBluescript KS+ | pUC ori Ampr | Agilent Technologies (Stratagene) | |
| pMS81 | oriT, ΦBT1 attB-int, Hygr | pSET152 | 10 |
| pIJ10257 | oriT, ΦBT1 attB-int, Hygr, ermEp* | pMS81 | 12 |
| pJS310 | ermEp*-SCO3334 ORF (trpRS1) | pIJ10257 | This study |
| pJS311 | ermEp*-SAV4725 ORF | pIJ10257 | This study |
| pJS312 | ermEp*-SGR3809 ORF | pIJ10257 | This study |
| pJS313 | S. coelicolor TrpRS2(WT) locus | pMS81 | This study |
| pJS314 | S. coelicolor TrpRS2[G(−13)T] locus | pMS81 | This study |
| pJS315 | S. coelicolor TrpRS2[G(−13)T/L9F] locus | pMS81 | This study |
| pJS316 | S. coelicolor TrpRS2 [G(−13)T/H48Q] locus | pMS81 | This study |
| pJS317 | S. coelicolor TrpRS2[C(−17)A] locus | pMS81 | This study |
| pJS318 | S. coelicolor TrpRS2[C(−17)A/L9F] locus | pMS81 | This study |
| pJS319 | S. coelicolor TrpRS2[C(−17)A/H48Q] locus | pMS81 | This study |
| pJS320 | ermEp*-S. coelicolor TrpRS2(L9F) ORF | pIJ10257 | This study |
| pJS321 | ermEp*-S. coelicolor TrpRS2(H48Q) ORF | pIJ10257 | This study |
| pJS322 | ermEp*-S. coelicolor TrpRS2(L9F/H48Q) ORF | pIJ10257 | This study |
| pJS323 | ermEp*-S. coelicolor TrpRS2(Q13K) ORF | pIJ10257 | This study |
| pJS324 | ermEp*-S. coelicolor TrpRS2(L9F/Q13K) ORF | pIJ10257 | This study |
| pJS325 | ermEp*-S. coelicolor TrpRS2(H48N) ORF | pIJ10257 | This study |
| pJS326 | SGI trpRS2 full-length cDNA from indolmycin producer | pGemT | This study |
| pJS327 | SGI3809cDNA fragment from indolmycin producer | pGemT | This study |
| pJS328 | S. coelicolor TrpRS2(WT) ORF | pBluescript KS+ | This study |
| pJS329 | S. coelicolor TrpRS2(L9F) ORF | pBluescript KS+ | This study |
| pJS330 | S. coelicolor TrpRS2[G(−13)T] locus | pBluescript KS+ | This study |
TABLE 3.
Primers used in this study
| Entry | Primer name | Application or function | Sequence (reference) |
|---|---|---|---|
| 1 | TrpRS1 MK54 | Detection of the S. coelicolor trpRS1 (SCO3334) transcript via RT-PCR | 5′-CAG GAG GTG GAC ATA TGA CAC GGG TTT TCA G-3′ (22) |
| 2 | TrpRS1 MK134 | Detection of the S. coelicolor trpRS1 (SCO3334) transcript via RT-PCR | 5′-CAC GTA CCC GGG ATC GGC GGA CAG C-3′ (22) |
| 3 | TrpRS2 MK133 | Detection of the S. coelicolor trpRS2 (SCO4839) transcript via RT-PCR | 5′-GCG TCT CCG GGT CGT CCA GGT ACT G-3′ (22) |
| 4 | TrpRS2 MK135 | Detection of the S. coelicolor trpRS2 (SCO4839) transcript via RT-PCR | 5′-CGC GAC CTC GCG GAC CGC TTC AAC CAG-3′ (22) |
| 5 | SAV3417 RT FOR | Detection of the S. avermitilis SAV3417 transcript via RT-PCR | 5′-CCA CCT CGG CAA CTA CCT C-3′ |
| 6 | SAV3417 RT REV | Detection of the S. avermitilis SAV3417 transcript via RT-PCR | 5′-TTG CCG GTG TAC TTC TCC TC-3′ |
| 7 | SAV4725 RT FOR | Detection of the S. avermitilis SAV4725 transcript via RT-PCR | 5′-ATC TGA CGC TGG GGA ACT AC-3′ |
| 8 | SAV4725 RT REV | Detection of the S. avermitilis SAV4725 transcript via RT-PCR | 5′-CCG TAC CGC TGG TTG AAG-3′ |
| 9 | SGR2702 RT FOR | Detection of the S. griseus NBRC 13350 SGR2702 transcript and corresponding transcript from the indolmycin producer S. griseus ATCC 12648 via RT-PCR | 5′-ACG ACG CCT TCT ACA TGG TC-3′ |
| 10 | SGR2702 RT REV | Detection of the S. griseus NBRC 13350 SGR2702 transcript and corresponding transcript from the indolmycin producer S. griseus ATCC 12648 via RT-PCR | 5′-GCC TGG TAG AGC AGG ATG TC-3′ |
| 11 | SGR3809 RT FOR 1 | Detection of the S. griseus NBRC 13350 SGR3809 transcript via RT-PCR | 5′-ACA CCC GCC GTC ACC AC-3′ |
| 12 | SGR3809 RT REV 1 | Detection of the S. griseus NBRC 13350 SGR3809 transcript via RT-PCR | 5′-GAG AGC ATG ATG TCC GGT TC-3′ |
| 13 | SGR3809 RT FOR 2 | Detection of the S. griseus ATCC 12648 SGR3809 homolog transcript via RT-PCR | 5′-GGC TGC TCC TGG ACT ATC TG-3′ |
| 14 | SGR3809 RT REV 2 | Detection of the S. griseus ATCC 12648 SGR3809 homolog transcript via RT-PCR | 5′-GTC GGG GTC GTA GGT GAT G-3′ |
| 15 | SCO4839 KO DET FOR | Cloning of the S. coelicolor trpRS2 locus located 93 nucleotides upstream of the translational start site | 5′-CCC CGC CCT TGT TAC AC-3′ |
