Abstract
Glucose homeostasis deficiency leads to a chronic increase in blood glucose concentration. In contrast to physiological glucose concentration, chronic superphysiological glucose concentration negatively affects a large number of organs and tissues. Glucose toxicity means a decrease in insulin secretion and an increase in insulin resistance due to chronic hyperglycemia. It is now generally accepted that glucose toxicity is involved in the worsening of diabetes by affecting the secretion of β-cells. Several mechanisms have been proposed to explain the adverse effects of hyperglycemia. It was found that persistent hyperglycemia caused the functional decline of neutrophils. Infection is thus the main problem resulting from glucose toxicity in the acute phase. In other words, continued hyperglycemia is a life-threatening risk factor, not only in the chronic but also the acute phase, and it becomes a risk factor for infection, particularly in the perioperative period.
Keywords: Glucose toxicity, Diabetes, Complication, Surgery, Surgical site infection, Emergency medicine, Critical care medicine
INTRODUCTION
Chronic hyperglycemia is a characteristic of the diabetic condition, while glucose toxicity is the main cause of diabetic complications, which are often observed only several years after the beginning of the illness[1]. Glucose toxicity, in its narrow sense, can indicate a clinical condition where control of diabetes in particular is poor, since hyperglycemia itself reduces the insulin secretion capacity of pancreatic β-cells, and the resultant increase in insulin resistance leads to further hyperglycemia. This vicious circle finally leads to the total incapacity of β-cells to secrete insulin[2,3].
On the other hand, acute hyperglycemia, similar to chronic hyperglycemia, is known to cause injury to many organs. Hyperglycemia in the acute phase causes the functional decline of neutrophils, and is a risk factor that causes infection in the perioperative period. In the first half of this review, we will present an introduction to the various mechanisms known to be involved in the control of glucose homeostasis and in the development of glucose toxicity. In the latter half, diabetic complications (chronic and acute) and implications for the fields of surgery, emergency and critical care medicine will be presented and discussed.
GLUCOSE HOMEOSTASIS
Glucose homeostasis is maintained by the highly coordinated interaction of three physiologic processes: insulin secretion, tissue glucose uptake and hepatic glucose production. In this way, the body tries to maintain a constant supply of glucose for cells by keeping glucose concentration in the blood constant. Normal glucose homeostasis represents the balance between intake (glucose absorption from the gut), tissue utilization (glycolysis, pentose phosphate pathway activity, tricarboxylic acid cycle activity, glycogen synthesis) and endogenous production (glycogenolysis and gluconeogenesis)[4]. The most important metabolic fuels are glucose and fatty acids. Glucose is preferentially used by brain and muscles, and to ensure a continuous supply of glucose to the brain and other tissues, metabolic fuels are stored for use in time of need. Glucose homeostasis is controlled primarily by the anabolic hormone insulin and also by some insulin-like growth factors[5]. Several catabolic hormones (glucagons, catecholamines, cortisol, growth hormone, and adrenocorticotropic hormone) may antagonize the action of insulin and are known as anti-insulin or counter-regulatory hormones[6].
It is often found that critically ill patients incur hyperglycemia because of insulin resistance even if it is not complicated by diabetes[7]. When severe stress occurs, insulin resistance and an insulin secretion decrease result from the response to stress by the neuroendocrine system because secretion of anti-insulin hormones is enhanced. This leads to enhancement of glucogenesis in the liver, of lipolysis in adipose tissue, and of protein catabolism in skeletal muscle. This is known as surgical diabetes. Patients with diabetes are more susceptible to stress and easily develop exacerbation of diabetes, resulting in an increase in the incidence of complications.
MECHANISM OF GLUCOSE TOXICITY
It has been found that oxidative stress is associated with the molecular mechanism of the decreased insulin biosynthesis and secretion, which is the main etiology of glucose toxicity. Because pancreatic islet cells show extremely weak manifestation of antioxidative enzymes[8,9], it is thought that the pancreas may be more susceptible to oxidative stress than other tissues and organs.
