Abstract
Purpose of review
The elderly constitute a substantial and growing fraction of the end-stage renal disease (ESRD) population. We review recent studies on ESRD incidence, management, and outcomes in the elderly.
Recent findings
Rates of treated ESRD among the elderly (>80 years) have risen by more than 50% in the last decade. In studies with a large number of elderly patients, median survival after dialysis initiation is modest, and although a majority have reasonable life expectancy, a substantial minority of elderly patients experience very high early mortality rates after dialysis initiation. Quality of life results are mixed – compared with younger ESRD patients or non-ESRD elderly, mental well being is similar and physical well being is reduced in elderly patients with ESRD. In several studies, elderly patients with ESRD initiating peritoneal dialysis had higher mortality rates than elderly patients with ESRD initiating hemodialysis. Strategies such as nondialytic management of ESRD or dietary protein restriction and delayed dialysis initiation may be alternatives for elderly patients wishing to avoid dialysis initiation, but further studies are needed to determine the patients best suited for these approaches. Quality improvement initiatives in geriatric ESRD care have been successfully implemented in some centers and may ultimately improve care for elderly patients with ESRD.
Summary
These findings should help to clarify some of the risks and benefits of dialysis in the elderly and may be useful in dialysis decision-making and management.
Keywords: dialysis, elderly, end-stage renal disease
Introduction
The elderly constitute a substantial and growing fraction of the end-stage renal disease (ESRD) population in the United States and other industrialized nations [1–3]. According to recent data from the United States Renal Data System (USRDS), one in four patients starting dialysis in the United States is over the age of 75 [1]. As a group, the elderly have a higher prevalence of comorbidities which reduce life expectancy, impair informed decision-making, and potentially increase the burden of dialysis. However, the elderly are quite heterogeneous and they may also be subject to inappropriate restrictions on access to dialysis care solely on the basis of age (implicit rationing). Until recently, there was very little published data to guide management decisions for elderly patients with ESRD. This article critically reviews recent studies on ESRD incidence, management, and outcomes in the elderly.
Incidence
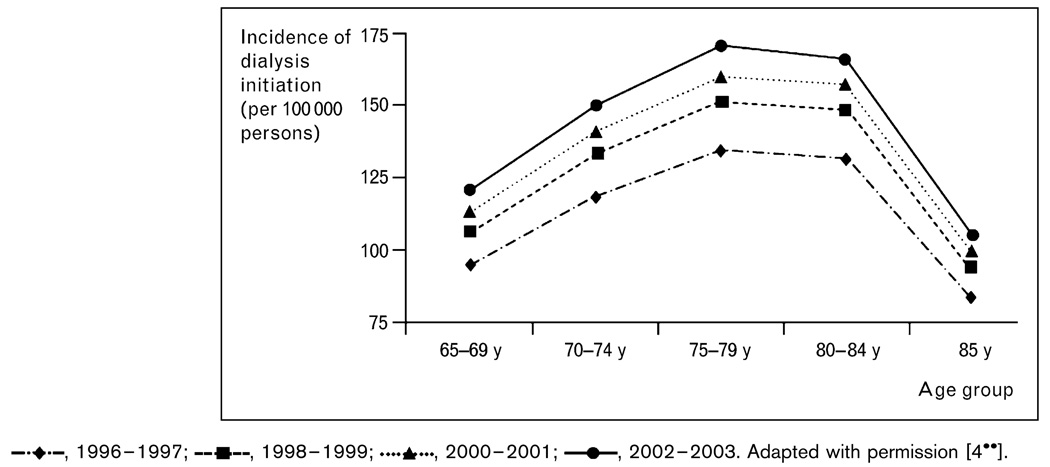
Based on estimates from the most recent USRDS Annual Data Report, the incidence of treated ESRD (i.e. dialysis initiation) is highest among those of at least 70 years, with incidence rates nearly three-fold higher than in the 50–59 age group [1]. Interestingly, when incidence rates among people in the over 70 age group are further subdivided into smaller age strata, treated ESRD incidence drops off markedly over the age of 85, most likely because of competing mortality risks and untreated ESRD (Fig. 1) [4••]. This implies that elderly patients with treated ESRD are highly selected; thus outcome data must be interpreted with this in mind.
Figure 1.
