Abstract
We studied the propensity of primary ovarian cancer cells to oncolytic adenoviruses. Using gene expression profiling of cancer cells either resistant or susceptible to viral oncolysis, we discovered that the epithelial phenotype of ovarian cancer represents a barrier to infection by commonly used oncolytic adenoviruses targeted to CAR or CD46. Specifically, we found that these adenovirus receptors were trapped in tight junctions and not accessible for virus binding. Accessibility to viral receptors was critically linked to depolarization and the loss of tight and adherens junctions, both hallmarks of epithelial-to-mesenchymal transition (EMT). We showed that specific, so far little explored adenovirus serotypes (Ad3, 7, 11, and 14) that use receptor(s) other than CAR and CD46 were able to trigger EMT in epithelial ovarian cancer cells and cause efficient oncolysis. Our studies on ovarian cancer cultures and xenografts also revealed a number of interesting cancer cell biology features. Tumors in situ as well as tumor xenografts in mice mostly contained epithelial cells and cells that were in a hybrid stage where they expressed both epithelial and mesenchymal markers (E/M cells). These E/M cells are the only xenograft-derived cells that can be cultured, and with passaging undergo EMT and differentiate into mesenchymal cells. Our study provides a venue for improved virotherapy of cancer as well as new insights into cancer cell biology.
Introduction
Cancer derived from ovarian surface epithelium accounts for more than 90% of ovarian cancer. Generally, epithelial cells are characterized by polarized membranes and tight junctions (TJ) that seal the paracellular space. During progression towards metastatic disease, epithelial cancers undergo an epithelial-mesenchymal transition (EMT), a cellular trans-differentiation program where epithelial cells lose characteristic features such as tight and adherens junctions and gain properties of mesenchymal cells (1). EMT as well as a high mutation rate and epigenetic instability of cancer cells contributes to genetic and phenotype heterogeneity of tumor cells present in a given tumor (2). We hypothesized that the phenotypic plasticity of ovarian cancer cells results in different susceptibility of malignant cell subsets to anti-tumor agents. Specifically, we focused our studies on susceptibility of ovarian cancer cells to oncolytic adenoviruses (Ads), e.g. viruses that are capable of amplifying the input dose through replication in a tumor dependent fashion. For humans, 51 different Ad serotypes have been identified, and classified into 6 species (A–F). So far, all oncolytic Ads used clinically were based on species C serotype 5. Although oncolytic adenoviruses have proved safe in patients, they have fallen short of their expected therapeutic value as monotherapies (3). Species A, C, D, E, and F use the coxsackie-adenovirus receptor (CAR) as a cellular receptor, while species B Ads use other attachment receptors, including CD46 and a yet non-identified receptor/s which is referred to as receptor X (4). CD46 is upregulated on many tumor cell cultures and tumors in situ and consequently, vectors based on Ads that utilize CD46 (in particular Ad35) have been developed (5).
In this study we discovered that in patient tumors or xenografted tumors in situ, the majority of ovarian cancer cells have either an epithelial or epithelial/mesenchymal (E/M) hybrid phenotype. The epithelial phenotype of ovarian cancer represents a barrier to infection by commonly used oncolytic adenoviruses targeted to CAR or CD46. This resistance was due to polarized expression of viral receptors and concomitant blockage of virion access by upregulated tight and adherens junctions. We also found that ovarian cancer cells that undergo EMT become susceptible to infection with oncolytic Ads. Our findings imply that i) Future clinical trials with CAR- and CD46-utilizing oncolytic adenoviruses should focus on non-epithelial malignancies. ii) Controlled induction of EMT in epithelial ovarian cancer cells can sensitize them to viral oncolysis. In this context we demonstrate that a specific subspecies of human Ads that uses receptor(s) different from CAR and CD46 was efficient in killing epithelial ovarian cancer cells, mainly by forcing these cells into EMT.
Materials in Methods
Tumor cell culture
Tumor tissue from biopsies was digested with proteases and cells were cultured as described in “Supplementary Material” Xenografts were established by injecting cancer cells in matrigel into the mammary fat pad of CB17 SCID-beige mice.
Adenoviruses
The following Ad vectors have been described previously: Ad5/35.IR-E1A/TRAIL, Ad5.IR-E1A/TRAIL(6), Ad5/35Δ24.Ki.COX (7), Ad5-GFP, Ad5/35-GFP, Ad5/35-bGal (8). The wild-type Ads Ad3 (GB strain), Ad7p (Gomen stain), Ad11p (Slobitski strain), Ad14 (DeWit strain), and Ad35 (Holden strain) were all obtained from the ATCC. The Ads were propagated in 293 cells, CsCl purified, titered for genomes and pfu as described previously (8).
Antibodies and inhibitors
A complete list of all antibodies and inhibitors is provided in the Supplemental Materials. Ads or the Ad hexon antibody were labeled with Cy3 using the Cy3 bis-Reactive Dye according to the manufacturer's instructions (Amersham, Little Chalfont, Buckinghamshire, UK).
Animal studies
All experiments involving animals were conducted in accordance with the institutional guidelines set forth by the University of Washington. To establish subcutaneous tumors, CB17 SCID-beige mice were injected into the mammary fat pad with 1 × 105 tumor cells. Ad vectors were injected when tumors reached a diameter of 5 mm. To establish mouse models with liver metastases, animals were infused with 2×106 of human tumor cells through a permanently placed portal vein catheter (9). For intravenous application, Ad vectors in 100μl of PBS were injected through the tail vein.
