Abstract
Although Southeast Asian women are at exceedingly high risk for cervical cancer, low rates of the Pap testing necessary for early detection and successful treatment continue among this group. Previous research suggests that discussions about Pap testing with important people in a woman's life, particularly her doctor, may increase the likelihood of screening; therefore increasing women's discussions about cancer screenings is an important step toward behavior change. The purpose of this study was to determine the effectiveness of a culturally sensitive, seven-minute video intervention in reducing barriers to discussions about Pap tests among Thai women. This unique video presented Thai actors, speaking in Thai, in a soap opera format. Participants completed a self-report questionnaire at baseline, immediately after the intervention and at 3-month follow-up. The comparison group received an educational pamphlet. Although the results indicated that both groups experienced reductions in barriers to communicating with others about Pap tests, the intervention group had significantly stronger outcomes than the comparison group for communicating about Pap tests in general as well as to doctors. These findings suggest that intermediate communication effects such as self-efficacy, collective efficacy and perhaps interpersonal communication may reduce barriers to discussion and positive decision making regarding Pap tests.
Introduction
Cancer of the cervix remains one of the most easily preventable and treatable cancers of all cancer sites, yet research continues to show low rates of Pap testing for many ethnic and racial groups in the United States [1, 2]. Taylor et al. [3] report Southeast Asian women in the United States are at exceedingly high risk for cervical cancer, with incidence rates as high as 35.2 per 100 000 and mortality rates of 8.9 per 100 000. Past studies have pointed to the importance of physician recommendation for promoting Pap testing [3]; however, many Southeast Asian women lack health insurance and a regular source of medical care [4]. Compounding the problem is the manner in which cancer and other stigmatized diseases are not discussed openly [5], leaving many women with not only a lack of understanding of the severity of cervical cancer but also a lack of support for seeking screening services.
As described in a previous paper [4], California is home to the largest Thai-American population in the country, with the 2000 US Census reporting the overwhelming majority (nearly 35 000) living in Southern California [6]. This group possesses low levels of income and education, and they are a significant medically underserved population [6]. Mead suggests video can be a particularly effective medium for reaching low-literacy, culturally diverse populations such as Thai Americans [7]. A communication strategy to guide scripting and production of such a video is the entertainment–education (EE) communication strategy, which Singhal et al. [8] define as ‘the process of purposely designing and implementing a media message to both entertain and educate in order to increase audience members’ knowledge about an educational issue, create favorable attitudes, shift social norms and change overt behavior. According to health behavior change theories, positive attitudes toward a behavior increases an individual's intention to perform the behavior [9]. Nariman reports positive attitudinal effects among viewers of three EE soap operas [10].
Previous use of EE
Over the past three decades, well over 200 EE programs have been implemented worldwide, most of which present health-related educational issues in a soap opera format. This format is particularly popular among low-literacy female populations [8]. While these programs were serialized and mass mediated, several scholars have attempted to use the same strategy in developing effective health-related interventions. Love found that a short EE soap opera themed, Spanish language video was effective in increasing knowledge and discussions about breast cancer and mammography with friends or family members among Latinas at the precontemplation stage [11]. Jibaja et al. [12] found that breast cancer knowledge increased among Latinas at the contemplation, action and maintenance stages. Borrayo developed a Spanish language soap opera video to move Latinas to the contemplation and action stages of breast cancer awareness and screening, but the video has not been evaluated [13]. Taylor et al. [14] used an EE-inspired video with other interventions in a study to promote cervical cancer screening among Chinese women in North America; however, effects from the video were not isolated from those of the other interventions.
How EE influences behavior change through communication
EE may lead to parasocial interactions and media-stimulated peer communication which could influence desired behavioral change [15]. Horton and Wohl's concept of parasocial interaction is defined as the quasi-interpersonal relationship between an audience member and a media personality (such as the lead character in the intervention) [16]. They argue that with this relationship the audience member often views a media character as a counselor, comforter and model. It is suggested that audience members of serialized, mass-mediated EE soap operas may be influenced to change their behavior through this parasocial interaction. It is also suggested by Singhal et al. that EE content may stimulate peer conversations among audience members, with people considering new patterns of thought and behavior as a result of opportunities for collective efficacy. Collective efficacy is defined as whether or not people feel that they can come together with others to solve problems [8].