| 16 | SCO4839 KO DET REV | Cloning of the S. coelicolor trpRS2 locus located 96 nucleotides downstream of the translational stop site | 5′-CAA CCG GAG TGA TGT GCA G-3′ |
| 17 | SAV4725 FOR | Cloning of the S. avermitilis SAV4725 ORF | 5′-CAT ATG AAG CGG ATC TTC AGC-3′a |
| 18 | SAV4725 REV | Cloning of the S. avermitilis SAV4725 ORF | 5′-CTC GAG TTA CGC CTC CAG CAA CC-3′b |
| 19 | SCO3334 FOR | Cloning of the S. coelicolor trpRS1 ORF | 5′-CAT ATG ACA CGG GTT TTC AGT G-3′a |
| 20 | SCO3334 REV | Cloning of the S. coelicolor trpRS1 ORF | 5′-CTC GAG CTA CCG GGC CGC GTT C-3′b |
| 21 | SGR3809 FOR | Cloning of the S. griseus NBRC 13350 SGR3809 ORF | 5′-CAT ATG ACC ACA CCC GCC G-3′a |
| 22 | SGR3809 REV 2.0 | Cloning of the S. griseus NBRC 13350 SGR3809 ORF | 5′-CTC GAG CTA CCG GAA CGC GCC CAT C-3′b |
| 23 | SCO4839 L9F FOR | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of L9F mutation | 5′-GAA CGT CCC CGT GTG TTC TCC GGT ATC CAG C-3′ |
| 24 | SCO4839 L9F REV | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of L9F mutation | 5′-GCT GGA TAC CGG AGA ACA CAC GGG GAC-3′ |
| 25 | SCO4839 Q13K FOR | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of Q13K mutation | 5′-GTG CTC TCC GGT ATC AAG CCG ACC TC-3′ |
| 26 | SCO4839 Q13K REV | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of Q13K mutation | 5′-GAG CCG GAG GTC GGC TTG ATA CCG GAG-3′ |
| 27 | SCO4839 H48Q FOR | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of H48Q mutation | 5′-GGT CGT CGA CCT GCA GGC GAT CAC GG-3′ |
| 28 | SCO4839 H48Q REV | Site-directed mutagenesis of the S. coelicolor trpRS2 locus, creation of H48Q mutation | 5′-CGG GAC CGT GAT CGC CTG CAG GTC G-3′ |
The engineered NdeI site is underlined.
The engineered XhoI site is underlined.
Indolmycin and chuangxinmycin.
(±)-Indolmycin was chemically synthesized according to the procedure developed by Hasuoka et al. (11). The 1H and 13C nuclear magnetic resonance spectra, as well as mass spectra, of the synthetic material were identical to those reported for authentic indolmycin (11). All amounts of (±)-synthetic indolmycin described herein are corrected to reflect only the active enantiomer. Chuangxinmycin was generously provided as a gift from Richard L. Jarvest of GlaxoSmithKline (3).
Selection of indolmycin-resistant mutants.
An S. coelicolor B725 (trpRS1::apr; indolmycin sensitive) spore suspension containing 1010 spores was spread over SFM supplemented with 1 μg/ml indolmycin. Several spontaneous low-level indolmycin-resistant mutants arose after incubation at 30°C for 7 days. Fifteen mutants were randomly harvested, and the trpRS2 locus of each mutant was analyzed by PCR using genomic DNA as the template with primers 15 and 16 (Table 3). Four low-level indolmycin-resistant mutants were chosen for selection for higher-level resistance (strains B730 to B733) (Table 1). A suspension containing 5 × 109 spores of each strain was spread over SFM supplemented with 10 μg/ml indolmycin; spontaneous high-level indolmycin-resistant mutants arose from each strain after incubation at 30°C for 7 days (strains B734 to B737) (Table 1).
Site-directed mutagenesis.
Mutations were created in the S. coelicolor trpRS2 open reading frame (ORF) using the Stratagene QuikChange site-directed mutagenesis kit by following the manufacturer's protocol. Using plasmid pJS330 (Table 2) as the template with primers 23 and 24 (Table 3), the TrpRS2 [G(−13)T/L9F] locus was created. The TrpRS2[G(−13)T/H48Q] locus was created using pJS330 as the template with primers 27 and 28 (Table 3). Plasmid pJS329 (Table 2) was used as the template with primers 25 and 26 (Table 3) to create the TrpRS2(L9F/Q13K) ORF, and the TrpRS2(L9F/H48Q) ORF was created using pJS329 as the template with primers 27 and 28. The TrpRS2(Q13K) ORF was created using plasmid pJS328 (Table 2) as the template with primers 25 and 26.