Incidence of dialysis initiation from 1996 to 2003 by year and age group (per 100 000 persons in US population), adjusted for sex and race
There is evidence that the incidence of treated ESRD among the very elderly has increased substantially over the last decade. Kurella et al. [4••] reported that, from 1996 to 2003, the incidence rate of dialysis initiation increased by 57% among people of at least 80 years of age in the United States. Previous studies, though not limited to the elderly [5,6], have suggested that factors such as rising chronic kidney disease (CKD) and diabetes prevalence and improved survival from cardiovascular disease do not explain the increase in ESRD incidence. Thus, it is likely that broader access to ESRD care and earlier initiation of dialysis explain the disproportionate increase in treated ESRD incidence among the very elderly. There is increasing interest in the role of acute kidney injury (AKI) as a contributor to the ESRD epidemic [7]. Elderly patients are at greater risk of AKI [8,9]; thus, the rising incidence of AKI together with improved survival from AKI episodes [10] may be another factor which in part explains the rising incidence of treated ESRD among the elderly. A recent meta-analysis of 17 AKI studies provides support for this hypothesis, demonstrating that patients of at least 65 years of age had a 28% higher risk for nonrecovery of kidney function following an episode of AKI than younger patients [11••].
A more subtle underlying issue that has not been explored is the degree to which time constraints, lack of training in palliative care, and financial incentives favoring dialysis care over palliative care might influence treatment choices. It will be interesting to see whether trends in treated ESRD incidence change over time if newly proposed reimbursement policies (HR 6331) supporting greater time for CKD education but also tying dialysis reimbursement to attainment of clinical performance measures are implemented [12]. One might expect these policies would restrain growth of the elderly ESRD population if reimbursement for CKD education provides greater incentive to delay dialysis initiation and provide education on treatment choices, while at the same time there may also be less incentive to accept elderly patients into dialysis programs if they are less likely to attain clinical performance targets such as fistula creation, nutritional status, or anemia management (though the elderly are probably more likely to attain other targets such as dialysis adequacy).
Survival after dialysis initiation and prognostic factors
In the United States, median survival after dialysis initiation is 15.6 months for patients 80–84 years of age, 11.6 months for patients 85–89 years of age, and 8.4 months for patients 90 years of age and older. The 1-year survival rate after dialysis initiation for all patients of at least 80 years is 54%; however, mortality is not constant over time and nearly 20% of patients die within the first 3 months after dialysis initiation (for comparison, 10% of patients of 65–79 years of age die within the first 3 months after dialysis initiation). Thus, whereas the majority of elderly patients experience a reasonable life expectancy on dialysis, a significant minority do not. Reasons for the high mortality rate in the first several months after dialysis initiation remain unclear, but may be related to severity of the underlying illness prompting dialysis initiation. Nevertheless, it raises several questions, including whether dialysis is life extending for these patients, whether early initiation of dialysis is beneficial, and whether high-risk patients can be identified prior to dialysis initiation.
Most studies of prognostic factors have been limited to patients starting dialysis. In addition to older age, several negative prognostic factors have been consistently identified in epidemiological studies, including reduced functional status [4••,13,14], low body weight [4••,14], number or severity of comorbidities [4••,13,15••], and late referral or unplanned dialysis initiation [13,14]. Risk stratification scores based on age, functional status, comorbidity, and planned versus unplanned dialysis initiation [13] or on body mass index, functional status, and early versus late referral [14] have been proposed for elderly patients and may be useful for communicating prognosis.
Dialysis versus nondialytic management of end-stage renal disease
Although USRDS and other national registry data provide useful information about survival among patients who start dialysis, they do not systematically track patients with ESRD who do not receive dialysis. Among studies which compared survival of elderly patients with ESRD receiving dialysis versus those receiving nondialytic management, patient characteristics, rates of dialysis initiation, and survival estimates vary considerably (Table 1) [14,15••,16–19,20••]. For example, rates of nondialytic management range from 20 to 60%, and 1-year survival rates among these patients range from 25 to 68%. These differences are likely due to regional differences in referral patterns, pooling of data from different eras, and nonuniform methods for determining the starting point for survival calculations between studies and within studies when comparing dialysis and nondialysis groups. Further, it should be noted that, in most of these studies, dialysis was initiated later in the course of CKD and median survival was longer than elderly ESRD patients receiving dialysis in the United States (Table 1), raising the question of whether more stringent criteria for acceptance into dialysis were applied in these cohorts (or, conversely, whether US dialysis programs are initiating dialysis in patients who would otherwise die from competing causes).