Thus, the role of the educator to stimulate interpersonal discussion among audience members is critical. It is also necessary that these discussions urge audience members to talk about the lead character and the intervention content with others.
The present study
In this paper, we report the longitudinal results of a quasi-experimental study to test the effectiveness of a Thai language, soap opera themed EE video on changes in attitudes toward discussions about cervical cancer and screening among Thai-American women in Los Angeles. In initial analyses, Love and Tanjasiri found that while short-term measures of behavior intention did not differ significantly between intervention and comparison groups [17], at 3-month follow-up women in the intervention group developed more positive attitudes toward discussions about cervical cancer and screening with their friends, doctors and family members relative to the comparison group.
Method
This quasi-experimental study was conducted in Los Angeles and Orange Counties, California in 2004–06 with the purpose of designing, developing and testing the effectiveness of a culturally sensitive video intervention to increase cervical cancer knowledge and promote positive attitudes and screening behavior among Thai women. Once our institution's Internal Review Board for research with human subjects approved this study, the video was scripted and produced using the theoretical framework that will be described here. Pre-test, post-test, and 3-month follow-up measures assessed changes in cervical cancer and Pap test knowledge, attitudes and behaviors (these results reported elsewhere). A further analysis isolated communication outcome attitude variables concerning participants’ discussions about cervical cancer screening with friends, doctors and family members.
Participant recruitment
Two Thai community health educators recruited a total of 498 Thai women aged 18 years and older for the baseline assessment. The educators were experienced in cancer control education for the Thai community in Los Angeles and Orange Counties. This study used purposive sampling based upon organizational sites. First, an organizational recruitment plan was developed which included input from the educators. Recruitment sites included beauty salons, Thai markets, massage parlors with Thai women employees and Thai temples. It should be noted that the massage parlors were not brothels, as is the case in some countries.
The Thai community health educators visited each site and recruited as many of the age-eligible women as possible. Pre-identified sites were then randomly assigned to receive either the EE video intervention (including viewing of the EE video and a facilitated discussion with a health educator) or a one-page Thai language handout on cervical cancer and Pap tests (see Fig. 1). A written informed consent form in the Thai language was given to all women by the educators, who explained the form personally. Only those women who signed the form were included in the study. The form indicated that participants would receive a cash incentive to participate ($10) at the time of recruitment and an additional $10 when they completed the follow-up questionnaire 3 months later.
Fig. 1.
Study Design.
Of the 498 women who completed the baseline assessment, nearly all of them (495, 99.4%) completed the post-test survey and 374 of them (75.1%) completed the 3-month follow-up survey. Of these 374 participants, 365 of them provided data on the variables of interest and comprised the analytic sample for this study. Therefore, the target sample size of 400 across the three assessments was nearly met. This target sample size was chosen based upon the number of participants needed to detect intervention group versus comparison group differences on dichotomous outcome variables using a chi-square test, at a power level of 80%, alpha = 0.05 and an effect size of 0.30 (which is in between a small and medium effect size).
Measures
Questionnaire items included demographic variables, health care access indicators and knowledge, attitude and behavior questions related to cervical cancer and screening. Demographic items on the survey, which were covariates in this study, included: country of birth, fluency in Thai, fluency in English, years of education, marital status, income range and age range. Health access questions, which assessed health insurance coverage and place of regular medical care, were adapted from the scientifically supported access items of the California Health Interview Survey [18]. The outcome variables of this study consisted of four statements that assessed attitudes toward discussions about cervical cancer screening: ‘I don't like to talk about Pap tests.’ ‘I would never talk to a doctor about a Pap test’; ‘I would never talk to a friend about a Pap test’; and ‘I would never talk to a family member about a Pap test’. Participants indicated whether they agreed or disagreed with each of these statements separately.
Procedures
Upon their consent to participate in the study, women were given the self-administered pretest questionnaire. At the conclusion of the assigned educational intervention, the women were administered the post-test questionnaire. Upon completion of the post-test, they were thanked, given $10 and reminded that they would be contacted again in approximately 3 months to schedule a follow-up survey. Three months later, a community health educator called each participant and set up a time to meet personally, or through an in-person visit to the workplace, to complete the follow-up survey (at the conclusion of which they were given the other $10 incentive).