The following methods are described in the “Supplementary Material”
Virus attachment/uptake assays, cytolysis assays, expression arrays, qRT-PCR and qPCR analyses, immunofluorescence/confocal analyses, Western Blot, and statistical analyses.
Results
Resistant ovarian cancer cells have an epithelial phenotype
We subjected primary cultures from tumor biopsies of III and IV ovarian cancer patients to limited dilution culturing and established >100 clonal cultures from each primary culture. Most of the data shown in this study were obtained with clonal cultures derived from biopsy ovc316 obtained from a stage IVB serous ovarian cancer that was resistant to primary chemotherapy. We have similar findings with clonal cultures from other chemotherapy resistant tumors. The morphology of clonal cultures from ovc316 varied greatly (Suppl. Fig.1). In a first study, we used Ad5/35.IR.E1A/TRAIL (6) as a model oncolytic adenovirus. This vector is targeted to CD46 by the Ad serotype 35 fiber, allows for tumor-specific, replication-activated expression of E1A and TRAIL, and efficient tumor cell killing. In cytolysis studies, we found that the morphological heterogeneity seen in clonal cultures was also reflected in a heterogeneic response to the infection by Ad5/35.IR-E1A/TRAIL (Fig.1A). Clonal cultures that were resistant to Ad5/35.IR-E1A/TRAIL lysis (N=15) were subjected to genome-wide mRNA expression analysis in comparison to clonal cultures susceptible to viral oncolysis (N=16). We found 983 differently expressed genes (p<0.017). Hierarchical clustering of these genes showed a clear-cut separation of resistant and susceptible clones (Suppl. Fig.2). Using gene ontology software (10), we found that pathways involving tight and adherens junction formation and cell adhesion were significantly different in resistant cells (p<0.008) (Suppl. Figs.3A-E). Altered RNA expression levels of key genes found in microarray studies was validated by qRT-PCR (Suppl. Fig.4). Gene expression on protein level was studied by immunofluorescence and flow cytometry analyses (Figs.1C and D). Immunofluorescence analyses demonstrated high-levels of adherens proteins (E-cadherin), tight junction proteins (occludin, claudin 1, 2, 3, 4, 7), and the epithelial marker EpCAM in resistant cells (Fig.1D-upper panel, Suppl. Fig.5). Conversely, susceptible cells predominantly expressed markers that are characteristic for mesenchymal cells (vimentin, laminin, collagen IV, fibronectin, N-cadherin) (Fig.1D- lower panel, Suppl. Fig.5). Furthermore, expression of CD44 was higher in susceptible than resistant clones. Notably, CD44 is considered a marker for mesenchymal stem cells (11-13). Of particular interest was the high prominence of p120 catenin containing the regulatory N-terminus in susceptible cells (N-p120), which, in part, explains why Ecadherin is absent on the surface of these cells (14) (Suppl. Fig.6). Other marker proteins that discriminated resistant and susceptible clones included cingulin, vinculin, the cytoskeleton protein F-actin, and netrin 4 (Suppl. Fig.5). Flow cytometry analyses corroborated that clonal ovarian cancer cultures express both epithelial and mesenchymal markers, whereby clones resistant or susceptible to Ad5/35.IR-E1A/TRAIL show the balance greatly shifted towards epithelial or mesenchymal markers, respectively (Fig.1C). In all studies described below, resistant and susceptible clones were designated as R/E (resistant/epithelial) and S/M (susceptible/mesenchymal), respectively.
Fig.1. Analysis of clonal ovarian cancer cultures that were either resistant or susceptible to lysis by Ad5/35.IR-E1A/TRAIL.
A) Cytolysis caused by Ad5/35.IR-E1A/TRAIL in clonal cultures derived from biopsy ovc316. Clonal cultures indicated in black were subjected to DNA expression array analysis. Standard deviation was less than 10% of the average for all samples. Infection at MOIs 10 and 200 pfu/cell resulted in a similar distribution. B) Focal adhesion, tight junction (TJ) and adherens junction (AJ) pathways. Genes that were found upregulated in arrays are marked red. Down-regulated genes are marked green. TJ proteins, include claudins and occludin. AJ proteins include E-cadherin. The cytoplasmic domain of E-cadherin interacts with ß-catenin and p120-catenin. Claudins and occludin interact with ZO-1, and subsequently with F-actin via cingulin. Caldesmon inhibits Arp2/3-mediated actin polymerization. Phosphoinositide 3-kinase (PI3K) and Focal adhesion kinase (FAK) are involved in the regulation of Rho GTPases downstream of integrin signaling. Rho kinase (ROCK) is activated by RhoA. Vinculin and α-actin crosslink the cytoskeleton to focal adhesion spots. Vimentin is the major intermediate filament (IF) protein of mesenchymal cells that is involved in regulation of attachment, migration, and cell signaling. Palladin functions as a scaffold that regulates actin organization. Profilin is involved in turnover of the actin filament network. C) Flow cytometry analysis of resistant and susceptible clones. Two representative clones are shown. D) Immunofluorescence analysis of epithelial marker proteins (upper panels) and mesenchymal marker proteins (lower panels) on resistant and susceptible clones. Representative clones are shown.
