Abstract
Limited research exists regarding methods for reducing problem gambling. Problem gamblers (N=180) were randomly assigned to: assessment only control, 10 minutes of Brief Advice, 1 session of motivational enhancement therapy (MET), or 1 session of MET plus 3 sessions of cognitive-behavioral therapy (CBT). Gambling was assessed at baseline, 6 weeks later, and a 9-month follow-up. Relative to assessment only, Brief Advice was the only condition that significantly decreased gambling between baseline and week 6, and it was associated with clinically significant reductions in gambling at month 9. Between week 6 and month 9, MET+CBT evidenced significantly reduced gambling on one index compared to the control condition. These results suggest the efficacy of a very brief intervention for reducing gambling among problem and pathological gamblers not actively seeking gambling treatment.
Keywords: gambling, brief interventions, motivational enhancement therapy, cognitive-behavioral therapy, treatment efficacy
About 1% of the population suffers from pathological gambling (Gerstein et al., 1999; Petry, Stinson, & Grant, 2005; Shaffer, Hall, & Vander Bilt, 1999; Welte, Barnes, Wieczorek, Tidwell, & Parker, 2001), and even more prevalent is a sub-threshold condition referred to as problem gambling. Typically, those who endorse some diagnostic criteria, but not five required for a diagnosis, are classified as problem gamblers. Up to 5% of the general population (Gerstein et al., 1999; National Research Council [NRC], 1999; Shaffer et al., 1999; Welte et al., 2001), and even higher proportions of some populations such as substance abusers, suffer from gambling problems. However, few problem or pathological gamblers seek treatment. The National Epidemiological Survey of Alcohol and Related Conditions (Slutske, 2006) found that only 7-12% of pathological gamblers, typically the most severely affected, access treatment.
Evaluating interventions for non-treatment seeking gamblers is important because problem and pathological gambling are associated with financial problems, psychiatric distress, and poor health. Problem gamblers spend a median of about $400 per month on gambling, with pathological gamblers typically wagering $2,000 or more per month (Hodgins, Currie, el-Guebaly, 2001; Petry, 2003a; Petry et al., 2006). Psychiatric disorders occur at high rates among problem and pathological gamblers, including mood, anxiety and substance use disorders (Cunningham-Williams, Cottler, Compton, & Spitznagel, 1998; Petry et al., 2005). In addition, those with even mild to moderate gambling problems are more likely to suffer from physical disabilities and some medical problems than their non-problem gambling counterparts (Morasco et al., 2006; Morasco & Petry, 2006). Problem gamblers also utilize expensive medical services such as emergency room visits and inpatient hospitalization at high rates (Morasco et al., 2006).
Brief interventions are widely used in treating some behavioral disorders, and they are typically defined as therapies lasting between 10 minutes and up to 4 sessions. They may be as simple as brief advice from a physician about adverse consequences of a behavior, such as heavy alcohol consumption or smoking. An extensive literature suggests that brief interventions are more effective than no treatment, and often as effective as more extended treatment, in reducing alcohol use (Babor, 1994; Bien, Miller, & Tonigan, 1993; Miller et al., 1995). Such interventions are especially efficacious and cost-effective for patients with less severe forms of a disorder, i.e., problem drinkers rather than dependent patients (Babor, 1994; Bertholet, Daeppen, Wietlisbach, Fleming, & Burnand, 2005; Cuijpers, Riper, & Lemmers, 2004). Their benefits have been extended to other conditions such as reducing onset of major depression and improving quality of life in those with sub-threshold depression (Willemse, Smit, Cuijpers, & Tiemens, 2004). Brief interventions may be particularly useful for those who do not specifically seek therapy for a disorder, and they have advantages of being low cost and widely applicable.
Motivational enhancement therapy (MET) is another brief intervention, based upon the transtheoretical model of change (Miller & Rollnick, 2002). This intervention presumes ambivalence about changing behaviors such as drinking or gambling, and encourages individuals to identify pros and cons of altering behavior. Hodgins and colleagues (2001) adapted MET for gambling and randomly assigned 102 individuals with at least moderate gambling problems to a cognitive-behaviorally based workbook only, the same workbook plus a telephone MET intervention, or a waitlist control condition. One month after the baseline evaluation, all groups decreased gambling relative to pre-treatment rates. A significant beneficial effect of the workbook plus MET condition was noted compared to the waitlist group on amounts wagered, but the workbook only condition did not differ from the waitlist control. In a 24-month follow-up, Hodgins, Currie, el-Guebaly, and Peden (2004) noted that the workbook plus MET group had lower SOGS scores and gambled less than those in the workbook only condition.
The workbook in Hodgins et al.'s (2001) study used cognitive-behavioral therapy (CBT). CBT views symptoms of psychological disorders as learned behavior patterns that constitute a maladaptive way of coping. These patterns can be altered via cognitive restructuring and behavior modification. CBT for substance use disorders teaches patients to identify and cope with situations that put them at risk for relapse (Kadden, Litt, Cooney, & Busher, 1992; Marlatt & Gordon, 1985). CBT may be particularly promising because of the potential of delayed effects. Studies in substance use disorder populations find beneficial effects of CBT emerge in longer-term follow-ups, even though CBT may be equally efficacious to other interventions in the short-term (Carroll et al., 1994; O'Malley et al., 1996). In the Hodgins et al. (2001) study of CBT for problem gamblers, participants assigned to the waitlist condition received treatment a month after randomization, so long-term benefits of the CBT workbook could not be determined.
Several independent groups described (Blaszczynski & Silove, 1995; Lopez-Viets & Miller, 1997; Petry, 2005a; Sharpe, 2002; Whelan, Steinbergh, & Meyers, 2007) and reported on the efficacy of CBT for pathological gambling (Echeburúa, Baez, & Fernandez-Montalvo, 1996, Echeburúa, Fernandez-Montalvo, & Baez, 2000; Ladouceur et al., 2001, 2003; Petry et al., 2006; Sylvain, Ladouceur, & Boisvert, 1997). Further, case reports detail combinations of MET and CBT for gamblers (e.g., Wulfert, Blanchard, & Martell, 2003).
In this study, we evaluated the efficacy of three brief interventions. A Brief Advice condition incorporated some aspects of motivational interviewing, including providing personalized feedback about one's gambling along with simple strategies for decreasing it. One session of MET was another condition; it addressed pros and cons of gambling and elicited change statements. A four-session intervention that combined MET and CBT was also evaluated. The initial session was identical to that provided in MET condition, and the three sessions of CBT were based on those described by Monti and colleagues (2002) and modified by Petry (2005a). Sessions focused on developing skills to promote alternatives for managing high-risk gambling situations and moods.
Each of the three interventions was compared to an assessment only control condition, as is recommended in initial stages of therapy development for conditions with no known efficacious intervention (Rounsaville, Carroll, & Onken, 2001). Analyses were conducted first over the short-term (baseline to week 6), and second throughout the rest of the study period (week 6 to month 9). We hypothesized that each condition would reduce gambling and related problems over the short term. Given prior evidence of a delayed effect of CBT, we expected that the MET+CBT condition may continue decreasing gambling throughout the follow-up period. Potential prognostic factors associated with clinically significant reductions in gambling at the long-term follow-up were also investigated, including pretreatment severity of gambling problems, psychiatric symptoms, substance abuse, and medical problems.
