Abstract
Considerable evidence supports the concept that CD4+ T cells are important in sarcoidosis pathogenesis, but the antigens responsible for the observed Th1 immunophenotype remain elusive. The epidemiologic association with bioaerosols and the presence of granulomatous inflammation support consideration of mycobacterial antigens. To explore the role of mycobacterial antigens in sarcoidosis immunopathogenesis, we assessed the immune recognition of mycobacterial antigens, the 6-kDa early secreted antigenic protein (ESAT-6) and catalase-peroxidase (KatG), by T cells derived from bronchoalveolar lavage (BAL) fluid obtained during diagnostic bronchoscopy. We report the presence of antigen-specific recognition of ESAT-6 and KatG in T cells from BAL fluid of 32/44 sarcoidosis subjects, compared to 1/27 controls (P < 0.0001). CD4+ T cells were primarily responsible for immune recognition (32/44 sarcoidosis subjects), although CD8+ T-cell responses were observed (25/41 sarcoidosis subjects). Recognition was significantly absent from BAL fluid cells of patients with other lung diseases, including infectious granulomatous diseases. Blocking of Toll-like receptor 2 reduced the strength of the observed immune response. The presence of immune responses to mycobacterial antigens in cells from BAL fluid used for sarcoidosis diagnosis suggests a strong association between mycobacteria and sarcoidosis pathogenesis. Inhibition of immune recognition with monoclonal antibody against Toll-like receptor 2 suggests that induction of innate immunity by mycobacteria contributes to the polarized Th1 immune response.
Sarcoidosis is a multisystem granulomatous disease of unknown etiology, characterized by a Th1 immunophenotype. The epidemiology and immunology of sarcoidosis suggest that an infectious agent could be involved in its pathogenesis. Immunologic studies of sarcoidosis have detected oligoclonal T cells in the sarcoid granuloma, consistent with a major histocompatibility complex-restricted antigen-driven process (33, 42). Analysis of cells from bronchoalveolar lavage (BAL) fluid from patients with acute forms of sarcoidosis has demonstrated overrepresentation of specific T-cell receptor alleles in combination with DRB3*0101 and DRB1*0301 major histocompatibility complex restrictions, strongly implicating an antigen-specific response in sarcoidosis pathogenesis (21).
Because sarcoidosis most commonly involves the lungs, eyes, and skin, the search for environmental causes has centered on exposures to airborne antigens (26). Several reports have noted associations with occupations such as agriculture, metalworking, firefighting, and the handling of building supplies (3, 30, 32, 38). The association of sarcoidosis with these occupations raises the possibility that disease may be caused by exposure to microbial bioaerosols, including inorganic particles, insecticides, and aerosols from moldy environments (3, 32, 35, 39). Sarcoidosis also demonstrates a seasonal and geographic variability (12, 29, 34, 50). The transmissibility, clustering of cases, and geographic and seasonal variability suggest that environmental factors are important in the acquisition of sarcoidosis. Moreover, these environmental risk factors correlate well with the typical distribution of environmental mycobacteria.
The potential role of mycobacteria in sarcoidosis immunopathogenesis is supported by recent studies reporting detection of mycobacterial proteins and nucleic acids in sarcoidosis granulomas, as well as humoral and peripheral cellular immune responses to mycobacterial antigen in sarcoidosis subjects (4, 9, 13-17, 22, 44). However, in order to understand disease pathogenesis, it is crucial to analyze the immunologic response at the site of active sarcoidosis involvement. Although sarcoidosis is a systemic disease, it most commonly affects the lungs. Taking advantage of the observation that most patients undergo bronchoscopy with BAL as a routine investigation (49), we assessed the specific immune recognition of mycobacterial virulence factors by T cells from BAL fluid derived from sarcoidosis patients from geographically distinct locales.
In order to investigate the role of mycobacterial antigen in lung involvement in sarcoidosis, we analyzed specific responses of BAL fluid-derived T cells to the mycobacterial 6-kDa early secreted antigenic protein (ESAT-6) and catalase-peroxidase (KatG). We chose ESAT-6 and KatG peptides due to prior reports of systemic cellular immune responses to these microbial virulence factors in sarcoidosis subjects (9, 13).
MATERIALS AND METHODS
Study subjects.
The study participants were recruited from the Cleveland Clinic, the Medical University of South Carolina, and Vanderbilt University Medical Center. We prospectively enrolled patients who were undergoing bronchoscopy and for whom sarcoidosis was a diagnostic consideration (Table 1; see Table S1 in the supplemental material). All subjects provided written informed consent that was approved by the appropriate Institutional Review Boards. Seventy-one patients were enrolled in this study. Forty-four were diagnosed with sarcoidosis, and 27 subjects had an alternative diagnosis reached after workup (Table 1; see Table S1 in the supplemental material). The 44 sarcoidosis subjects included 15 African-Americans, 28 Caucasians, and 1 Caucasian-Hispanic, and 25 of the subjects were males. The median age of the sarcoidosis subjects was 45 years. The 27 disease controls included 4 African Americans and 23 Caucasians, and 11 controls were males. Their median age was 60 years. All the sarcoidosis subjects who underwent tuberculin skin testing at the discretion of their physician were skin test negative. A Wilcoxon rank sum test used to determine whether there was a difference in age distributions between the two diagnostic groups indicated a significant difference (P < 0.0009; Table 1); there was no difference according to race or sex (Table 1).
TABLE 1.
Characteristics of the study populationa
| Characteristic | Value for:
|
P value | |
|---|---|---|---|
| Sarcoidosis patients | Disease controls | ||
| No. of: | |||
| Patients (total) | 44 | 27 | NS |
| Females/males | 19/25 | 11/16 | NS |
| African-Americans, Caucasians, and Caucasian/Hispanics | 15, 28, 1 | 4, 23 | NS |
| Patients at stage 0/1/2/3/4 | 0/11/25/5/3 | ND | |
| Patients with IS at bronchoscopy | 13 | 5 | |
| Patients with response to ESAT-6 or KatG/total no. | |||
| CD4+ | 32/44 | 1/27 | 0.00005 |
| CD8+ | 25/41 | 1/26 | 0.0003 |
| Median yr of age (min, max) | 45 (21, 80) | 60 (28, 79) | 0.0009 |
| Median % Lym (min, max) | 17 (1, 66) | 6 (1, 85) | NS |
Comparison between the two groups for sex, age, and race were assessed using the Wilcoxon rank sum test. Fisher's exact test was used to compare CD4+ and CD8+ responders across the two groups. The CD4+ or CD8+ response was defined as positive when the frequency of recognition was at least twice background fluorescence and greater than 0.5%. min, minimum; max, maximum; IS, immunosuppression; Lym, lymphocyte; ND, not done; NS, not significant.