We next tested whether our findings could be validated in the primary (low passage) ovc316 culture from which the clones were derived. We found that E-cadherin-positive and laminin-negative cells were resistant to lysis by Ad5/35.IR-E1A/TRAIL (Fig.2A). At day 4 after infection most susceptible cells (laminin- and N-p120-positive) showed bright red viral hexon signals, indicating viral replication. At day 8 day p.i., only E-cadherin positive cells remained in infected ovc316 cultures. Flow cytometry analyses revealed that the percentage of vimentinhigh (mesenchymal) cells decreased over time, while the percentage of E-cadherinhigh cells increased (Fig.2B). Notably, E-cadherinhigh/vimentinlow cells appeared to be more resistant than E-cadherinhigh/vimentinhigh cells.1 Greater resistance of cells that differentiated towards epithelial cells is also seen in flow cytometry analysis of E-cadherin/N-p120 and EpCAM/CD44.
Fig.2. Analysis of primary ovarian cancer culture ovc316 for epithelial and mesenchymal markers after infection with Ad5/35.IR-E1A/TRAIL.

A) Primary cultures (passage 10) were infected with Ad5/35.IR-E1A/TRAIL at an MOI of 100 pfu/cell and analyzed at day 2, 4, and 8 after infection for immunofluorescence of as indicated. Uninfected cells were used as a control. B) Flow cytometry of infected cells. Representative samples are shown. Notably, resistant cells that showed cytoplasmic E-cadherin staining in immunofluorescence studies scored negative by flow cytometry analysis for surface E-cadherin.
Adenovirus receptors are trapped within tight junctions of epithelial ovarian cancer cells
To study the mechanisms of resistance to killing by Ad5/35.IR-E1A/TRAIL, we first analyzed attachment of 3H-labelled Ad5/35.IR-E1A/TRAIL particles. We found >3-times more Ad particles attached to S/M clones than to R/E clones (Fig.3A-left panel). Consequently, subsequent infection steps, including virus genome replication and gene expression were affected in R/E cells (Fig.3A-middle and right panels, Suppl. Fig.7A). Using fluorophore-labeled Ad5/35 particles, we showed inefficient attachment to R/E cells also in immunofluorescence studies (Suppl. Fig.7B). These studies revealed that the post-attachment signaling which results in re-organization of the F-actin network or recruitment of the focal adhesion protein vinculin in S/M clones, is not activated in R/E clones. Because our data suggested that inefficient attachment of Ad particles to epithelial ovarian cancer cells is largely responsible for resistance to killing by Ad5/35.IRE1A/TRAIL, we concluded that other vectors with an Ad5/35 capsid will also be inefficient in infection/lysis of epithelial ovarian cancer cells. We showed that transduction with an Ad5/35.GFP vector was significantly less efficient in E/R clones than in S/M clones (Suppl. Fig.8). Overall, the efficiency of Ad5/35.GFP transduction correlated with Ad5/35.IRE1A/TRAIL mediated oncolysis when analyzed in individual R/E and S/M clones (Suppl.Fig.8B).
Fig.3. Analysis of adenovirus receptors.
A) Ad infection of R/E and S/M cells. Left panel: Attachment of 3H-labeled particles to cells. Middle and right panels: Virus uptake and genome replication. The amount of viral genomes in cells was measured 3 and 72 hours after infection with Ad vectors at an MOI of 100 pfu/cell by qPCR. B) Flow cytometry analysis of surface CD46 and αV integrins on R/E (resistant) and S/M (susceptible) clones. C) Confocal microscopy analysis of CD46, αV integrin, and claudin 7 on cells that were incubated with Cy3-labeled Ad5/35.IR-E1A/TRAIL (4,000 vp/cell) on ice for 30 min (“attachment”) or incubated with virus for 2 hours at 37°C (“internalization”). D) Infection of cells with Ad5/35.GFP from the apical and basal side. Clonal cultures were seeded using tissue culture inserts in 48 well plates and virus was added to medium on top or below cells at an MOI of 10 or 100 pfu/cell. GFP expression was analyzed 48 hours later by flow cytometry.
An oncolytic Ad5/35 vector (Ad5/35Δ24Ki/Cox) expressing the Ad E1 and E4 gene products under the control of the Ki67 and the cyclooxygenase-2 promoter, respectively (7) predominantly killed mesenchymal cells (vimentinhigh/p120high), while epithelial cells (E-cadherinhigh) were resistant (Suppl. Fig.9).
