Abstract
Physical performance limitations are one of the potential long-term consequences following diagnosis and treatment for childhood cancer. The purpose of this review is to describe the risk factors for and the participation restrictions that result from physical performance limitations among childhood cancer survivors who participated in the Childhood Cancer Survivor Study (CCSS). Articles previously published from the CCSS cohort related to physical performance limitations were reviewed and the results summarized. Our review showed that physical performance limitations are prevalent among childhood cancer survivors and may increase as they age. Host-based risk factors for physical disability include an original diagnosis of bone tumor, brain tumor, or Hodgkin's disease; female sex; and an income less than $20,000 per year. Treatment-based risk factors include radiation and treatment with a combination of alkylating agents and anthracyclines. Musculoskeletal, neurologic, cardiac, pulmonary, sensory, and endocrine organ system dysfunction also increase the risk of developing a physical performance limitation. In summary, monitoring of physical performance limitations in an aging cohort of childhood cancer survivors is important and will help determine the impact of physical performance limitations on morbidity, mortality, and caregiver burden. In addition, in developing restorative and preventive interventions for childhood cancer survivors, we must take into account the special needs of survivors with physical disability to optimize their health and enhance participation in daily living activities.
INTRODUCTION
Function and Physical Disability
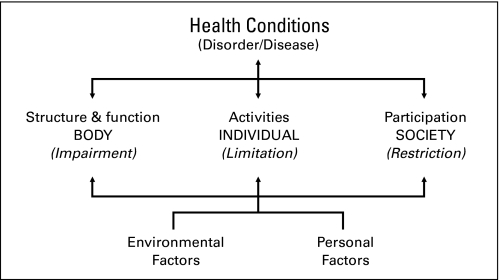
One of the possible long-term consequences of childhood cancer and its treatment is physical disability. Disability implies a substantial decrease or absence of function, as characterized by WHO in the International Classification of Function, Disability, and Health (ICF; Fig 1).1 In this model, function is an umbrella term used to describe human capacity in relation to the body, the individual, and society. These interdependent domains include: 1) the structure and function of the body's organ systems; 2) the abilities of the individual to perform regular tasks or activities, like walking, dressing, and taking a bath; and 3) the capacity of the individual to participate fully in life's roles as a member of his or her family, work or school environment, or community. Both personal and host factors, including disease states like cancer, interact with these three functional domains to determine whether or not a person has a disability.
Fig 1.
The interaction between the components of the International Classification of Functioning, Disability, and Health.
Problems at the body structure and function levels are called impairments; the inability to perform usual tasks at the individual level are termed activity or performance limitations; and suboptimal capacity in societal roles are referred to as participation restrictions. For example, a child who is diagnosed with a brain tumor may have residual ataxia and poor balance related to cerebellar damage. As a result, this child may have suboptimal skills and efficiency performing tasks like walking, running, stopping, and starting, thus making it difficult to participate in physical education classes and afterschool sports activities. Throughout childhood and into adulthood, his or her ataxic movements may limit recreational or career choices to those that require only minimal motor skill competency.
Educational and Economic Impact of Physical Performance Limitations
The incidence of physical performance limitations and associated participation restrictions may place young cancer survivors with physical disability at risk for less than optimal attainment of economic, educational and occupational goals. Physical disability in the general population is associated with lower income levels, less educational attainment, and lower rates of employment.2,3 Across all age ranges, individuals with physical disability are more likely to live in poverty than those without physical disability. The percentage of children in the United States from 5 to15 years of age with a physical disability who live in a household with an annual income below the poverty level is 32% compared with 17% of children without physical disability in the same age range. This income disparity persists across age groups, with 30% of physically disabled persons age 16 to 20 years living below the poverty line compared with 17% of their nondisabled counterparts.2,3 Among people age 21 to 64 years, 26% of those with a physical disability and 10% of those without a physical disability have incomes below the poverty level.2 Adults with a physical disability are also more likely to lack a high school degree (28.7% v 16.7%) and be unemployed (68% v 26.6%) than those without a physical disability.2
Social and Health Care Access Consequences of Physical Performance Limitations
Physical disability is also potentially associated with poor health care access, and with limited opportunity for participation in community or social roles. Individuals with physical disability are less likely to report having a primary care provider than are persons without physical disability.4 Physical disability among women is associated with lower rates of screening for breast cancer, cervical cancer, and osteoporosis.5–7 Eighteen percent of persons in the United States with a disability compared with 7% of persons without a disability report not getting needed health care on at least one occasion in the past year.3 Poor health care access in the disabled population is attributed to barriers related to employment and insurance, environment and physical structures, and process- and health provider-based barriers.4,8–10 According to the Harris Surveys of Americans with Disabilities, 3 individuals with a disability are less likely to socialize with close friends neighbors or relatives (89% v 79%), to attend relevant religious services (49% v 57%), or to eat at a restaurant (57% v 73%) than are persons without a disability. Lack of access to the community because of inadequate access to transportation is thought to contribute to these restrictions on social participation.3,8,10 Among persons with a disability, 31% report that access to transportation is a problem. Only 13% of persons without a disability have this same concern.8
PHYSICAL PERFORMANCE LIMITATIONS IN THE CHILDHOOD CANCER SURVIVOR STUDY COHORT
Data from the first Childhood Cancer Survivor Study (CCSS) survey in 1995 and 1996 indicate that physical performance limitations, including the inability to lift objects, move a table, carry groceries, bowl, walk uphill, climb a few flights of stairs, bend, lift, stoop, walk one block, eat, dress, bathe, or use the toilet, were prevalent among 19.6% of survivors at a median age of 23 years (range, 8 to 47 years), with consequences to work or school participation reported by 7.9%.11 These numbers are expected to rise as the cohort ages. The purpose of this manuscript is to provide a summary of physical performance limitations that have been documented in the CCSS cohort, both at cohort entry, and where possible, over time. We will describe the reported diagnosis, treatment, and personal/demographic risk factors for functional loss. We will summarize the evidence that indicates that certain categories of medical late effects (disorders of body structure and function) are related to physical performance limitations. We will also briefly describe the impact of physical performance limitations on participation in roles at home, work, and in the environment.