The subjects had their chest radiographs or chest computer tomography scans staged according to the method described by Scadding (41) as follows: stage 0, no infiltrates or adenopathy; stage 1, hilar adenopathy alone; stage 2, adenopathy plus infiltrates; stage 3, infiltrates alone; and stage 4, fibrosis. Unlike the traditional Scadding system, these determinations were made by viewing the chest computer tomography scan when one was available (it was available for 46/71 subjects). Otherwise, the chest radiograph was used for this staging.
Histopathological diagnosis of sarcoidosis was confirmed by a pathologist (i.e., specimens from each patient had confluent noncaseating granulomas, with negative cultures and stains for bacteria, fungi, and acid-fast bacilli), and there was no history of exposure to antigens known to cause granulomatous lung disease. Disease controls were subjects for whom an alternate diagnosis was obtained after bronchoscopy.
BAL fluid and PBMC isolation and culture.
BAL fluid was obtained from diagnostic bronchoscopy and centrifuged at 1,500 rpm for 15 min. The BAL fluid cell pellet was washed with supplemented RPMI 1640 medium. Peripheral blood mononuclear cells (PBMC) were separated from buffy coats of sarcoidosis subjects and disease controls through Ficoll-Hypaque gradient centrifugation (GE Healthcare). BAL fluid cells and PBMC were either stored in liquid nitrogen in freezing medium for future analysis or analyzed immediately. The medium used in all experiments was RPMI 1640 (Cellgro) supplemented with 10% fetal bovine serum (FBS) (Gemini Bio-Products), penicillin (50 U/ml; Cellgro), streptomycin (50 μg/ml; Cellgro), sodium pyruvate (1 mM; Cellgro), and glutamine (2 mM; Cellgro). Freezing medium consisted of 50% supplemented RPMI 1640 medium, 40% FBS, and 10% dimethyl sulfoxide.
Synthesis of Mycobacterium peptides.
The ESAT-6 peptide, NNALQNLARTISEANTIGENQAMAS, and KatG peptide, WTNTPTKWDNSFLEI, were synthesized as described previously (37). Each peptide was synthesized by solid-phase Fmoc (9-fluorenylmethoxy carbonyl) chemistry (Genemed Synthesis, San Diego, CA) to a purity of >70%. Identity was confirmed by mass spectroscopy, and purity was assessed by high-performance liquid chromatography.
Synthesis of Propionibacterium acnes supernatant.
One milligram of Propionibacterium acnes dried culture (ATCC 6919) was transferred to a UV-sterilized Eppendorf tube. Six hundred microliters of 1× phosphate-buffered saline (PBS) was added to the vial and reconstituted. The solution was boiled in water at 100°C for 10 min and then centrifuged at 14,000 rpm for 10 min. The supernatant, at a concentration of 20 μg/ml, was used to stimulate sarcoidosis patient and control BAL fluid cells.
Flow cytometry analysis: cytokine and proliferation assays.
Intracellular staining was performed in order to identify interleukin-2 (IL-2) and gamma interferon (IFN-γ)-secreting T cells in response to microbial stimulation. For the intracellular cytokine assay, 1 × 105 to 2 × 105 BAL fluid cells were incubated in supplemented RPMI 1640 medium with or without antigen (ESAT-6 or KatG peptide; 20 μg/ml) or staphylococcal enterotoxin B (SEB) (10 μg/ml; Sigma) as a positive control and anti-CD28 and anti-CD49d antibodies (1 μg/ml each; BD Biosciences) at 37°C under 5% CO2 for 1 h before the addition of BD GolgiStop (BD Biosciences). In addition, to assess nonspecific recognition, neoantigen keyhole limpet hemocyanin (KLH) (10 μg/ml; Calbiochem) was included as an additional negative control. For BAL fluid samples with enough cells, BAL fluid cells were first incubated at room temperature for 30 min with a monoclonal anti-Toll-like receptor 2 (anti-TLR2) antibody (10 μg/ml of the blocking antibody) (clone TLR2.1; eBiosciences) or the corresponding isotype control [mouse immunoglobulin G2a(κ)] prior to antigen stimulation. Following a 13-h incubation at 37°C under 5% CO2, cells were washed and stained with the surface antibodies anti-CD3, anti-CD4, and anti-CD8 (BD Biosciences) at 4°C for 30 min. After cells were washed, fixed, and permeabilized by using the Cytofix/Cytoperm kit according to the manufacturer's instructions (BD Biosciences), anti-IFN-γ and anti-IL-2 (BD Biosciences) were added at 4°C for 45 min. Cells were washed and analyzed via flow cytometry. The IFN-γ and IL-2 frequencies were defined as the subject's percentage of stimulated CD3+ CD4+ or CD3+ CD8+ T cells minus his or her unstimulated background frequency. Based upon previous studies, a response was considered positive when the frequency of recognition was at least twice background fluorescence and greater than 0.5% (5, 20, 28).
For the extracellular cytokine assay, 1 × 105 to 2 × 105 BAL fluid cells were incubated in supplemented RPMI 1640 medium with or without 10 μM peptide, SEB, or KLH and anti-CD28 and anti-CD49d antibodies (1 μg/ml each; BD Biosciences) at 37°C under 5% CO2 for 24 h. Supernatants were then collected and analyzed for extracellular cytokine by using a cytokine bead array according to the manufacturer's instructions (BD Biosciences).
To determine proliferation and quantitate cell division, purified BAL fluid cells were labeled with carboxyfluorescein succinimidyl ester (CFSE; Molecular Probes). Purified cells were first washed and resuspended in PBS. While the cells were subjected to a vortex, CFSE was added at a final concentration of 5 μM. The mixture was subjected to a vortex for an additional 15 s and incubated at 37°C for 3 min. Labeling was quenched by the addition of 50% FBS in PBS. Cells were washed once more with 50% serum in PBS, followed by two washes with supplemented RPMI 1640 medium. CFSE-labeled BAL fluid cells were stimulated in supplemented RPMI 1640 medium with or without 10 μM peptide or SEB as a positive control.
Data for all flow cytometry experiments were acquired with a FACSCalibur or LSR-II flow cytometer (BD Biosciences). Live cells were gated based on forward- and side-scatter properties, and analysis was performed using FlowJo software (Tree Star). A minimum of 30,000 events were acquired per sample.
Statistical analysis.