MIC assays.
All MIC assays were performed on Difco nutrient agar medium supplemented with the indicated concentrations of indolmycin. Growth was assessed after incubation at 30°C for 48 h.
RNA isolation and RT-PCR.
The transcriptional analyses of the S. coelicolor trpRS1 and trpRS2 genes were performed as described previously (36). To analyze the transcription of the tryptophanyl-tRNA synthetase genes in other Streptomyces species, two NMMP cultures were inoculated for each organism to test transcription in the presence or absence of indolmycin. Strains were grown for 21 h prior to treatment with 40 μg/ml indolmycin for 3 h. Cells were washed once with 10.3% (wt/vol) aqueous sucrose, resuspended in L (lysis) buffer (20), and incubated for 15 min at 30°C. Total RNA then was isolated using the RNeasy Mini kit (Qiagen) by following the manufacturer's protocol. The concentration of each purified, DNA-free total RNA isolate was measured with a NanoDrop ND-1000 spectrophotometer. An equal quantity of total RNA (1.8 μg) was employed in all reverse transcription-PCRs (RT-PCRs). RT-PCR was performed with the OneStep RT-PCR kit (Qiagen) according to the manufacturer's protocol for transcripts with high GC content (which requires the use of the Q-solution). Primers used for RT-PCR analyses are listed in Table 3 (primers 1 to 14). The PCR program used for the detection of all transcripts was 50°C for 30 min, 95°C for 15 min, N cycles of 94°C for 30 s, 58°C for 30 s, and 72°C for 60 s, and a final elongation at 72°C for 10 min. For the analysis of SAV3417, 35 cycles was employed. All other genes were analyzed at 25 cycles except SAV4725 and SGR3809, which were analyzed at 20 cycles. No signals were detected in control experiments with Pfu polymerase, indicating that the RT-PCR signals correspond to the amplification of transcripts.
Detection of indolmycin in culture media by LC-MS.
A published procedure was adapted for the isolation and detection of indolmycin (37). For the LC-MS analysis of secreted indolmycin in culture supernatants, S. griseus ATCC 12648 was grown in NMMP without PEG. Culture filtrates then were adjusted to pH 3 with 4N HCl and extracted twice with 20 ml ethyl acetate. The organic phases were combined and extracted with 4 ml of a 10% (wt/vol) Na2CO3 solution and then dried over Na2SO4. Solvent was removed under reduced pressure to leave residues that were purified twice by solid-phase extraction using strata-x 60-mg, 3-ml columns (part no. 8B-S100-UBJ-TN; Phenomenex) by following the manufacturer's protocol. Purified residues were dissolved in 100 μl methanol for LC-MS analysis. LC-MS analysis was performed with a Thermo LCQ DECA XP MAX ion trap mass spectrometer (C18 column; gradient: 5 to 65% mobile phase B for 30 min, where mobile phase B is acetonitrile plus 0.1% formic acid and mobile phase A is water plus 0.1% formic acid; Waters part no. WAT058965).
Sequence accession numbers.
All sequences described in this work are available at the NCBI database under the accession numbers listed in Table S1 in the supplemental material. The nucleotide sequences of both tryptophanyl-tRNA synthetase genes from the indolmycin producer S. griseus ATCC 12648 were deposited in the GenBank database under accession numbers FJ744752 (SGI3809) and FJ744751 (SGItrpRS2).
RESULTS
An auxiliary tryptophanyl-tRNA synthetase gene from S. griseus NBRC 13350 encodes an indolmycin-resistant enzyme.
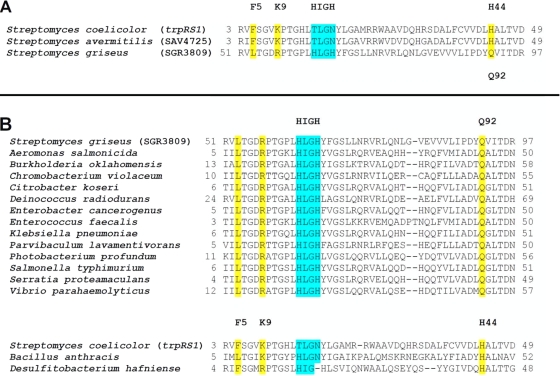
Bioinformatic analysis revealed that Streptomyces griseus NBRC 13350 has a unique auxiliary tryptophanyl-tRNA synthetase gene (SGR3809) (Fig. 2A). The tryptophanyl-tRNA synthetase encoded by SGR3809 is only 34% identical in amino acid sequence to TrpRS1, a known indolmycin resistance determinant from S. coelicolor. Curiously, auxiliary tryptophanyl-tRNA synthetases homologous to SGR3809 were observed in several bacterial genera (Fig. 2B). We detected a cDNA 93% identical in sequence to SGR3809 by the RT-PCR analysis of RNA from the indolmycin producer, Streptomyces griseus ATCC 12648 (see Fig. S1 in the supplemental material). The indolmycin producer is classified distinctly from S. griseus NBRC 13350, which does not produce indolmycin.