Table 1.
Comparison of studies evaluating different management strategies in elderly patients with end-stage renal disease
| Study | Type and year of study |
Country | Number of participants |
Mean age or age range (years) |
Nonwhite (%) |
Diabetes (%) |
Ischemic heart disease (%) |
12-month survival (%) |
Starting point for survival calculation* |
|---|---|---|---|---|---|---|---|---|---|
| Kurella et al. (USRDS) [4••] | Observational | USA | |||||||
| Dialysis | 1996–2003 | 83 996 | ≥80 | 21 | 30 | 35 | 54 | Start of dialysis, mean eGFR 10 | |
| Joly et al. [14] | Observational | France | |||||||
| Dialysis | 1989–2000 | 107 | 83 | 6 | 7 | 42 | 74 | Start of dialysis | |
| No dialysis | 37 | 84 | 14 | 22 | 49 | 29 | Date of decision not to start dialysis |
||
| Smith et al. [18] | Observational | UK | |||||||
| Dialysis | 1996–2000 | 258 | 59 | 19 | 27 | NA | ~90 | Start of dialysis | |
| No dialysis | 63 | 71 | 13 | 43 | ~25 | Date eGFR first <10–12 | |||
| Murtagh et al. [15••] | Observational | UK | Date eGFR first <15 | ||||||
| Dialysis | 2003–2004 | 52 | 80 | 19 | 25 | 33 | 84 | ||
| No dialysis | 77 | 83 | 16 | 23 | 39 | 68 | |||
| Wong et al. [19] | Observational | UK | |||||||
| No dialysis | 2003–2006 | 71 | 79 | NA | 28 | 34 | 65 | NA | |
| Brunori et al. [20••] | RCT | Italy | NA | eGFR 5–7 | |||||
| Early dialysis | 2000–2005 | 56 | 77 | 0 | 25 | 84 | |||
| Delayed dialysis + diet | 56 | 79 | 0 | 16 | 87 |
Characteristics of elderly end-stage renal disease patients in the United States are shown for comparison. eGFR, estimated glomerular filtration rate (in ml/min/1.73m2); NA, not available; RCT, randomized controlled trial; USRDS, United States Renal Data System.
Starting point for survival calculation indicates the date used for the start of survival calculations. In some studies, this is the date dialysis was started, and for other studies as indicated, this is the date that laboratory testing indicated an eGFR below a specific value.
Joly et al. [14] reported one of the first relatively large series comparing outcomes of elderly patients with a creatinine clearance less than 10 ml/min/1.73m2 choosing nondialytic management of ESRD versus those choosing dialysis. Of 144 patients of at least 80 years referred over a 12-year period, 74% were recommended dialysis and 26% were recommended nondialytic management, and few patients (<5%) changed therapy. In as-treated analyses, median survival was 20 months longer in the group choosing dialysis. Murtagh et al. [15••] reported results from 129 patients of at least 75 years with an estimated glomerular filtration rate (GFR) of 15 ml/min/1.73m2 or less. Forty percent of patients were recommended dialysis and 60% were recommended nondialytic management, and no patients changed therapy, although a substantial fraction in the dialysis group had not yet started dialysis by the end of the observation period. In intention to treat analyses, 1-year survival rates were 84% in the group choosing dialysis and 68% in the group choosing nondialytic management. However, among those with high comorbidity or among those with ischemic heart disease, survival did not differ between groups choosing dialysis and nondialytic management. Smith et al. [18] noted similar results in a study of 328 patients with advanced CKD. Although there were large differences in survival between those choosing dialysis versus nondialytic management, there was no difference in survival of those who were recommended nondialytic management but ultimately choosing to receive dialysis compared with those receiving nondialytic management [18]. These findings seem to support the idea that there is a group of patients with ESRD who may not benefit from dialysis, but, in the absence of large prospective studies, identifying these patients remains difficult.