Method
Participants
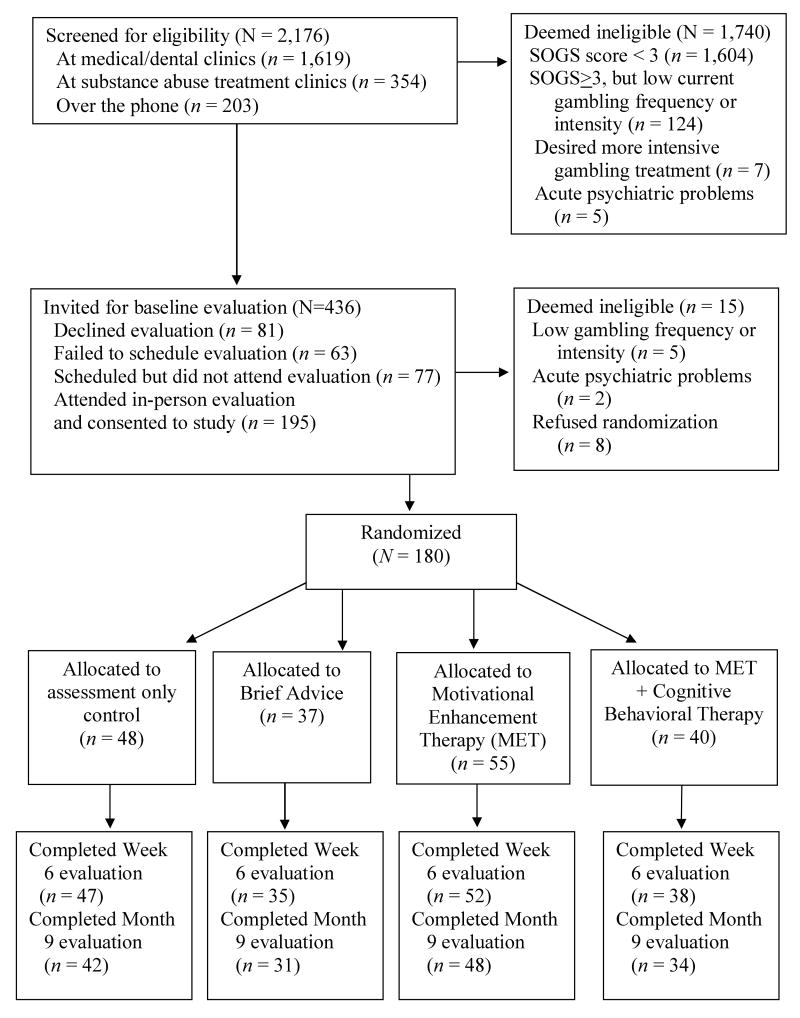
Participants were recruited via screening efforts primarily at substance abuse treatment clinics, medical clinics that serve the underprivileged, and flyers placed at locations between 1999 and 20051. A brief screen consisting of demographic items, recent gambling activities, and the South Oaks Gambling Screen (SOGS; Lesiuer & Blume, 1987) was administered to all individuals in waiting rooms when screeners were present, or over the phone for those who called in response to flyers. Individuals who endorsed at least 3 items on the SOGS, spent at least $100 wagering and had gambled on at least 4 occasions in the past 2 months, and were 18 years or older were invited to participate in the full evaluation, before which written informed consent, approved by the University's Institutional Review Board, was obtained. Exclusion criteria were reading level below 5th grade, past month suicidal intentions or psychotic symptoms, or interest in receiving more intensive gambling treatment than provided in the study. The consent form clearly indicated that participants would be randomly assigned to one of four conditions, one of which involved assessment only. All potential participants were asked if they wanted to be ensured gambling treatment before randomization, and such individuals were referred to a gambling treatment program. Figure 1 shows flow of participants through the protocol; 180 participants were eligible and randomized to a treatment condition.
Figure 1.
Flow of participants through study protocol.
Assessments
Assessments were administered at baseline and 6 weeks and 9 months later. Participants received $20 in gift certificates for the baseline evaluation, which took about 45 minutes, and $15 for each of the follow-ups, which took about 20 minutes and could be done in person or by phone. Typically, the person who conducted the baseline evaluation also provided the therapy (if so assigned), but 11 research assistants shared responsibilities for administering follow-up evaluations, and the condition to which participants were assigned was not stated on the follow-up forms. Follow-up rates ranged from 83.8% to 97.9% in each condition at every post-baseline evaluation (see Figure 1). No differences in follow-up rates occurred across treatment groups, χ2(3) = 1.05, p = .79 for the week 6 evaluation and χ2(3) = 0.35, p = .95 for the month 9 evaluation. Some post-baseline data were available on all but 4 participants (2.2%).
At baseline only, the National Opinion Research Center DSM-IV Screen for Gambling Problems (NODS) assessed lifetime pathological gambling using DSM-IV criteria. The NODS identified 95% of treatment-seeking gamblers as pathological, and test-retest reliability is 0.99 (Gerstein et al., 1999; Hodgins, 2004). In the present sample, Cronbach's alpha was 0.88.
The Addiction Severity Index (ASI; McLellan et al., 1988) evaluated problems at baseline and follow-up in seven domains commonly affected by addictive disorders, including medical, employment, alcohol, drug, legal, family/social and psychiatric. Scores range from 0 to 1.0, with higher scores reflecting more severe problems. Psychometric properties are established in substance abusers (McLellan et al., 1988), general medical patients (Weisner, McLellan, & Hunkeler, 2000) and pathological gamblers (Petry, 2003b; Petry, 2007). The ASI has been adapted to include a gambling section that includes questions about dollars wagered (net expenditures) and days gambled in the past month; scoring methods are similar to ASI-drug scales (Lesieur & Blume, 1991; Petry 2003b). The ASI-Gambling (ASI-G) section has good internal consistency, test-retest reliability and validity in assessing gambling problems and changes over time (Lesieur & Blume, 1991; Petry, 2003b; Petry, 2007). In 176 treatment-seeking gamblers (Petry et al., 2006), dollars wagered in the past month as determined by the ASI were highly correlated with collateral reports of amounts gambled (r =.68, p<.001). Cronbach's alpha in this sample was 0.73.
The SOGS (Lesieur & Blume, 1987) examined past-month gambling problems at baseline and through follow-up, with scores of 5 and higher indicating probable pathological gambling, and scores of 3 or higher considered problem gambling. SOGS scores are highly correlated with DSM criteria and other measures of gambling severity (Stinchfield, 2002; Hodgins, 2004). Gambling treatment studies have utilized SOGS scores as an outcome measure (Hodgins et al., 2004; Petry et al., 2006), and Wulfert et al. (2005) found that shortening the time frame of assessment did not adversely impact psychometric properties. In this sample, Cronbach's alpha ranged from 0.86 to 0.88 across the three administration periods. Past-month SOGS scores correlated 0.72 with ASI-G scores at baseline, 0.73 at week 6, and 0.80 at month 9, all p values <.001.
The Brief Symptom Inventory (BSI; Derogatis, 1993) is a reliable and valid 53-item scale assessing past week psychiatric symptoms, and it was administered at baseline only to provide an overall index of psychiatric severity. A Global Index score is derived, with higher scores indicative of greater severity of symptoms.
The Treatment Service Review (TSR; McLellan et al., 1992) evaluated services received, including substance abuse, medical, and professional gambling treatment and self-help (Gamblers Anonymous, GA). Follow-up versions assessed services since the past evaluation.