To understand the mechanisms of decreased attachment of Ad5/35 particles to epithelial cells, we analyzed the levels of the primary Ad5/35 attachment receptor CD46, and the levels of αV-integrins, which are considered to be involved in Ad5/35 uptake (15). Surprisingly, there was no significant difference both in the percentage of CD46 and αV -integrin positive cells and in the mean fluorescence levels between R/E clones, S/M clones, and the original (p1) ovc316 culture (Fig.3B). However, confocal microscopy revealed that the majority of CD46 signals were inside tight junctions, with few receptor molecules localized to the apical and basolateral membrane of E/R cells. In contrast, in S/M cells, CD46 was evenly distributed over the entire cell membrane. Cy-3 labeled Ad particles did not bind to CD46 trapped in tight junctions (Fig.3C, Suppl. Fig.10). In contrast, in S/M cells, Ad particles attached to cells from both apical and basolateral sides. In R/E cells, αV integrins were found in tight junctions and on the basolateral membrane. Consequently, Ad particles that were attached to the few apically localized CD46 molecules cannot be internalized into R/E cells. In contrast, in S/M cells both CD46 and αV-integrin co-localize, conferring efficient Ad internalization. These findings were corroborated by transduction studies in trans-well chambers, where Ad5/35.GFP vectors were applied either from the apical or basolateral sides of cells (Fig.3D, Suppl. Fig.8C-D). While the percentage of GFP-expressing cells was comparable in S/M cells and ovc316m cells infected from either, the apical or basolateral side, in R/E cells apical infection was markedly less efficient due to the low numbers of CD46 receptors and the apparent lack of αV integrins on the apical side. The finding that basolateral transduction of R/E cells was efficient can be explained by the high density of αV integrins and the presence of a few CD46 receptors on this membrane side.
The epithelial phenotype of ovarian cancer cells is a barrier to Ad infection in vivo
On tumor sections from ovarian cancer patients, we found large subsets of malignant epithelial cells surrounded by tumor stroma, consisting of laminin (Fig.4A). This morphology could be reproduced in mouse xenografts derived from ovarian cancer cultures. In both patient tumors and xenografts, CD46 and αV integrins were co-localized with the tight junction protein claudin 7, supporting our in vitro findings (Fig.4A and Suppl. Figs. 11A, B). This histology was observed for all ten analyzed biopsies from ovarian cancer patients (Suppl. Fig.11C) as well as in xenografts derived from the ovarian cancer cell line SKOV3-ip1 (Suppl. Fig.11D). As expected from this morphology, both intratumoral and intravenous injection of Ad5/35.IR-E1A/TRAIL into mice bearing subcutaneous ovc316 xenografts had no effect on tumor growth compared to PBS injected mice (data not shown). No viral replication (based on Ad hexon staining) was detectable in ovc316 tumors at day 8 after intratumoral injection of Ad5/35.IR-E1A/TRAIL (Fig.4A, lower panel). Intratumoral injection of Ad5/35-GFP resulted in very few GFP-expressing cells directly surrounding the needle track. Intravenous injection of an Ad5/35 vector conferred transgene expression only in sparse cells around the tumor periphery, a tumor area that contained blood vessels.
Fig.4. Analysis of ovc316 xenografts.

A) Analysis of tumor sections. Upper panel: Expression of E-cadherin (green) and laminin (red) Middle panel: Co-localization of CD46 (green) or αV integrins (green) with the tight junction protein claudin 7 (red). Lower panel: Viral hexon and E-cadherin expression at day 8 post injection of 2×109 pfu of Ad5/35.IR-E1A/TRAIL; In vivo GFP expression after intratumoral injection of Ad5/35.GFP. In vivo βGal expression after intravenous injection of Ad5/35. βGal. B) Flow cytometry of cell suspensions and cultured ovc316 cells at passage 1 and 20. C) Western blot for key members of pathways that regulate tight junction reorganization and EMT. D) Effect of inhibitors {exoenzyme C3 from Clostridium botulinum (inhibitor of Rho A, B and C GTPases), H-1152 (Rho-kinase inhibitor), Clostridium difficile toxin B (inhibitor for Rho, Rac, and Cdc42), Wortmannin (inhibitor of PI3K)} on viability of Ad5/35.IR-E1A/TRAIL infected R/E and S/M cells. Cell viability was measured at day 4 after infection at an MOI of 100 pfu/cell. Significance was compared to infected, Mock treated cells. ***p<0.001, **p<0.01, *p<0.05
Although the majority of cells in early passage ovc316 cultures was susceptible to Ad5/35 infection in vitro (see Fig.2), in vivo transduction after Ad5/35 injection into ovc316 xenografts was very inefficient. To clarify this discrepancy, we performed flow cytometry analyses for EpCAM, vimentin, and CD44 on cell suspensions of ovc316 xenograft tumors and on cultured ovc316 cells from passage 1 and 20 (Fig.4B). In xenografts the vast majority of ovarian cancer cells (>80%) expressed high levels of EpCAM, whereby a significant faction of these cells were also positive for vimentin and CD44, indicating that these cells were in a hybrid epithelial/mesenchymal stage (E/M cells). Interestingly, most cells isolated from xenografts that adapted to tissue culture were E/M cells. When further passaged, E/M cells lost EpCAM expression and differentiated towards the mesenchymal phenotype. As outlined above, E/M cells with intracellular mesenchymal features, and mesenchymal cells represented the populations susceptible to oncolysis in vitro. Similar to what we observed for ovc316, there was an in vivo and in vitro discrepancy between the phenotypes for ovarian cancer SKOV3-ip1 cells, cervical adenocarcinoma HeLa cells, colon cancer HT-29, and liver endothelial cancer SK-Hep1 cells (Suppl. Fig.12). Notably, R/E cell clones do not form tumors. Tumor formation requires the presence of E/M hybrid cells, which differentiate in vivo to epithelial cells (Strauss et al. in preparation). In situ, these hybrid cells are embedded in nests of epithelial cancer cells, which protects them from Ad5/35 transduction in vivo.