Dietary protein restriction and delayed initiation of dialysis
Given uncertainty regarding the optimal GFR at which to start dialysis [21] and concern for potential adverse consequences (such as catheter infections, loss of residual renal function) and known increased costs associated with early dialysis initiation, Brunori et al. [20••] investigated the safety of delayed initiation of dialysis when combined with a supplemented very low protein diet (‘diet arm’) versus immediate dialysis initiation (‘dialysis arm’) in 112 individuals of more than 70 years of age with an estimated GFR of 5–7 ml/min/1.73m2. Those with diabetes, heart failure, pulmonary disease, cancer, liver disease, or an acute life-threatening illness were excluded. Participants in the diet arm received nutritional counseling to follow a vegan diet with a caloric intake of 35 kcal/kg and protein intake of 0.3 g/kg, supplemented with keto-analogues, amino acids, and vitamins. Dialysis was initiated in the diet arm for signs or symptoms of uremia, including fluid overload, uncontrolled hypertension, hyperkalemia, malnutrition, or nausea. The study was designed to test the noninferiority of diet versus dialysis over 12 months of follow-up. Seventy-one percent of participants in the diet arm initiated dialysis after an average of 10.7 months. In intention to treat analyses, 1-year survival rates were 83.7% [95% confidence interval (CI) 74.5–94.0] in the dialysis arm and 87.3% (95% CI 78.9–96.5) in the diet arm. In analyses correcting for an imbalance in randomization as well as in as-treated analyses, the differences between diet and dialysis were accentuated in favor of the diet arm. Hospitalization rates and hospital days were lower in the diet arm, though hospitalization for fluid overload occurred more commonly in the diet arm. Furthermore, there was no evidence for malnutrition in the diet arm, either by loss of body weight or decline in serum albumin concentration. There are limitations of this study, including the potential for bias because the intervention was not blinded [22]. It is also unclear whether these results could be generalized to sicker patients, especially those with heart failure, and whether the dietary recommendations could be followed in ‘real world’ settings or among the 30–40% of ESRD patients who have diabetes. Nevertheless, if confirmed these provocative findings could help elderly patients safely postpone the need for dialysis.
Quality of life
Quality of life concerns play an important role in treatment decisions among elderly patients. Two studies suggest that, although physical well being is reduced in elderly dialysis patients, mental well being is comparable to younger dialysis patients and to the age-matched general population. In cross-sectional analyses from the North Thames Dialysis Study, Lamping et al. [23] reported that elderly patients (≥70 years) on dialysis had lower SF-36 Physical Component Scores (PCS) but similar Mental Component Scores (MCS) to similarly aged persons in the general UK and US population. Unruh et al. [24•] recently studied changes in several dimensions of quality of life over time among elderly (≥70 years) versus nonelderly hemodialysis patients participating in the hemodialysis (HEMO) study, a randomized trial of dialysis dose and membrane flux. Similar to the North Thames study, at baseline, elderly participants had lower PCS scores and similar MCS scores to young or middle-aged participants. In addition, elderly participants also experienced fewer effects of kidney disease and better sleep quality than young or middle-aged participants. Over 3 years of follow-up, there were trends for larger declines in the symptoms and problems, cognitive function, and sleep scales of the Kidney Disease Quality of Life Instrument, and less extensive decline in the Index of Well Being among elderly participants than among young or middle-aged participants, though in most cases these declines were relatively small in magnitude.
Dialysis modality
A number of studies have reviewed outcomes of peritoneal dialysis versus hemodialysis [25,26], including several studies devoted exclusively to the elderly [27–29]. Although analytical techniques differ across studies, the results consistently show higher mortality for elderly patients starting peritoneal dialysis versus hemodialysis. Using a propensity score approach, Winkelmayer et al. [29] reported a 16–45% increased risk for mortality in the first year after dialysis initiation among 2503 patients of at least 65 years of age initiating peritoneal dialysis versus hemodialysis. Couchoud et al. [28] evaluated the association between dialysis modality and mortality using data from the French Renal Epidemiology and Information Network (REIN) registry of ESRD. After adjustment for case-mix differences, patients started on peritoneal dialysis had 30% higher 2-year mortality rates versus patients started on hemodialysis.