Statistical analyses were performed using the statistical programming language R (version 2.7.1). Of primary interest was an assessment of specific antigens and their potential role in the observed Th1 immunophenotype found in the pathogenesis of sarcoidosis. To this end, differences in the distributions of immune recognition of mycobacterial antigen by CD4+ and CD8+ T cells from BAL fluid were tested across diagnosis groups by using the Wilcoxon rank sum test at an α level of 0.05. In addition, it is unclear whether each radiographic stage of sarcoidosis reflects a different etiology or a distinct immune response to the same antigen. Therefore, differences in the distributions of immune recognition in sarcoidosis patients across the four radiographic stages were assessed using the Kruskal-Wallis rank sum test. Differences were considered significant at a P value of <0.05.
RESULTS
CD4+ Th1 immune responses in the BAL fluid of sarcoidosis patients exhibit specific recognition.
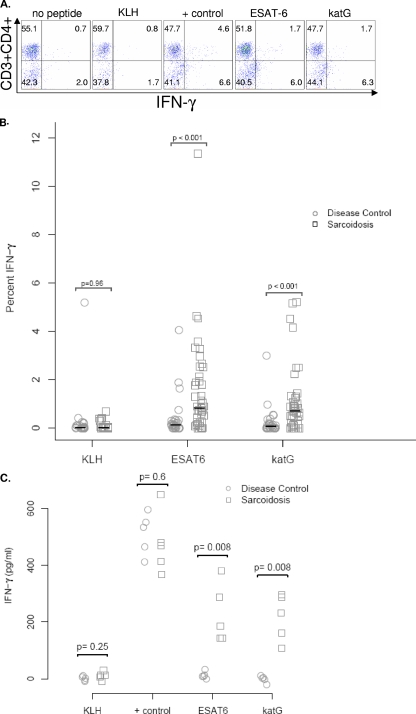
Thirty-two of the 44 sarcoidosis patient BAL fluid samples displayed a CD4+ IFN-γ response to ESAT-6 or KatG, compared to 1 of the 27 controls (P < 0.0001; Fisher's exact test) (Table 1 and Fig. 1A; see Table S1 in the supplemental material). In some subjects, 3 to 5% of BAL fluid CD4+ T cells recognized mycobacterial antigen (Fig. 1B). In addition, eight controls and three sarcoidosis subjects exhibited strong responses to antigenic stimulation. However, this corresponded with high background; therefore, the responses were not positive as defined by the predetermined criteria of at least twice background fluorescence and greater than 0.5% recognition. For example, disease control 7 displayed a CD4+ IFN-γ response to ESAT-6 of 12.18%, and the corresponding background was 10.55%. To confirm that the high-background responders were not skewing the results, we reanalyzed the data with these subjects removed. The statistical significance was unchanged (data not shown). In order to assess nonspecific recognition, neoantigen KLH was included as an additional negative control according to cell availability. Positive responses to ESAT-6 and KatG, but not to KLH, were observed in BAL fluid of sarcoidosis subjects (Fig. 1B). These frequencies were similar to those reported among smear-negative tuberculosis subjects with active disease (5, 28). Not only was there a significant difference in the percentages of subjects recognizing mycobacterial antigen but the distribution of the T-cell responses to these antigens among the sarcoidosis subjects was distinct from that for the disease controls (Fig. 1B). We investigated the peripheral Th1 response to mycobacterial antigens in matched PBMC from five sarcoidosis subjects at the time of diagnosis. While PBMC exhibited appropriate responses to SEB, there was a lack of response to mycobacterial antigens among four of the five subjects, despite positive responses in BAL fluid cells (data not shown). There also was no recognition of mycobacterial antigens in control PBMC. We also assessed extracellular cytokine production from BAL cells in five sarcoidosis and five control subjects. Analogous to the intracellular cytokine assays, there was extracellular production of IFN-γ and IL-2 among the sarcoidosis subjects but not among the disease controls (Fig. 1C).
FIG. 1.
Sarcoidosis patient BAL fluid demonstrates CD4+ Th1 immune responses to mycobacterial virulence factors. Intracellular cytokine staining for IFN-γ was performed on BAL fluid cells from sarcoidosis subjects and disease controls after stimulation with neoantigen (KLH), ESAT-6, and KatG peptides and either SEB (+ control). (A) Shown are representative flow cytometry dot plots indicating percentages of CD3+ CD4+ T-cell responses to mycobacterial antigen from sarcoidosis subject 13, who displayed high-level recognition of both ESAT-6 and KatG peptides. Despite a lack of recognition of KLH, both mycobacterial peptides were recognized by sarcoidosis patient CD3+ CD4+ T cells producing IFN-γ. (B) Percentages of CD3+ CD4+ T cells that produced IFN-γ in response to KLH, ESAT-6, or KatG stimulation, with a no-peptide control subtracted out, for all 44 sarcoidosis subjects and 27 disease controls. Differences in the distributions of immune recognition of mycobacterial antigen by BAL fluid CD3+ CD4+ T cells were noted between sarcoidosis patients and disease controls by using the Wilcoxon rank sum test. Medians are depicted by horizontal lines. Stimulation of BAL fluid cells with SEB resulted in 2% to 15% of CD4+ T cells producing IFN-γ for sarcoidosis subjects and disease controls (P = 0.15; data not shown). Eight controls and three sarcoidosis subjects exhibited strong responses to antigenic stimulation; however, this corresponded with high background, and therefore the responses were not positive as defined by predetermined criteria. (C) A significant difference in extracellular Th1 cytokine production levels in response to mycobacterial antigens was also noted between sarcoidosis and controls subjects.
A prior study noted that environmental mycobacteria home to established granulomas (11). There was a significant difference in recognition of mycobacterial antigens among sarcoidosis subjects compared to that among controls with granulomatous diseases (32/44 compared to 1/10; P value of 0.001 by two-tailed Fisher test) (see Table S1 in the supplemental material). These findings demonstrate that cytokine responses to mycobacterial antigens are present in a site of active sarcoidosis involvement but notably absent from BAL fluid of other lung diseases, including infectious and noninfectious granulomatous diseases.
CD8+ T cells from sarcoidosis patient BAL fluid recognize mycobacterial antigen.