Pathway of oxidative stress production
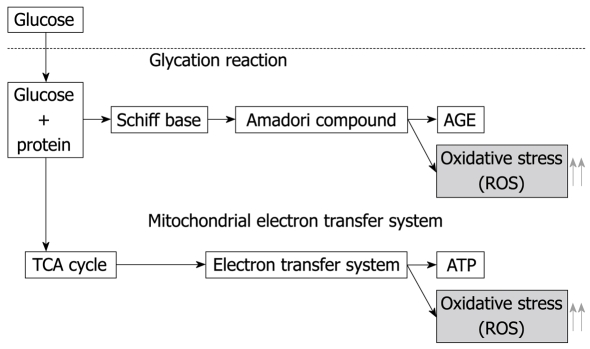
Metabolic reactions continuously produce reactive oxygen species (ROS), such as superoxides (O2-), hydroxyl radicals (OH-), peroxyl radicals (ROO-) or nitric oxide. ROS are involved in a diversity of biological phenomena, such as inflammation, carcinogenesis, aging, and atherosclerosis. However, several antioxidant enzymes help to maintain low levels of ROS. Oxidative stress corresponds to the overproduction of ROS that can damage cellular components, such as lipids, proteins or DNA[10]. There are strong indications that oxidative stress may be a key event in diabetic complications[11,12]. It is reported that 8-hydroxy-2-deoxyguanosine (8-OHdG), which is an indicator of oxidative damage of DNA, increases in patients with type 2 diabetes mellitus[13], and that 8-OHdG, 4-hydroxy-2-nonenal and heme oxygenase-1, all oxidative stress markers, increase in the pancreatic islet cells of type 2 diabetes mellitus animal models[14,15]. Generation of ROS in diabetes seems to be directly linked to chronic hyperglycemia. Various pathways are thought to be involved in the increase in oxidative stress in a hyperglycemic state (Figure 1). With the first pathway, more oxidative stress is caused by hyperglycemia because a non-enzymatic glycosylation reaction (glycation) is enhanced in the hyperglycemic state. ROS are then generated by the Amadori compound, which is an intermediate metabolite, before leading to the production of metabolites, known as advanced glycosylation end products (AGE) as the result of a glycation reaction[16]. Another pathway involves the mitochondrial electron transfer system, which also becomes a source of oxidative stress. This system is located in the mitochondrial inner membrane, where Adenosine tri-phosphate is produced as an important organic energy source. In this electron transfer system, water molecules are generated by deoxidation of four of the electrons of oxygen molecules, ROS is produced as an intermediate product in this process, and some of the ROS leak out from this system. Part of the oxygen used for this process is produced as superoxide anions even under physiological conditions, and their production increases in the hyperglycemic state[17]. Furthermore, the hexosamine pathway also becomes a source of oxidative stress. It was found that glucosamine, which is an intermediate metabolite in this process, also brings about oxidative stress[18]. Because this hexosamine pathway is enhanced in the diabetic state, the oxidative stress thus generated will increase.
Figure 1.
Increase in oxidative stress in the diabetic state. Acceleration of glycation response and the intramitochondrial electron transfer system was detected in the diabetic state, causing oxidative stress as the responses accelerated. Black arrows indicate pathway, grey arrows indicate increase or decrease. AGE: Advanced glycosylation end products; ROS: Reactive oxygen species; TCA cycle: Tricarboxylic acid cycle; ATP: Adenosine tri-phosphate.
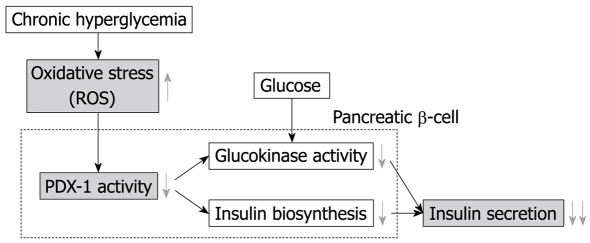
Reduction of insulin biosynthesis and secretion by oxidative stress
Figure 2 shows the mechanism of the reduction of insulin secretion by oxidative stress. It is known that biosynthesis of insulin decreases when pancreatic β-cells are exposed to chronic hyperglycemia in animal models of type 2 diabetes mellitus, and a similar phenomenon was induced by oxidative stress caused in the diabetic state. In other words, promoter activity of the insulin gene and mRNA expression decrease, and insulin gene expression is thus inhibited, when the β-cell line and isolated pancreatic islet cells are exposed to oxidative stress. It was also found that the DNA binding capacity of Pancreatic duodenal homeobox-1 (PDX-1), which is a very important transcription factor for insulin genes, decreases[18,19]. Finally, as for the control of glucokinase transcription by PDX-1, it is reported the promoter activity, manifestation, and the enzyme activity of glucokinase decreases with oxidative stress[20]. In fact, the use of antioxidant drugs resulted in an improvement of insulin secretion capacity as well as an increase in insulin mRNA expression[21]. On the other hand, it was also found that oxidative stress and activation of the c-Jun N-terminal kinase pathway are involved in a decline in insulin biosynthesis and secretion due to chronic hyperglycemia[22].