The epithelial phenotype of ovarian cancer cells is also a barrier to infection with CAR-interacting, Ad5-based vectors
The finding that the Ad5/35 receptor, CD46, is trapped in tight junctions is reminiscent of the situation with the Ad5 receptor, CAR, which is known to be an integral tight junction protein (16). We found that CAR levels were not significantly different between epithelial and mesenchymal ovarian cancer cultures (Suppl. Fig.13A). As seen with Ad5/35.IR-E1A/TRAIL, epithelial cultures could not be infected from the apical side with an Ad5 vector expressing GFP (Suppl Fig.13B). We also observed a correlation between resistance to infection by an Ad5-based oncolytic vector (Ad5.IR-E1A/TRAIL) and the epithelial cell phenotype of ovarian cancer in immunofluorescence and flow cytometry studies (Suppl. Figs.13C and D). On sections of ovc316 xenografts, CAR was found to be co-localized with the tight junction protein claudin 7 (Suppl. Fig.14) and in vivo application of Ad5 vectors resulted in similarly inefficient tumor cell transduction as described above for Ad5/35 vectors (data not shown).
Analysis of pathways that are involved in maintaining the epithelial phenotype of ovarian cancer cells
To understand the regulation of tight and adherens junction pathways in ovarian cancer cells, we studied the presence of key members of these pathways in clonal R/E and S/M cultures, as well as in xenograft tumors and cultures derived from them at passage 1 and 20 by Western blotting. As expected, we found high levels of E-cadherin in R/E cells and tumors, while with passaging of primary cells the level of E-cadherin decreased (Fig.4C). In agreement with the immunofluorescence data (Fig.1D), N-p120 is expressed at higher levels in S/M clones, and its expression increases with differentiation of epithelial/mesenchymal hybrid cells into mesenchymal cells during passaging of ovc316 cultures. Differences in N-p120 levels indicate a role of Rho GTPases in conferring resistance to Ad5/35 infection. Along this line, we found different RhoA levels in R/E and S/M clones. Our Western blot analyses further corroborated that R/E clones are closer to tumor cells in vivo and represent a more adequate model for attempts to overcome resistance than populations of primary ovarian cancer cells. Interestingly, expression of ROCK, the downstream effector kinase of Rho, was almost undetectable in R/E cells. Like Np120, active ROCK is reported to contribute to EMT and the invasive phenotype of epithelial cancers (17, 18), highlighting the importance of mesenchymal features for the susceptibility to viral infection and oncolysis. For focal adhesion kinase, a difference between xenograft tumor and in vitro cultures was observed.
To validate the role of these pathways in maintenance of epithelial morphology and to potentially manipulate these pathways, we used a series of inhibitors. Treatment of S/M and R/E-EMT cells with Rac/Cdc42/RhoA, Rho (A/B/C) or ROCK inhibitors increased their resistance to killing by Ad5/35.IR-E1A/TRAIL (Fig.4D). This is most likely due to inhibition of Rho family GTPases that are involved in formation of tight/adherens junctions and that are also required for efficient integrin-mediated Ad internalization and/or intracellular trafficking (19). Surprisingly, unlike GFP expression after infection with Ad5/35.GFP, basal infection of R/E cells with Ad5/35.IR-E1A/TRAIL had no enhancing effect on cell killing compared to apical application of viral particles. This indicates that viral replication and spread is affected in R/E cells even after successful infection. Inhibitors of Rho GTPases did not increase expression of tight or adherens junction proteins or change the localization of Ad receptors in S/M cells. This is in line with our conclusion that defects in regulation of Rho-GTPases represent another, independent mechanism that inhibits oncolysis in resistant cells, in addition to upregulated tight and adherence junctions and receptor trapping that prevents Ad infection.
Ad5/35 vectors transduce non-epithelial tumors in vivo
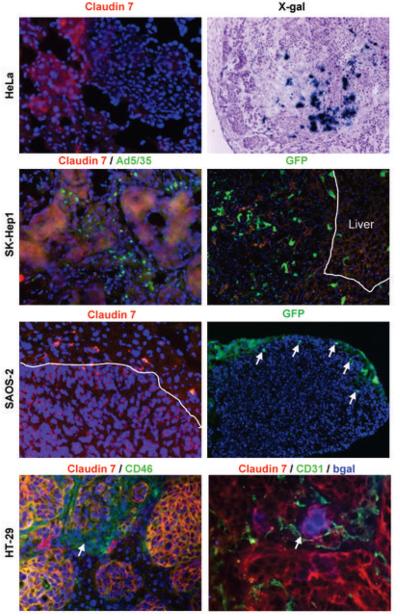
If our hypothesis that the epithelial phenotype of cancer cells prevents infection by Ad5/35 vectors is correct, tumors derived from non-epithelial cells should be more susceptible to Ad5/35 infection. To test this, we employed a more clinically relevant metastasis model with human cancer cell lines derived from either epithelial tumors (HT29-colon cancer; SAOS-epithelial sarcoma) or non-epithelial tumors (SKHep1-liver endothelial cancer; HeLa-cervical adenocarcinoma) (Fig.5). Mice with pre-established liver metastases received a tail vein injection of Ad5/35.GFP or Ad5/35.bGal and tumor/liver sections were analyzed for GFP/β-galactosidase, claudin 7, and/or CD46 three days later. HeLa and SK-Hep1 cell-derived liver metastases did not express claudin 7 in cell junctions and therefore could be efficiently transduced with an Ad5/35 vector. In contrast, in SAOS- and HT-29-derived liver metastases, the majority of tumor cells were claudin 7-positive 7, and could not be transduced with Ad5/35 vectors. Interestingly, a sparse number of HT29 cells had a different morphology (see arrow), with CD46 evenly distributed over the cell surface and it was these cells that expressed bGal after tail vein injection of Ad5/35bGal. In agreement with our earlier findings, access to tumor cells by blood vessels was another limiting factor for transduction of HT29 cells in vivo (9). Notably, we also found in vitro a correlation between the level of epithelial marker expression and Ad5/35 transduction of HeLa, HT-29, and SK-Hep1 cells (Suppl. Fig.15).