Elevated Risk of Physical Performance Limitations Among Survivors Compared With Siblings
CCSS investigators initially evaluated physical performance limitations and participation restrictions as components of overall health status among adults who were ≥ 5-year survivors of childhood cancer. These outcomes were assessed in 9,535 CCSS participants and in a randomly selected cohort of the survivors' siblings (n = 2,916). For these analyses, questions assessing activity limitations (mobility skills including lifting and carrying, climbing stairs, and walking one block), and functional status (a combination of participation skills including self-care, community mobility, and the ability to attend work or school) were adapted from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System Survey Questionnaire.12,13 Survivors reported a 2.7-fold increased odds of activity limitations and a 5.2-fold increased odds of functional status impairment relative to the sibling control group.14
Given these data, an additional analysis was completed among cancer survivors and a sibling comparison group that focused specifically on physical performance limitations and restricted participation in home, work, or school environments.11 That study included 11,481 child, adolescent, and adult members of the cohort. The comparison group included 3,839 siblings. Physical performance was evaluated by summarizing responses to six questions that asked about the participants' performance of physical activities during the past 2 years. These included vigorous activities like running or participating in strenuous sports, moderate activity like bowling or carrying groceries, walking uphill, bending, lifting, walking one block, dressing, and bathing. Participation restrictions were evaluated in three separate categories: limited personal care skills, limited routine activities, and poor health preventing school or work attendance. After adjustment for age and sex, survivors were nearly twice as likely to report performance limitations when compared with siblings (rate ratio [RR], 1.8; 95% CI, 1.7 to 2.0). Survivors were 4.7 times (95% CI, 3.0 to 7.2) more likely to report restricted ability to perform personal care or routine activities such as shopping or housework, and 5.9 times (95% CI, 4.5 to 7.6) more likely than the sibling group to report that their poor health interfered with attending school or work.
Physical performance limitations and associated participation restrictions were also evaluated at a later point in the cohorts history as part of a quality-of-life measure.15 Using questions from the 2003 follow-up survey, Zeltzer et al16,17 compared CCSS cohort members with CCSS siblings and with general population norms on the physical function (performance) and role physical (participation) subscales of the Medical Outcomes Survey Short From-36 (SF-36). After adjusting for age, gender, and family membership, members of the CCSS cohort on average reported lower scores on the physical function and role physical scales of the SF-36 than either the sibling comparison group or the general US population. Mean T-scores for adult survivors and siblings, respectively, were 51.3 v 55.0 on physical function and 49.9 v 52.3 on role physical subscales. Mean T-scores in the similar-aged general population were 53.3 on physical function and 52.5 on role physical subscales. One standard deviation (SD) on these SF-36 subscales is 10 points. Therefore, although the survivors had statistically worse scores in both performance and participation, the differences were not large and may not represent meaningful effects.
Association Between Cancer Diagnosis Group and Physical Performance Limitations
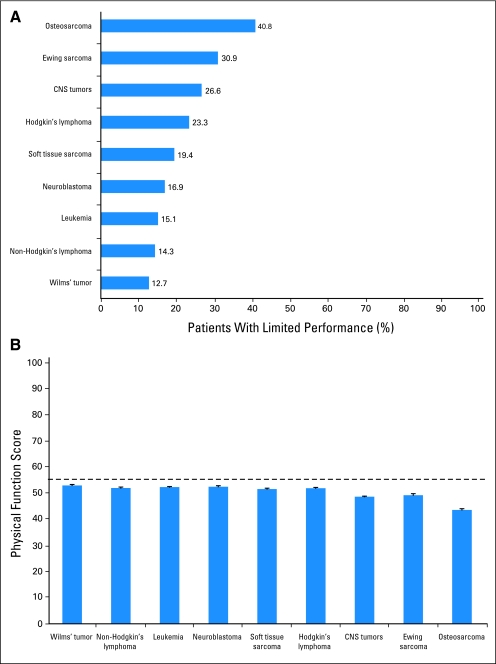
The risk of having a physical performance limitation following a diagnosis of childhood cancer varies by cancer type, both because of the differential impact of the malignancy on a particular body system, and also because of the heterogeneous nature of the treatments necessary to impart a cure. Tumors located directly in the bone, brain, and mediastinum interfere with the structure and function of organs in these areas because of tumor invasion and because of the toxic effects of localized therapies. The CCSS, because of the sheer magnitude of the number of participants within each diagnosis category, has provided investigators with unique opportunities to document the prevalence of physical performance outcomes and to compare adverse effects among diagnosis groups. Using information from the 1995 to 1996 baseline questionnaire, Hudson et al14 initially reported an elevated risk of physical activity limitations among adult survivors who had bone tumors (odds ratio [OR], 6.4; 95% CI, 5.2 to 8.0) or brain tumors (OR, 4.1; 95% CI, 3.3 to 5.1) as children, compared with those who had leukemia. These findings were extended in another publication that used data from the baseline questionnaire,11 where the highest prevalence of physical performance limitations in the CCSS cohort were reported among survivors of brain tumor (36.9%), bone tumor (26.6%), and Hodgkin's lymphoma (23.3%; Fig 2A). Subsequently, using data from the 2003 follow-up questionnaire, Zeltzer et al15 reported that the lowest scores on the role physical subscale of the SF-36 were among survivors of bone tumors, brain tumors, and Hodgkin's lymphoma (Fig 2B).