Geriatric end-stage renal disease care
Almost 5% of patients with ESRDreside in nursing homes and this number is expected to rise as the ESRD population continues to age. An even larger fraction of ESRD patients is frail or cognitively impaired [30–33], and at risk for future disability and the need for long-term nursing home care. Transportation to and from dialysis facilities for disabled patients is cumbersome and costly; thus, interest in preventing disability and in reducing the burden of dialysis for nursing home patients has grown over the last several years. Li et al. [34•] recently reported the outcomes of 164 patients with ESRD admitted to a geriatric rehabilitation program. The mean age of patients was 74.5 ± 7.8 years and the mean dialysis vintage was 1.4 years. Most patients were admitted from the hospital; falls were the second most common reason for admission. Overall, 68% of patients were discharged home, 21% to assisted living or to a nursing home, and 11% to acute or palliative care. Sixty-seven percent of patients met all rehabilitation goals. The authors speculated that daily dialysis (as opposed to thrice weekly dialysis) may have limited post-dialysis symptoms and increased flexibility for scheduling rehabilitation treatments and thus possibly accounted for the success of their program.
Reddy et al. [35•] recently reported their experience with staff-assisted nursing home hemodialysis in five nursing homes in the Chicago area. A total of 296 patients were enrolled in the program over a 3.5-year period. The majority of patients were dialyzed with catheters (65%) and 47% had been on dialysis for less than 3 months prior to entry in the program. Forty percent of patients were unable to ambulate. During the study period, 46% died (including 4% who withdrew from dialysis), 37% were successfully discharged to outpatient dialysis programs, and the remainder (16%) remained active in the program. Together these pilot studies demonstrate that geriatric ESRD programs can be successfully implemented. Future quality improvement initiatives will need to determine whether such programs improve quality of life, promote independent living, and reduce resource use as compared with usual care.
Summary
Rates of treated ESRD among the elderly have been rising dramatically over the last decade. In studies with a large number of elderly patients, median survival after dialysis initiation is modest, and although a majority have reasonable life expectancy, a substantial minority of elderly patients experience very high early mortality rates. Quality of life results are mixed – compared with younger ESRD patients or non-ESRD elderly, mental well being is similar and physical well being is reduced in elderly patients with ESRD at baseline, and these findings remain generally similar over time. In several studies, elderly patients with ESRD initiating peritoneal dialysis had higher mortality rates than elderly patients with ESRD initiating hemodialysis. Strategies such as nondialytic management of ESRD or dietary protein restriction and delayed dialysis initiation may be alternatives for elderly patients wishing to avoid dialysis initiation, but further studies are needed to determine the patients best suited for these approaches. Quality improvement initiatives in geriatric ESRD care have been successfully implemented in some centers and may ultimately improve care for elderly patients with ESRD. These findings should help to clarify some of the risks and benefits of dialysis in the elderly and may be useful in dialysis decision-making and management.
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
• • of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (p. 273).
- 1.Collins AJ, Foley R, Herzog C, et al. Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis. 2008;51:S1–S320. doi: 10.1053/j.ajkd.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 2.seki K, Tozawa M, Iseki C, et al. Demographic trends in the Okinawa Dialysis Study (OKIDS) registry (1971–2000) Kidney Int. 2002;61:668–675. doi: 10.1046/j.1523-1755.2002.00147.x. [DOI] [PubMed] [Google Scholar]
- 3.McDonald S, McCredie M, Williams S, Stewart J. Factors influencing reported rates of treated end-stage renal disease. Adv Chronic Kidney Dis. 2005;12:32–38. doi: 10.1053/j.ackd.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 4. Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and non-agenarians starting dialysis in the United States. Ann Intern Med. 2007;146:177–183. doi: 10.7326/0003-4819-146-3-200702060-00006. This study on secular trends in dialysis initiation among the very elderly describes a rapid increase in dialysis initiation among the very elderly while at the same time median life expectancy was modest.