Intervention development and implementation
The overall goal of the intervention was to increase cervical cancer knowledge and promote positive attitudes and screening behavior among Thai women. Creativity and cultural sensibility are demanded in developing and presenting health messages in an EE drama format [8]. Piotrow and DeFossard of Johns Hopkins University's Center for Communication Programs, which has assisted over the past 20 years in some 125 EE programs in 40 countries worldwide, identified six major challenges faced when attempting to keep EE interventions credible and entertaining [19]. The intervention script for this study addressed three of these challenges: (i) the EE is of high quality and is emotionally resonant to the target audience; (ii) health messages are woven into program naturally, gradually and subtly and (iii) is research based. The secondary goal of this video was to facilitate discussion between the educator and the video viewers, promoting parasocial interactions and ultimately media-stimulated peer communication.
Initial development
This study's video script took over 4 months to develop. Initially, the two bilingual Thai–English health educators developed a draft script, based upon their experience and numerous informal conversations with the target audience. There was also input from the non-Thai researchers on the study, who emphasized the necessity of using positive and negative role models for the desired behavior change (Pap testing), as suggested by Bandura's social modeling theory [20]. In using the EE communication strategy, the researchers avoided detailed medical information, and emphasized credible characters who delivered a message within the dramatic context of a soap opera. Every effort was made to balance entertainment values with medical facts; for example, the lead character has ongoing, serious abdominal pain which enhances the dramatic elements of the story, eventually resulting in a fact-filled doctor visit and a happy ending.
Content of the video
The main character and her friend in the video were shown to be in their 40s. While the target audience was Thai women 18+, because cervical cancer incidence increases with age, it was decided to portray the main character as early middle aged, a woman who should be aware of the necessity for yearly screening. The script's negative role model, who is also the main character, is a mother who is seen with her close-knit family. Mother continually ignores the abdominal pain the audience sees her experience until her good friend, the positive role model, insists she see her doctor for a checkup and that she also have a Pap test. The main character is seen discussing with her doctor why the Pap test is necessary and also asking questions about cervical cancer based on the lack of knowledge identified by Tsui and Tanjasiri [4].
Feedback from the community and final production
After the script was developed, it was shown to a Thai physician, staff at Thai health clinics and a Thai filmmaker for their input. After undergoing several rewrites, the final version of the script, with appropriate approvals, was translated into Thai by the two bilingual health educators. Time and budget constraints did not permit a pilot study of the video. The Thai filmmaker who produced the video used broadcast-quality production methods with a special emphasis on creating the ‘look’ of a Thai soap opera.
Administering the intervention
Upon completion of the video, the two Thai community educators went to organizational sites within the Thai community to either show the video (for intervention participants) or distribute an information handout in Thai (for comparison participants). The bilingual educator for the intervention groups carried a small, portable DVD player and showed the video to small groups of participants. For comparison groups, the bilingual educator brought small, printed handouts about cervical cancer and distributed these to small groups of participants. After either modality (video or handout), the educators answered questions and facilitated a discussion with the participants regarding their knowledge, attitudes and beliefs about Pap testing and cervical cancer. As mentioned earlier, the paper and pencil survey assessments were administered at pretest (prior to watching the video or receiving the pamphlet), at post-test (immediately after watching the video or receiving the pamphlet) and at 3-month follow-up.
Data analyses
Statistical analyses were performed using SPSS version 14.0. Only those participants who completed both the pretest and 3-month follow-up surveys were included in the analyses. Differences between intervention and comparison group participants on demographic variables were assessed with a series of chi-square tests. Chi-square tests were also used to compare intervention and comparison group participants on the four communication attitude variables at pretest. The final set of analyses were only conducted on those participants who responded ‘yes’ to any of the four communication attitude variables at pretest. The target population for this study consisted of this group, as a yes answer indicated a reluctance to communicate to others about Pap tests. First, chi-square tests were calculated to determine intervention versus comparison group differences on ‘improvement’ on each of the communication attitude variables. Improvement for a given individual was defined as movement from a yes on a communication attitude variable at pretest to a no on the same variable at 3-month follow-up. Last, four logistic regression models were performed to further assess intervention effects after adjusting for the effects of demographic covariates.