Flow cytometry revealed that immune responses of CD3+ CD4− T cells were also present in sarcoidosis patient BAL fluid. There is mounting evidence that CD8+ T cells play a protective role in the host response to pathogenic mycobacteria (7, 8, 19, 23, 46). To determine if mycobacterial antigens elicit a CD8+ T-cell immune response in sarcoidosis or control subjects, BAL fluid cells were stimulated with ESAT-6 and KatG peptides, and then the CD8+ T cells were analyzed for intracellular cytokine production of IL-2 and IFN-γ by flow cytometry. For three of the sarcoidosis subjects and one control subject, the CD8 cell count was too low to determine cytokine production. Among the remaining subjects, there was lack of significant immune responses to KLH; however, strong CD8+ T-cell responses to ESAT-6 and KatG were observed (Fig. 2A). Indeed, 25 of the 41 sarcoidosis subjects exhibited CD8+ IFN-γ responses compared to 1 of the 26 control BAL fluid samples (P value of <0.0001 by Fisher's exact test). Not only was there a significant difference in the percentages of sarcoidosis subjects recognizing ESAT-6 and KatG but a significant difference in the distributions of the T-cell responses was also observed (Table 1 and Fig. 2B; see Table S1 in the supplemental material). Moreover, several subjects displayed 3 to 12% CD8+ IFN-γ responses to mycobacterial antigen (Fig. 2B; see Table S1 in the supplemental material). Six controls and two sarcoidosis subjects exhibited strong CD8+ responses to antigenic stimulation, similar to the case for CD4+ immune responses. For example, disease control 19 displayed a CD8+ IFN-γ response to ESAT-6 of 15.48%, and the corresponding background was 12.32%. Therefore, the response was not positive as defined by the predetermined criteria of at least twice background fluorescence and recognition greater than 0.5%. Similar to the case for the CD4 immune response data, we reanalyzed the CD8 immune response data with the high-background subjects removed to confirm that these subjects were not skewing the results. The statistical significance was unchanged (data not shown).
FIG. 2.
Sarcoidosis patient BAL fluid CD8+ T cells display antigen-specific Th1 immune responses to mycobacterial antigen. Intracellular cytokine staining for IFN-γ was performed on BAL fluid cells from sarcoidosis subjects and disease controls after stimulation with no peptide, neoantigen (KLH), ESAT-6, and KatG peptides and either SEB or phytohemagglutinin (+ control). Both mycobacterial peptides were recognized by sarcoidosis patient CD3+ CD8+ T cells, as evidenced by the production of IFN-γ. (A) Shown is a representative flow cytometry analysis for a sarcoidosis subject who displayed significant CD3+ CD8+ T-cell IFN-γ responses to mycobacterial antigen (sarcoidosis patient 32). (B) Percentages of CD3+ CD8+ T cells that produced IFN-γ in response to KLH, ESAT-6, or KatG stimulation, with a no-peptide control subtracted out, for sarcoidosis subjects and disease controls. Differences in the distributions of immune recognition of mycobacterial antigen by BAL fluid CD3+ CD8+ T cells were noted between the sarcoidosis and control subjects by using the Wilcoxon rank sum test. Medians are depicted by horizontal lines. Stimulation of BAL cells with SEB resulted in 2% to 15% of CD3+ CD8+ T cells producing IFN-γ for sarcoidosis subjects and disease controls (P = 0.49; data not shown). Six controls and two sarcoidosis subjects exhibited strong responses to antigenic stimulation; however, this corresponded with high background, and therefore the responses were not positive as defined by predetermined criteria.
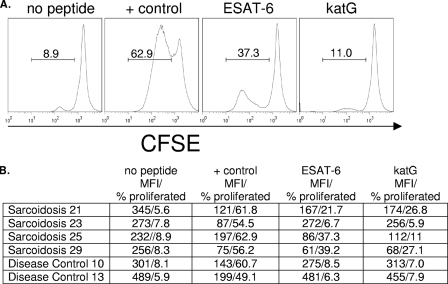
Sarcoidosis patient BAL fluid cells proliferate in response to mycobacterial antigen.
Antigen recognition by T cells initiates cytokine production and proliferation. However, in chronic inflammatory states, nonspecific recognition can induce cytokine production. Although the lack of recognition of KLH and the detection of immune responses to mycobacterial antigens suggested that the recognition observed was not secondary to nonspecific proliferation, we tested the ability of the cells to proliferate in response to ESAT-6 and KatG peptides. BAL fluid cells were labeled with CFSE, a fluorescent dye used to monitor the number of cell divisions, and then stimulated with ESAT-6 and KatG peptides. Activation with mycobacterial antigen resulted in proliferation of the CD4+ T cells. The proliferation correlated with the cytokine data. In sarcoidosis patient 25, activation with ESAT-6 resulted in moderate proliferation of the CD4+ T cells compared to those of the positive and negative controls, while KatG elicited low-level proliferation (Fig. 3A). This lack of proliferation to KatG peptide was consistent with the lack of immune recognition of KatG observed in sarcoidosis patient 25. The mean fluorescence intensities and percentages of proliferating CD4+ T cells for the four sarcoidosis subjects and two disease controls are listed in Fig. 3B.
FIG. 3.
Sarcoidosis patient BAL fluid CD4+ T cells demonstrate antigen-specific proliferation in response to mycobacterial antigens. (A) Sarcoidosis patient BAL fluid cells from sarcoidosis subject 25 were CFSE labeled and activated with SEB (10 μg/ml), ESAT-6 peptide, and KatG peptide. Day 4 postactivation, antigen-specific proliferation of CD4+ cells was assessed by gating on CD3+ CD4+ T cells and analyzing the CFSE expression of this subset by flow cytometry. Percent proliferation is indicated above the scale bars. These results were reproducible for all three of the other sarcoidosis subjects tested. In sarcoidosis subject 25, antigen-specific responses to ESAT-6 were observed, but there were none to KatG. There was no recognition of KatG by flow cytometry. (B) The mean fluorescence intensities (MFI) of proliferating cells and percentages of proliferating CD4+ T cells for the four sarcoidosis subjects and two disease controls tested.
Propionibacterium acnes is also postulated to have a role in sarcoidosis pathogenesis (27). Due to limitations in cell availability, we were not able to test each sarcoidosis patient and control specimen. We were able to assess recognition of P. acnes among five sarcoidosis patient samples (from sarcoidosis patients 33 to 37) and five control samples (from disease controls 22, 23, 24, 25, and 26) by intracellular cytokine production analysis. There was no recognition among any of the sarcoidosis subjects, and there was recognition by only one of the control specimens (disease control 25). Two of these five sarcoidosis subjects (sarcoidosis patients 35 and 37) had responses to mycobacterial antigens. Three sarcoidosis samples were negative for immune responses to mycobacterial or propionibacterial antigens. These results, combined with the lack of recognition of KLH (Fig. 1 and 2), provide compelling evidence of specific recognition of mycobacterial antigen at an active site of sarcoidosis involvement.