Figure 2.
The mechanism of insulin secretion reduction due to glucose toxicity. DNA binding capacity of PDX-1 decreases as a result of oxidative stress caused by hyperglycemia, while insulin biosynthesis and secretion also decrease. Black arrows indicate pathway, grey arrows indicate increase or decrease. PDX-1: Pancreatic duodenal homeobox-1.
Increase in insulin resistance caused by oxidative stress
Glucotoxicity not only affects the secretion of pancreatic hormones but also participates in insulin resistance of insulin-sensitive tissues, which include liver, skeletal muscle, and adipose tissue. Insulin resistance has been shown to be present before the onset of chronic hyperglycemia, although the latter may contribute to aggravation of the diabetic state by increasing insulin resistance[23].
Oxidative stress is also strongly suspected to be involved in chronic hyperglycemia-induced insulin resistance[24]. Indeed, it is known that incubation of primary adipocyte cells with chronic high glucose concentration can induce oxidative stress[25]. Moreover, it was demonstrated that oxidative stress induces insulin resistance in the 3T3-L1 adipocyte cell line by inhibiting the translocation of Glut 4 to the plasma membrane[26]. Finally, it was found that oxidative stress can induce insulin resistance in intact rat muscle[27].
GLUCOSE TOXICITY AND DIABETIC COMPLICATIONS
The prevalence of diabetes mellitus is increasing worldwide at an alarming rate due to population growth, obesity, sedentary life style and aging. Consequently, diabetic complications are also on the increase. Prevention and treatment of complications are considered to be most important for general care of diabetic patients. The basic causes of complications include tissue metabolism disorders caused by chronic hyperglycemia, which results in damage to many organs. The main diabetic complications are listed in Table 1. They are divided into chronic and acute complications based on the disease course.
Table 1.
Types of diabetic complications
| Chronic complications |
| Microvascular diseases: retinopathy, neuropathy, nephropathy |
| Macrovascular diseases: aortic sclerosis, stroke, myocardial infarction, angina pectoris, obstructive peripheral vascular disease, etc |
| Others: cataract, dermatopathy, hypertension, osteopenia, osteomalacia, arthropathy, soft tissue fibromatosis, etc |
| Acute complications |
| Diabetic coma: ketoacidotic coma, non-ketotic hyperosmolar coma, lactic acidosis |
| Acute infection: bacterial, mycotic, viral, etc |
Chronic complications
When metabolic disorders due to diabetes continue for many years, vascular tissue is affected the most. Chronic complications are divided into microvascular diseases that are specific to and common in diabetes and macrovascular diseases that are not specific but frequent and thus important for a prognosis. Vascular endothelial cell function in the blood vessels of diabetic patients is impaired, and many basic research endeavors have demonstrated that vasodilative reaction is also impaired[28,29]. Hyperglycemia-induced oxidative stress is also involved in the development of both macrovascular and microvascular diabetic complications[30].
Chronic hyperglycemia can induce microvascular complications such as retinopathy, neuropathy or nephropathy[31]. The retina is highly sensitive to oxidative stress since it has higher oxygen uptake and glucose oxidation than any other tissue[32]. Studies of diabetic rat retina and retinal cells incubated with a high-concentration of glucose have shown that the concentration of superoxides is elevated[33]. It has been demonstrated in animal models that oxidative stress is not only involved in the development of retinopathy but also in the persistence of the pathology after normalization of glucose concentration, probably as the result of persistent ROS[34]. Oxidative stress is also strongly suspected to be involved in the development of diabetic neuropathy[35]. Several studies have shown the capacity of antioxidant enzymes to prevent or reverse the toxic effect of chronic hyperglycemia in the nerves[36]. Moreover, oxidative stress may contribute to the pathogenesis of diabetic nephropathy since the presence of high concentrations of mitochondrial oxidative stress markers has been demonstrated in the urine and kidneys of diabetic rats[37].