Results
Demographic characteristics of study participants
Table I presents the demographic characteristics of the entire analytic sample (n = 365) and of each group (n = 177 for the intervention group; n = 188 for the comparison group). Nearly all (96.5%) the participants were born in Thailand and spoke Thai either fluently or well (90.7%). Over two-thirds of the sample reported that Thai was the language that they are most comfortable speaking. Nearly half (46.1%) of the sample was married, and the comparison group had a significantly higher percentage of married women relative to the intervention group (50.5 and 41.3%, respectively). About half (50.7%) of the sample was 36–55 years old and nearly two-thirds reported a family income of less than $2,000 per month. Nearly half (47.9%) of the sample reported having health insurance; however, the comparison group was much more often insured than the intervention group (56.6 versus 38.5%). Over four-fifths (81.7%) of the sample had had a Pap test at least once in their lifetime.
Table I.
Demographics of study participants at pretest (n = 365)
| Intervention (n = 177) |
Comparison (n = 188) |
χ2(df) | Total (n = 365) |
||||
| n | % | n | % | n | % | ||
| Place of birth | |||||||
| Thailand | 155 | 95.1 | 177 | 97.8 | 1.85 (1) | 332 | 96.5 |
| Other | 8 | 4.9 | 4 | 2.2 | 12 | 3.5 | |
| Speak Thai | |||||||
| Fluently/well | 149 | 88.2 | 174 | 93.0 | 2.52 (1) | 323 | 90.7 |
| Fair/poor/not at all | 20 | 11.8 | 13 | 7.0 | 33 | 9.3 | |
| Language most comfortable | |||||||
| Only/mostly Thai | 123 | 71.5 | 121 | 65.4 | 1.54 (1) | 244 | 68.3 |
| Other | 49 | 28.5 | 64 | 34.6 | 113 | 31.7 | |
| Marital status | |||||||
| Married | 71 | 41.3 | 94 | 50.5 | 9.85* (4) | 165 | 46.1 |
| Divorced/separated | 24 | 14.0 | 28 | 15.1 | 52 | 14.5 | |
| Long-term relationship | 14 | 8.1 | 6 | 3.2 | 20 | 5.6 | |
| Single | 33 | 19.2 | 40 | 21.5 | 73 | 20.4 | |
| Widowed | 30 | 17.4 | 18 | 9.7 | 58 | 13.4 | |
| Age group | |||||||
| 18–35 | 32 | 18.7 | 40 | 21.5 | 2.85 (4) | 72 | 20.2 |
| 36–45 | 30 | 17.5 | 42 | 22.6 | 72 | 20.2 | |
| 46–55 | 57 | 33.3 | 52 | 28.0 | 109 | 30.5 | |
| 56–65 | 32 | 18.7 | 29 | 15.6 | 61 | 17.1 | |
| 66+ | 20 | 11.7 | 23 | 12.4 | 43 | 12.0 | |
| Family income | |||||||
| <$500/month | 25 | 14.7 | 16 | 9.0 | 8.55 (5) | 41 | 11.8 |
| $500–999 | 55 | 32.4 | 48 | 27.1 | 103 | 29.7 | |
| $1000–1499 | 31 | 18.2 | 27 | 15.3 | 58 | 16.7 | |
| $1500–1999 | 18 | 10.6 | 22 | 12.4 | 40 | 11.5 | |
| $2000–2999 | 19 | 11.2 | 25 | 14.1 | 44 | 12.7 | |
| $3000+ | 22 | 12.9 | 39 | 22.0 | 61 | 17.6 | |
| Have health insurance | |||||||
| Yes | 65 | 38.5 | 103 | 56.6 | 11.54*** | 168 | 47.9 |
| No | 104 | 61.5 | 79 | 43.4 | (1) | 183 | 52.1 |
| Ever had a Pap test | |||||||
| Yes | 139 | 84.2 | 146 | 79.3 | 1.39 (1) | 285 | 81.7 |
| No | 26 | 15.8 | 38 | 20.7 | 64 | 18.3 | |
Note: Includes only women who completed both pretest and 3-month post-test. Frequencies for each variable do not add up to the total sample size (n = 365) because of missing data. *P < 0.05, ***P < 0.001.