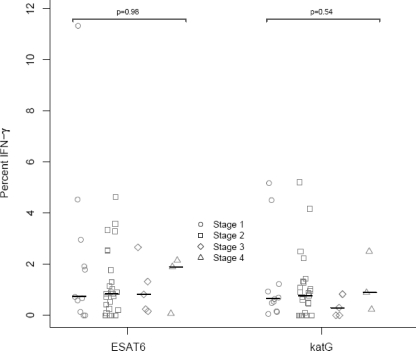
CD4+ immune responses observed at all radiographic stages of sarcoidosis.
When a sarcoidosis patient is being evaluated, a chest radiograph can be used to describe the disease stage upon presentation. An alternate explanation of the disease is that each radiographic stage of sarcoidosis reflects a different etiology. It is also possible that each stage represents a distinct immune response to the same microbial antigen, analogous to what is observed in the varied presentations of Histoplasma capsulatum disease.
We evaluated the immune responses to ESAT-6 and KatG in terms of radiographic stages and found evidence of recognition in 50 to 75% of subjects from each stage (Fig. 4). There was no significant difference in the degrees or percentages of sarcoidosis subjects recognizing these mycobacterial antigens. These findings suggest that regardless of radiographic stage, sarcoidosis subjects have had exposure to mycobacterial antigens at some point.
FIG. 4.
Sarcoidosis patient immune responses to mycobacterial antigen were present in all radiographic stages. CD3+ CD4+ T-cell responses to mycobacterial antigens were present in 50 to 75% of all sarcoidosis subjects, despite differences in radiographic staging. Medians are depicted by horizontal lines. Differences in the distributions of immune recognition in sarcoidosis patients across the four radiographic stages were assessed using the Kruskal-Wallis rank sum test. There was no significant difference in the strengths of responses between stages.
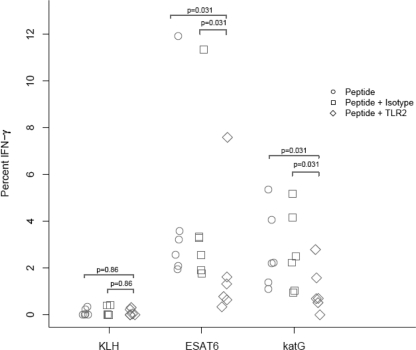
TLR2 inhibition reduces the immune response in sarcoidosis.
TLR2, TLR4, and TLR9 play an important role in the immune response to mycobacterial infections (31, 48). Recent evidence of direct interactions between mycobacterial ESAT-6 and TLR2 has been reported (36). Treatment of sarcoidosis patient BAL fluid cells with monoclonal antibody against TLR2 resulted in a significant reduction in immune responses against ESAT-6 and KatG (Fig. 5). Treatment with an isotype control antibody did not inhibit the immune response (Fig. 5).
FIG. 5.
TLR2 inhibition reduces the sarcoidosis patient immune response. Sarcoidosis patient BAL fluid was incubated with anti-TLR2 or isotype control for 30 min and then stimulated with KLH, ESAT-6, KatG, or SEB for 14 h. Intracellular cytokine staining for IFN-γ was then performed. Shown are the percentages of CD3+ CD4+ T cells that produced IFN-γ in response to KLH, ESAT-6, or KatG stimulation, with a no-peptide control subtracted out, for six sarcoidosis subjects. Inhibition by anti-TLR2 suggests that TLR2 signaling is required for the sarcoidosis patient immune response. Medians are depicted by horizontal lines. The pairwise Wilcoxon rank sum test was used to analyze the data set. The lower-bracket value is for the comparison between the isotype and anti-TLR2 conditions. The upper-bracket value is for the comparison between peptide stimulation alone and anti-TLR2 conditions.
DISCUSSION
This study demonstrates that mycobacterial antigens induce a T-cell-specific response in the BAL fluid cells of sarcoidosis patients. The presence of these responses at the time of diagnosis is supportive of prior exposure to mycobacteria, and the confinement of responses to the lung at the time of diagnosis is congruent with prior epidemiologic studies suggesting that exposure to bioaerosols is a risk factor for the disease. These results are supported by a recent report showing responses to KatG whole protein in sarcoidosis patient BAL fluid from two research center study cohorts (10).
It has been reported that superinfecting environmental mycobacteria preferentially home to tuberculous granulomas (11). The significant absence of immune responses to mycobacterial virulence factors among granulomatous control subjects suggest that the immune responses detected in sarcoidosis subjects do not reflect superinfection but rather a role in pathogenesis. The presence of congruent recognition of two mycobacterial proteins, not just one, argues against the hypothesis that sarcoidosis is caused by retention of a single poorly cleared or poorly degraded antigen or protein (Fig. 1). The specificity of the responses is evidenced by the lack of responses among the seven subjects with hypersensitivity pneumonitis or MycobacteriumY avium infection. Furthermore, prior reports have identified the KatG protein by immunohistochemistry, mass spectrometry, and T-cell response assays with sarcoidosis subjects (9, 10, 13, 44). Moreover, a comparison of the KatG sequences of M. bovis, M. avium, M. smegmatis, and M. tuberculosis reveal a 99.9% identity in the 740-amino-acid overlap (GenBank accession no. NP_855594, NP_960602, YP_888029, and NP_216424, respectively). It has also been demonstrated that patients with pulmonary M. avium do not react to ESAT-6, although rare responses have been reported (1). Immune recognition of ESAT-6 has been reported in infections with other pathogenic mycobacteria, such as M. tuberculosis, M. marinum, and M. kansasii (2). The significant difference in responses to mycobacterial antigens among sarcoidosis patient and control specimens supports the concept that ESAT-6-specific immune responses are not due to contamination of laboratory reagents with environmental mycobacteria (Fig. 1B). A lone control specimen (disease control 25) had strong reactions to KLH, ESAT-6, KatG, and propionibacterial supernatant. These responses may reflect infection with a microorganism that secretes these proteins, contamination, or possibly nonspecific reactivity.
Prior reports have found an association between sarcoidosis and propionibacteria in sarcoidosis patient specimens (25). Although the assays were performed on limited numbers of sarcoidosis patient and control BAL fluid specimens, a preliminary investigation did not reveal immunologic evidence of P. acnes in the study participants. Molecular analysis for P. acnes was also performed and was negative for all five sarcoidosis patient specimens and four of the five control specimens tested (data not shown). Future studies will be performed to delineate the role of P. acnes in American sarcoidosis subjects.
