Abstract
A case of severe human cytomegalovirus esophagitis after short-term corticosteroid therapy in a patient with no other apparent cause of immunodeficiency, such as human immunodeficiency virus infection, neoplasia, or previous organ transplantation, is described herein. The cytomegalovirus esophagus infection was successfully treated with ganciclovir.
CASE REPORT
A 63-year-old male patient was taken to the hospital by the on-call emergency physician with the working hypothesis of an acute myocardial infarction—the patient had presented with massive chest pain. The patient reported that the pain was directly related to the intake of food and drink, resulting in a bolus feeling and a burning sensation similar to heartburn. The increasing discomfort had, during a course of approximately 6 weeks, caused a decreased food intake, resulting in a weight loss of about 14 kg, with even the intake of fluids becoming an increasing problem. In prior months, the patient had repeatedly presented at his general practitioner's office with severe dyspnea due to chronic obstructive pulmonary disease (COPD). For the COPD, he had earlier received short-term treatment with corticosteroids while being treated with antibiotics, although this was not known at the time of presentation. At the time of admission, the patient was hygienically unkempt and of a severely reduced status. Because the patient clinically showed signs of only chronic bronchitis, a myocardial infarction was ruled out. With the patient reporting increasing odynophagia (pain on swallowing) and the chest pain occurring most frequently after eating, a gastroscopy was performed, showing a massive ulcerous esophagitis with sprinkled whitish plaques. Biopsies from the ulcers and plaques were taken, and due to the lack of a better explanation, an oral treatment with amphotericin B was initiated for potential Candida esophagitis. The microbiological examination and histology findings of the biopsies ruled out a Candida infection, and the histology report suggested a herpes simplex virus (HSV) esophagitis, since no typical owl's eye appearance of cytomegalovirus (CMV)-infected cells was seen. Following these findings, the patient received intravenous acyclovir. After 7 days of treatment, gastroscopy showed no clear sings of healing, so biopsies were taken again, this time for real-time PCR testing for HSV, CMV, and Epstein-Barr virus (EBV). The PCR results were strongly positive for CMV DNA, weakly positive for EBV, and negative for HSV. Due to the PCR results, the treatment was consequently changed to ganciclovir via a central venous line. In the absence of clinical signs of EBV infection, the positive EBV PCR was interpreted as an incidental finding with no therapeutic consequences. The therapy was well tolerated with no adverse effects. The patient reported a continuous reduction of the odynophagia which corresponded with a much-improved gastroscopic finding obtained after 14 days of intravenous therapy (Fig. 1). The biopsies taken during this gastroscopy showed no more CMV DNA by PCR testing, and the patient was soon discharged in much better condition. Because of the unusual diagnosis, the patient was screened for any immunocompromising factor to explain the CMV infection. All tumor markers and imaging diagnostics were without significant findings, and human immunodeficiency virus and hepatitis C virus tests were negative (serology and PCR). Quite late during hospitalization—due to the family physician being on vacation for 2 weeks around the time of these curious findings—a careful case history revealed earlier short-term treatment with corticosteroids by the family physician for COPD which had been aggravated by ongoing tobacco smoking.
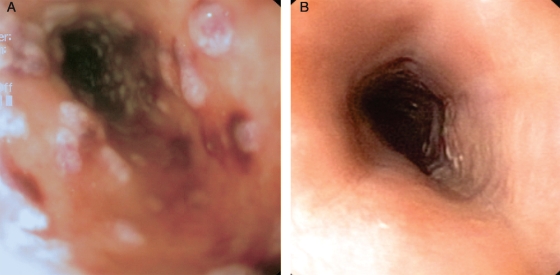
FIG. 1.
Endoscopy pictures of CMV-associated esophagitis before and after ganciclovir treatment. (A) Esophageal ulceration caused by CMV infection at multiple sites, as seen on endoscopy. (B) Follow-up endoscopic image after 14 days of intravenous ganciclovir therapy showing healed ulcers.
The spectrum of human illness caused by CMV is diverse, is mostly dependent on the host, and can affect almost all organs. CMV infections in immunocompromised patients, especially transplant recipients and those infected with human immunodeficiency virus, cause substantial morbidity and mortality. Infection in the immunocompetent host is generally asymptomatic or may present as a form of mononucleosis syndrome. However, occasionally primary CMV infection can lead to severe organ-specific complications with significant morbidity and mortality (4, 7). Infection of pregnant women, even if asymptomatic, is occasionally associated with the syndrome of congenital CMV infection in newborns. Secondary, symptomatic disease may present later in the life of the host, reflecting one of two possibilities, i.e., reactivation of latent CMV or reinfection with a novel exogenous strain. Reactivation of CMV may occur at any time during the life of the human host, though it is most common in the setting of systemic immunosuppression, either iatrogenic or secondary to underlying medical conditions, such as AIDS (6, 9). Patients with CMV esophagitis present with odynophagia or dysphagia, described as difficulty swallowing or a sense of obstruction—either substernal, epigastric, or in the throat. Liquids are often better tolerated than solids such as meat, which may worsen both odynophagia and dysphagia. Pain may be exacerbated by the ingestion of acidic liquids and by eructation. Ulcerative esophagitis is characterized primarily by odynophagia, which can be severe, at times to the point of limiting oral intake and resulting in weight loss and dehydration. Spontaneous substernal pain or burning may also occur intermittently, unrelated to swallowing. Fever accompanies esophagitis in 20% of patients with CMV infection, and 42% of patients present with nausea and vomiting. CMV esophagitis occurs most often in patients with AIDS or severe immunosuppression. Rare cases of immunocompetent hosts have been reported (1). Symptoms are indistinguishable from those associated with Candida or HSV esophagitis. The endoscopic appearance of CMV esophagitis usually is typified by large (sometimes >10 cm2), shallow, “punched-out” ulcers, either solitary or multiple, located in the middle or distal part of the esophagus (12). Histopathologic examination, immunohistochemical and direct fluorescence staining, and PCR techniques are the most reliable diagnostic methods. Coinfections of the esophagus are common in patients with CMV; concomitant candidiasis (73%) and HSV infection (12%) have been reported among these patients (3).