Chronic hyperglycemia can also induce macrovascular complications. Cardiovascular complications are the most prevalent cause of death in diabetic patients. Moreover, it has been clearly shown that chronic hyperglycemia during diabetic and pre-diabetic states is linked to an increased risk for the development of cardiovascular diseases[38]. Long-term incubation of macrovessels with high-concentration glucose was found to strongly increase the risk of cardiovascular, cerebrovascular and peripheral arterial diseases[39]. Activation of protein kinase C by hyperglycemia is thought to play a central role in vascular complications since it leads to: (1) modification of contractile protein function, (2) an increase in the activity of nitric oxide synthase, and (3) activation of the angiotensin-converting enzyme (ACE). Activation of ACE has been linked with apoptosis and necrosis of cardiomyocytes and endothelial cells[40]. The importance of ACE in cardiovascular disease development was confirmed by studies showing the inhibition of ACE can protect against cardiovascular diseases[41]. Finally, protein glycation is another factor probably involved in the development of cardiovascular diseases[42].
Acute complications
Hyperglycemia can exacerbate a number of perioperative problems, including cardiac, neurologic, and infectious complications. In general, most outcomes tend to improve with treatment of hyperglycemia[43]. Diabetic coma is a form of consciousness disturbance that is characteristic of diabetes in acute complications. Diabetic coma has three categories, ketoacidotic coma due to hyperglycemia, non-ketotic hyperosmolar coma without ketoacidosis, and, rarely, lactic acidosis.
Infection in acute complications is a clinical condition that is not specific to but can easily become complicated in diabetic states. Diabetic patients have reduced immune function and enhanced bactericidal activity, so that special attention is required since the infection focus expands much faster than in non-diabetic patients. This becomes a problem particularly in the fields of surgery, emergency and critical care medicine.
Association between hyperglycemia and infection
It has been confirmed that perioperative appropriate glycemic control promotes wound healing. Perioperative infectious complications, including surgical site infection, represent serious postoperative complications. It is well known that, compared with non-diabetic patients, diabetic patients suffer from an increased incidence of perioperative infections, especially surgical site infection. It was reported that patients with preoperative elevation of HbA1c levels show a significantly higher incidence of surgical site infection than patients with normal HbA1c levels[44,45].
Recent basic researches have found that the functional decline of neutrophils is caused by a hyperglycemic state[46], and that the mechanism of this decline includes increased adhesive capacity and diminished chemotaxis, phagocytic activity and bactericidal capacity[47,48]. Neutrophilic function is reduced in proportion to an increase in the blood glucose level, and 200 mg/dL is assumed to be the threshold of neutrophil dysfunction. Furnary et al[49] reported that the incidence of deep sternal wound infection decreased from 2.0% to 0.8% in a patient group whose blood glucose level was kept below 200 mg/dL by insulin administration, and there are other reports of reduced infectious risk due to strict glycemic control[50]. Maintenance of a perioperative hyperglycemic state, since the stress response is a risk factor of postoperative infection, is extremely important for postoperative infection prophylaxis.
CONCLUSION
Several recent clinical studies have demonstrated the efficacy of strict glycemic control for reducing the mortality rate of post-operative or emergency patients[51-53]. It was thought that perioperative strict glycemic control was essential to relieve a perioperative inflammatory response and improve patient outcome. However, despite frequent blood glucose testing, it has been shown that intensive insulin therapy is sometimes difficult to perform when using sliding-scale manual insulin injection. Consequently, hypoglycemic events could not be avoided during intensive insulin therapy with intermittent blood glucose sampling. It has therefore been suggested that continuous blood glucose monitoring would be beneficial for maintaining target blood glucose levels[54,55]. We also believe that it is necessary to establish more accurate glycemic control methods because, in view of the global increase in diabetes, it is expected that glycemic control in surgical and emergency settings will become increasingly important.
Recently the usefulness of a closed-loop system (artificial endocrine pancreas), which provides continuous monitoring and strict control of blood glucose, was reported. STG-22™ (Nikkiso, Tokyo, Japan) is a novel artificial endocrine pancreas with a closed-loop glycemic control system that provides continuous blood glucose monitoring through a glucose sensor electrode and subsequent automatic insulin and glucose infusion to maintain appropriate blood glucose levels[54-57]. The usefulness of a closed-loop system providing continuous monitoring and strict control of post-operative blood glucose in patients after hepatic resection was also reported[58]. Accurate and continuous blood glucose monitoring and close glycemic control may be possible with an artificial endocrine pancreas. Establishment of a new perioperative blood glucose control method with the aid of an artificial endocrine pancreas is urgently needed.