FIG. 2.
(A) Alignment of trpRS1 with other indolmycin resistance genes. The aligned sequences show the region surrounding the HIGH signature consensus of class I aminoacyl-tRNA synthetases. Positions found to correlate to indolmycin resistance in this study are shaded yellow, and the class I aminoacyl-tRNA synthetase signature sequence HIGH is shaded blue. trpRS1 is highly similar in sequence to the indolmycin-resistant tryptophanyl-tRNA synthetase gene SAV4725 from S. avermitilis but is dissimilar to the indolmycin-resistant tryptophanyl-tRNA synthetase gene SGR3809 from S. griseus NBRC 13350 (SGR3809). NCBI accession numbers are provided in the supplementary information (see Table S1 in the supplemental material). (B) Translated sequences of the trpRS1 and SGR3809 genes aligned with homologs from various bacterial species. NCBI accession numbers are provided in the supplementary information (see Table S1 in the supplemental material).
The observation of an SGR3809 homolog in the indolmycin producer and the robust growth of S. griseus NBRC 13350 in media supplemented with inhibitory concentrations of indolmycin suggested that SGR3809 encodes an antibiotic-resistant enzyme. S. griseus NBRC 13350, like all other indolmycin-resistant streptomycetes, also grows in the presence of chuangxinmycin (Fig. 3); these are the only bacteria known to be resistant to chuangxinmycin. To determine if SGR3809 is an antibiotic resistance gene, it was heterologously expressed in Streptomyces coelicolor B725, the indolmycin-sensitive trpRS1 null strain (Table 1) (36). In this genetic background, its capacity to confer indolmycin resistance was compared to that of trpRS1 and its homolog in S. avermitilis (SAV4725). The indolmycin MIC for S. coelicolor B725 increased from 0.25 to 15 μg/ml upon the expression of the novel tryptophanyl-tRNA synthetase gene SGR3809 (Table 4). A similar MIC elevation was observed upon the expression of trpRS1 in this background (Table 4). Thus, SGR3809 encodes an antibiotic-resistant tryptophanyl-tRNA synthetase.
FIG. 3.
Various Streptomyces species grown in the presence of inhibitory concentrations (100 μM) of indolmycin and chuangxinmycin. SAV, Streptomyces avermitilis ATCC 31267; SCO, Streptomyces coelicolor M600; SGI, Streptomyces griseus ATCC 12648; SGR, Streptomyces griseus NBRC 13350; SLI, Streptomyces lividans TK24; SVZ, Streptomyces venezuelae ATCC 10712.
TABLE 4.
Comparison of indolmycin resistance genes from Streptomyces species
| Entry | ORFa expressed in B725 (indolmycin-sensitive S. coelicolor) | MICb (μg/ml) |
|---|---|---|
| 1 | S. coelicolor B725 (trpRS1 null strain) | 0.25 |
| 2 | Wild-type S. coelicolor | >150 |
| 3 | S. coelicolor trpRS1 (SCO3334) | 10 |
| 4 | S. avermitilis SAV4725 (trpRS1 homolog) | 5 |
| 5 | S. griseus NBRC 13350 SGR3809 | 15 |
All ORFs were introduced into strain B725 under the ermE* promoter for equalized expression in vivo (see Materials and Methods).
The MIC is the concentration of indolmycin sufficient to inhibit the growth of each strain after 2 days on Difco nutrient agar (see Materials and Methods).
Antibiotic-resistant tryptophanyl-tRNA synthetase genes are transcribed differently.
The transcription of the S. coelicolor trpRS1 gene is induced in the presence of indolmycin and chuangxinmycin (22, 36). Transcriptional analyses of the antibiotic-resistant tryptophanyl-tRNA synthetase genes in other streptomycetes were performed to determine if they are regulated in a similar fashion. Using RT-PCR analysis, we found that the transcription of the trpRS1 ortholog in S. avermitilis (SAV4725) also is induced by indolmycin (Fig. 4A). In contrast, SGR3809 in S. griseus NBRC 13350 and its ortholog in the indolmycin producer were constitutively transcribed (Fig. 4B). Curiously, the transcript of the SGR3809 ortholog from the indolmycin producer was present when secreted indolmycin could not be detected by LC-MS (Fig. 4B; also see Fig. S5 in the supplemental material). This observation is noteworthy because in antibiotic-producing organisms, resistance genes often are cotranscribed with genes encoding enzymes for antibiotic biosynthesis (13, 33).
FIG. 4.
RT-PCR analyses of the tryptophanyl-tRNA synthetase genes from indolmycin and chuangxinmycin-resistant Streptomyces species. (A) RT-PCR analyses of tryptophanyl-tRNA synthetase genes in S. avermitilis and S. coelicolor. The transcription of the trpRS1 homolog SAV4725 also is induced in S. avermitilis upon exposure to indolmycin. (B) RT-PCR analyses of tryptophanyl-tRNA synthetase genes in the streptomycin producer S. griseus NBRC 13350 and in the indolmycin producer S. griseus ATCC 12648. The transcription of these genes was not influenced by indolmycin.