Randomization to treatments
Participants selected from envelopes containing slips of paper indicating the treatment group to which they were randomly assigned. More envelopes were prepared than participants were randomized so sample sizes are not equal across groups. Sample size, at about 45 per group, was estimated from effect sizes of other gambling studies (Hodgins et al., 2001). No stratification variables were used, and blinding participants to conditions was not possible.
Interventions were provided at no cost, but participation in sessions was voluntary and no compensation was provided for attending them. Following treatment delivery (or after a description of follow-up procedures for those assigned to the assessment only control condition), all participants were instructed to contact research staff if gambling intensified or they desired additional gambling treatment, although none did so. No study-related adverse events occurred.
Assessment only control
After completing the baseline evaluation, research assistants informed participants assigned to the assessment only control condition that they would be re-contacted in 6 weeks and 9 months for follow-up evaluations.
Brief Advice
Participants assigned to this condition met with a research therapist immediately after the evaluation for about 10 minutes. Using a one page handout (available in Petry, 2005a), the research therapist described the participant's own level of gambling in relation to the general population, outlined risk factors for development of severe gambling problems, and provided four steps to curtail development of significant gambling problems. These steps included limiting amount of money spent gambling, reducing amount of time and days gambling, not viewing gambling as a way of making money, and spending time doing other activities.
MET
A 50-minute MET session was held after the baseline evaluation. Therapists initially provided personalized feedback about participants' gambling. Next, they explored with participants positive and negative consequences of gambling and discussed how gambling fit within their goals and values. Lastly, participants completed a change plan worksheet.
MET+CBT
Participants assigned to this condition also met with a research therapist after the baseline evaluation. They received the same MET session described above and were encouraged to return for three sessions of CBT in the subsequent weeks. CBT sessions involved (1) determining internal and external triggers of gambling, (2) discussing methods for coping with internal gambling triggers such as lonely, depressed or anxious moods, and (3) developing methods for coping with external gambling triggers, such as assertiveness training, and methods for coping with gambling cues or cravings. CBT session handouts were modified from those in Petry (2005a) to emphasize reductions in gambling, rather than abstinence, as the goal.
Therapists
Nine therapists (2 Bachelor level and 7 with Masters degrees) delivered each of the three forms of therapy. They received didactic training and close supervision of at least one case. Ongoing supervision consisted of regular review of therapy notes and audiotapes and case discussion. Using a modification of the Yale Adherence Competence Scale (Carroll et al., 2000), four individuals rated 37 randomly selected audiotapes for brief advice, MET, and CBT items on a 7-point likert scale (1 = none/poor, 3 = some/adequate, 7 = extensive/exceptional). An example of a Brief Advice item was: “To what extent did the therapist provide concrete recommendations for reducing gambling?” An example of an MET item was: “To what extent were the therapist's questions open-ended and reflective?” A CBT item included: “To what extent did the therapist attempt to teach, model, or rehearse specific coping skills (problem solving, coping with craving, social skills)?” Inter-rater reliability as assessed by the intraclass correlation coefficient was 0.82.
In Brief Advice sessions, means and standard deviations on Brief Advice items were 5.25±1.31 (reflecting average rankings of about “good/quite a bit”). In contrast, during Brief Advice sessions, average ratings on MET and CBT items were 1.00±0.00 and 1.05±0.13, respectively (reflecting average ratings of about “none/poor”). In MET sessions, MET adherence items were rated 5.07±1.16, versus 1.08±0.34 for Brief Advice items and 1.28±0.76 for CBT items. CBT sessions were rated as 3.32±1.32 for CBT items, 2.21±0.56 for MET items, and 1.00±0.00 for Brief Advice items. Thus, the therapies were distinguishable (p values <.05).
Data analysis
Analysis of variance and Chi-square tests examined baseline differences across groups. Non-normally distributed data were transformed, e.g., log transformations for dollars wagered.
Intent-to-treat analyses were conducted. The primary analytic strategy was random effect regression (Hedeker, 1993), which models slopes based upon actual time of assessments. Hierarchical linear model (HLM) analyses take into account whatever data are available for each participant, and all participants had at least baseline data available which are included in the analyses. The primary outcome was ASI-G scores. To provide a more intuitive account of gambling behavior, dollars wagered in the prior 30 days, as assessed by the ASI, was also evaluated as a secondary outcome measure. Days gambled is a less sensitive index to change, as gambling frequency varies markedly based on preferred forms of gambling (Petry, 2003c), and was found to be less sensitive to change than dollars gambled in another treatment study (Petry et al., 2006). Further, none of the interventions tested in this study were abstinence oriented due to the nature of the sample, who were not actively seeking gambling treatment.
Three contrasts were evaluated, and each compared an active intervention (Brief Advice, MET, or MET+CBT) to the assessment only condition. In each case, the intervention was assigned a weight of 1 and the control condition 0. Contrast by time analyses evaluated if groups differed over time. Analyses were conducted (a) from baseline through the 6-week evaluation, and (b) from week 6 throughout the 9-month period to assess any enduring effects.
As an indicator of clinically significant change (Jacobson & Truax, 1991), participants were classified into one of three categories based upon their post-treatment SOGS scores and dollars wagered: “Recovered” (SOGS<3 and a substantial decrease in dollars wagered of <30% baseline rates, one SD below the mean group change), “Improved” (SOGS<3 or substantial decrease in dollars gambled, but not both), or “Unchanged” (SOGS≥3 and small or no reduction in gambling amounts; there were no substantial increases in gambling from baseline to month 9). Mann Whitney U tests evaluated proportions of participants classified into these categories at week 6 and month 9, comparing each intervention to the assessment only condition.
Finally, logistic regressions evaluated variables associated with recovered/improved versus unchanged gambling status at month 9. Gender, age, and baseline BSI, SOGS, and ASI alcohol, drug and medical composite scores were entered in the first step. Gender was a dichotomous variable, and others were continuous. In Step 2, treatment condition was entered, with the control condition indicated as the reference category, to determine if any of the interventions increased the odds of recovered/improved status relative to the assessment only condition. Analyses were conducted including only follow-up completers and then repeated coding non-completers as gambling problematically. Significance was set at p < .05 two-tailed; all analyses other than HLM were conducted using SPSS for Windows.
Results
Sample description and treatment participation
Baseline indices are shown in Table 1. Groups did not differ significantly on any demographic characteristic or measures of gambling or gambling problem severity at baseline.
Table 1. Demographic and baseline characteristics.