Footnotes
Peer reviewer: Christa Buechler, PhD, Regensburg University Medical Center, Internal Medicine I, Franz Josef Strauss Allee 11, 93042 Regensburg, Germany
S- Editor Li LF L- Editor Lutze M E- Editor Zheng XM
References
- 1.Reusch JE. Diabetes, microvascular complications, and cardiovascular complications: what is it about glucose? J Clin Invest. 2003;112:986–988. doi: 10.1172/JCI19902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LeRoith D. Beta-cell dysfunction and insulin resistance in type 2 diabetes: role of metabolic and genetic abnormalities. Am J Med. 2002;113 Suppl 6A:3S–11S. doi: 10.1016/s0002-9343(02)01276-7. [DOI] [PubMed] [Google Scholar]
- 3.Dubois M, Vacher P, Roger B, Huyghe D, Vandewalle B, Kerr-Conte J, Pattou F, Moustaïd-Moussa N, Lang J. Glucotoxicity inhibits late steps of insulin exocytosis. Endocrinology. 2007;148:1605–1614. doi: 10.1210/en.2006-1022. [DOI] [PubMed] [Google Scholar]
- 4.Meyer C, Dostou JM, Welle SL, Gerich JE. Role of human liver, kidney, and skeletal muscle in postprandial glucose homeostasis. Am J Physiol Endocrinol Metab. 2002;282:E419–E427. doi: 10.1152/ajpendo.00032.2001. [DOI] [PubMed] [Google Scholar]
- 5.Dunger DB. Insulin and insulin-like growth factors in diabetes mellitus. Arch Dis Child. 1995;72:469–471. doi: 10.1136/adc.72.6.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerich JE, Campbell PJ. Overview of counterregulation and its abnormalities in diabetes mellitus and other conditions. Diabetes Metab Rev. 1988;4:93–111. doi: 10.1002/dmr.5610040202. [DOI] [PubMed] [Google Scholar]
- 7.Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478. doi: 10.4065/78.12.1471. [DOI] [PubMed] [Google Scholar]
- 8.Tiedge M, Lortz S, Drinkgern J, Lenzen S. Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes. 1997;46:1733–1742. doi: 10.2337/diab.46.11.1733. [DOI] [PubMed] [Google Scholar]
- 9.Robertson RP. Oxidative stress and impaired insulin secretion in type 2 diabetes. Curr Opin Pharmacol. 2006;6:615–619. doi: 10.1016/j.coph.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Vincent AM, Russell JW, Low P, Feldman EL. Oxidative stress in the pathogenesis of diabetic neuropathy. Endocr Rev. 2004;25:612–628. doi: 10.1210/er.2003-0019. [DOI] [PubMed] [Google Scholar]
- 11.Baynes JW, Thorpe SR. Role of oxidative stress in diabetic complications: a new perspective on an old paradigm. Diabetes. 1999;48:1–9. doi: 10.2337/diabetes.48.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Brunner Y, Schvartz D, Priego-Capote F, Couté Y, Sanchez JC. Glucotoxicity and pancreatic proteomics. J Proteomics. 2009;71:576–591. doi: 10.1016/j.jprot.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Dandona P, Thusu K, Cook S, Snyder B, Makowski J, Armstrong D, Nicotera T. Oxidative damage to DNA in diabetes mellitus. Lancet. 1996;347:444–445. doi: 10.1016/s0140-6736(96)90013-6. [DOI] [PubMed] [Google Scholar]
- 14.Ihara Y, Toyokuni S, Uchida K, Odaka H, Tanaka T, Ikeda H, Hiai H, Seino Y, Yamada Y. Hyperglycemia causes oxidative stress in pancreatic beta-cells of GK rats, a model of type 2 diabetes. Diabetes. 1999;48:927–932. doi: 10.2337/diabetes.48.4.927. [DOI] [PubMed] [Google Scholar]
- 15.Gorogawa S, Kajimoto Y, Umayahara Y, Kaneto H, Watada H, Kuroda A, Kawamori D, Yasuda T, Matsuhisa M, Yamasaki Y, et al. Probucol preserves pancreatic beta-cell function through reduction of oxidative stress in type 2 diabetes. Diabetes Res Clin Pract. 2002;57:1–10. doi: 10.1016/s0168-8227(02)00005-0. [DOI] [PubMed] [Google Scholar]