Fig 2.
(A) Percent of childhood cancer survivors with a physical performance limitation by diagnosis as reported on the baseline questionnaire in 1995 to 1996. (B) Age- and gender-adjusted score on the physical function subscale of the Medical Outcomes Survey Short Form-36 by diagnosis in 2002. The horizontal dashed line indicates the age- and gender-adjusted sibling mean score on this instrument.
Physical performance limitations among survivors of lower-extremity bone tumors have been examined in a fair amount of detail in the CCSS cohort. In addition to providing specific information about physical performance outcomes among survivors of lower-extremity bone tumors, a report by Nagarajan et al18 illustrates how the cohort can be accessed to provide an adequate sample size for evaluation of particular outcomes of interest when the disease is rare. This group of investigators identified 629 survivors of either osteosarcoma or Ewing sarcoma whose tumor was located in the lower extremity or pelvis, and mailed them an additional questionnaire that asked specific questions about physical disability and health-related quality of life. Overall, 84% of eligible participants returned their questionnaires and were included in the analyses for physical performance outcomes. These survivors were a median of 20.8 years (range, 13 to 31 years) from surgery and were a median age of 35 years (range, 19 to 49 years). On average, they scored an 85.4 (SD = 14.3) on the Toronto Extremity Salvage Scale (TESS), an instrument that asks specific questions about task performance,19 and a 7.9 (SD = 1.6) on the physical quality of life subscale of the Quality of Life for Cancer Survivors.20 These values were somewhat lower than expected when compared with a similarly aged healthy population (‘no disability’ would be a score of 100 on the TESS, and the healthy population norm for the physical subscale of the Quality of Life for Cancer Survivors is 8.25 [SD = 1.35]).20 From this questionnaire, 71.8% of these lower-extremity bone tumor survivors reported some level of disability, with 25.6% considering themselves moderately or severely limited in their ability to perform tasks necessary for daily life.
Further evaluations are pending of physical performance outcomes among the other two highest-risk groups for physical performance limitations (ie, survivors of childhood brain tumors and Hodgkin's lymphoma). However, evaluations of rhabdomyosarcoma, acute lymphoblastic leukemia (ALL), neuroblastoma, and Wilms tumor survivors participating in CCSS have been published. These have examined physical performance limitations among both diagnosis categories where clinical experience indicates potential physical disability and where it may not. Punyko et al21 reported performance limitations among 14.1% of survivors diagnosed with rhabdomyosarcoma as children, a group whose solid tumor type would suggest the potential for adverse physical performance outcome, whereas Mody et al22 reported this adverse outcome among only 7% of ALL survivors. Nathan et al23 reported that survivors of Wilms tumor and neuroblastoma on average did not report problems with physical performance when compared with population norms. However, the risk of a poor outcome was elevated among those whose tumor required a surgical procedure of the spine.23
Association Between Treatment and Physical Performance Limitations
Therapy for childhood cancer changed substantially from 1970 to 1986, the period of diagnosis for participants in the original CCSS cohort. The development of multimodality treatment approaches using surgery or radiation therapy for local tumor control and chemotherapy for systemic disease control significantly improved survival for many pediatric malignancies, but often with compromise of functional outcomes in children who required more intensive therapy to optimize outcomes. Over the years, advances in cancer biology and appreciation of the late morbidity associated with specific therapies instigated the evolution to risk-adapted treatment strategies, in which the magnitude of treatment intensity was determined by clinical and biologic factors that predicted response to therapy. The trajectory of change varied across specific cancer diagnostic types as progress was made in developmental therapeutics, radiation technology, diagnostic imaging, and surgical treatment approaches. Several CCSS investigations describe the impact of these treatment changes on physical performance outcomes in long-term survivors. The two studies summarized in this section11,14 provide a global overview of cancer treatment effects on physical performance that has been more thoroughly characterized by detailed investigations in specific diagnostic types.18,21–26,28
Hudson et al14 evaluated the impact of treatment on activity status (physical performance limitations) and functional limitations (participation restrictions) among a group of 9,535 adult CCSS participants. The analysis dichotomized treatment exposures generically as yes/no for surgery, four radiation treatment volumes (head/brain, chest/mantle, brain/chest, other) and four classes of chemotherapeutic agents (alkylators, anthracyclines, alkylators plus anthracyclines, other; Table 1). In an analysis adjusted for age, sex, race, and diagnosis, survivors treated with radiation to the head/brain were 1.3 times (95% CI, 1.0 to 1.6) more likely to report a physical performance limitation and 2.1 times more likely to report participation restrictions (95% CI, 1.7 to 2.6) than were survivors who did not receive radiation to the head/brain; survivors treated with brain/chest radiation were twice as likely to report physical performance limitations (OR, 2.0; 95% CI, 1.2 to 3.4), and almost four times more likely to report participation restrictions (OR, 3.6; 95% CI, 2.2 to 5.9) compared with survivors who did not receive radiation therapy. Survivors treated with a combination of alkylating and anthracycline agents demonstrated an increased risk of physical performance limitations. Those treated with alkylating or anthracycline agents or a combination of the two also had an increased risk of performance limitations when compared with survivors who did not receive these agents (Table 1). These results are consistent with physical performance limitations and participation restrictions resulting from cardiovascular, musculoskeletal, and neurological morbidities observed in survivors of CNS, soft tissue sarcomas, and bone tumors, who generally require multimodality therapy including high cumulative chemotherapy and radiation doses to optimize disease control.18,21,25,26
Table 1.