Fig.5. Correlation between epithelial and mesenchymal phenotype of liver metastases and Ad5/35 vectors transduction after intravenous injection.
Human tumor cells (HeLa, SK-Hep1, SAOS, or HT-29) were injected into the portal vein of immunodeficient mice. After liver metastases formed, mice received a tail vein injection of 2 × 109 pfu of Ad5/35 vectors expressing either GFP or βGal. Tumor-bearing livers were analyzed 3 days later for claudin 7 and transgene expression. HT-29 tumor bearing liver sections were also stained for CD31. For SK-Hep1 tumors, viral particles were visualized with an anti-hexon-FITC antibody at 2 hours post-injection.
Human Ad serotypes that do not use CD46 or CAR trigger removal of E-cadherin from cell surface and allow for infection of R/E cells
Recently, we found that that human species B Ads serotypes Ad3, Ad7, Ad11, and Ad14 use a yet unknown receptor (receptor X), which is different from CAR and CD46 (4). These serotypes use at least two binding moieties on the cell membrane. The C-terminal part of the Ad fiber (the fiber knob) binds to sulfated carbohydrate chains of heparan-sulphate proteoglycans (HSPGs). This Ad knob – interaction with heparan sulphate glycosaminoglycans (HS-GAGs) allows for subsequent high affinity attachment and/or access to receptor X, whereby receptor X is either the protein part of the HSPG that interacts with the Ad3 knob or an independent non-HSPG protein (20). Based on this, we hypothesized that these Ads were better candidates for achieving infection of R/E cells than Ad5 and Ad35. In support of this we found that HSPGs expressed on E/R cells were not trapped in tight junctions (Fig.6A, left upper panel). Cy3-labeled Ad3 particles efficiently bound to R/E cells, whereas cell-associated Cy3-Ad35 signals were detectable on only sparse R/E cells (Fig.6A, left lower panel). Importantly, incubation of R/E cells with wild-type Ad viruses mediated removal of E-cadherin from the cell surface for Ad3, 7, 11, and 14 but not for the CAR-interacting Ad5 and the CD46-interacting Ad35 (Fig.6A right panel) and Ad5/35 viruses. This study also shows that Ad3, 7, 11, and 14 are able to kill R/E cells which is reflected in plaque-like foci within the cell monolayer, with hexon expressing cells along the periphery of the lysis plaques. We also found a clear grouping of Ads in cytolysis assays (Suppl. Fig.16). Ad3, 7, 11, and 14 were significantly more efficient in lysing R/E cells than Ad5 and Ad35. Changes of membrane E-cadherin in R/E cells depending on the serotype used for infection were corroborated by flow cytometry studies (Fig.6B). Mean E-cadherin fluorescence on R/E cells infected with Ad3, 7, 14, and Ad11 was about one order of magnitude less than in Ad5-, Ad35-, and Ad5/35-infected cells. Finally, after intratumoral injection into subcutaneous ovc316 tumors, we found markedly more hexon-positive cells in Ad3 injected tumors than in Ad35 injected tumors (Suppl.Fig.17). Hexon staining was found in both claudin7-positive and –negative cells, indicating that both epithelial and non-epithelial cancer cell subsets were transduced. The latter was also confirmed by flow cytometry for E-cadherin and GFP (data not shown). In an attempt to quantify in vivo transduction, we measured hexon mRNA levels in total RNA isolated from transduced tumors by qRT-PCR. Hexon mRNA levels were about 10-fold higher in Ad3 injected tumors compared to Ad35 injected tumors at day 3 p.i., and continued to rise by day 11, indicating viral replication (Fig.6C). We also found that a single intratumoral injection of 2×109pfu of wtAd3 significantly delayed tumor growth, while Ad35 injection had no therapeutic effect (Fig.6D). It was impossible to conduct longer studies because mice became moribund after day 10, which we attributed to low-level replication of wild-type virus in normal tissue. At necropsy, we found enlarged livers and spleens, and histological analysis revealed signs of hepatitis. More detailed therapy studies require therefore the generation of conditionally replicating Ad3, 7, 11, or 14 vectors. This task would first require basic studies on DNA replication of these serotypes, which would go beyond the scope of the present paper.
Fig.6. Analysis of infectivity of ovarian cancer cells by different Ad serotypes.