Selection of indolmycin-resistant mutants yields point mutations in the tryptophanyl-tRNA synthetase ORF and promoter.
We used the indolmycin-sensitive S. coelicolor trpRS1 null strain B725 to select for spontaneous indolmycin-resistant mutants. We sought to compare the identities of resistance-conferring substitutions to the sequences of the native indolmycin-resistant enzymes. This strain lacks trpRS1 but has the trpRS2 gene that encodes an indolmycin-sensitive tryptophanyl-tRNA synthetase. In the initial selection, the indolmycin-sensitive trpRS1 null mutant (MIC, 0.25 μg/ml) was grown on solid medium supplemented with 1 μg/ml of indolmycin. Spontaneous indolmycin-resistant mutants were observed at a frequency of approximately 10−8. Fifteen indolmycin-resistant mutants were isolated, and their TrpRS2 loci were cloned and sequenced. Only 1 of the 15 strains had a mutation in the trpRS2 locus; mutations in the other strains were not identified. This strain (B730; see Table S1 in the supplemental material) had a single point mutation in the trpRS2 ORF that changed leucine at position 9 to phenylalanine [TrpRS2(L9F)].
A number of high-level resistant strains were selected from the low-level resistant strains (i.e., strain B730 and strains B731 to B733 with unidentified resistance-conferring mutations). The selected high-level resistant strains had point mutations in the trpRS2 ORF and/or upstream of the trpRS2 transcription start site. Two strains selected at 10 μg/ml had single point mutations in the trpRS2 ORF that resulted in substitutions of the histidine at position 48 of the synthetase; one strain (B734) had TrpRS2(H48N) and the other (B735) had TrpRS2(H48Q).
To enable the direct comparison of the trpRS2 point mutants and the trpRS1 and SGR3809 genes, they were cloned into pIJ10257 for expression under the control of the constitutive ermE* promoter (ermE*p) and introduced into the S. coelicolor trpRS1 null strain (B725). TrpRS2 L9F increased the MIC for the null strain 20-fold (Table 5); by comparison, TrpRS1 increased the MIC 40-fold (Table 4). It is remarkable that TrpRS2(H48N) and TrpRS2(H48Q) increased the MIC for the null strain more than 300-fold (Table 5), far more than the native resistance genes (Table 4).
TABLE 5.
Comparison of resistance-conferring point mutations in the S. coelicolor trpRS2 locus
| Entry | ORFa or locusb introduced into B725 (indolmycin-sensitive S. coelicolor) | MICc (μg/ml) | Fold increase in MICd |
|---|---|---|---|
| 1 | S. coelicolor trpRS2 ORF | 0.25 | 1 |
| 2 | S. coelicolor TrpRS2(L9F) ORF | 5 | 20 |
| 3 | S. coelicolor TrpRS2(H48Q) ORF | >75 | >300 |
| 4 | S. coelicolor TrpRS2(H48N) ORF | >75 | >300 |
| 5 | S. coelicolor TrpRS2(Q13K) ORF | 3 | 12 |
| 6 | S. coelicolor TrpRS2(L9F/Q13K) ORF | 8 | 32 |
| 7 | S. coelicolor TrpRS2(L9F/H48Q) ORF | >75 | >300 |
| 8 | S. coelicolor trpRS2 locus | 0.25 | 1 |
| 9 | S. coelicolor TrpRS2[C(−17)A] locus | 2 | 8 |
| 10 | S. coelicolor TrpRS2[C(−17)A/L9F] locus | 5 | 20 |
| 11 | S. coelicolor TrpRS2[C(−17)A/H48Q] locus | >75 | >300 |
| 12 | S. coelicolor TrpRS2[G(−13)T] locus | 5 | 20 |
| 13 | S. coelicolor TrpRS2[G(−13)T/L9F] locus | 12 | 48 |
| 14 | S. coelicolor TrpRS2[G(−13)T/H48Q] locus | >75 | >300 |
All ORFs were introduced into strain B725 under the ermE* promoter for equalized expression in vivo (see Materials and Methods).
Locus refers to the region spanning 93 nucleotides upstream and 96 nucleotides downstream of the trpRS2 ORF (see Materials and Methods).
MIC is the concentration of indolmycin sufficient to inhibit the growth of each strain after 2 days on Difco nutrient agar (see Materials and Methods).
Fold increase in MIC relative to that of indolmycin-sensitive S. coelicolor strain B725 (MIC = 0.25 μg/ml). Note that wild-type S. coelicolor (MIC > 150 μg/ml) is more than 600-fold more resistant to indolmycin than strain B725.