| Control | Brief Advice | MET | MET + CBT | Statistic (df) | p-value | |
|---|---|---|---|---|---|---|
| N | 48 | 37 | 55 | 40 | ||
| Age, mean (SD) | 41.4 (12.5) | 43.5 (14.4) | 45.0 (13.8) | 44.0 (10.2) | F(3,178)=0.69 | .56 |
| Female, No. (%) | 15 (31.3) | 19 (51.4) | 20 (36.4) | 18 (45.0) | χ2(3) = 4.23 | .24 |
| Ethnicity, No. (%) | χ2 (9) = 9.09 | .43 | ||||
| African American | 10 (21.7) | 6 (17.1) | 15 (27.8) | 10 (25.0) | ||
| European American | 28 (60.9) | 23 (65.7) | 35 (64.8) | 24 (60.0) | ||
| Hispanic American | 8 (17.4) | 6 (17.1) | 3 (5.6) | 4 (10.0) | ||
| Other | 0 | 0 | 1 (1.9) | 2 (5.0) | ||
| Marital Status, No. (%) | χ2 (9) = 10.66 | .30 | ||||
| Never Married | 21 (43.8) | 19 (51.4) | 20 (36.4) | 15 (37.5) | ||
| Married/Cohabitating | 19 (39.6) | 9 (24.3) | 14 (25.5) | 11 (27.5) | ||
| Divorced/Separated | 8 (16.7) | 7 (18.9) | 18 (32.7) | 13 (32.5) | ||
| Widowed | 0 | 2 (5.4) | 3 (5.5) | 1 (2.5) | ||
| Income, mean (SD), $ | 25,871 (43,000) | 23,583 (24,569) | 27,277 (27,260) | 31,552 (34,527) | F (3,178) = 0.37 | .78 |
| Education, mean (SD) | 12.5 (2.8) | 13.5 (2.5) | 13.8 (2.5) | 13.2 (2.0) | F (3,179) = 2.21 | .09 |
| Received in past month, No.(%) | ||||||
| Substance abuse treatment | 23 (47.9) | 16 (43.2) | 24 (43.6) | 20 (50.0) | χ2 (3) = 0.86 | .84 |
| Medical treatment | 25 (52.1) | 20 (54.1) | 28 (50.9) | 20 (50.0) | χ2 (3) = 0.15 | .99 |
| Addiction Severity Index Scores | ||||||
| Medical | .27 (.35) | .41 (.37) | .33 (.36) | .26 (.34) | F (3,179) = 1.57 | .20 |
| Employment | .55 (.39) | .52 (.36) | .53 (.36) | .54 (.39) | F (3,179) = 0.04 | .99 |
| Alcohol | .11 (.18) | .08 (.12) | .12 (.11) | .07 (.11) | F (3,179) = 1.16 | .33 |
| Drug | .04 (.06) | .03 (.05) | .03 (.06) | .05 (.08) | F (3,179) = 1.12 | .34 |
| Legal | .13 (.22) | .06 (.11) | .08 (.18) | .07 (.14) | F (3,179) = 1.24 | .30 |
| Family/social | .21 (.23) | .21 (.24) | .21 (.19) | .17 (.17) | F (3,179) = 0.46 | .71 |
| Psychiatric | .17 (.22) | .25 (.23) | .17 (.18) | .16 (.19) | F (3,179) = 1.57 | .20 |
| Brief Symptom Inventory | 1.8 (0.8) | 1.8 (0.7) | 1.6 (0.6) | 1.6 (0.6) | F (3,174) = 1.05 | .37 |
| NODS lifetime score | 5.2 (3.1) | 5.1 (3.1) | 5.5 (3.3) | 5.5 (2.5) | F (3,179) = 0.19 | .91 |
| Lifetime pathological gambler based on NODS, No (%) | 25 (52.1) | 23 (62.2) | 32 (58.2) | 28 (65.0) | χ2 (3) = 1.71 | .64 |
| SOGS past-month score | 8.9 (5.1) | 8.9 (4.7) | 9.2 (5.2) | 9.1 (4.2) | F (3,179) = 0.05 | .98 |
| Past-month probable pathological | 24 (50.0) | 19 (51.4) | 31 (56.4) | 21 (52.5) | χ2 (3) = 0.46 | .93 |
| Gambler, based on SOGS, No (%) | ||||||
| Days gambled in past month | 19.0 (10.6) | 17.5 (11.5) | 17.2 (10.1) | 16.3 (11.6) | F (3,179) = 0.48 | .70 |
| Dollars gambled in past month, Median (interquartile range) $ | 500 (1150) | 300 (800) | 440 (675) | 450 (550) | χ2 (3) = 7.09 | .07 |
| Preferred gambling, No. (%) | χ2 (15) = 15.11 | .44 | ||||
| Scratch/lottery | 21 (43.8) | 17 (45.9) | 23 (41.8) | 17 (42.5) | ||
| Slots machines | 7 (14.6) | 6 (16.2) | 12 (21.8) | 7 (17.5) | ||
| Cards | 13 (27.1) | 3 (8.1) | 8 (14.5) | 7 (17.5) | ||
| Sports | 6 (12.5) | 5 (13.5) | 5 (9.1) | 4 (10.0) | ||
| Dice | 1 (2.1) | 5 (13.5) | 4 (7.3) | 5 (12.5) | ||
| Other | 3 0 (0.0) | 8 1 (2.7) | 6 3 (5.5) | 7 0 (0.0) |
NODS=National Opinion Research Center DSM-IV Screen. SOGS=South Oaks Gambling Screen.
Numbers do not always add up to full sample size because of some missing variables.
All participants assigned to Brief Advice received it. Some participants assigned to MET (n = 3; 5.5%) and some assigned to MET+CBT (n = 5; 12.5%) scheduled their session for another day and failed to attend. In the MET+CBT condition, 13 (32.5%) attended all four sessions, while 3 (7.5%) came to three sessions, 5 (12.5%) to two, and 14 (35.0%) to only one (the initial MET session). Conservative intent-to-treat analyses were specified as interventions may not be particularly useful if only a minority of individuals receive them. Thus, all participants assigned to a condition were included in the analyses, regardless of their attendance.
Although no participants requested additional gambling treatment, review of the TSR at week 6 revealed that 3 participants (one from each of the 3 intervention conditions) received one professional gambling treatment session or attended between 1 and 2 GA meetings in addition to therapy received in the study. At month 9, one of these individuals (from the MET+CBT condition) attended another professional gambling treatment session outside of the study, and 5 others (one from the assessment only and two each from MET and MET+CBT conditions) received either professional gambling therapy (N = 1) or attended a GA meeting in the prior 7.5 months (N = 4). Because this level of involvement in non-study gambling treatment was low (<5%) and consistent across groups, all participants were included in the intent-to-treat analyses.
Effects of interventions on gambling
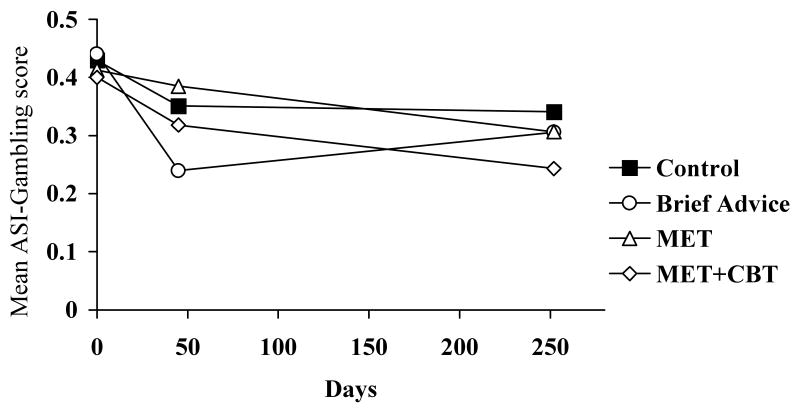
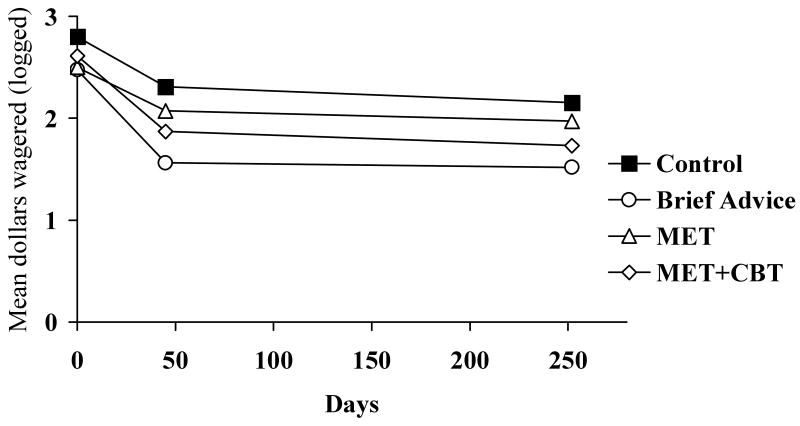
Table 2 shows gambling variables over time. Time effects, indicating general declines in gambling over time, were significant for ASI-G scores between baseline and week 6 (middle columns). The group by time interaction comparing the Brief Advice and control condition was significant between baseline and week 6. The Brief Advice condition evidenced significantly steeper slopes in reductions of ASI-G scores over time (Figure 2). Similar effects were noted with dollars wagered over time (Table 2; Figure 3). The other conditions showed similar declines in gambling as the assessment only condition between baseline and week 6.