A) Immunofluorescence analyses on R/E cells. Left upper panel: Expression of HSPGs (green) and claudin 7 (red) on R/E cells. Left lower panel: Cy3-Ad3 and Cy3-Ad35 attachment in R/E cells (right panel). Right panel: Effect of Ad 3, 5, 7, 11, 14, and 35 infection (MOI 100pfu/cell) on cell morphology and E-cadherin (green) expression in R/E cells. Viral replication was visualized by staining for hexon (red). The analysis was done at day 4 p.i. B) Flow cytometry analyses of Ad infected cells (same conditions as in B). C and D) In vivo transduction of wAd3 and wtAd35. A total of 2×109 pfu of Ad3 and Ad35 was intratumorally injected into subcutaneous ovc316 tumors. C) Transduction was quantified by qRT-PCR for hexon mRNA using pan-serotype hexon primers that can detect both Ad3 and Ad35 hexon mRNA (23). N=5. D) Ovc316 tumor volume after mock injection or intratumoral injection of 2×109 pfu of wtAd3 or wtAd35, N=5.
Discussion
We discovered that the epithelial phenotype of ovarian cancer represents a barrier to oncolysis by oncolytic Ads targeted to CAR, CD46, or αV integrins. Specifically, we demonstrated that these Ad receptors were trapped in tight junctions and not accessible to virus binding. Xenograft tumors contained almost exclusively cells in an epithelial or epithelial/mesenchymal (E/M) hybrid stage, based on their surface markers. Ovarian cancer cells in situ where therefore resistant to infection by CAR- and CD46-targeting Ads. Cells that adapted to tissue culture were in an E/M stage, however, in contrast to E/M cells in vivo, cultured cells already acquired mesenchymal markers such as intracellular N-p120 (Fig.1C) in a process reminiscent of EMT. Over passaging, E/M cells further differentiated into mesenchymal cells, a cell type that is not present in the tumor in situ. Cells undergoing EMT and mesenchymal cells were susceptible to infection by Ad5 and Ad5/35 vectors. Our findings imply that the cell biology of populations of primary ovarian cancer cell cultures and cancer cells in situ is different and that population cell cultures have only limited value for studying resistance to Ad infection. Importantly, clonal R/E cultures were not able to undergo EMT and retained the epithelial phenotype reminiscent of the tumor in situ. The inability of R/E cells to undergo EMT and to maintain the epithelial phenotype seems to be directly linked to the absence and/or inactivity of ROCK in these cells. This speculation is supported by a recent study, demonstrating that Rho-Dia1 signaling stabilized adherens junctions (21). Notably, using tumor cell lysis as the endpoint for resistance studies, expression array studies revealed significantly altered expression for 983 genes, only 33 of which were involved in tight and adherens junction pathways. This indicates that mechanisms other than upregulated tight and adherens junctions and Ad receptor trapping are involved in conferring resistance to viral oncolysis. Although the absence/inactivity of ROCK and, potentially other defects in the regulation of Rho-GTPases, are indicative, further studies are needed to delineate the cellular factors and pathways required for efficient infection and oncolysis of epithelial ovarian cancer cells.
An important conclusion from our study is that non-epithelial tumors are more susceptible to treatment with currently existing oncolytic viruses. Unfortunately, most cancers are derived from epithelial cells and approaches to target epithelial cancers by virotherapy are needed. We showed that Ad3, 7, 11, and 14, serotypes that use receptor(s) other than CAR and CD46 efficiently infected epithelial ovarian cancer cells and caused oncolysis in vitro and in vivo. We demonstrated that Ad3, 7, 11, and 14 efficiently infected R/E cells and triggered removal of E-cadherin from the cell surface and dissolution of adherens junctions. This indicates that these Ads forced R/E cells into EMT thus conferring susceptibility to infection/ and virus spread. So far little is known about the infection mechanism and the key attachment receptor (receptor X) of these serotypes is still elusive. In this context, induction of EMT-like events in R/E cells could be the result of Ad receptor signaling and/or E1A expression upon infection (22), or both.
Our study helps to better understand the cell biology of ovarian cancer, specifically mechanisms that confer resistance to currently used oncolytic Ads. The discrepancies that we found in the phenotype of ovarian cancer cells in vitro and in vivo, in part, explain why approaches using oncolytic adenoviruses showed promising results in vitro, however failed in patients. Finally, our findings give a rationale for the development of conditionally replicating, oncolytic vectors based on serotype 3, 7, 11, or 14.
Supplementary Material
Acknowledgments
The work was supported by NIH grants R01 CA080192, R01 HLA078836, and P50 CA83636. We thank Robert Gentleman, Robert Haynor, and Deepayan Sarkar for help with the analysis of the microarray data. We are grateful to Kathy O'Briant, Markus Welcker, and Daniel Stone for providing materials and helpful comments.