Another interesting observation was the presence of immune responses to mycobacterial antigens in BAL fluid cells and not in circulating cells. This has been reported in M. tuberculosis infection also (6, 40). A recent study of tuberculosis patients found heterogeneity in recognition of mycobacterial antigens by BAL fluid cells (40). In addition, the peripheral blood response to antigens did not always match the responses observed at the active site. In tuberculosis patients, the observed response to purified protein derivative of M. tuberculosis in the lung was 100-fold greater than that in blood (4). In prior reports, we demonstrated peripheral blood responses to mycobacterial antigens (9, 13). However, in these studies, the majority of the sarcoidosis subjects had been diagnosed for a year or longer, while in this study, we evaluated sarcoidosis subjects at the time of diagnosis. These data suggest that the immune response may be mainly localized to the site of active granulomatous inflammation.
The detection of CD8+ T-cell responses in sarcoidosis patient BAL fluid suggests important immunologic and genetic implications. The role of CD8+ T cells in sarcoidosis has not been well studied. It has been shown that CD8+ T cells secrete IFN-γ and tumor necrosis factor alpha in response to M. tuberculosis antigen in M. tuberculosis infection (18, 24, 43). There is mounting evidence that CD8+ T cells play a protective role in the host response to pathogenic mycobacteria (7, 8, 10, 19, 23, 46). Moreover, CD8+ T cells can kill infected cells via a granule-dependent mechanism involving perforin and granulysin, which also possess direct antimicrobial activities (45). Therefore, CD8+ T cells may play a crucial role in the sarcoidosis clinical outcomes.
We are also interested in innate and adaptive signaling mechanisms important in the sarcoidosis patient immune response against microbial antigens. As cited earlier, direct interaction of mycobacterial ESAT-6 with TLR2 has been reported. It has also been demonstrated that TLR2 is recruited to the phagosomes of macrophages, thus allowing them to promptly respond to the invading pathogens (47). A recent report suggests that ESAT-6 of M. tuberculosis inhibits TLR2 signaling in macrophages (36). While we were limited by cell availability, preliminary evidence suggests that inhibition of TLR2 signaling results in a reduced immune response. These preliminary results suggest that TLR2 signaling plays a role in the sarcoidosis patient immune response against ESAT-6. Due to limitations in the availability of BAL fluid cells, we were not able to investigate the role of other TLRs in this study. However, a more in-depth investigation including the role of other TLRs, such as TLR4 and TLR9, is warranted.
In conclusion, these findings demonstrate specific recognition of mycobacterial virulence factors at the time of diagnosis. It adds additional support to an association between mycobacteria and sarcoidosis but does not show causality. It remains feasible that the relationship of mycobacteria to sarcoidosis may represent an abnormal host response to nonviable organisms. Additional studies are also required to delineate the role of TLR2 signaling in the sarcoidosis patient immune response. An investigation to determine if pulmonary and extrapulmonary sarcoidosis involvements reflect the same pathogenesis is warranted. The current study cannot address extrapulmonary sarcoidosis involvement. Further investigation into the role of mycobacteria as an etiologic contributor to sarcoidosis pathogenesis is warranted.
Supplementary Material
Acknowledgments
This work was supported by National Institutes of Health grants (RO1-HL83839, RO1-AI65744, MO1 RR-00095 to W.P.D., and T32 HL069765 to K.A.O.-R.).
We thank Laura Kasman for the mailing of patient samples and critical reading of the manuscript. We thank Doug Kernodle and the Vanderbilt Editors' Club for critical reading of the manuscript. We thank Heidi Grund for her assistance with data collection and coordination.
Editor: J. L. Flynn
Footnotes
Published ahead of print on 13 July 2009.
Supplemental material for this article may be found at http://iai.asm.org/.
REFERENCES
- 1.Adams, L. V., R. D. Waddell, and C. F. Von Reyn. 2008. T-SPOT.TB Test(R) results in adults with Mycobacterium avium complex pulmonary disease. Scand. J. Infect. Dis. 40196-203. [DOI] [PubMed] [Google Scholar]
- 2.Arend, S. M., K. E. van Meijgaarden, K. de Boer, E. C. de Palou, D. van Soolingen, T. H. Ottenhoff, and J. T. van Dissel. 2002. Tuberculin skin testing and in vitro T cell responses to ESAT-6 and culture filtrate protein 10 after infection with Mycobacterium marinum or M. kansasii. J. Infect. Dis. 1861797-1807. [DOI] [PubMed] [Google Scholar]
- 3.Barnard, J., C. Rose, L. Newman, M. Canner, J. Martyny, C. McCammon, E. Bresnitz, M. Rossman, B. Thompson, B. Rybicki, S. E. Weinberger, D. R. Moller, G. McLennan, G. Hunninghake, L. DePalo, R. P. Baughman, M. C. Iannuzzi, M. A. Judson, G. L. Knatterud, A. S. Teirstein, H. Yeager, Jr., C. J. Johns, D. L. Rabin, and R. Cherniack. 2005. Job and industry classifications associated with sarcoidosis in A Case-Control Etiologic Study of Sarcoidosis (ACCESS). J. Occup. Environ. Med. 47226-234. [DOI] [PubMed] [Google Scholar]
- 4.Barry, S. M., M. C. Lipman, B. Bannister, M. A. Johnson, and G. Janossy. 2003. Purified protein derivative-activated type 1 cytokine-producing CD4+ T lymphocytes in the lung: a characteristic feature of active pulmonary and nonpulmonary tuberculosis. J. Infect. Dis. 187243-250. [DOI] [PubMed] [Google Scholar]