Table 2. Gambling outcome measures and results from random regression models analyses.
| Outcome measures, raw means (SD) | Baseline through week 6, T, p-values | Week 6 through Month 9, T, p-values | |||||
|---|---|---|---|---|---|---|---|
| Variable | Baseline N=180 | Week 6 N=172 | Month 9 N=155 | Time | Group × time | Time | Group × time |
| ASI-Gambling | |||||||
| Control | 0.44 (0.21) | 0.34 (0.19) | 0.33 (0.24) | -2.49, p<.05 | 0.36, p=.72 | ||
| Brief Advice | 0.44 (0.24) | 0.31 (0.31) | 0.31 (0.27) | -2.40, p<.02 | 0.34, p=.74 | ||
| MET | 0.41 (0.22) | 0.39 (0.25) | 0.31 (0.24) | 1.10, p=.27 | -1.90, p=.06 | ||
| MET+CBT | 0.40 (0.18) | 0.32 (0.19) | 0.25 (0.17) | -0.08, p=.92 | -2.05, p<.05 | ||
| Dollars gambled | (logged) | ||||||
| Control | 2.8 (0.6) | 2.4 (1.0) | 2.1 (1.4) | -2.08, p<.05 | -0.28, p=.78 | ||
| Brief Advice | 2.5 (0.5) | 1.6 (1.4) | 1.5 (1.5) | -2.04, p<.05 | 0.43, p=.67 | ||
| MET | 2.5 (0.7) | 2.2 (1.2) | 2.0 (1.3) | 0.04, p=.97 | -0.02, p=.98 | ||
| MET+CBT | 2.6 (0.8) | 2.0 (1.0) | 1.8 (1.5) | -1.13, p=.19 | -0.34, p=.74 | ||
Note. ASI = Addiction Severity Index. MET = Motivational Enhancement Therapy. MET + CBT = Motivational Enhancement Therapy plus Cognitive-Behavioral Therapy.
Figure 2.
Addiction Severity Index (ASI) Gambling scores by days since randomization to a treatment condition. Values represent past-month measures and are estimates from random effects regression analyses, and as such do not always match raw means presented in Table 2. MET= Motivational Enhancement Therapy; CBT=Cognitive-Behavioral Therapy.
Figure 3.
Dollars wagered per month by days since randomization to a treatment condition. Values plotted are log transformed means. Values represent past-month measures and are estimates from random effects regression analyses, and as such do not always match raw means presented in Table 2. MET= Motivational Enhancement Therapy; CBT=Cognitive-Behavioral Therapy.
Table 2 also shows gambling indices between week 6 and month 9 (right columns). The Brief Advice condition evidenced no further changes compared to the assessment only condition, but both groups continued gambling at lower levels than baseline during this later assessment point (Figures 2-3). Compared with assessment only participants, the MET+CBT participants had a steeper slope with respect to declines in ASI-G scores between week 6 and month 9, but group by time effects were not significant for dollars wagered. In comparing the MET and control conditions, no significant group by time interactions emerged, although the group by time interaction for ASI-G scores approached significance between week 6 and month 9.
Clinically significant changes in problem gambling status
At week 6, the proportions (and numbers) of participants classified as “recovered” based on SOGS scores and dollars wagered were 4.3% (n = 2 of 47), 20.0% (n = 7 of 35), 11.5% (n = 6 of 52), and 2.6% (n = 1 of 38) in the assessment only, Brief Advice, MET, and MET+CBT conditions. The respective proportions (and n) “improved” were: 42.6% (20), 45.7% (16), 42.3% (22), and 47.4% (18). “Unchanged” participants constituted 53.7% (25), 34.3% (12), 46.2% (24), and 50.0% (19) in the groups. Only the Brief Advice group differed significantly from the assessment only control condition at week 6, U = 613.00, p <.03, effect size θ = .37.
By month 9, the proportions and number of participants who were “recovered” were 14.3% (6 of 42), 25.8% (8 of 31), 14.6% (7 of 48), and 20.6% (7 of 34) in the four respective groups. Proportions “improved” were 33.3% (14), 45.2% (14), 43.8% (21), and 38.2% (13). Those classified as unchanged from baseline to month 9 represented 52.4% (22), 29.0% (9), 41.7% (20), and 41.2% (14) of each group. Only Brief Advice differed significantly from the assessment only condition U = 485.00, p <.05, effect size θ = .37
Predictors of improvement at month 9
As shown in Table 3, logistic regression examined variables putatively associated with improved/recovered status at the 9-month follow-up. Step 1, with demographics and baseline severity scores included, was significant, χ2(df = 7, n = 1492) = 28.84, p <.001. Higher baseline SOGS scores and ASI-medical scores were significantly and inversely associated with the likelihood of improved/recovered status at month 9. The inclusion of group assignment in Step 2 was also significant, χ2(df = 3, n = 149) = 9.48, p<.05, and improved the overall model, χ2(df = 10, n = 149) = 38.32, p<.001, with 70.5% of the cases correctly identified. Baseline SOGS scores and baseline ASI-medical scores remained significant in the model. Relative to the assessment only group, the Brief Advice group had a significant positive relationship with improved/recovered status at month 9. The odds ratio (OR) of 6.08 indicates that those receiving Brief Advice had a 6-fold increased chance of being improved or recovered at month 9 relative to participants in the assessment only control condition. The MET and MET+CBT conditions did not significantly alter odds of being improved or recovered. Gender, age, severity of alcohol or drug problems, and psychological distress levels at baseline were all unrelated to this outcome.