Two spontaneous high-level indolmycin-resistant strains had point mutations immediately upstream of the trpRS2 ORF. These mutations were predicted to lie within the trpRS2 promoter region (36) (Fig. 5). One strain (B736) (Table 1) had a point mutation (G to T) 13 nucleotides upstream of the predicted trpRS2 start codon. This mutation changed the sequence of the predicted −10 region (GAGAAT to TAGAAT; the change is in boldface) such that it matched the −10 consensus (T-A-G-purine-purine-T) for streptomycete promoters (31) (Fig. 5). The other strain (B737) (Table 1) had a point mutation (C to A) in the spacer region between the −10 and −35 regions of the trpRS2 promoter, as well as a mutation in the ORF that substitutes phenylalanine for leucine at position 9 (Fig. 5). To compare the resistance-conferring promoter mutations, trpRS2 loci with either the mutation in the −10 region or the mutation in the spacer region were cloned and introduced into the S. coelicolor trpRS1 null strain B725 via the integrative plasmid pMS81. The G-to-T mutation in the −10 region increased the MIC 20-fold, while the C-to-A mutation in the −10 and −35 spacer increased the MIC only 8-fold (Table 5). The results of these selections demonstrate that point mutations in the trpRS2 promoter can contribute significantly to indolmycin resistance.
FIG. 5.
Mutations in the trpRS2 promoter that confer resistance to indolmycin. Brackets mark the boundaries of the trpRS2 promoter. The −10 and −35 regions are in boldface, and the spontaneous mutation sites are shaded gray.
Combinations of mutations in the trpRS2 locus synergistically enhance indolmycin resistance.
We used site-directed mutagenesis to determine if specific combinations of mutations in the trpRS2 locus would act synergistically with respect to indolmycin resistance. Indeed, promoter mutations and ORF mutations enhanced indolmycin resistance synergistically (Table 5). We also examined combinations of resistance-conferring point mutations in the trpRS2 ORF. The mutation causing the L9F substitution was combined with a mutation that changes glutamine at position 13 to lysine (Q13K). The former mutation increased the MIC for the null strain 20-fold (Table 5). The latter mutation was reported to confer weak resistance to trpRS2 (22), and in our studies it enhanced the MIC for the null strain only 12-fold (Table 5). These mutations acted synergistically; the MIC for the null strain expressing the double mutant was 32-fold higher than that for the parent (Table 5). It is interesting that this TrpRS2 (L9F/Q13K) double mutant confers nearly as much indolmycin resistance as TrpRS1 (Tables 4 and 5). The combination of L9F and H48Q did not have an obvious effect on indolmycin resistance below 300 μg/ml (Table 5), but the strain expressing this double mutant grew poorly compared to the growth of the wild-type strain (data not shown).
DISCUSSION
We identified a new, indolmycin-resistant tryptophanyl-tRNA synthetase gene (SGR3809) in S. griseus NBRC 13350 whose product has low homology to a known antibiotic-resistant tryptophanyl-tRNA synthetase (trpRS1 in S. coelicolor) and high homology to a gene in the indolmycin producer S. griseus ATCC 12648. Selections for indolmycin-resistant bacterial strains led to the discovery of point mutations in the tryptophanyl-tRNA synthetase ORF and promoter that confer indolmycin resistance. In some cases, there were novel point mutations in the trpRS2 gene that resulted in products with sequences similar to those of the products of the native resistance genes. For instance, the resistance-conferring L9F substitution in S. coelicolor TrpRS2 has never been reported, but a phenylalanine is located at the analogous position of the indolmycin-resistant enzyme TrpRS1. Likewise, the H48Q substitution in S. coelicolor TrpRS2 that we identified has never been reported, but a glutamine is located at the analogous position of the SGR3809 product. The H48N substitution in the indolmycin-resistant TrpRS2 that we observed is analogous to the H43N substitution observed in indolmycin-resistant tryptophanyl-tRNA synthetases of Bacillus stearothermophilus (22) and Staphylococcus aureus (16). A consensus of substitutions at this position reflects the fact that the histidine makes a critical hydrogen bond to indolmycin (22). In addition to the ORF mutations, we observed promoter mutations. To our knowledge, this is the first time that promoter mutations have been reported in resistance to aminoacyl-tRNA synthetase inhibitors. Mutations in the trpRS2 promoter presumably enhance the expression of the tryptophanyl-tRNA synthetase gene to levels that confer resistance via titration.
In this work, analyses of streptomycete genome sequences led to the discovery of a new indolmycin resistance determinant. As producers of nearly half of the 10,000 known antibiotics, Streptomyces bacteria have been particularly important in drug discovery and are a major source of drug resistance genes (14). It is tempting to speculate that homologs of SGR3809 in other bacterial genera encode antibiotic-resistant tryptophanyl-tRNA synthetases. In any case, it is intriguing that genome mining can be used to predict resistance and/or guide the development of aminoacyl-tRNA synthetase inhibitors and other types of drugs (6, 24). Accordingly, one can predict that resistance to indolmycin and chuangxinmycin is widespread.
Supplementary Material
Acknowledgments
We acknowledge Tun Li Shen for LC-MS assistance and Richard Jarvest of GlaxoSmithKline for generously donating the chuangxinmycin used in this work.
J.J.V. acknowledges an NSF EPSCoR fellowship. Brown University is gratefully acknowledged for funding.