Intervention group differences on communication attitude variables at pretest
Table II presents intervention versus comparison group differences on each of the four communication attitude variables at pretest. The majority of participants indicated that they did not like talking to doctors (67.4%) or friends (68.8%) about Pap tests. Less than half (43.8%) reported that they did not like talking about Pap tests in general, and relatively few (11.0%) reported that they did not like talking to their family members about Pap tests. Chi-square test statistics indicated that at pretest, comparison group participants were more likely to report less favorable attitudes toward talking about Pap tests to doctors (74.5%), friends (73.4%) and family (14.4%) relative to the intervention group.
Table II.
Pretest intervention group differences on communication attitude variables
| Intervention (n = 177) |
Comparison (n = 188) |
χ2(1) | Total (n = 365) |
||||
| n | % | n | % | n | % | ||
| Don't like to talk about Pap tests | |||||||
| Yes | 69 | 39.0 | 91 | 48.4 | 3.29 | 160 | 43.8 |
| No | 108 | 61.0 | 97 | 51.6 | |||
| Never talk to doctor about Pap tests | |||||||
| Yes | 106 | 59.9 | 140 | 74.5 | 8.82** | 246 | 67.4 |
| No | 71 | 40.1 | 48 | 25.5 | |||
| Never talk to friend about Pap tests | |||||||
| Yes | 113 | 63.8 | 138 | 73.4 | 3.88* | 251 | 68.8 |
| No | 64 | 32.2 | 50 | 26.6 | |||
| Never talk to family members about Pap tests | |||||||
| Yes | 13 | 7.3 | 27 | 14.4 | 4.60* | 40 | 11.0 |
| No | 164 | 92.7 | 161 | 85.6 | |||
Note: Includes only women who completed both pretest and 3-month post-test. * P < 0.05, **P < 0.01.
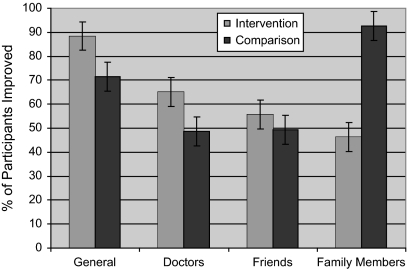
Figure 2 presents the percentage of women who improved from yes to no on each of the communication attitude variables at 3-month follow-up. The intervention group demonstrated greater improvement on attitudes toward talking about Pap tests in general and talking to doctors relative to the comparison group. Of the 69 intervention participants who reported at pretest that they do not like talking about Pap tests in general, all but 8 (88.4%) of them changed their mind by 3-month follow-up, while less than three-quarters of the 91 control participants (71.4%) showed the same improvement (χ2(1) = 6.76, P < 0.01). Similarly, of the 106 intervention participants who reported at pretest that they would never talk to a doctor about Pap tests, nearly two-thirds of them (65.1%) indicated that they changed their mind at post-test, while less than half (48.6%) of the 140 comparison group participants showed the same improvement (χ2(1) = 6.67, P = 0.01). On the other hand, the comparison group participants showed greater improvement on attitudes toward talking to family members relative to the intervention group. All but 2 of the 27 (92.6%) comparison group participants who reported that they would not talk to their family about Pap tests at baseline changed their mind by 3-month follow-up, while less than half (46.2%) of the 13 intervention group participants showed the same improvement (χ2(1) = 10.85, P < 0.001). No group differences were found for the friends’ variable; slightly over half of the entire sample (52.2%) who reported not wanting to talk to their friends at baseline changed their mind by 3-month follow-up.
Fig. 2.
Improvement on Communication Variables at Posttest #2.