Table 3. Logistic regression analysis predicting recovered/improved status at month 9 (N=149).
| Beta (Standard error) |
Wald | Significance | Odds ratio (95% Confidence interval) |
|
|---|---|---|---|---|
| Step 1 | ||||
| Female gender | -0.15 (0.38) | 0.16 | 0.70 | 0.86 (0.41-1.82) |
| Age | -0.01 (0.02) | 0.20 | 0.66 | 0.99 (0.96-1.03) |
| Baseline SOGS | -0.16 (0.05) | 9.87 | p<.01 | 0.85 (0.77-0.94) |
| ASI-medical | -1.03 (0.54) | 3.72 | 0.05 | 0.36 (0.13-1.02) |
| ASI-alcohol | 1.22 (1.50) | 0.66 | 0.42 | 3.38 (0.77-63.53) |
| ASI-drug | -2.83 (3.20) | 0.78 | 0.38 | 0.06 (0.96-31.46) |
| Brief Symptom Inventory | 0.00 (.31) | 0.00 | 0.99 | 1.00 (0.41-1.84) |
| Step 2 | ||||
| Female gender | -0.36 (0.41) | 0.80 | 0.37 | 0.70 (0.32-1.54) |
| Age | -0.01 (0.02) | 0.36 | 0.55 | 0.99 (0.96-1.02) |
| Baseline SOGS | -0.17 (0.05) | 10.50 | p<.001 | 0.84 (0.76-0.93) |
| ASI-medical | -1.28 (0.57) | 5.11 | p<0.05 | 0.28 (0.09-0.84) |
| ASI-alcohol | 1.61 (1.64) | 0.97 | 0.33 | 5.01 (0.20-124.09) |
| ASI-drug | -3.07 (3.36) | 0.83 | 0.36 | 0.05 (0.00-34.04) |
| Brief Symptom Inventory | -0.02 (0.33) | 0.00 | 0.96 | 1.02 (0.54-1.92) |
| Treatment group | 8.52 | p<.05 | ||
| Brief Advice | 1.81 (0.62) | 8.42 | p<.01 | 6.08 (1.80-20.57) |
| MET | 0.86 (0.51) | 2.85 | 0.09 | 2.37 (0.87-6.43) |
| MET+CBT | 0.78 (0.56) | 1.96 | 0.16 | 2.18 (0.73-6.49) |
Note. SOGS=South Oaks Gambling Screen; ASI=Addiction Severity Index; MET=Motivational Enhancement Therapy; CBT=Cognitive-behavioral Therapy.
If participants with missing data at Month 9 were coded as gambling problematically (n's = 6, 6, 7, and 6 in the four respective groups), results remained similar. The overall model was significant, χ2(df = 10, n = 174) = 31.22, p <.001, and again baseline SOGS scores (Wald = 8.04, p <.005; OR = 0.88, 95% CI = 0.81-0.96) and ASI-medical scores (Wald = 4.64, p <.05; OR = 0.31, 95% CI = 0.12-0.91) were significantly inversely associated with improved/recovered status, but not any other baseline characteristics. Only the Brief Advice condition was significantly associated with improved/recovered status compared to the control condition (Wald=4.52, p <.05), with OR of 2.97 (95% CI = 1.09-8.09) when all participants were included.
Discussion
Gambling decreased among the majority of participants in this study, even those who were assigned to the assessment only control condition. Significant time effects were noted with respect to ASI-G scores and dollars wagered. Reductions in gambling with no or minimal interventions have also been reported in pharmacological (Kim, Grant, Adson, & Shin; 2001; Grant et al., 2006) and other psychosocial treatment studies of gamblers (Hodgins et al., 2001; Petry et al., 2006). Decreases in gambling are reflected in epidemiological research as well. Lifetime rates of problem and pathological gambling are higher than past-year rates despite the fact that few problem or pathological gamblers report seeking treatment for gambling, suggesting that many individuals overcome gambling problems on their own (Slutske, 2006). Further, a longitudinal study of non-treatment seeking adults found that many problem gamblers were no longer experiencing problems 3-4 years later (Slutske, Jackson, & Sher, 2003).
Thus, multiple lines of evidence suggest that gambling problems wax and wane over time, without formal interventions. Motivation to change gambling behaviors may result in reductions in wagering prior to or during initial stages of treatment (Petry, 2005b). In the present study, participation in the baseline evaluation itself may have raised awareness of levels of gambling, which in turn may have increased participants' desires to reduce gambling involvement, regardless of which (or whether any) specific intervention was applied.
Although even assessment only participants decreased gambling, benefits of the Brief Advice condition emerged during the first 6 weeks after treatment. When clinically significant indicators classified participants by both SOGS scores and changes in amounts wagered, the Brief Advice condition differed significantly from the control condition at both week 6 and month 9. In the logistic regression analysis, having been assigned to the Brief Advice condition was significantly related to a substantial improvement or “recovered” status at the most distal follow-up, even after controlling for baseline characteristics and gambling severity. Thus, the Brief Advice condition evidenced consistent reductions across gambling outcomes.
In contrast to treatment of other disorders (Baer, Kivlahan, Blume, McKnight, & Marlatt, 2001; Carroll et al., 1994; Project Match Research Group, 1998), this study found few benefits of the other interventions. MET alone engendered no significant effects on any outcomes, although trends were noted with respect to reductions in ASI-G scores. Availability of the three CBT sessions led to significant improvements on ASI-G scores relative to the assessment condition between week 6 and month 9, and these effects were noted with a conservative intent-to-treat analysis. While MET+CBT did show improvements compared to the control condition on one domain, effects overall were less pronounced than those obtained with the Brief Advice.
Of the 40 participants assigned to MET+CBT, 19 did not receive any CBT. Limiting analyses to treatment attendees did not substantially alter results (data not shown, available from authors), perhaps in part because those who substantially reduced gambling after the baseline assessment may have had little desire to continue with more extended treatment.
Having lower SOGS scores and less severe medical problems at baseline were associated with greater likelihood of improved/recovered status at follow-up. It is not surprising that less severe gambling problems at baseline were related to less severe gambling problems 9 months later. Interestingly, those with greater medical problems at baseline were more likely to be gambling problematically 9 months later. Physical disability and medical problems have been linked to problem gambling in patients seeking medical treatment (Morasco & Petry, 2006; Pasternak & Fleming, 1999) and in epidemiological research (Morasco et al., 2006). The present results extend these findings, suggesting perhaps that different or more integrated and targeted interventions may be necessary to reduce problem gambling among individuals with poor physical health. In any case, the Brief Advice condition was efficacious in decreasing gambling, even after controlling for baseline health and problem gambling severity.
Prior studies demonstrate that psychiatric symptoms may interact with treatment outcomes, such that more psychiatrically impaired individuals do poorer in response to gambling treatment (Hodgins, Peden & Cassidy, 2005). Given the high rates of comorbidity between substance use and gambling disorders (Petry et al., 2005), controversy exists regarding whether specialized interventions are required for dually-diagnosed gamblers (Walker et al., 2006). However, in this study, severity of alcohol, drug and psychiatric problems at baseline were not associated with gambling problems at the follow-up, and nearly half of this sample was recruited from drug abuse treatment programs. Thus, reductions in gambling with Brief Advice occurred regardless of severity of baseline problems along these domains.
Strengths of this study include a large sample size, high follow-up rates, and application of intent-to-treat analyses. Many therapists provided the interventions, reducing the impact of any particular therapist on outcomes. Further, employing few exclusion criteria enhanced generalization of the findings. Study participants were not actively seeking treatment for gambling, making this sample similar to the majority of problem and pathological gamblers in the community, as very few individuals seek treatment for gambling. Both problem and pathological gamblers were included in the study, which is both a strength with respect to external validity, but also could be interpreted as a weakness as more extended therapies than those utilized herein may be necessary for those with more severe gambling problems. In any case, these results demonstrate that identifying and treating individuals via this Brief Advice can assist in decreasing problem gambling behaviors in a fairly large proportion of gamblers.
A limitation of the study was that therapist attention was not controlled across conditions, and interventions differed not only in contact time, but also content. However, this design was intentional, and all interventions were modeled after those with theoretical and empirical support in treatment of related behavioral disorders. Surprisingly few benefits of the more intensive intervention (MET+CBT) were noted, although more than half the participants assigned to this intervention did not receive the full treatment dose. Although adequate, therapists' competence in CBT delivery was ranked relatively lower than their delivery of the other interventions, and CBT is rarely designed for such a short-term intervention. Perhaps effects may have been stronger if more sessions were offered. Nevertheless, in the present study, the Brief Advice condition engendered benefits similar to those observed in other disorders (DeRubeis & Crits-Cristoph, 1998). Future studies may dismantle aspects of the Brief Advice condition to isolate whether personal feedback or specific advice suggestions brought about decreases in gambling.