Footnotes
Published ahead of print on 22 June 2009.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Bentley, S. D., K. F. Chater, A. M. Cerdeño-Tarraga, G. L. Challis, N. R. Thomson, K. D. James, et al. 2002. Complete genome sequence of the model actinomycete Streptomyces coelicolor. Nature 417:141-147. [DOI] [PubMed] [Google Scholar]
- 2.Brown, J. R., D. Gentry, J. A. Becker, K. Ingraham, D. J. Holmes, and M. J. Stanhope. 2003. Horizontal transfer of drug-resistant aminoacyl-transfer-RNA synthetases of anthrax and gram-positive pathogens. EMBO Rep. 4:692-698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown, M. J., P. S. Carter, A. E. Fenwick, A. P. Fosberry, D. W. Hamprecht, M. J. Hibbs, et al. 2002. The antimicrobial natural product chuangxinmycin and some synthetic analogues are potent and selective inhibitors of bacterial tryptophanyl-tRNA synthetase. Bioorg. Med. Chem. Lett. 12:3171-3174. [DOI] [PubMed] [Google Scholar]
- 4.Casewell, M. W., and R. L. Hill. 1987. Mupirocin (pseudomonic acid)-a promising new topical antimicrobial agent. J. Antimicrob. Chemother. 19:1-5. [DOI] [PubMed] [Google Scholar]
- 5.Davies, J. 2008. Resistance redux. Infectious diseases, antibiotic resistance and the future of mankind. EMBO Rep. 9:S18-S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Costa, V. M., K. M. McGrann, D. W. Hughes, and G. D. Wright. 2006. Sampling the antibiotic resistome. Science 311:374-377. [DOI] [PubMed] [Google Scholar]
- 7.El-Sayed, A. K., J. Hothersall, S. M. Cooper, E. Stephens, T. J. Simpson, and C. M. Thomas. 2003. Characterization of the mupirocin biosynthesis gene cluster from Pseudomonas fluorescens NCIMB 10586. Chem. Biol. 10:419-430. [DOI] [PubMed] [Google Scholar]
- 8.Fuller, A. T., G. Mellows, M. Woolford, G. T. Banks, K. D. Barrow, and E. B. Chain. 1971. Pseudomonic acid: an antibiotic produced by Pseudomonas fluorescens. Nature 234:416-417. [DOI] [PubMed] [Google Scholar]
- 9.Gentry, D. R., K. A. Ingraham, M. J. Stanhope, S. Rittenhouse, R. L. Jarvest, P. J. O'Hanlon, et al. 2003. Variable sensitivity to bacterial methionyl-tRNA synthetase inhibitors reveals subpopulations of Streptococcus pneumoniae with two distinct methionyl-tRNA synthetase genes. Antimicrob. Agents Chemother. 47:1784-1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gregory, M. A., R. Till, and M. C. M. Smith. 2003. Integration site for Streptomyces phage ΦBT1 and development of site-specific integrating vectors. J. Bacteriol. 185:5320-5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hasuoka, A., Y. Nakayama, M. Adachi, H. Kamiguchi, and K. Kamiyama. 2001. Development of a stereoselective practical synthetic route to indolmycin, a candidate anti-H. pylori agent. Chem. Pharm. Bull. 49:1604-1608. [DOI] [PubMed] [Google Scholar]
- 12.Hong, H. J., M. I. Hutchings, L. M. Hill, and M. J. Buttner. 2005. The role of the novel Fem protein VanK in vancomycin resistance in. Streptomyces coelicolor. J. Biol. Chem. 280:13055-13061. [DOI] [PubMed] [Google Scholar]
- 13.Hopwood, D. A. 2007. How do antibiotic-producing bacteria ensure their self-resistance before antibiotic biosynthesis incapacitates them? Mol. Microbiol. 63:937-940. [DOI] [PubMed] [Google Scholar]
- 14.Hopwood, D. A. 2007. Streptomyces in nature and medicine. Oxford University Press, New York, NY.
- 15.Hughes, J., and G. Mellows. 1978. Inhibition of isoleucyl-transfer ribonucleic acid synthetase in Escherichia coli by pseudomonic acid. Biochem. J. 176:305-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurdle, J. G., A. J. O' Neill, and I. Chopra. 2004. Anti-staphylococcal activity of indolmycin, a potential topical agent for control of staphylococcal infections. J. Antimicrob. Chemother. 54:549-552. [DOI] [PubMed] [Google Scholar]
- 17.Hurdle, J. G., A. J. O'Neill, and I. Chopra. 2005. Prospects for aminoacyl-tRNA synthetase inhibitors as new antimicrobial agents. Antimicrob. Agents Chemother. 49:4821-4833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ikeda, H., J. Ishikawa, A. Hanamoto, M. Shinose, H. Kikuchi, T. Shiba, Y. Sakaki, M. Hattori, and S. Omura. 2003. Complete genome sequence and comparative analysis of the industrial microorganism Streptomyces avermitilis. Nat. Biotechnol. 21:526-531. [DOI] [PubMed] [Google Scholar]
- 19.Kanamaru, T., Y. Nakano, Y. Toyoda, K. I. Miyagawa, M. Tada, T. Kaisho, and M. Nakao. 2001. In vitro and in vivo antibacterial activities of TAK-083, an agent for treatment of Helicobacter pylori infection. Antimicrob. Agents Chemother. 45:2455-2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kieser, T., M. J. Bibb, M. J. Buttner, K. F. Chater, and D. A. Hopwood. 2000. Practical Streptomyces genetics. John Innes Foundation, Norwich, CT.