Associations Between Cancer Treatment and Reporting Limited Physical Performance or Participation Restrictions Among Adult Participants in the Childhood Cancer Survivor Survey Surveyed at Cohort Entry in 1995-1996
| Treatment | Physical Performance Limitation |
Participation Restriction |
||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Surgery | ||||
| No | 1.0 | 1.0 | ||
| Yes | 1.1 | 0.9 to 1.4 | 1.2 | 0.9 to 1.5 |
| Radiation therapy | ||||
| None | 1.0 | 1.0 | ||
| Head/brain | 1.3 | 1.0 to 1.6 | 2.1 | 1.7 to 2.6 |
| Chest/mantle | 1.3 | 1.0 to 1.6 | 1.1 | 0.8 to 1.4 |
| Brain/chest | 2.0 | 1.2 to 3.4 | 3.6 | 2.2 to 5.9 |
| Other | 1.2 | 1.0 to 1.5 | 1.4 | 1.1 to 1.8 |
| Chemotherapy | ||||
| None | 1.0 | 1.0 | ||
| Alkylating agent | 1.1 | 0.9 to 1.4 | 1.4 | 1.1 to 1.8 |
| Anthracycline | 1.3 | 1.0 to 1.8 | 1.5 | 1.1 to 2.1 |
| Alkylating agent + anthracycline | 1.4 | 1.1 to 1.8 | 1.5 | 1.1 to 1.9 |
| Other | 1.1 | 0.8 to 1.5 | 1.4 | 1.1 to 2.0 |
A subsequent investigation by Ness et al11 evaluated therapy associations with performance limitations among members of all ages in the cohort. Because most survivors had undergone surgical procedures, therapy was grouped into broad categories that included surgery only; radiation with or without surgery; chemotherapy with or without surgery; chemotherapy and radiation with or without surgery; treatment other than surgery, radiation, or chemotherapy; or unknown. In an analysis adjusted for age, sex, and cancer type, survivors treated with radiation were more likely to report limitations in physical performance (RR, 1.4; 95% CI, 1.1 to 1.7) and participation restrictions in self-care activities (RR, 1.7; 95% CI, 1.1 to 2.6), routine activities (RR, 1.9, 95% CI, 1.4 to 2.6), or work or school (RR, 1.8; 95% CI, 1.3 to 2.3) than were those who received surgery only. The chemotherapy and radiation group was more likely than the surgery-only group to report physical performance limitations (RR, 1.4; 95% CI, 1.2 to 1.7) and participation restrictions in self- care activities (RR, 2.3; 95% CI, 1.5 to 3.4), routine activities like shopping and housework (RR, 2.3; 95% CI, 1.7 to 3.1), and school or work attendance (RR, 2.3; 95% CI, 1.3 to 8.1). Future investigations evaluating functional status in relation to more precise treatment parameters (eg, anthracycline and alkylating agent cumulative dose, radiation dosimetry to targeted sites, and specific surgical procedures) will be important to fully characterize treatment groups at greatest risk for functional morbidity that require intervention to optimize long-term health outcomes.
Association Between Chronic Conditions and Physical Performance Limitations
Certain medical late effects have a greater effect on physical performance than do others. Importantly, research on the CCSS cohort has documented that some organ system impairments, not immediately apparent at the conclusion of cancer treatment may emerge many years later. As survivors age, these chronic conditions may interfere with the physical abilities necessary for daily life. Previous documentation of chronic medical conditions in the CCSS cohort is reviewed in this issue by Sklar et al.27 Here we focus on two reports that examined the impact of specific musculoskeletal system impairments on physical performance. We also briefly review CCSS reported prevalence of neurosensory, neurologic, endocrine, and cardiopulmonary system impairments that are likely to have immediate and potential future impact on physical performance.
Childhood cancer survivors have a documented risk of poor skeletal integrity with over 10% of survivors in the CCSS cohort reporting musculoskeletal problems.28 These include amputation,18,28 osteoporosis,28,29 major joint replacement,28 short stature,30,31 osteonecrosis (ON),32 and loss of lean muscle mass and strength.33–35 Two investigations, one that required the use of an additional questionnaire and one that invited a subset of the cohort to participate in a clinical evaluation, have taken advantage of the CCSS resource to more closely examine associations between musculoskeletal late effects and physical performance limitations.
The first article focused on CCSS cohort members who reported ON—also known as avascular necrosis, ischemic necrosis, or aseptic necrosis—a potentially serious complication of therapy that can limit physical performance both in daily activities and in the work place.32 Kadan-Lottick et al32 examined the prevalence of self-reported ON among 9,261 patients enrolled in CCSS, and compared this rate with the rate in a random sample of 2,872 siblings of survivors. Fifty-two cancer survivors reported ON in 78 joints, yielding 20-year cumulative incidence of 0.43% and an RR of 6.2 (95% CI, 2.3 to 17.2) compared with siblings (cumulative incidence of 0.03%), adjusted for age and sex. Of the 52 reported cases of ON in the CCSS cohort, 60% reported involvement of more than one joint. The most common sites of involvement in descending order were hips, shoulders, and knees. The 52 survivors with ON were further questioned regarding difficulty with daily living activities of walking inside, climbing stairs, rising from a chair, putting on pants, reaching into low cupboards, and opening containers. Difficulty with at least one of these activities was reported by 57%, and with at least two activities by 44%. Also, 33% reported difficulty while walking inside, and 41% reported pain at rest in the affected joints.