Another weakness of this study is that it only evaluated gambling for 9 months following randomization. Changes in gambling behavior, either relapses or further reductions, may have occurred later. Additional benefits of MET+CBT may have been uncovered if longer time frames were evaluated. To minimize time burdens on participants, diagnoses of other psychiatric conditions were not made, but comorbidity was likely high (Petry et al., 2005). Nevertheless, baseline levels of psychiatric distress were not associated with outcomes in this study.
Across all treatment conditions, scratch and lottery tickets were the most popular form of gambling. In contrast, most treatment-seeking samples in North America prefer electronic gaming machines (e.g., Hodgins et al., 2001; Petry et al., 2006). These discrepancies may relate to differences in recruitment strategies or the focus on inner city clinics and non-gambling treatment seeking individuals, and the results can only be generalized to similar samples.
In addition, measures of gambling outcomes are debated (NRC, 1999; Walker et al., 2006). Several outcome measures were utilized in this study, and most showed some degree of concordance. While the present study did not include independent confirmation of gambling behaviors, other studies that have done so found high agreement between self- and collateral reports (Hodgins & Makarchuk, 2003; Petry, 2003a; Petry et al., 2006). If any biases are noted, they are in the direction of participants reporting more frequent and intense gambling than their collaterals are aware. While these self-report data are thought to be reliable and valid indicators of gambling, future studies may include objective or other independent reports of gambling.
As awareness of problem and pathological gambling grows (Shaffer & Korn, 2002), more providers are expressing interest in learning about assessment and treatment of gambling (National Council on Problem Gambling, 2003). Data from this study suggest that screening for gambling problems, especially in high-risk populations such as substance abusers and general medical patients, may uncover fairly high proportions of problem gamblers. A very brief and directive intervention may assist in reducing gambling problems in these individuals.
Acknowledgments
This study and preparation of this report were supported in part by the Patrick and Catherine Weldon Donaghue Medical Research Foundation and National Institutes of Health grants R01-MH60417, R01-MH60417-Supp, R01-DA021567, R01-DA13444, R01-DA018883, RO1-DA016855, T32-AA07290, P50-AA03510, P50-DA09241. We thank Yola Ammerman, Anne Doersch, Heather Gay, Cheryl Molina, Betsy Parker, Nicole Reilly, and Drs. Ronald Kadden and Karen Steinberg for assistance with this project.
Footnotes
Although the study was ongoing for over 5 years, the project was conducted on a part-time basis contingent upon staff availability, with no single person dedicated to screening and recruitment efforts. Hence, recruitment was intentionally slow.
Although 155 participants completed the 9-month follow-up evaluation, six participants had missing values on a baseline demographic characteristic or assessments (e.g., Brief Symptom Inventory) and therefore, were excluded from the logistic regression analysis.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/ccp/
References
- Babor TF. Avoiding the horrid and beastly sin of drunkenness: Does dissuasion make a difference? Journal of Consulting and Clinical Psychology. 1994;62:1127–1140. doi: 10.1037//0022-006x.62.6.1127. [DOI] [PubMed] [Google Scholar]
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Archives of Internal Medicine. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Blaszczynski A, Silove D. Cognitive and behavioral therapies for pathological gambling. Journal of Gambling Studies. 1995;11:195–220. doi: 10.1007/BF02107115. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence. Delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: A meta-analysis. Addiction. 2004;99:839–845. doi: 10.1111/j.1360-0443.2004.00778.x. [DOI] [PubMed] [Google Scholar]
- Cunningham-Williams RM, Cottler LB, Compton WM, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders--results from the St. Louis Epidemiologic Catchment Area Study. American Journal of Public Health. 1998;88:1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, Scoring, and Procedures Manual. Minneapolis: National Computer systems, Inc.; 1993. [Google Scholar]
- DeRubeis RJ, Crits-Christoph P. Empirically supported individual and group psychological treatments for adult mental disorders. Journal of Consulting and Clinical Psychology. 1998;66:37–52. doi: 10.1037//0022-006x.66.1.37. [DOI] [PubMed] [Google Scholar]
- Echeburua E, Baez C, Fernandez-Montalvo J. Comparative effectiveness of three therapeutic modalities in the psychological treatment of pathological gambling: Long-term outcome. Behavioural and Cognitive Psychotherapy. 1996;24:51. [Google Scholar]
- Echeburua E, Fernandez-Montalvo J, Baez C. Relapse prevention in the treatment of slot-machine pathological gambling: Long-term outcome. Behavior Therapy. 2000;31:351–364. [Google Scholar]
- Gerstein DR, Volberg RA, Toce MT, Harwood H, Johnson RA, Buie T, et al. Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission. National Opinion Research Center; University of Chicago, IL: 1999. [Google Scholar]
- Grant JE, Potenza MN, Hollander E, Cunningham-Williams R, Nurminen T, Smits G, et al. Multicenter investigation of the opioid antagonist nalmefene in the treatment of pathological gambling. American Journal of Psychiatry. 2006;163:303–312. doi: 10.1176/appi.ajp.163.2.303. [DOI] [PubMed] [Google Scholar]
- Hedeker DH. MIXREG: A fortran program for mixed-effects linear regression models. (Computer Program) Rockville, MD: NIMH Division of Services Research; 1993. [Google Scholar]
- Hodgins DC. Using the NORC DSM Screen for Gambling Problems as an outcome measure for pathological gambling: Psychometric evaluation. Addictive Behaviors. 2004;29:1685–1690. doi: 10.1016/j.addbeh.2004.03.017. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Makarchuk K. Trusting problem gamblers: Reliability and validity of self-reported gambling behavior. Psychology of Addictive Behaviors. 2003;17:244–248. doi: 10.1037/0893-164X.17.3.244. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, el-Guebaly N. Motivational enhancement and self-help treatments for problem gambling. Journal of Consulting and Clinical Psychology. 2001;69:50–57. doi: 10.1037//0022-006x.69.1.50. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie S, el-Guebaly N, Peden N. Brief motivational treatment for problem gambling: A 24-month follow-up. Psychology of Addictive Behaviors. 2004;18:293–296. doi: 10.1037/0893-164X.18.3.293. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Peden N, Cassidy E. The association between comorbidity and outcome in pathological gambling: A prospective follow-up of recent quitters. Journal of Gambling Studies. 2005;21:255–271. doi: 10.1007/s10899-005-3099-3. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Cooney NL, Busher DA. Relationship between role-play measures of coping skills and alcoholism treatment outcome. Addictive Behaviors. 1992;17:425–437. doi: 10.1016/0306-4603(92)90003-e. [DOI] [PubMed] [Google Scholar]