- 16.Kaneto H, Fujii J, Myint T, Miyazawa N, Islam KN, Kawasaki Y, Suzuki K, Nakamura M, Tatsumi H, Yamasaki Y, et al. Reducing sugars trigger oxidative modification and apoptosis in pancreatic beta-cells by provoking oxidative stress through the glycation reaction. Biochem J. 1996;320(Pt 3):855–863. doi: 10.1042/bj3200855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sakai K, Matsumoto K, Nishikawa T, Suefuji M, Nakamaru K, Hirashima Y, Kawashima J, Shirotani T, Ichinose K, Brownlee M, et al. Mitochondrial reactive oxygen species reduce insulin secretion by pancreatic beta-cells. Biochem Biophys Res Commun. 2003;300:216–222. doi: 10.1016/s0006-291x(02)02832-2. [DOI] [PubMed] [Google Scholar]
- 18.Kaneto H, Xu G, Song KH, Suzuma K, Bonner-Weir S, Sharma A, Weir GC. Activation of the hexosamine pathway leads to deterioration of pancreatic beta-cell function through the induction of oxidative stress. J Biol Chem. 2001;276:31099–31104. doi: 10.1074/jbc.M104115200. [DOI] [PubMed] [Google Scholar]
- 19.Matsuoka T, Kajimoto Y, Watada H, Kaneto H, Kishimoto M, Umayahara Y, Fujitani Y, Kamada T, Kawamori R, Yamasaki Y. Glycation-dependent, reactive oxygen species-mediated suppression of the insulin gene promoter activity in HIT cells. J Clin Invest. 1997;99:144–150. doi: 10.1172/JCI119126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kajimoto Y, Matsuoka T, Kaneto H, Watada H, Fujitani Y, Kishimoto M, Sakamoto K, Matsuhisa M, Kawamori R, Yamasaki Y, et al. Induction of glycation suppresses glucokinase gene expression in HIT-T15 cells. Diabetologia. 1999;42:1417–1424. doi: 10.1007/s001250051313. [DOI] [PubMed] [Google Scholar]
- 21.Del Guerra S, Lupi R, Marselli L, Masini M, Bugliani M, Sbrana S, Torri S, Pollera M, Boggi U, Mosca F, et al. Functional and molecular defects of pancreatic islets in human type 2 diabetes. Diabetes. 2005;54:727–735. doi: 10.2337/diabetes.54.3.727. [DOI] [PubMed] [Google Scholar]
- 22.Kawamori D, Kaneto H, Nakatani Y, Matsuoka TA, Matsuhisa M, Hori M, Yamasaki Y. The forkhead transcription factor Foxo1 bridges the JNK pathway and the transcription factor PDX-1 through its intracellular translocation. J Biol Chem. 2006;281:1091–1098. doi: 10.1074/jbc.M508510200. [DOI] [PubMed] [Google Scholar]
- 23.Zhao H, Yakar S, Gavrilova O, Sun H, Zhang Y, Kim H, Setser J, Jou W, LeRoith D. Phloridzin improves hyperglycemia but not hepatic insulin resistance in a transgenic mouse model of type 2 diabetes. Diabetes. 2004;53:2901–2909. doi: 10.2337/diabetes.53.11.2901. [DOI] [PubMed] [Google Scholar]
- 24.Eriksson JW. Metabolic stress in insulin's target cells leads to ROS accumulation - a hypothetical common pathway causing insulin resistance. FEBS Lett. 2007;581:3734–3742. doi: 10.1016/j.febslet.2007.06.044. [DOI] [PubMed] [Google Scholar]
- 25.Lu B, Ennis D, Lai R, Bogdanovic E, Nikolov R, Salamon L, Fantus C, Le-Tien H, Fantus IG. Enhanced sensitivity of insulin-resistant adipocytes to vanadate is associated with oxidative stress and decreased reduction of vanadate (+5) to vanadyl (+4) J Biol Chem. 2001;276:35589–35598. doi: 10.1074/jbc.M106783200. [DOI] [PubMed] [Google Scholar]
- 26.Rudich A, Tirosh A, Potashnik R, Hemi R, Kanety H, Bashan N. Prolonged oxidative stress impairs insulin-induced GLUT4 translocation in 3T3-L1 adipocytes. Diabetes. 1998;47:1562–1569. doi: 10.2337/diabetes.47.10.1562. [DOI] [PubMed] [Google Scholar]