The second article focused on body composition and muscle strength, and their respective associations with physical performance.33 Ness et al33 evaluated lean body mass and muscle strength among 75 survivors of childhood ALL who were participants in the CCSS cohort. Dual energy X-ray absorptiometry scans were performed to evaluate body composition, and myometry was used to measure strength. Mobility was evaluated with the Timed Up and Go and 2-Minute Walk. Both male and female survivors had more body fat than same age and gender population norms (26.0% v 21.5% for males; 38.3% v 36% females). Quadriceps strength values were also less than same age and gender population norms (13% decrease among both males and females) and were associated with shorter walking distances on the 2-Minute Walk and longer time requirements on the Timed Up and Go.
Neurologic and neurosensory outcomes, including paralysis, poor coordination, poor balance, and tremor, have been documented among survivors of brain tumors, ALL, acute myeloid leukemia, and soft tissue sarcoma.22,24–26 Bodily pain15 and fatigue36 may also interfere with physical performance and are prevalent in 13% and 19%, respectively, of cohort members. Pulmonary dysfunction and cardiac abnormalities have also been documented in the CCSS cohort, and can emerge as problematic years after treatment has ended. Mertens et al37 evaluated the incidence of pulmonary conditions among CCSS survivors and indicated that even among individuals who had survived 5 years after diagnosis, rates of lung fibrosis, emphysema, and supplemental oxygen use continued to rise. Mody et al22 reported a 6.9-fold increased risk of cardiac conditions among ALL survivors when compared with siblings, and Ness et al33 reported lower than expected exercise capacity among 75 ALL survivors when estimated peak oxygen capacity was compared with same age and gender population normative values. Later onset of cardiac conditions has also been documented among acute myeloid leukemia,24 soft tissue sarcoma,26 and brain tumor survivors.29 Of particular concern is the elevated risk of stroke among survivors of brain tumor, leukemia, and lymphoma who received radiation.38,39 This neurovascular late effect has profound implications for both long-term neurologic function and for physical performance.
Associations between organ system impairments and physical performance, self-care abilities, routine activity participation, and attendance at work or school are listed in Table 2. These data were collected as part of the baseline questionnaire in 1995, and demonstrate that even among young adult survivors of childhood cancer, organ system dysfunction is associated with physical performance limitations.
Table 2.
Association Between Organ System Medical Late Effects and Physical Performance Limitations or Participation Restrictions Among All Members of the Childhood Cancer Survivor Survey Surveyed at Cohort Entry in 1995-1996
| Late Effect Impairment | Physical Performance Limitation |
Need Assistance With Self-Care Activities |
Need Assistance With Routine Household and Community Tasks |
Health Prevents School or Work Attendance |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Row (%) | Rate Ratio | 95% CI | Row (%) | Rate Ratio | 95% CI | Row (%) | Rate Ratio | 95% CI | Row (%) | Rate Ratio | 95% CI | |
| Musculoskeletal | ||||||||||||
| Yes | 42.9 | 1.9 | 1.7 to 2.0 | 5.8 | 1.8 | 1.4 to 2.2 | 14.8 | 1.9 | 1.6 to 2.2 | 15.1 | 1.3 | 1.2 to 1.6 |
| No | 16.9 | 2.5 | 5.6 | 7.1 | ||||||||
| Endocrine | ||||||||||||
| Yes | 25.9 | 1.2 | 1.1 to 1.3 | 6.0 | 1.8 | 1.4 to 2.3 | 12.4 | 1.6 | 1.4 to 1.9 | 13.2 | 1.4 | 1.2 to 1.6 |
| No | 18.2 | 2.2 | 5.3 | 6.7 | ||||||||
| Neurologic | ||||||||||||
| Yes | 30.5 | 2.0 | 1.9 to 2.2 | 5.9 | 7.6 | 5.5 to 10.6 | 13.1 | 5.7 | 4.6 to 6.9 | 15.6 | 5.3 | 4.5 to 6.4 |
| No | 11.6 | 0.6 | 1.8 | 2.3 | ||||||||
| Sensory | ||||||||||||
| Yes | 29.2 | 1.3 | 1.1 to 1.4 | 10.0 | 2.7 | 2.1 to 3.4 | 20.6 | 2.6 | 2.3 to 3.0 | 19.1 | 2.0 | 1.7 to 2.3 |
| No | 18.6 | 2.1 | 5.0 | 6.7 | ||||||||
| Pulmonary | ||||||||||||
| Yes | 36.5 | 1.4 | 1.3 to 1.6 | 4.8 | 1.1 | 0.8 to 1.4 | 10.3 | 1.0 | 0.8 to 1.2 | 15.1 | 1.2 | 1.1 to 1.4 |
| No | 17.6 | 2.6 | 6.2 | 7.1 | ||||||||
| Cardiac | ||||||||||||
| Yes | 34.3 | 1.4 | 1.3 to 1.6 | 5.4 | 1.5 | 1.2 to 1.9 | 12.4 | 1.5 | 1.3 to 1.7 | 16.4 | 1.6 | 1.4 to 1.9 |
| No | 16.3 | 2.3 | 5.3 | 6.0 | ||||||||
Personal and Demographic Factors That Influence Physical Performance Outcomes
The CCSS has also provided documentation about personal and demographic factors that may increase the risk for the development of physical performance limitations. In several CCSS manuscripts, females, compared with males, have demonstrated an increased risk for poor physical performance outcomes. On the baseline questionnaire, 15.5% of females and 9.9% of males reported activity limitations. In an ancillary questionnaire mailed later to only lower-extremity bone tumor survivors,18 29.2% of females, compared with 19.1% of males, scored below the 25th percentile on the TESS, a measure of physical disability. Additionally, on the 2003 follow-up questionnaire, females were 1.7 times more likely than males to report problems with physical function.15 These differences were all reported in age-adjusted models, and add to the overall evidence that female survivors of childhood cancer have a greater risk than male survivors for late effects, including physical disability.40