- 21.Kim, S., S. W. Lee, E. C. Choi, and S. Y. Choi. 2003. Aminoacyl-tRNA synthetases and their inhibitors as a novel family of antibiotics. Appl. Microbiol. Biotechnol. 61:278-288. [DOI] [PubMed] [Google Scholar]
- 22.Kitabatake, M., K. Ali, A. Demain, K. Sakamoto, S. Yokoyama, and D. Söll. 2002. Indolmycin resistance of Streptomyces coelicolor A3(2) by induced expression of one of its two tryptophanyl-tRNA synthetases. J. Biol. Chem. 277:23882-23887. [DOI] [PubMed] [Google Scholar]
- 23.Marsh, W. S., A. L. Garretson, and E. M. Wesel. 1960. PA 155 A, B, and X antibiotics produced by a strain of Streptomyces albus. Antibiot. Chemother. 10:316-320. [PubMed] [Google Scholar]
- 24.Martínez, J. L., F. Baquero, and D. I. Andersson. 2007. Predicting antibiotic resistance. Nat. Rev. Microbiol. 5:958-965. [DOI] [PubMed] [Google Scholar]
- 25.Ochsner, U. A., X. Sun, T. Jarvis, I. Critchley, and N. Janjic. 2007. Aminoacyl-tRNA synthetases: essential and still promising targets for new anti-infective agents. Expert Opin. Investig. Drugs 16:573-593. [DOI] [PubMed] [Google Scholar]
- 26.Ohnishi, Y., J. Ishikawa, H. Hara, H. Suzuki, M. Ikenoya, H. Ikeda, A. Yamashita, M. Hattori, and S. Horinouchi. 2008. Genome sequence of the streptomycin-producing microorganism Streptomyces griseus IFO 13350. J. Bacteriol. 190:4050-4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Omura, S., H. Ikeda, J. Ishikawa, A. Hanamoto, C. Takahashi, M. Shinose, Y. Takahashi, H. Horikawa, H. Nakazawa, T. Osonoe, H. Kikuchi, T. Shiba, Y. Sakaki, and M. Hattori. 2001. Genome sequence of an industrial microorganism Streptomyces avermitilis: deducing the ability of producing secondary metabolites. Proc. Natl. Acad. Sci. USA 98:12215-12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pohlmann, J., and H. Broetz-Oesterhelt. 2004. New aminoacyl-tRNA synthetase inhibitors as antibacterial agents. Curr. Drug. Targets 4:261-272. [DOI] [PubMed] [Google Scholar]
- 29.Routien, J. B. 1966. Identity of streptomycete producing antibiotic PA155A. J. Bacteriol. 91:1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 31.Strohl, W. R. 1992. Compilation and analysis of DNA sequences associated with apparent streptomycete promoters. Nucleic Acids Res. 20:961-974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sutherland, R., R. J. Boon, K. E. Griffin, P. J. Masters, B. Slocombe, and A. R. White. 1985. Antibacterial activity of mupirocin (pseudomonic acid), a new antibiotic for topical use. Antimicrob. Agents Chemother. 27:495-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tahlan, K., S. K. Ahn, A. Sing, T. D. Bodnaruk, A. R. Willems, A. R. Davidson, and J. R. Nodwell. 2007. Initiation of actinorhodin export in Streptomyces coelicolor. Mol. Microbiol. 63:951-961. [DOI] [PubMed] [Google Scholar]
- 34.Tao, J., and P. Schimmel. 2000. Inhibitors of aminoacyl-tRNA synthetases as novel anti-infectives. Expert Opin. Investig. Drugs 9:1767-1775. [DOI] [PubMed] [Google Scholar]
- 35.Udo, E. E., L. E. Jacob, and E. M. Mokadas. 1997. Conjugative transfer of high-level mupirocin resistance from Staphylococcus haemolyticus to other staphylococci. Antimicrob. Agents Chemother. 41:693-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vecchione, J. J., and J. K. Sello. 2008. Characterization of an inducible, antibiotic-resistant aminoacyl-tRNA synthetase gene in Streptomyces coelicolor. J. Bacteriol. 190:6253-6257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Werner, R. G., and A. L. Demain. 1981. Directed biosynthesis of new indolmycins. J. Antibiot. 34:551-554. [DOI] [PubMed] [Google Scholar]
- 38.Werner, R. G., L. F. Thorpe, W. Reuter, and K. H. Nierhaus. 1976. Indolmycin inhibits prokaryotic tryptophanyl-tRNA ligase. Eur. J. Biochem. 68:1-3. [DOI] [PubMed] [Google Scholar]
- 39.Yanagisawa, T., and M. Kawakami. 2003. How does Pseudomonas fluorescens avoid suicide from its antibiotic pseudomonic acid? Evidence for two evolutionarily distinct isoleucyl-tRNA synthetases conferring self-defense. J. Biol. Chem. 278:25887-25894. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.