Table III presents the adjusted odds ratios (AORs) for the effects of the intervention and the demographic covariates on improvement on each of the communication attitude variables. As mentioned previously, improvement was defined as movement from a yes to a communication attitude variable at pretest to a no on the same variable at 3-month follow-up. Therefore, these analyses were restricted to participants who responded yes to the variable at baseline. Consistent with the findings in Fig. 2, the AORs indicated that the intervention group had greater improvements on attitudes toward talking about Pap tests in general (AOR = 4.05) and to doctors (AOR = 1.98) relative to the comparison group and less improvement on talking to family members (AOR = 0.03) relative to the comparison group. The variables of ‘comfort level speaking Thai’, age and ‘ever having had a Pap test’ were also associated with improvement on communication attitudes. Specifically, women who were more comfortable speaking Thai had greater improvements on attitudes toward communicating about Pap tests in general (AOR = 3.04) and to friends (AOR = 1.99) relative to those who were less comfortable speaking Thai. Older women demonstrated greater improvement in attitudes toward talking to doctors (AOR = 1.24). Last, those women who reported ever having a Pap test in the past demonstrated greater improvement in attitudes toward talking about Pap tests in general (AOR = 4.02).
Table III.
Logistic regression of improvement on communication attitude variables at 3-month post-test
| Talk about Pap tests |
Talk to doctor about Pap tests |
Talk to friends about Pap tests |
Talk to family about Pap tests |
|||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Intervention (versus comparison) | 4.05** | 1.48–11.05 | 1.98* | 1.10–3.54 | 1.28 | 0.73–2.25 | 0.03** | 0.02–0.48 |
| Comfortable speaking Thai | 3.04* | 1.11–8.32 | 1.24 | 0.66–2.32 | 1.99* | 1.07–3.70 | 2.46 | 0.14–42.00 |
| Married (versus other) | 1.12 | 0.43–2.88 | 0.88 | 0.49–1.59 | 0.86 | 0.48–1.52 | 0.61 | 0.04–8.85 |
| Age group | 0.99 | 0.73–1.35 | 1.24* | 1.00–1.53 | 1.00 | 0.81–1.22 | 0.97 | 0.42–2.24 |
| Family income | 1.32 | 0.99–1.75 | 0.99 | 0.84–1.17 | 1.08 | 0.92–1.27 | 0.67 | 0.30–1.50 |
| Health insurance (yes versus no) | 1.53 | 0.56–1.45 | 1.18 | 0.63–2.22 | 1.08 | 0.58–2.02 | 0.50 | 0.03–9.39 |
| Pap test (yes versus no) | 4.02* | 1.15–14.01 | 1.67 | 0.81–3.44 | 1.49 | 0.72–3.09 | 4.04 | 0.30–54.82 |
Note: Includes only women who completed both pretest and post-test and were at risk. CI, confidence interval. *P < 0.05, **P < 0.01.
Discussion
The significant changes in communication attitudes of the intervention group within 3 months suggest that the intervention may have resulted in a type of audience involvement called parasocial interaction between the main EE character and audience members (see Introduction). Audience involvement is a very complex concept and operationalizing it is well beyond the scope of this paper.
The changes in intervention group participants’ communication patterns suggest modeling behavior [20]. The main character in the intervention eventually modeled desirable behavior by discussing the Pap test extensively with her friend and subsequently talking to her doctor about the test and understanding why the test was so important to her health. Nearly all intervention group members (∼89%) who reported not liking to talk about Pap tests in general changed their minds by the 3-month follow-up. We also saw significant increases in communication about Pap tests with doctors (just >65%) and with friends (nearly 69%), which reminds us that Horton and Wohl [16] argued that parasocial interaction can be extremely influential for audience members who may identify with the main character, perhaps perceiving him/her as a role model.
The EE video provides its audience with examples of both socially desirable or undesirable behavior through the use of positive and negative role models. Papa et al. [21, 22] suggest that a process of change is facilitated when conversations between groups of people become shared stories about how one should respond to problems that are commonly experienced. Intuitively, it is suggested audience members may perceive cervical cancer screening as a problem or something they do not wish to do, based on the very low compliance rates among this population and as such a subject that may become part of a shared conversation among women.
The potential increased interpersonal communication about Pap tests seen between pretest and 3-month follow-up for the intervention group holds promise for promoting behavior change. Scholars such as Lazarsfeld, Berelson and Gaudet believe that interpersonal communication is essential before change in behavior can be achieved [23]. Scholars such as Rogers and Kincaid [24], Rogers et al. [25] and Valente et al. [26] suggest that mass-mediated EE programs have been shown to facilitate interpersonal communication about the media program itself. It is suggested that an EE video such as the one in this study, combined with interpersonal discussion between the educator and the participants, holds potential for intermediate communication effects.