Several CCSS publications have also indicated that lower annual household incomes may on average be associated with poorer physical performance, although the data could not establish the temporal relation of this association. Hudson et al,14 using data from the baseline questionnaire, reported that those with annual household incomes of less than $20,000 were more likely than those with incomes of $20,000 or more to report activity limitations. This discrepancy continued at the 2003 follow-up questionnaire. Those survivors with annual household incomes of less than $20,000 per year were 1.8 times (range, 1.5 to 2.3) more likely to report poor physical function than those with annual household incomes of $20,000 or more.15 The direction of the association between annual household income and physical performance limitations is unclear. It is possible that those who come from less advantaged backgrounds may be more prone to long-term physical disability, because of their life situations make it difficult to get treatment for organ system impairments that predispose disability, or alternatively, that those who have physical performance limitations are less likely to be able to work and contribute to the annual household incomes of their families. We describe information from the CCSS that has explored the direction of the association in the second case below.
Educational, Economic, Social, Health Care, and Lifestyle Consequences of Physical Performance Limitations in the CCSS Cohort
Perhaps the most important consequence of a physical disability is that it has the potential to restrict participation in expected adult social roles among childhood cancer survivors, and, as in the general population, may result in lower levels of educational attainment, employment, marriage, insurability and access to health care. These associations have been documented in the CCSS cohort, as a whole and among specific diagnosis groups. The article by Gurney et al,41 also included in this special issue, is devoted to social adaptation, and covers this topic in detail. Briefly, in adjusted models, CCSS investigators reported that, overall, cohort members with physical performance limitations were 43% less likely to graduate from high school, 60% less likely to be employed, 18% less likely to be married, and 38% less likely to have an annual household income ≥ $20,00042 than those without physical performance limitations. Another group of CCSS investigators, in an analysis limited to rhabdomyosarcoma survivors only, reported that high school graduation rates were lower among those with performance limitation when compared with those without.21 These outcomes are similar to reports from the general population of individuals with physical disability. However, in another CCSS publication by Nathan et al,43 after adjusting for a host of sociodemographic factors including insurance status, survivors who reported poor physical health were 30% more likely to receive risk-based survivor-focused care that those who did not report poor physical health. This differs from reports in the general population, where persons with physical disability are less likely than those without to have access to needed health care services.
Lifestyle choices among childhood cancer survivors with physical disability have not been examined in great detail in the CCSS. CCSS data do suggest that there are some cancer survivors with increased risks for smoking, less than optimal levels of physical activity, and excessive alcohol consumption. Low income and less education were associated with increased risk of smoking44 and with an increased risk for an inactive lifestyle45 in this cohort and, as we have demonstrated, were also associated with physical performance limitations. A combination of any of these risk factors has the potential to increase an individual's risk for other poor outcomes like heart or lung disease, and perhaps second malignant neoplasms. Recently, Lown et al46 reported that among members of the CCSS, survivors with activity limitations were 1.3 times (95% CI, 1.1 to 1.5) more likely than those without activity limitations to report heavy drinking. This is concerning because heavy drinking has the potential to alter physical performance, both acutely and over time, placing survivors with physical performance limitations who abuse alcohol at risk for further physical disability and for injury.
CONCLUSION
This review of previous publications from CCSS data indicates that childhood cancer survivors are at increased risk for physical performance limitations when compared with the CCSS sibling cohort or the general population. This increased risk begins during or early after the treatment period and is likely to increase with age. Survivors whose surgical interventions, radiation therapies, or chemotherapeutic protocols damage body structures and/or interfere with organ system functions are at the greatest risk for subsequent physical disability. Among CCSS survivors treated between 1970 and 1986, brain tumor survivors, bone tumor survivors, and survivors of Hodgkin's disease appear to be at the greatest risk for physical performance limitations. Female sex and low socioeconomic status are also associated with a poorer outcome. This compilation of data from CCSS has important implications for the current cohort of adult survivors of childhood cancer as they age, and also for the upcoming cohort of childhood cancer survivors as they transition into adulthood and begin to pursue and attain adult roles in their family, society, and community.
The CCSS also offers access to a well-defined cohort of individuals willing to participate in research and likely amenable to interventions that will benefit health. Fortunately, as the literature on aging and adult chronic disease demonstrates,47 individuals with physical performance limitations will benefit from intervention services to restore lost organ system function, instruction in adaptive techniques to restore independent task performance, the provision of environmental adaptations to optimize participation, or from lifestyle interventions to optimize health and prevent further loss of physical function.