- Kim SW, Grant JE, Adson DE, Shin YC. Double-blind naltrexone and placebo comparison study in the treatment of pathological gambling. Biological Psychiatry. 2001;49:914–921. doi: 10.1016/s0006-3223(01)01079-4. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, Leblond J. Group therapy for pathological gamblers: A cognitive approach. Behaviour Research and Therapy. 2003;41:587–596. doi: 10.1016/s0005-7967(02)00036-0. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, Leblond J, et al. Cognitive treatment of pathological gambling. Journal of Nervous and Mental Disease. 2001;189:774–780. doi: 10.1097/00005053-200111000-00007. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. Evaluation of patients treated for pathological gambling in a combined alcohol, substance abuse and pathological gambling treatment unit using the Addiction Severity Index. British Journal of Addiction. 1991;86:1017–1028. doi: 10.1111/j.1360-0443.1991.tb01863.x. [DOI] [PubMed] [Google Scholar]
- Lopez-Viets VC, Miller WR. Treatment approaches for pathological gamblers. Clinical Psychology Review. 1997;17:689–702. doi: 10.1016/s0272-7358(97)00031-7. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford Press; 1985. [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O'Brien CP. A new measure of substance abuse treatment. Initial studies of the Treatment Services Review. Journal of Nervous and Mental Disease. 1992;180:101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, McGahan P, O'Brien CP. Guide to the Addiction Severity Index: Background, Administration, and Field Testing Results (US Publication No (ADM) 88-1419) Washington DC: U.S. Department of Health and Human Services; 1988. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Brown JM, Simpson TL, Handmaker NS, Bein TH, Luckie LF, et al. What works? A methodological analysis of the alcohol treatment outcome literature. In: Hester RK, editor. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 2nd. Boston, MA: Allyn & Bacon; 1995. pp. 12–44. [Google Scholar]
- Monti PM, Kadden R, Rohsenow DJ, Conney NL, Abrams DB. Treating alcohol dependence: A coping skills training guide. 2. New York: Guilford Press; 2002. [Google Scholar]
- Morasco BJ, Petry NM. Gambling problems and health functioning in individuals receiving disability. Disability and Rehabilitation. 2006;28:619–623. doi: 10.1080/09638280500242507. [DOI] [PubMed] [Google Scholar]
- Morasco BJ, Pietrzak RH, Blanco C, Grant BF, Hasin D, Petry NM. Health problems and medical utilization associated with gambling disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic Medicine. 2006;68:976–984. doi: 10.1097/01.psy.0000238466.76172.cd. [DOI] [PubMed] [Google Scholar]
- National Council on Problem Gambling. Counselor Search. Retrieved October 13, 2003 from http://www.ncpgambling.org/counselor_Search.asp.
- Pathological Gambling: A Critical Review. National Research Council; Washington, DC: National Academy Press; 1999. [Google Scholar]
- O'Malley SS, Jaffe AJ, Chang G, Rode S, Schottenfeld R, Meyer RE, et al. Six-month follow-up of naltrexone and psychotherapy for alcohol dependence. Archives of General Psychiatry. 1996;53:217–224. doi: 10.1001/archpsyc.1996.01830030039007. [DOI] [PubMed] [Google Scholar]
- Pasternak AV, Fleming MF. Prevalence of gambling disorders in a primary care setting. Archives of Family Medicine. 1999;8:515–520. doi: 10.1001/archfami.8.6.515. [DOI] [PubMed] [Google Scholar]
- Petry NM. Patterns and correlates of Gamblers Anonymous attendance in pathological gamblers seeking professional treatment. Addictive Behaviors. 2003a;28:1049–1062. doi: 10.1016/s0306-4603(02)00233-2. [DOI] [PubMed] [Google Scholar]
- Petry NM. Validity of a gambling scale for the Addiction Severity Index. Journal of Nervous and Mental Disease. 2003b;191:399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- Petry NM. A comparison of treatment-seeking pathological gamblers based on preferred gambling activity. Addiction. 2003c;98:645–655. doi: 10.1046/j.1360-0443.2003.00336.x. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological Gambling: Etiology, Comorbidity, and Treatments. Washington, DC: American Psychological Association Press; 2005a. [Google Scholar]
- Petry NM. Stages of change in treatment-seeking pathological gamblers. Journal of Consulting and Clinical Psychology. 2005b;73:312–322. doi: 10.1037/0022-006X.73.2.312. [DOI] [PubMed] [Google Scholar]
- Petry NM. Concurrent and predictive validity of the addiction severity index in pathological gamblers. American Journal on Addictions. 2007;16:272–282. doi: 10.1080/10550490701389849. [DOI] [PubMed] [Google Scholar]
- Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, et al. Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology. 2006;74:555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol, Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A Stage model of behavior therapies research: Getting started and moving on from stage 1. Clinical Psychology. 2001;8:133–142. [Google Scholar]
- Shaffer HJ, Korn DA. Gambling and related mental disorders: A public health analysis. Annual Review of Public Health. 2002;23:171–212. doi: 10.1146/annurev.publhealth.23.100901.140532. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health. 1999;89:1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe L. A reformulated cognitive-behavioral model of problem gambling. A biopsychosocial perspective. Clinical Psychology Review. 2002;22:1–25. doi: 10.1016/s0272-7358(00)00087-8. [DOI] [PubMed] [Google Scholar]
- Slutske WS. Natural recovery and treatment-seeking in pathological gambling: Results of two U.S. national surveys. American Journal of Psychiatry. 2006;163:297–302. doi: 10.1176/appi.ajp.163.2.297. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Jackson KM, Sher KJ. The natural history of problem gambling from age 18 to 29. Journal of Abnormal Psychology. 2003;112:263–274. doi: 10.1037/0021-843x.112.2.263. [DOI] [PubMed] [Google Scholar]
- Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addictive Behaviors. 2002;27:1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- Sylvain C, Ladouceur R, Boisvert JM. Cognitive and behavioral treatment of pathological gambling: A controlled study. Journal of Consulting and Clinical Psychology. 1997;65:727–732. doi: 10.1037//0022-006x.65.5.727. [DOI] [PubMed] [Google Scholar]
- Walker M, Toneatto T, Potenza MN, Petry N, Ladouceur R, Hodgins DC, et al. A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta Consensus. Addiction. 2006;101:504–511. doi: 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- Weisner C, McLellan AT, Hunkeler EM. Addiction Severity Index data from general membership and treatment samples of HMO members. One case of norming the ASI. Journal of Substance Abuse Treatment. 2000;19:103–109. doi: 10.1016/s0740-5472(99)00103-8. [DOI] [PubMed] [Google Scholar]
- Welte J, Barnes G, Wieczorek W, Tidwell MC, Parker J. Alcohol and gambling pathology among U.S. adults: Prevalence, demographic patterns and comorbidity. Journal of Studies on Alcohol. 2001;62:706–712. doi: 10.15288/jsa.2001.62.706. [DOI] [PubMed] [Google Scholar]
- Whelan JP, Steinberg TA, Meyers AW. Problem and Pathological Gambling: Advances in Psychotherapy - Evidenced-Based Practices. Vol. 8. Cambridge, MA: Hogrefe & Hunber; 2007. [Google Scholar]
- Willemse GR, Smit F, Cuijpers P, Tiemens BG. Minimal-contact psychotherapy for sub-threshold depression in primary care. Randomised trial. British Journal of Psychiatry. 2004;185:416–421. doi: 10.1192/bjp.185.5.416. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Hartley J, Lee M, Wang N, Franco C, Sodano R. Gambling screens: Does shortening the time frame affect their psychometric properties? Journal of Gambling Studies. 2005;21:521–536. doi: 10.1007/s10899-005-5561-7. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Blanchard EB, Martell R. Conceptualizing and treating pathological gambling: A motivationally enhanced cognitive behavioral approach. Cognitive and Behavioral Practice. 2003;10:61–72. [Google Scholar]