- 5.Breen, R. A., G. A. Hardy, F. M. Perrin, S. Lear, S. Kinloch, C. J. Smith, I. Cropley, G. Janossy, and M. C. Lipman. 2007. Rapid diagnosis of smear-negative tuberculosis using immunology and microbiology with induced sputum in HIV-infected and uninfected individuals. PLoS ONE 2e1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breen, R. A., G. Janossy, S. M. Barry, I. Cropley, M. A. Johnson, and M. C. Lipman. 2006. Detection of mycobacterial antigen responses in lung but not blood in HIV-tuberculosis co-infected subjects. AIDS 201330-1332. [DOI] [PubMed] [Google Scholar]
- 7.Brookes, R. H., A. A. Pathan, H. McShane, M. Hensmann, D. A. Price, and A. V. Hill. 2003. CD8+ T cell-mediated suppression of intracellular Mycobacterium tuberculosis growth in activated human macrophages. Eur. J. Immunol. 333293-3302. [DOI] [PubMed] [Google Scholar]
- 8.Canaday, D. H., R. J. Wilkinson, Q. Li, C. V. Harding, R. F. Silver, and W. H. Boom. 2001. CD4(+) and CD8(+) T cells kill intracellular Mycobacterium tuberculosis by a perforin and Fas/Fas ligand-independent mechanism. J. Immunol. 1672734-2742. [DOI] [PubMed] [Google Scholar]
- 9.Carlisle, J., W. Evans, R. Hajizadeh, M. Nadaf, B. Shepherd, R. D. Ott, K. Richter, and W. Drake. 2007. Multiple Mycobacterium antigens induce interferon-gamma production from sarcoidosis peripheral blood mononuclear cells. Clin. Exp. Immunol. 150460-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen, E. S., J. Wahlstrom, Z. Song, M. H. Willett, M. Wiken, R. C. Yung, E. E. West, J. F. McDyer, Y. Zhang, A. Eklund, J. Grunewald, and D. R. Moller. 2008. T cell responses to mycobacterial catalase-peroxidase profile a pathogenic antigen in systemic sarcoidosis. J. Immunol. 1818784-8796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cosma, C. L., O. Humbert, and L. Ramakrishnan. 2004. Superinfecting mycobacteria home to established tuberculous granulomas. Nat. Immunol. 5828-835. [DOI] [PubMed] [Google Scholar]
- 12.Demirkok, S. S., M. Basaranoglu, E. Coker, and T. Karayel. 2007. Seasonality of the onset of symptoms, tuberculin test anergy and Kveim positive reaction in a large cohort of patients with sarcoidosis. Respirology 12591-593. [DOI] [PubMed] [Google Scholar]
- 13.Drake, W. P., M. S. Dhason, M. Nadaf, B. E. Shepherd, S. Vadivelu, R. Hajizadeh, L. S. Newman, and S. A. Kalams. 2007. Cellular recognition of Mycobacterium tuberculosis ESAT-6 and KatG peptides in systemic sarcoidosis. Infect. Immun. 75527-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drake, W. P., and L. S. Newman. 2006. Mycobacterial antigens may be important in sarcoidosis pathogenesis. Curr. Opin. Pulm. Med. 12359-363. [DOI] [PubMed] [Google Scholar]
- 15.Drake, W. P., Z. Pei, D. T. Pride, R. D. Collins, T. L. Cover, and M. J. Blaser. 2002. Molecular analysis of sarcoidosis tissues for mycobacterium species DNA. Emerg. Infect. Dis. 81334-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubaniewicz, A., M. Dubaniewicz-Wybieralska, A. Sternau, Z. Zwolska, E. Izycka-Swieszewska, E. Augustynowicz-Kopec, J. Skokowski, M. Singh, and L. Zimnoch. 2006. Mycobacterium tuberculosis complex and mycobacterial heat shock proteins in lymph node tissue from patients with pulmonary sarcoidosis. J. Clin. Microbiol. 443448-3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubaniewicz, A., P. Trzonkowski, M. Dubaniewicz-Wybieralska, A. Dubaniewicz, M. Singh, and A. Mysliwski. 2007. Mycobacterial heat shock protein-induced blood T lymphocytes subsets and cytokine pattern: comparison of sarcoidosis with tuberculosis and healthy controls. Respirology 12346-354. [DOI] [PubMed] [Google Scholar]
- 18.Flynn, J. L., and J. Chan. 2001. Immunology of tuberculosis. Annu. Rev. Immunol. 1993-129. [DOI] [PubMed] [Google Scholar]
- 19.Flynn, J. L., M. M. Goldstein, K. J. Triebold, B. Koller, and B. R. Bloom. 1992. Major histocompatibility complex class I-restricted T cells are required for resistance to Mycobacterium tuberculosis infection. Proc. Natl. Acad. Sci. USA 8912013-12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuhrmann, S., M. Streitz, and F. Kern. 2008. How flow cytometry is changing the study of TB immunology and clinical diagnosis. Cytometry A 731100-1106. [DOI] [PubMed] [Google Scholar]
- 21.Grunewald, J., J. Wahlstrom, M. Berlin, H. Wigzell, A. Eklund, and O. Olerup. 2002. Lung restricted T cell receptor AV2S3+ CD4+ T cell expansions in sarcoidosis patients with a shared HLA-DRbeta chain conformation. Thorax 57348-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hajizadeh, R., H. Sato, J. Carlisle, M. T. Nadaf, W. Evans, B. E. Shepherd, R. F. Miller, S. A. Kalams, and W. P. Drake. 2007. Mycobacterium tuberculosis antigen 85A induces Th-1 immune responses in systemic sarcoidosis. J. Clin. Immunol. 27445-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harty, J. T., A. R. Tvinnereim, and D. W. White. 2000. CD8+ T cell effector mechanisms in resistance to infection. Annu. Rev. Immunol. 18275-308. [DOI] [PubMed] [Google Scholar]
- 24.Henderson, R. A., S. C. Watkins, and J. L. Flynn. 1997. Activation of human dendritic cells following infection with Mycobacterium tuberculosis. J. Immunol. 159635-643. [PubMed] [Google Scholar]
- 25.Hiramatsu, J., M. Kataoka, Y. Nakata, K. Okazaki, S. Tada, M. Tanimoto, and Y. Eishi. 2003. Propionibacterium acnes DNA detected in bronchoalveolar lavage cells from patients with sarcoidosis. Sarcoidosis Vasc. Diffuse Lung Dis. 20197-203. [PubMed] [Google Scholar]
- 26.Iannuzzi, M. C., B. A. Rybicki, and A. S. Teirstein. 2007. Sarcoidosis. N. Engl. J. Med. 3572153-2165. [DOI] [PubMed] [Google Scholar]
- 27.Ishige, I., Y. Usui, T. Takemura, and Y. Eishi. 1999. Quantitative PCR of mycobacterial and propionibacterial DNA in lymph nodes of Japanese patients with sarcoidosis. Lancet 354120-123. [DOI] [PubMed] [Google Scholar]
- 28.Jafari, C., M. Ernst, B. Kalsdorf, U. Greinert, R. Diel, D. Kirsten, K. Marienfeld, A. Lalvani, and C. Lange. 2006. Rapid diagnosis of smear-negative tuberculosis by bronchoalveolar lavage enzyme-linked immunospot. Am. J. Respir. Crit. Care Med. 1741048-1054. [DOI] [PubMed] [Google Scholar]
