Abstract
Background
In 2004, the State of Wisconsin introduced a change to their Medicaid Policy allowing medical care providers to be reimbursed for fluoride varnish treatment provided to Medicaid enrolled children.
Objective
To determine the extent by which a state-level policy change impacted access to fluoride varnish treatment (FVT) for Medicaid enrolled children.
Data Source
The Electronic Data Systems of Medicaid Evaluation and Decision Support database for Wisconsin from 2002 to 2006.
Study Design
We analyzed Wisconsin Medicaid claims for FVT for children between the ages of 1 and 6 years, comparing rates in the prepolicy period (2002–2003) to the period (2004–2006) following the policy change.
Principal Findings
Medicaid claims for FVT in 2002–2003 totaled 3,631. Following the policy change, claims for FVT increased to 28,303, with 38.0 percent submitted by medical care providers. FVT rates increased for children of both sexes and all ages, rising from 1.4 per 1,000 person-years of enrollment in 2002–2003 to 6.6 per 1,000 person-years in 2004–2006. Overall, 48.6 percent of the increase in FVT was attributable to medical care providers. The largest increase was seen in children 1–2 years of age, among whom medical care providers were responsible for 83.5 percent of the increase.
Conclusions
A state-level Medicaid policy change was followed by both a significant involvement of medical care providers and an overall increase in FVT. Children between the ages of 1 and 2 years appear to benefit the most from the involvement of medical care providers.
Keywords: Medicaid-enrolled children, oral health disparities, fluoride varnish treatment, medical care providers, policy change
Although the oral health of most Americans has improved (U.S. Department of Health and Human Services 2000), dental caries, a preventable disease, still remains the single most prevalent childhood disease (Edelstein 1998; Vargas, Crall, and Schneider 1998; Vargas and Ronzio 2006;). Untreated dental caries cause many children to experience needless pain, suffer from social stigma, lowered self-esteem, and loss of school time (Newacheck et al. 2000b; Chu et al. 2007;). In addition, the burden of dental caries is disproportionately shouldered by poor and racial/ethnic minority children, as well as those with special health care needs (Newacheck et al. 2000a). Most of these children rely on public programs, such as Medicaid, to pay for medical and dental care services. Under Medicaid, the Early, Periodic Screening, Diagnosis, and Treatment program requires that basic dental services be covered for children (Department of Health and Human Services, Medicaid at-a-Glance 2005), including services aimed at caries prevention. However, inadequate access to these services have led to oral health disparities for Medicaid enrolled children (U.S. Department of Health and Human Services 2000).
Currently, a number of explanations for inadequate access to dental care for the Medicaid-enrolled population have been put forth in the literature. One reason is the geographic maldistribution of dentists (Mertz and Grumbach 2001), leading to severe shortages in communities where oral health care services are needed the most. Another reason is the severe shortage of minority dentists to serve this population, as one study has reported that minority dentists are more likely to accept new Medicaid patients (Okunseri et al. 2008). In addition, Valdes et al. (2007) pointed out that while parents of enrolled children are aware of the need for preventive dental procedures covered by Medicaid, their lack of usage may be driven by inappropriate pain management and a lack of cultural sensitivity among dentists.
From a public health perspective, it is important to provide adequate access to measures aimed at primary prevention of caries because of their self-compounding effects. As discussed by Vargas et al. (2002) and Vargas and Ronzio (2006) dental caries produce a self-sustaining spiral of unmet needs whereby untreated caries become more severe and difficult to treat, thereby increasing treatment costs and reducing the availability of clinicians able to perform more complicated treatments. Therefore, a reduction in the prevalence of caries for high-risk populations requires the early availability of services designed to stop the initiation of this cycle. One such measure, fluoride varnish treatment (FVT), has been advocated by the American Dental Association (ADA) for high-risk children as young as 6 months old, where the definition of high-risk includes children from low-socioeconomic backgrounds (American Dental Association Council on Scientific Affairs 2006). The ADA's recommendation states that from 6 months of age, children at high risk of caries development should receive FVT at 6-month intervals (American Dental Association Council on Scientific Affairs 2006). However, many of these high-risk children are unable to receive care from a dentist, due in part to low number of dentists who are Medicaid providers in most states. Thus, there is need to pursue alternative delivery mechanisms for preventive dental services to public program patients in a sustainable and effective manner.
One such alternative put forth by oral health stakeholders in America is the involvement of medical care providers such as physicians and nurses. The involvement of medical care providers was proposed because (1) physician offices represent an opportune site to reach a large number of children who make medical visits, but do not see a dentist (Casamassimo 1996; American Academy of Pediatrics, Committee on Practice and Ambulatory Medicine 2000; Schafer and Adair 2000; Sonis and Zaragoza 2001; American Academy of Pediatrics 2003;); (2) physicians have a relatively high participation rate in Medicaid, compared with a much lower rate among dentists (Dela Cruz, Rozier, and Slade 2004); (3) most infants and children see their pediatricians and family physicians for early preventive procedures such as immunizations and for other health care checks; and (4) medical provider clinics are often open for longer hours than regular dental offices. Therefore, by allowing dental providers and medical care providers to apply FVT, a wider array of access points for Medicaid-enrolled children may be created.