Future directions
Results of this study suggest several ways in which the intervention could be improved. Pre-development focus group discussions with targeted women are needed to ensure as many barriers as possible are identified and addressed. Cultural barriers should receive particular attention and discussion. Additional focus groups should center on the video itself, specifically discussions of preferred entertainment genre, reactions to soap operas and opinions regarding soap opera characters. Some focus groups should be shown the existing intervention to determine and discuss audience attention levels and involvement, as well as reaction to characters and their actions. Length of the video should also be addressed, specifically whether audience members can establish a relationship with a character in a seven-minute video.
The significant increase in communication about Pap tests seen in this study suggests a number of ways in which the present study could be improved. Using the present study as a pilot, the authors plan a follow-up study incorporating these improvements and using the existing intervention, a valuable asset already paid for and produced. The authors will consider a focus on communication variables using established measures of parasocial interactions, self-efficacy and collective efficacy and explore using a Likert scale on existing study items to get a more rigorous measure of shifts in attitudes.
In the way of study improvement, more time and effort should be devoted to recruitment of participants to ensure that more non-English speaking, unscreened women are included. Prior to data collection, targeted women in focus groups should see the video to discuss attention levels and potential editing. These discussions will also be used to improve educators’ discussions by identifying specific points to be discussed about characters’ actions and factual information that should be reinforced. The authors did not record communications between health educators and intervention group participants after the intervention showing; this will be done in the follow-up study in order to gain insight into participants’ reactions.
The authors will re-examine data collection sites, as discussion with the educators in this study revealed intervention group programs at some work sites were interrupted. The follow-up study should focus on more communication variables, including measures of the audience's involvement. Additionally, since the printed handout produced significant increases on two of the communication measures, and to enhance methodological/statistical rigor, the follow-up study should employ four groups: (i) a true control group which receives no intervention or handout, (ii) a group receiving the video intervention only, (iii) a group receiving the handout only and (iv) a group receiving both the video intervention and the handout to test the interaction effect. This is particularly important in that production of a handout is substantially less expensive and requires fewer resources. It should be noted that the study intervention was developed within a theoretical framework which relates the video content to interpersonal discussion between the educator and the audience. The intervention was not developed to stand alone without an educator, and was not distributed to the community to be used in a ‘stand alone’ capacity, but to educators who would use it in their programs.
While improvement on communication variables were seen in both the intervention group and the comparison group, the authors believe the effects in the intervention group were strong enough to merit further study in the use of the EE communication strategy to promote both the quantity and quality of communication among women about cervical cancer and its risks.
Using the present study results and the present intervention in a new study incorporating communication, concepts such as parasocial interactions and collective efficacy may hold promise for a better understanding of the biggest challenge of all—achieving behavior change.
Funding
National Cancer Institute (R03 CA113158).
Conflict of interest statement
None declared.
Acknowledgments
The authors gratefully acknowledge the invaluable contributions of Jackie Tran, Waraporn ‘Nid’ Tiaprasith, Srinapha ‘Noi’ Vasunilashorn, the entire study team and all the study participants.