- 29.Kajdasz, D. K., M. A. Judson, L. C. Mohr, Jr., and D. T. Lackland. 1999. Geographic variation in sarcoidosis in South Carolina: its relation to socioeconomic status and health care indicators. Am. J. Epidemiol. 150271-278. [DOI] [PubMed] [Google Scholar]
- 30.Kern, D. G., M. A. Neill, D. S. Wrenn, and J. C. Varone. 1993. Investigation of a unique time-space cluster of sarcoidosis in firefighters. Am. Rev. Respir. Dis. 148974-980. [DOI] [PubMed] [Google Scholar]
- 31.Krutzik, S. R., M. T. Ochoa, P. A. Sieling, S. Uematsu, Y. W. Ng, A. Legaspi, P. T. Liu, S. T. Cole, P. J. Godowski, Y. Maeda, E. N. Sarno, M. V. Norgard, P. J. Brennan, S. Akira, T. H. Rea, and R. L. Modlin. 2003. Activation and regulation of Toll-like receptors 2 and 1 in human leprosy. Nat. Med. 9525-532. [DOI] [PubMed] [Google Scholar]
- 32.Kucera, G. P., B. A. Rybicki, K. L. Kirkey, S. W. Coon, M. L. Major, M. J. Maliarik, and M. C. Iannuzzi. 2003. Occupational risk factors for sarcoidosis in African-American siblings. Chest 1231527-1535. [DOI] [PubMed] [Google Scholar]
- 33.Moller, D. R., and E. S. Chen. 2002. Genetic basis of remitting sarcoidosis: triumph of the trimolecular complex? Am. J. Respir. Cell Mol. Biol. 27391-395. [DOI] [PubMed] [Google Scholar]
- 34.Morimoto, T., A. Azuma, S. Abe, J. Usuki, S. Kudoh, K. Sugisaki, M. Oritsu, and T. Nukiwa. 2008. Epidemiology of sarcoidosis in Japan. Eur. Respir. J. 31372-379. [DOI] [PubMed] [Google Scholar]
- 35.Newman, L. S., C. S. Rose, E. A. Bresnitz, M. D. Rossman, J. Barnard, M. Frederick, M. L. Terrin, S. E. Weinberger, D. R. Moller, G. McLennan, G. Hunninghake, L. DePalo, R. P. Baughman, M. C. Iannuzzi, M. A. Judson, G. L. Knatterud, B. W. Thompson, A. S. Teirstein, H. Yeager, Jr., C. J. Johns, D. L. Rabin, B. A. Rybicki, and R. Cherniack. 2004. A case control etiologic study of sarcoidosis: environmental and occupational risk factors. Am. J. Respir. Crit. Care Med. 1701324-1330. [DOI] [PubMed] [Google Scholar]
- 36.Pathak, S. K., S. Basu, K. K. Basu, A. Banerjee, S. Pathak, A. Bhattacharyya, T. Kaisho, M. Kundu, and J. Basu. 2007. Direct extracellular interaction between the early secreted antigen ESAT-6 of Mycobacterium tuberculosis and TLR2 inhibits TLR signaling in macrophages. Nat. Immunol. 8610-618. [DOI] [PubMed] [Google Scholar]
- 37.Pathan, A. A., K. A. Wilkinson, P. Klenerman, H. McShane, R. N. Davidson, G. Pasvol, A. V. Hill, and A. Lalvani. 2001. Direct ex vivo analysis of antigen-specific IFN-gamma-secreting CD4 T cells in Mycobacterium tuberculosis-infected individuals: associations with clinical disease state and effect of treatment. J. Immunol. 1675217-5225. [DOI] [PubMed] [Google Scholar]
- 38.Prezant, D. J., A. Dhala, A. Goldstein, D. Janus, F. Ortiz, T. K. Aldrich, and K. J. Kelly. 1999. The incidence, prevalence, and severity of sarcoidosis in New York City firefighters. Chest 1161183-1193. [DOI] [PubMed] [Google Scholar]
- 39.Rybicki, B. A., K. L. Amend, M. J. Maliarik, and M. C. Iannuzzi. 2004. Photocopier exposure and risk of sarcoidosis in African-American sibs. Sarcoidosis Vasc. Diffuse Lung Dis. 2149-55. [DOI] [PubMed] [Google Scholar]
- 40.Sable, S. B., D. Goyal, I. Verma, D. Behera, and G. K. Khuller. 2007. Lung and blood mononuclear cell responses of tuberculosis patients to mycobacterial proteins. Eur. Respir. J. 29337-346. [DOI] [PubMed] [Google Scholar]
- 41.Scadding, J. G. 1961. Prognosis of intrathoracic sarcoidosis in England. A review of 136 cases after five years' observation. Br. Med. J. 21165-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Semenzato, G., M. Bortoli, and C. Agostini. 2002. Applied clinical immunology in sarcoidosis. Curr. Opin. Pulm. Med. 8441-444. [DOI] [PubMed] [Google Scholar]
- 43.Serbina, N. V., and J. L. Flynn. 1999. Early emergence of CD8+ T cells primed for production of type 1 cytokines in the lungs of Mycobacterium tuberculosis-infected mice. Infect. Immun. 673980-3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Song, Z., L. Marzilli, B. M. Greenlee, E. S. Chen, R. F. Silver, F. B. Askin, A. S. Teirstein, Y. Zhang, R. J. Cotter, and D. R. Moller. 2005. Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. J. Exp. Med. 201755-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stenger, S., D. A. Hanson, R. Teitelbaum, P. Dewan, K. R. Niazi, C. J. Froelich, T. Ganz, S. Thoma-Uszynski, A. Melian, C. Bogdan, S. A. Porcelli, B. R. Bloom, A. M. Krensky, and R. L. Modlin. 1998. An antimicrobial activity of cytolytic T cells mediated by granulysin. Science 282121-125. [DOI] [PubMed] [Google Scholar]
- 46.Sud, D., C. Bigbee, J. L. Flynn, and D. E. Kirschner. 2006. Contribution of CD8+ T cells to control of Mycobacterium tuberculosis infection. J. Immunol. 1764296-4314. [DOI] [PubMed] [Google Scholar]
- 47.Underhill, D. M., A. Ozinsky, A. M. Hajjar, A. Stevens, C. B. Wilson, M. Bassetti, and A. Aderem. 1999. The Toll-like receptor 2 is recruited to macrophage phagosomes and discriminates between pathogens. Nature 401811-815. [DOI] [PubMed] [Google Scholar]
- 48.Underhill, D. M., A. Ozinsky, K. D. Smith, and A. Aderem. 1999. Toll-like receptor-2 mediates mycobacteria-induced proinflammatory signaling in macrophages. Proc. Natl. Acad. Sci. USA 9614459-14463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wahlström, J., J. Dengjel, B. Persson, H. Duyar, H. G. Rammensee, S. Stevanovic, A. Eklund, R. Weissert, and J. Grunewald. 2007. Identification of HLA-DR-bound peptides presented by human bronchoalveolar lavage cells in sarcoidosis. J. Clin. Investig. 1173576-3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilsher, M. L. 1998. Seasonal clustering of sarcoidosis presenting with erythema nodosum. Eur. Respir. J. 121197-1199. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.