While manifestations of CMV infection in immunocompromised hosts have been reported extensively in the biomedical literature, those observed in immunocompetent patients have received comparatively little attention (8). Various considerations that may lead to underreporting of severe CMV infections should be taken into account (2). This may be due, at least in part, to the rather moderate accuracy of some routinely available diagnostic methods, such as serological tests. On the other hand, molecular diagnostic methods such as PCR, which is not universally available, appear to be more sensitive than serological or virus isolation tests, and they are also more rapid. Severe CMV infections in immunocompetent patients can affect almost every system. In our case, the described CMV esophagitis was highly related to the short-term treatment with corticosteroids by the family physician, a fact which was not reported when the patient presented at the emergency department of the hospital and which could not be clarified contemporarily. CMV infection of the gastrointestinal tract in immunocompetent patients (5) or as a result of corticosteroid therapy for COPD (11) has been described before. Although rare in immunocompetent patients, one should keep CMV in mind as an etiologic agent when dealing with esophagitis, even if the patient does not show the classical risk factors associated with CMV infection (10).
Acknowledgments
We thank the Robert Bosch Foundation for financial support.
Footnotes
Published ahead of print on 1 July 2009.
REFERENCES
- 1.Altman, C., P. Bedossa, E. Dussaix, and C. Buffet. 1995. Cytomegalovirus infection of esophagus in immunocompetent adult. Dig. Dis. Sci. 40606-608. [DOI] [PubMed] [Google Scholar]
- 2.Arend, S. A., and A. C. M. Kroes. 2003. Look and ye shall find…cytomegalovirus infection in immunocompetent patients. Clin. Infect. Dis. 371607-1608. [DOI] [PubMed] [Google Scholar]
- 3.Bonacini, M., T. Young, and L. Laine. 1991. The causes of esophageal symptoms in human immunodeficiency virus infection. A prospective study of 110 patients. Arch. Intern. Med. 1511567-1572. [PubMed] [Google Scholar]
- 4.Cohen, J. I., and G. R. Corey. 1985. Cytomegalovirus infection in the normal host. Medicine (Baltimore) 64100-114. [DOI] [PubMed] [Google Scholar]
- 5.Galiatsatos, P., I. Shrier, and E. Lamoureux. 2005. Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hosts. Dig. Dis. Sci. 50609-616. [DOI] [PubMed] [Google Scholar]
- 6.Gandhi, M. K., and R. Khanna. 2004. Human cytomegalovirus: clinical aspects, immune regulation, and emerging treatments. Lancet Infect. Dis. 4725-738. [DOI] [PubMed] [Google Scholar]
- 7.Horwitz, C. A., W. Henle, G. Henle, D. Snover, H. Rudnick, H. H. Balfour, M. H. Mazur, R. Watson, B. Schwartz, and N. Muller. 1986. Clinical and laboratory evaluation of cytomegalovirus-induced mononucleosis in previously healthy individuals. Report of 82 cases. Medicine (Baltimore) 65124-134. [DOI] [PubMed] [Google Scholar]
- 8.Rafailidis, P., E. G. Mourtzoukou, I. C. Varbobitis, and M. E. Falagas. 2008. Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic review. Virol. J. 547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soderberg-Naucler, C., K. N. Fish, and J. A. Nelson. 1997. Reactivation of latent human cytomegalovirus by allogeneic stimulation of blood cells from healthy donors. Cell 91119-126. [DOI] [PubMed] [Google Scholar]
- 10.Venkataramani, A., A. J. Schlueter, T. J. Spech, and E. Greenberg. 1994. Cytomegalovirus esophagitis in an immunocompetent host. Gastrointest. Endosc. 40392-393. [DOI] [PubMed] [Google Scholar]
- 11.Wiest, P. M., T. Flanigan, R. A. Salata, D. M. Shlaes, M. Katzman, and M. M. Lederman. 1989. Serious infectious complications of corticosteroid therapy for COPD. Chest 951180-1184. [DOI] [PubMed] [Google Scholar]
- 12.Wilcox, C. M., D. L. Diehl, J. P. Cello, W. Margaretten, and M. A. Jacobson. 1990. Cytomegalovirus esophagitis in patients with AIDS. A clinical, endoscopic, and pathologic correlation. Ann. Intern. Med. 113589-593. [DOI] [PubMed] [Google Scholar]