References
- 1.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Asian and Pacific Islander Women in the United States, 1994-1997. Cancer Epidemiol Biomarkers Prev. 2000;9:597–603. [PubMed] [Google Scholar]
- 2.Adams EK, Breen N, Joski PJ. Impact of the national breast and cervical cancer early detection program on mammography and pap test utilization among white, Hispanic and African-American women: 1996-2000. Cancer. 2007;109(2 Suppl.):348–58. doi: 10.1002/cncr.22353. [DOI] [PubMed] [Google Scholar]
- 3.Taylor VM, Schwartz SM, Jackson JC, et al. Cervical cancer screening among Cambodian-American women. Cancer Epidemiol Biomarkers Prev. 1999;8:541–6. [PubMed] [Google Scholar]
- 4.Tsui J, Tanjasiri SP. Cervical cancer screening among Thai women in Northern California. J Womens Health. 2008;17:393–401. doi: 10.1089/jwh.2007.0427. [DOI] [PubMed] [Google Scholar]
- 5.Special Service for Groups. Report on the Breast and Cervical Cancer Screening Needs and Recommendations for Cambodians, Chamorros, Laotians, Samoans, Thais, Tongans, and Vietnamese. Los Angeles: Special Service for Groups, Inc.; 2001. [Google Scholar]
- 6.APALC. The Diverse Face of Asians and Pacific Islanders in Los Angles, CA. Los Angeles: Asian Pacific American Legal Center; 2005. [Google Scholar]
- 7.Mead CD. Producing videotapes for cancer education: methods and examples. Oncol Nurs Forum. 1996;23:837–46. [PubMed] [Google Scholar]
- 8.Singhal A, Cody M, Rogers E, et al., editors. Entertainment-Education and Social Change: History, Research, and Practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 9.Montano DE, Kasprizk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, editor; Lewis F, Rimer B, editors. Health Behavior and Health Education: Theory, Research and Practice. 4thedn. San Francisco: Jossey Bass; 2002. [Google Scholar]
- 10.Nariman HN. Soap Operas for Social Change. Westport, CT: Praeger; 1993. [Google Scholar]
- 11.Love GD. An Entertainment-Education Video as a Tool to Influence Mammography Compliance Behavior in Latinas. Kansas City: 2003. Proceedings, Assn for Ed in Jnl and Mass Comm. Available online at www.AEJMC.com/Scholarship/Abstract Archive/Science Communication. [Google Scholar]
- 12.Jibaja ML, Kingery P, Neff NE, et al. Tailored, interactive soap operas for breast cancer education of high-risk Hispanic women. J Cancer Ed. 2000;15:237–42. doi: 10.1080/08858190009528705. [DOI] [PubMed] [Google Scholar]
- 13.Borrayo EA. Where's Maria? A video to increase awareness about breast cancer and mammography screening among low-literacy Latinas. Prev Med. 2004;39:99–110. doi: 10.1016/j.ypmed.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 14.Taylor VM, Hislop TG, Jackson JC, et al. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. J Natl Cancer Inst. 2002;94:670–7. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singhal A, Rogers E. Entertainment-Education: A Communication Strategy for Social Change. Mahwah, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- 16.Horton D, Wohl RR. Mass communication and parasocial interaction: observation on intimacy at a distance. Psychiatry. 1956;19:215–29. doi: 10.1080/00332747.1956.11023049. [DOI] [PubMed] [Google Scholar]
- 17.Love G, Tanjasiri S. Using entertainment-education to promote cervical cancer screening in Thai women. J Cancer Ed. 2008 doi: 10.1007/s13187-012-0369-5. Reviewed and Resubmitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.California Health Interview Survey. Available at: http://www.chis.ucla.edu/. Accessed: 13 September 2007. [Google Scholar]
- 19.Piotrow PT, de Fossard E. Entertainment-education as a public health intervention. In: Singhal A, Cody MJ, Rogers E, et al., editors. Entertainment-Education and Social Change: History, Research, and Practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 20.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 21.Papa MJ, Auwal MA, Singhal A. Dialectic of control and emancipation in organization for social change: a multitheoretic study of the Grameen Bank in Bangladesh. Commun Theory. 1995;5:189–223. doi: 10.1111/j.1468-2885.1995.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 22.Papa MJ, Auwal MA, Singhal A. Organizing for social change within concertive control systems: member identification, empowerment, and the masking of discipline. Communn Monogr. 1997;64:219–50. [Google Scholar]
- 23.Lazarsfeld P, Berleson B, Gauder H. The peoples’ choice: How the voter makes up his mind in a presidential campaign. New York: Columbia University Press; 1968. [Google Scholar]
- 24.Rogers EM, Kincaid DL. Communication Networks: Toward a New Paradigm for Research. New York: Free Press; 1981. [Google Scholar]
- 25.Rogers EM, Vaughan P, Swalehe R, et al. Effects on an entertainment-education radio soap opera on family planning and HIV/AIDS prevention behavior in Tanzania. Stud Fam Plann. 1999;50:17–36. doi: 10.1111/j.1728-4465.1999.00193.x. [DOI] [PubMed] [Google Scholar]
- 26.Valente T, Poppe P, Payne-Merritt A. Mass media generated interpersonal communication as sources of information about family planning. J Health Comm. 1996;1:247–65. doi: 10.1080/108107396128040. [DOI] [PubMed] [Google Scholar]