- 27.Dokken BB, Saengsirisuwan V, Kim JS, Teachey MK, Henriksen EJ. Oxidative stress-induced insulin resistance in rat skeletal muscle: role of glycogen synthase kinase-3. Am J Physiol Endocrinol Metab. 2008;294:E615–E621. doi: 10.1152/ajpendo.00578.2007. [DOI] [PubMed] [Google Scholar]
- 28.Deedwania PC. Diabetes is a vascular disease: the role of endothelial dysfunction in pathophysiology of cardiovascular disease in diabetes. Cardiol Clin. 2004;22:505–509, v. doi: 10.1016/j.ccl.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Winer N, Sowers JR. Diabetes and arterial stiffening. Adv Cardiol. 2007;44:245–251. doi: 10.1159/000096745. [DOI] [PubMed] [Google Scholar]
- 30.King GL, Loeken MR. Hyperglycemia-induced oxidative stress in diabetic complications. Histochem Cell Biol. 2004;122:333–338. doi: 10.1007/s00418-004-0678-9. [DOI] [PubMed] [Google Scholar]
- 31.Yamagishi S, Imaizumi T. Diabetic vascular complications: pathophysiology, biochemical basis and potential therapeutic strategy. Curr Pharm Des. 2005;11:2279–2299. doi: 10.2174/1381612054367300. [DOI] [PubMed] [Google Scholar]
- 32.Kowluru RA, Chan PS. Oxidative stress and diabetic retinopathy. Exp Diabetes Res. 2007;2007:43603. doi: 10.1155/2007/43603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Du Y, Miller CM, Kern TS. Hyperglycemia increases mitochondrial superoxide in retina and retinal cells. Free Radic Biol Med. 2003;35:1491–1499. doi: 10.1016/j.freeradbiomed.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 34.Kowluru RA. Effect of reinstitution of good glycemic control on retinal oxidative stress and nitrative stress in diabetic rats. Diabetes. 2003;52:818–823. doi: 10.2337/diabetes.52.3.818. [DOI] [PubMed] [Google Scholar]
- 35.van Dam PS. Oxidative stress and diabetic neuropathy: pathophysiological mechanisms and treatment perspectives. Diabetes Metab Res Rev. 2002;18:176–184. doi: 10.1002/dmrr.287. [DOI] [PubMed] [Google Scholar]
- 36.Ametov AS, Barinov A, Dyck PJ, Hermann R, Kozlova N, Litchy WJ, Low PA, Nehrdich D, Novosadova M, O'Brien PC, et al. The sensory symptoms of diabetic polyneuropathy are improved with alpha-lipoic acid: the SYDNEY trial. Diabetes Care. 2003;26:770–776. doi: 10.2337/diacare.26.3.770. [DOI] [PubMed] [Google Scholar]
- 37.Prabhakar S, Starnes J, Shi S, Lonis B, Tran R. Diabetic nephropathy is associated with oxidative stress and decreased renal nitric oxide production. J Am Soc Nephrol. 2007;18:2945–2952. doi: 10.1681/ASN.2006080895. [DOI] [PubMed] [Google Scholar]
- 38.Grobbee DE. How to ADVANCE prevention of cardiovascular complications in type 2 diabetes. Metabolism. 2003;52:24–28. doi: 10.1016/s0026-0495(03)00214-2. [DOI] [PubMed] [Google Scholar]
- 39.Thompson CS. Animal models of diabetes mellitus: relevance to vascular complications. Curr Pharm Des. 2008;14:309–324. doi: 10.2174/138161208783497679. [DOI] [PubMed] [Google Scholar]
- 40.Díez J, Panizo A, Hernández M, Vega F, Sola I, Fortuño MA, Pardo J. Cardiomyocyte apoptosis and cardiac angiotensin-converting enzyme in spontaneously hypertensive rats. Hypertension. 1997;30:1029–1034. doi: 10.1161/01.hyp.30.5.1029. [DOI] [PubMed] [Google Scholar]
- 41.Kamalesh M. Heart failure in diabetes and related conditions. J Card Fail. 2007;13:861–873. doi: 10.1016/j.cardfail.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Misciagna G, De Michele G, Trevisan M. Non enzymatic glycated proteins in the blood and cardiovascular disease. Curr Pharm Des. 2007;13:3688–3695. doi: 10.2174/138161207783018545. [DOI] [PubMed] [Google Scholar]