- 5.Hsu CY, Vittinghoff E, Lin F, Shlipak MG. The incidence of end-stage renal disease is increasing faster than the prevalence of chronic renal insufficiency. Ann Intern Med. 2004;141:95–101. doi: 10.7326/0003-4819-141-2-200407200-00007. [DOI] [PubMed] [Google Scholar]
- 6.Muntner P, Coresh J, Powe NR, Klag MJ. The contribution of increased diabetes prevalence and improved myocardial infarction and stroke survival to the increase in treated end-stage renal disease. J Am Soc Nephrol. 2003;14:1568–1577. doi: 10.1097/01.asn.0000067420.83632.c1. [DOI] [PubMed] [Google Scholar]
- 7.Waikar SS, Liu KD, Chertow GM. The incidence and prognostic significance of acute kidney injury. Curr Opin Nephrol Hypertens. 2007;16:227–236. doi: 10.1097/MNH.0b013e3280dd8c35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pascual J, Orofino L, Liano F, et al. Incidence and prognosis of acute renal failure in older patients. J Am Geriatr Soc. 1990;38:25–30. doi: 10.1111/j.1532-5415.1990.tb01592.x. [DOI] [PubMed] [Google Scholar]
- 9.Hsu CY, McCulloch CE, Fan D, et al. Community-based incidence of acute renal failure. Kidney Int. 2007;72:208–212. doi: 10.1038/sj.ki.5002297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waikar SS, Curhan GC, Wald R, et al. Declining mortality in patients with acute renal failure, 1988 to 2002. J Am Soc Nephrol. 2006;17:1143–1150. doi: 10.1681/ASN.2005091017. [DOI] [PubMed] [Google Scholar]
- 11. Schmitt R, Coca S, Kanbay M, et al. Recovery of kidney function after acute kidney injury in the elderly: a systematic review and meta-analysis. Am J Kidney Dis. 2008;52:262–271. doi: 10.1053/j.ajkd.2008.03.005. This meta-analysis of 17 studies of AKI in the elderly demonstrates that elderly patients are more likely to develop AKI and less likely to recover kidney function.
- 12.Langhofer S. What lies ahead in 2008. Nephrol News Issues. 2008;22:34–35. [PubMed] [Google Scholar]
- 13.Chandna SM, Schulz J, Lawrence C, et al. Is there a rationale for rationing chronic dialysis? A hospital based cohort study of factors affecting survival and morbidity. BMJ. 1999;318:217–223. doi: 10.1136/bmj.318.7178.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joly D, Anglicheau D, Alberti C, et al. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J Am Soc Nephrol. 2003;14:1012–1021. doi: 10.1097/01.asn.0000054493.04151.80. [DOI] [PubMed] [Google Scholar]
- 15. Murtagh FE, Marsh JE, Donohoe P, et al. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22:1955–1962. doi: 10.1093/ndt/gfm153. This study compares survival among elderly patients choosing dialysis versus nondialytic management and suggests there is no survival benefit for dialysis among patients with severe comorbidity.
- 16.Burns A, Carson R. Maximum conservative management: a worthwhile treatment for elderly patients with renal failure who choose not to undergo dialysis. J Palliat Med. 2007;10:1245–1247. doi: 10.1089/jpm.2007.0009. [DOI] [PubMed] [Google Scholar]
- 17.De Biase V, Tobaldini O, Boaretti C, et al. Prolonged conservative treatment for frail elderly patients with end-stage renal disease: the Verona experience. Nephrol Dial Transplant. 2008;23:1313–1317. doi: 10.1093/ndt/gfm772. [DOI] [PubMed] [Google Scholar]
- 18.Smith C, Da Silva-Gane M, Chandna S, et al. Choosing not to dialyse: evaluation of planned nondialytic management in a cohort of patients with end-stage renal failure. Nephron Clin Pract. 2003;95:c40–c46. doi: 10.1159/000073708. [DOI] [PubMed] [Google Scholar]
- 19.Wong CF, McCarthy M, Howse ML, Williams PS. Factors affecting survival in advanced chronic kidney disease patients who choose not to receive dialysis. Ren Fail. 2007;29:653–659. doi: 10.1080/08860220701459634. [DOI] [PubMed] [Google Scholar]
- 20. Brunori G, Viola BF, Parrinello G, et al. Efficacy and safety of a very-low-protein diet when postponing dialysis in the elderly: a prospective randomized multicenter controlled study. Am J Kidney Dis. 2007;49:569–580. doi: 10.1053/j.ajkd.2007.02.278. This small randomized trial examines the safety of dietary protein restriction and delayed initiation of dialysis versus immediate dialysis initiation in healthy nondiabetic elderly with ESRD.