Footnotes
Supported by Grant No. CA 55727 (L.L.R., Principal Investigator), National Cancer Institute, Bethesda, MD, with additional support provided to St Jude Children's Research Hospital by American Lebanese Syrian Associated Charities.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Manuscript writing: Kirsten K. Ness, Melissa M. Hudson, Jill P. Ginsberg, Rajaram Nagarajan, Sue Kaste, Neyssa Marina, John Whitton, Leslie Robison, James Gurney
REFERENCES
- 1.World Health Organization. Towards a Common Language for Functioning, Disability, and Health. http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf.
- 2.US Census Bureau Housing and Household Economic Statistics Division. 2006 American Community Survey. Washington, DC: US Census Bureau; 2006. [Google Scholar]
- 3.National Organization on Disability. Key Indicators from the 2004 N.O.D./Harris Survey of Americans with Disabilities. http://www.nod.org/Resources/harris2004/harris2004_summ.doc.
- 4.Kroll T, Jones GC, Kehn M, et al. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: A qualitative inquiry. Health Soc Care Community. 2006;14:284–293. doi: 10.1111/j.1365-2524.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 5.Wei W, Findley PA, Sambamoorthi U. Disability and receipt of clinical preventive services among women. Women's Health Issues. 2006;16:286–296. doi: 10.1016/j.whi.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chevarley FM, Thierry JM, Gill CJ, et al. Health, preventive health care, and health care access among women with disabilities in the 1994-1995 National Health Interview Survey, Supplement on Disability. Women's Health Issues. 2006;16:297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Smeltzer SC. Preventive health screening for breast and cervical cancer and osteoporosis in women with physical disabilities. Fam Community Health. 2006;29:35S–43S. doi: 10.1097/00003727-200601001-00007. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Environmental barriers to health care among persons with disabilities: Los Angeles County, California, 2002-2003. MMWR Morb Mortal Wkly Rep. 2006;55:1300–1303. [PubMed] [Google Scholar]
- 9.Ephraim PL, MacKenzie EJ, Wegener ST, et al. Environmental barriers experienced by amputees: The Craig Hospital Inventory of Environmental Factors–Short Form. Arch Phys Med Rehabil. 2006;87:328–333. doi: 10.1016/j.apmr.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Iezzoni LI, Killeen MB, O'Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Serv Res. 2006;41:1258–1275. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ness KK, Mertens AC, Hudson MM, et al. Limitations on physical performance and daily activities among long-term survivors of childhood cancer. Ann Intern Med. 2005;143:639–647. doi: 10.7326/0003-4819-143-9-200511010-00007. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: US Department of Health and Human Services; 1993. [Google Scholar]
- 13.Centers for Disease Control and Prevention. National Health Interview Survey. Atlanta, GA: US Department of Human Health Services; 1993. [Google Scholar]
- 14.Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. JAMA. 2003;290:1583–1592. doi: 10.1001/jama.290.12.1583. [DOI] [PubMed] [Google Scholar]
- 15.Zeltzer LK, Lu Q, Leisenring W, et al. Psychosocial outcomes and health-related quality of life in adult childhood cancer survivors: A report from the Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev. 2008;17:435–446. doi: 10.1158/1055-9965.EPI-07-2541. [DOI] [PubMed] [Google Scholar]
- 16.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 17.Ware JE, Sherbourne CD. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: Quality Metric Incorporated; 2003. [Google Scholar]
- 18.Nagarajan R, Clohisy DR, Neglia JP, et al. Function and quality-of-life of survivors of pelvic and lower extremity osteosarcoma and Ewing's sarcoma: The Childhood Cancer Survivor Study. Br J Cancer. 2004;91:1858–1865. doi: 10.1038/sj.bjc.6602220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis AM, Wright JG, Williams JI, et al. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res. 1996;5:508–516. doi: 10.1007/BF00540024. [DOI] [PubMed] [Google Scholar]
- 20.Ferrell BR, Dow KH, Grant M. Measurement of the quality of life in cancer survivors. Qual Life Res. 1995;4:523–531. doi: 10.1007/BF00634747. [DOI] [PubMed] [Google Scholar]
- 21.Punyko JA, Gurney JG, Scott Baker K, et al. Physical impairment and social adaptation in adult survivors of childhood and adolescent rhabdomyosarcoma: A report from the Childhood Cancer Survivors Study. Psychooncology. 2006;16:26–37. doi: 10.1002/pon.1072. [DOI] [PubMed] [Google Scholar]
- 22.Mody R, Li S, Dover DC, et al. Twenty-five-year follow-up among survivors of childhood acute lymphoblastic leukemia: A report from the Childhood Cancer Survivor Study. Blood. 2008;111:5515–5523. doi: 10.1182/blood-2007-10-117150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nathan PC, Ness KK, Greenberg ML, et al. Health-related quality of life in adult survivors of childhood Wilms tumor or neuroblastoma: A report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2006;49:704–715. doi: 10.1002/pbc.20949. [DOI] [PubMed] [Google Scholar]
- 24.Mulrooney DA, Dover DC, Li S, et al. Twenty years of follow-up among survivors of childhood and young adult acute myeloid leukemia: A report from the Childhood Cancer Survivor Study. Cancer. 2008;112:2071–2079. doi: 10.1002/cncr.23405. [DOI] [PubMed] [Google Scholar]