References
- 1.Weinberg RA. Twisted epithelial-mesenchymal transition blocks senescence. Nat Cell Biol. 2008;10:1021–3. doi: 10.1038/ncb0908-1021. [DOI] [PubMed] [Google Scholar]
- 2.Loeb LA, Bielas JH, Beckman RA. Cancers exhibit a mutator phenotype: clinical implications. Cancer Res. 2008;68:3551–7. doi: 10.1158/0008-5472.CAN-07-5835. discussion 7. [DOI] [PubMed] [Google Scholar]
- 3.Hermiston T. A demand for next-generation oncolytic adenoviruses. Curr Opin Mol Ther. 2006;8:322–30. [PubMed] [Google Scholar]
- 4.Tuve S, Wang H, Ware C, et al. A new group B adenovirus receptor is expressed at high levels on human stem and tumor cells. J Virol. 2006;80:12109–20. doi: 10.1128/JVI.01370-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiPaolo N, Ni S, Gaggar A, et al. Evaluation of adenovirus vectors containing serotype 35 fibers for vaccination. Mol Ther. 2006;13:756–65. doi: 10.1016/j.ymthe.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sova P, Ren X-W, Shaoheng N, et al. A tumor-targeted and conditionally replicating oncolytic adenovirus vector expressing TRAIL for treatment of liver metastases. Mol Ther. 2004;9:496–509. doi: 10.1016/j.ymthe.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann D, Bayer W, Heim A, Potthoff A, Nettelbeck DM, Wildner O. Evaluation of twenty-one human adenovirus types and one infectivity-enhanced adenovirus for the treatment of malignant melanoma. J Invest Dermatol. 2008;128:988–98. doi: 10.1038/sj.jid.5701131. [DOI] [PubMed] [Google Scholar]
- 8.Shayakhmetov DM, Papayannopoulou T, Stamatoyannopoulos G, Lieber A. Efficient gene transfer into human CD34(+) cells by a retargeted adenovirus vector. J Virol. 2000;74:2567–83. doi: 10.1128/jvi.74.6.2567-2583.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li ZY, Ni S, Yang X, Kiviat N, Lieber A. Xenograft models for liver metastasis: Relationship between tumor morphology and adenovirus vector transduction. Mol Ther. 2004;9:650–7. doi: 10.1016/j.ymthe.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 10.Khatri P, Desai V, Tarca AL, et al. New Onto-Tools: Promoter-Express, nsSNPCounter and Onto-Translate. Nucleic Acids Res. 2006;34:W626–31. doi: 10.1093/nar/gkl213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barry FP, Murphy JM. Mesenchymal stem cells: clinical applications and biological characterization. Int J Biochem Cell Biol. 2004;36:568–84. doi: 10.1016/j.biocel.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 13.Conget PA, Minguell JJ. Phenotypical and functional properties of human bone marrow mesenchymal progenitor cells. J Cell Physiol. 1999;181:67–73. doi: 10.1002/(SICI)1097-4652(199910)181:1<67::AID-JCP7>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 14.Yanagisawa M, Huveldt D, Kreinest P, et al. A p120 catenin isoform switch affects Rho activity, induces tumor cell invasion, and predicts metastatic disease. J Biol Chem. 2008;283:18344–54. doi: 10.1074/jbc.M801192200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murakami S, Sakurai F, Kawabata K, et al. Interaction of penton base Arg-Gly-Asp motifs with integrins is crucial for adenovirus serotype 35 vector transduction in human hematopoietic cells. Gene Ther. 2007;14:1525–33. doi: 10.1038/sj.gt.3303019. [DOI] [PubMed] [Google Scholar]
- 16.Coyne CB, Bergelson JM. CAR: a virus receptor within the tight junction. Adv Drug Deliv Rev. 2005;57:869–82. doi: 10.1016/j.addr.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Croft DR, Sahai E, Mavria G, et al. Conditional ROCK activation in vivo induces tumor cell dissemination and angiogenesis. Cancer Res. 2004;64:8994–9001. doi: 10.1158/0008-5472.CAN-04-2052. [DOI] [PubMed] [Google Scholar]
- 18.Han Z, Xu G, Zhou J, et al. Inhibition of motile and invasive properties of ovarian cancer cells by ASODN against Rho-associated protein kinase. Cell Commun Adhes. 2005;12:59–69. doi: 10.1080/15419060500383168. [DOI] [PubMed] [Google Scholar]
- 19.Li E, Stupack D, Bokoch GM, Nemerow GR. Adenovirus endocytosis requires actin cytoskeleton reorganization mediated by Rho family GTPases. J Virol. 1998;72:8806–12. doi: 10.1128/jvi.72.11.8806-8812.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tuve S, Wang H, Jacobs JD, Yumul RC, Smith DF, Lieber A. Role of cellular heparan sulfate proteoglycans in infection of human adenovirus serotype 3 and 35. PLoS Pathog. 2008;4:e1000189. doi: 10.1371/journal.ppat.1000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sahai E, Marshall CJ. ROCK and Dia have opposing effects on adherens junctions downstream of Rho. Nat Cell Biol. 2002;4:408–15. doi: 10.1038/ncb796. [DOI] [PubMed] [Google Scholar]
- 22.Behzad AR, Morimoto K, Gosselink J, Green J, Hogg JC, Hayashi S. Induction of mesenchymal cell phenotypes in lung epithelial cells by adenovirus E1A. Eur Respir J. 2006;28:1106–16. doi: 10.1183/09031936.06.00060105. [DOI] [PubMed] [Google Scholar]
- 23.Stone D, Liu Y, Li ZY, Tuve S, Strauss R, Lieber A. Comparison of adenoviruses from species B, C, E, and F after intravenous delivery. Mol Ther. 2007;15:2146–53. doi: 10.1038/sj.mt.6300319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.