- 21.Beddhu S, Samore MH, Roberts MS, et al. Impact of timing of initiation of dialysis on mortality. J Am Soc Nephrol. 2003;14:2305–2312. doi: 10.1097/01.asn.0000080184.67406.11. [DOI] [PubMed] [Google Scholar]
- 22.Friedman AN. New evidence for an old strategy to help delay the need for dialysis. Am J Kidney Dis. 2007;49:563–565. doi: 10.1053/j.ajkd.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 23.Lamping DL, Constantinovici N, Roderick P, et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. Lancet. 2000;356:1543–1550. doi: 10.1016/S0140-6736(00)03123-8. [DOI] [PubMed] [Google Scholar]
- 24. Unruh ML, Newman AB, Larive B, et al. The influence of age on changes in health-related quality of life over three years in a cohort undergoing hemodialysis. J Am Geriatr Soc. 2008;56:1608–1617. doi: 10.1111/j.1532-5415.2008.01849.x. This study in a large, representative cohort of participants participating in the HEMO study evaluates whether longitudinal changes in quality of life differ among elderly versus nonelderly on dialysis.
- 25.Vonesh EF, Snyder JJ, Foley RN, Collins AJ. Mortality studies comparing peritoneal dialysis and hemodialysis: what do they tell us? Kidney Int Suppl. 2006:S3–S11. doi: 10.1038/sj.ki.5001910. [DOI] [PubMed] [Google Scholar]
- 26.Jaar BG, Coresh J, Plantinga LC, et al. Comparing the risk for death with peritoneal dialysis and hemodialysis in a national cohort of patients with chronic kidney disease. Ann Intern Med. 2005;143:174–183. doi: 10.7326/0003-4819-143-3-200508020-00003. [DOI] [PubMed] [Google Scholar]
- 27.Collins AJ, Weinhandl E, Snyder JJ, et al. Comparison and survival of hemodialysis and peritoneal dialysis in the elderly. Semin Dial. 2002;15:98–102. doi: 10.1046/j.1525-139x.2002.00032.x. [DOI] [PubMed] [Google Scholar]
- 28.Couchoud C, Moranne O, Frimat L, et al. Associations between comorbidities, treatment choice and outcome in the elderly with end-stage renal disease. Nephrol Dial Transplant. 2007;22:3246–3254. doi: 10.1093/ndt/gfm400. [DOI] [PubMed] [Google Scholar]
- 29.Winkelmayer WC, Glynn RJ, Mittleman MA, et al. Comparing mortality of elderly patients on hemodialysis versus peritoneal dialysis: a propensity score approach. J Am Soc Nephrol. 2002;13:2353–2362. doi: 10.1097/01.asn.0000025785.41314.76. [DOI] [PubMed] [Google Scholar]
- 30.Cook WL, Jassal SV. Functional dependencies among the elderly on hemodialysis. Kidney Int. 2008;73:1289–1295. doi: 10.1038/ki.2008.62. [DOI] [PubMed] [Google Scholar]
- 31.Johansen KL, Chertow GM, Jin C, Kutner NG. Significance of frailty among dialysis patients. J Am Soc Nephrol. 2007;18:2960–2967. doi: 10.1681/ASN.2007020221. [DOI] [PubMed] [Google Scholar]
- 32.Kurella M, Chertow GM, Luan J, Yaffe K. Cognitive impairment in chronic kidney disease. J Am Geriatr Soc. 2004;52:1863–1869. doi: 10.1111/j.1532-5415.2004.52508.x. [DOI] [PubMed] [Google Scholar]
- 33.Murray AM, Tupper DE, Knopman DS, et al. Cognitive impairment in hemodialysis patients is common. Neurology. 2006;67:216–223. doi: 10.1212/01.wnl.0000225182.15532.40. [DOI] [PubMed] [Google Scholar]
- 34. Li M, Porter E, Lam R, Jassal SV. Quality improvement through the introduction of interdisciplinary geriatric hemodialysis rehabilitation care. Am J Kidney Dis. 2007;50:90–97. doi: 10.1053/j.ajkd.2007.04.011. This study describes the successful implementation and outcomes of a geriatric hemodialysis rehabilitation program.
- 35. Reddy NC, Korbet SM, Wozniak JA, et al. Staff-assisted nursing home haemodialysis: patient characteristics and outcomes. Nephrol Dial Transplant. 2007;22:1399–1406. doi: 10.1093/ndt/gfl809. This study describes initial experience implementing a large-scale nursing home-based hemodialysis program.