- 25.Packer RJ, Gurney JG, Punyko JA, et al. Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: Childhood Cancer Survivor Study. J Clin Oncol. 2003;21:3255–3261. doi: 10.1200/JCO.2003.01.202. [DOI] [PubMed] [Google Scholar]
- 26.Punyko JA, Mertens AC, Gurney JG, et al. Long-term medical effects of childhood and adolescent rhabdomyosarcoma: A report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2005;44:643–653. doi: 10.1002/pbc.20310. [DOI] [PubMed] [Google Scholar]
- 27.Diller L, Chow EJ, Gurney JG, et al. Chronic disease in the Childhood Cancer Survivor Study cohort: A review of published findings. J Clin Oncol. 2009;27:2339–2355. doi: 10.1200/JCO.2008.21.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–1582. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 29.Gurney JG, Kadan-Lottick NS, Packer RJ, et al. Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer. 2003;97:663–673. doi: 10.1002/cncr.11095. [DOI] [PubMed] [Google Scholar]
- 30.Gurney JG, Ness KK, Stovall M, et al. Final height and body mass index among adult survivors of childhood brain cancer: Childhood Cancer Survivor Study. J Clin Endocrinol Metab. 2003;88:4731–4739. doi: 10.1210/jc.2003-030784. [DOI] [PubMed] [Google Scholar]
- 31.Chow EJ, Friedman DL, Yasui Y, et al. Decreased adult height in survivors of childhood acute lymphoblastic leukemia: A report from the Childhood Cancer Survivor Study. J Pediatr. 2007;150:370–375. doi: 10.1016/j.jpeds.2006.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kadan-Lottick NS, Dinu I, Wasilewski-Masker K, et al. Osteonecrosis in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2008;26:3038–3045. doi: 10.1200/JCO.2007.14.9088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ness KK, Baker KS, Dengel DR, et al. Body composition, muscle strength deficits and mobility limitations in adult survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2007;49:975–981. doi: 10.1002/pbc.21091. [DOI] [PubMed] [Google Scholar]
- 34.Meacham LR, Gurney JG, Mertens AC, et al. Body mass index in long-term adult survivors of childhood cancer: A report of the Childhood Cancer Survivor Study. Cancer. 2005;103:1730–1739. doi: 10.1002/cncr.20960. [DOI] [PubMed] [Google Scholar]
- 35.Gurney JG, Ness KK, Sibley SD, et al. Metabolic syndrome and growth hormone deficiency in adult survivors of childhood acute lymphoblastic leukemia. Cancer. 2006;107:1303–1312. doi: 10.1002/cncr.22120. [DOI] [PubMed] [Google Scholar]
- 36.Mulrooney DA, Ness KK, Neglia JP, et al. Fatigue and sleep disturbance in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study (CCSS) Sleep. 2008;31:271–281. doi: 10.1093/sleep/31.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mertens AC, Yasui Y, Liu Y, et al. Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer. 2002;95:2431–2441. doi: 10.1002/cncr.10978. [DOI] [PubMed] [Google Scholar]
- 38.Bowers DC, McNeil DE, Liu Y, et al. Stroke as a late treatment effect of Hodgkin's Disease: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2005;23:6508–6515. doi: 10.1200/JCO.2005.15.107. [DOI] [PubMed] [Google Scholar]
- 39.Bowers DC, Liu Y, Leisenring W, et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2006;24:5277–5282. doi: 10.1200/JCO.2006.07.2884. [DOI] [PubMed] [Google Scholar]
- 40.Armstrong GT, Sklar CA, Hudson MM, et al. Long-term health status among survivors of childhood cancer: Does sex matter? J Clin Oncol. 2007;25:4477–4489. doi: 10.1200/JCO.2007.11.2003. [DOI] [PubMed] [Google Scholar]
- 41.Gurney JG, Krull KR, Kadan-Lottick N, et al. Social outcomes in the Childhood Cancer Survivor Study cohort. J Clin Oncol. 2009;27:2390–2395. doi: 10.1200/JCO.2008.21.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ness KK, Gurney JG, Zeltzer LK, et al. The impact of limitations in physical, executive, and emotional function on health-related quality of life among adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Arch Phys Med Rehabil. 2008;89:128–136. doi: 10.1016/j.apmr.2007.08.123. [DOI] [PubMed] [Google Scholar]
- 43.Nathan PC, Greenberg ML, Ness KK, et al. Medical care in long-term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2008;26:4401–4409. doi: 10.1200/JCO.2008.16.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Emmons K, Li FP, Whitton J, et al. Predictors of smoking initiation and cessation among childhood cancer survivors: A report from the Childhood Cancer Survivor Study. J Clin Oncol. 2002;20:1608–1616. doi: 10.1200/JCO.2002.20.6.1608. [DOI] [PubMed] [Google Scholar]
- 45.Florin TA, Fryer GE, Miyoshi T, et al. Physical inactivity in adult survivors of childhood acute lymphoblastic leukemia: A report from the Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev. 2007;16:1356–1363. doi: 10.1158/1055-9965.EPI-07-0048. [DOI] [PubMed] [Google Scholar]
- 46.Lown EA, Goldsby R, Mertens AC, et al. Alcohol consumption patterns and risk factors among childhood cancer survivors compared to siblings and general population peers. Addiction. 2008;103:1139–1148. doi: 10.1111/j.1360-0443.2008.02242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barondess JA. Toward healthy aging: The preservation of health. J Am Geriatr Soc. 2008;56:145–148. doi: 10.1111/j.1532-5415.2007.01513.x. [DOI] [PubMed] [Google Scholar]