- 43.Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27:553–591. doi: 10.2337/diacare.27.2.553. [DOI] [PubMed] [Google Scholar]
- 44.Dronge AS, Perkal MF, Kancir S, Concato J, Aslan M, Rosenthal RA. Long-term glycemic control and postoperative infectious complications. Arch Surg. 2006;141:375–380; discussion 380. doi: 10.1001/archsurg.141.4.375. [DOI] [PubMed] [Google Scholar]
- 45.Halkos ME, Puskas JD, Lattouf OM, Kilgo P, Kerendi F, Song HK, Guyton RA, Thourani VH. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136:631–640. doi: 10.1016/j.jtcvs.2008.02.091. [DOI] [PubMed] [Google Scholar]
- 46.Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S, Ohta S. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13:688–694. doi: 10.1038/nm1577. [DOI] [PubMed] [Google Scholar]
- 47.Nielson CP, Hindson DA. Inhibition of polymorphonuclear leukocyte respiratory burst by elevated glucose concentrations in vitro. Diabetes. 1989;38:1031–1035. doi: 10.2337/diab.38.8.1031. [DOI] [PubMed] [Google Scholar]
- 48.McManus LM, Bloodworth RC, Prihoda TJ, Blodgett JL, Pinckard RN. Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol. 2001;70:395–404. [PubMed] [Google Scholar]
- 49.Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg. 1999;67:352–360; discussion 360-362. doi: 10.1016/s0003-4975(99)00014-4. [DOI] [PubMed] [Google Scholar]
- 50.Zerr KJ, Furnary AP, Grunkemeier GL, Bookin S, Kanhere V, Starr A. Glucose control lowers the risk of wound infection in diabetics after open heart operations. Ann Thorac Surg. 1997;63:356–361. doi: 10.1016/s0003-4975(96)01044-2. [DOI] [PubMed] [Google Scholar]
- 51.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 52.Van den Berghe G, Wouters PJ, Bouillon R, Weekers F, Verwaest C, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P. Outcome benefit of intensive insulin therapy in the critically ill: Insulin dose versus glycemic control. Crit Care Med. 2003;31:359–366. doi: 10.1097/01.CCM.0000045568.12881.10. [DOI] [PubMed] [Google Scholar]
- 53.Finney SJ, Zekveld C, Elia A, Evans TW. Glucose control and mortality in critically ill patients. JAMA. 2003;290:2041–2047. doi: 10.1001/jama.290.15.2041. [DOI] [PubMed] [Google Scholar]
- 54.Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, Hanazaki K. The accuracy of a continuous blood glucose monitor during surgery. Anesth Analg. 2008;106:160–163, table of contents. doi: 10.1213/01.ane.0000296461.26492.3c. [DOI] [PubMed] [Google Scholar]
- 55.Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, Hanazaki K. Accuracy and reliability of continuous blood glucose monitor in post-surgical patients. Acta Anaesthesiol Scand. 2009;53:66–71. doi: 10.1111/j.1399-6576.2008.01799.x. [DOI] [PubMed] [Google Scholar]
- 56.Hanazaki K, Nosé Y, Brunicardi FC. Artificial endocrine pancreas. J Am Coll Surg. 2001;193:310–322. doi: 10.1016/s1072-7515(01)01014-6. [DOI] [PubMed] [Google Scholar]
- 57.Kono T, Hanazaki K, Yazawa K, Ashizawa S, Fisher WE, Wang XP, Nosé Y, Brunicardi FC. Pancreatic polypeptide administration reduces insulin requirements of artificial pancreas in pancreatectomized dogs. Artif Organs. 2005;29:83–87. doi: 10.1111/j.1525-1594.2004.29008.x. [DOI] [PubMed] [Google Scholar]
- 58.Okabayashi T, Hnazaki K, Nishimori I, Sugimoto T, Maeda H, Yatabe T, Dabanaka K, Kobayashi M, Yamashita K. Continuous post-operative blood glucose monitoring and control using a closed-loop system in patients undergoing hepatic resection. Dig Dis Sci. 2008;53:1405–1410. doi: 10.1007/s10620-007-0010-3. [DOI] [PubMed] [Google Scholar]