In 2004, the State of Wisconsin introduced a change to their Medicaid Policy allowing medical care providers to be reimbursed for FVT. This allowed pediatricians and other primary health care providers to become sources of FVT, risk assessment, preventive oral health education, and care for young children and others who are unable to readily gain access to dental care. Before the implementation of the policy change, employees of the Wisconsin Department of Health and Family Services, Division of Public Health conducted a series of training sessions for physicians, physician assistants, pediatricians, and nurse practitioners regarding the need and proper application techniques for FVT to young children's teeth. However, to date, there has not been any assessment of whether this policy change and additional training have led to an improvement in access to FVT for Medicaid-enrolled children. Despite the lack of evidence indicating whether the involvement of medical care providers has been effective in improving access to FVT, presently about 24 other states in America have adopted similar policies. The primary purpose of the present study was to evaluate whether the inclusion of medical care providers has led to an increase in the rate of FVT claims for Medicaid-enrolled children in Wisconsin.
METHODS
Data Source
The study used data from the Electronic Data Systems of Medicaid Evaluation and Decision Support (MEDS) database for Wisconsin from 2002 to 2006. This database, managed by the Division of Health Care Financing in the Wisconsin Department of Health and Family Services (WDHFS), contains all Medicaid claims for the state of Wisconsin. The data extracted for this study consisted of two primary components: claim level data for fluoride varnish applications and enrollment data that defined the Medicaid-enrolled population in Wisconsin. The targeted Medicaid-enrolled population consisted of children between the ages of 1 year to 6 years with at least 1 month of eligibility between January 1, 2002, and December 31, 2006. The claims data consisted of fee-for-service claims and managed care encounter information for those children receiving FVT (as indicated by procedure code D1203). The claim- level data were merged with the eligibility data by patient identification number. The provider type was unknown for 112 records (0.3 percent). Because an individual's enrollment status can change within the course of a year, enrollment data were used to normalize the rate of claims for fluoride varnish applications relative to the number of person-years of enrollment. For example, a child enrolled for an entire year contributes one person-year of enrollment.
Demographic Variables
Demographic variables obtained from the MEDS database included gender, race/ethnicity, and age of each Medicaid-enrolled child. Race/ethnicity was self-designated under the following categories: White, African American, Hispanic/Latino, Asian/Pacific Islander, Native American, and Multiracial; Unknown (2,189 records, 6.7 percent) was treated as a separate category. Age groups were defined as 1–<2, 2–<3, 3–<4, 4–<5, and 5–<6 years.
Study Design and Analytic Methods
The study is a retrospective secondary analysis of all Wisconsin Medicaid dental claims for fluoride varnish application submitted for 2002–2006. Descriptive statistics (means, sample proportions) were computed to examine the distribution of study variables within the Wisconsin Medicaid population. The primary statistical analysis consisted of comparing the overall rate of fluoride varnish claims before and after the policy change in 2004. The number of claims and person-years of eligibility was calculated for each age and period (pre- or postintervention) separately for every individual. Poisson regression was used to estimate the rate of claims per person-year of enrollment; repeated measurements within an individual were incorporated using a Generalized Estimating Equation approach (Zeger, Liang, and Albert 1988). All analyses were performed using SAS v9.1.3 (SAS Institute, Cary, NC). The study was approved by the Institutional Review Boards of Marquette University and the Medical College of Wisconsin.
RESULTS
Characteristics of Medicaid-Enrolled Children in Wisconsin
Overall, there was a steady increase in the size of the Medicaid-enrolled population in Wisconsin from 2002 to 2006 (Table 1). The enrolled population for children between the ages of 1 and 6 years increased from 99.7 thousand person-years in 2002, to a high of 121.3 thousand person-years in 2006 (an increase of 21.7 percent). The largest group of Medicaid-enrolled children was between the ages of 1–<2 years (ranging from 21.5 to 22.4 percent between 2002 and 2006), and males outnumbered females by roughly 2 percent during the same period. Almost half of the study population designated their race/ethnicity as white; African American was the most common racial/ethnic minority group, accounting for 24.1 percent of the person-years of enrollment in 2002. There was a steady decline in the proportion of person-years accounted for by African American children, reaching a low of 20.1 percent in 2006. Conversely, there was a corresponding increase in the number of Hispanic children, rising from 12.9 percent of the total person-years of enrollment in 2002 to 15.9 percent in 2006.
Table 1.
Characteristics of Wisconsin Medicaid-Enrolled Children between the Ages of 1 Year to 6 Years from 2002 to 2006
| Prepolicy Period |
Postpolicy Period |
||||
|---|---|---|---|---|---|
| Characteristics | 2002 | 2003 | 2004 | 2005 | 2006 |
| Overall person-years of enrollment* | 99.7 | 109.0 | 115.8 | 120.0 | 121.3 |
| Subcategory of enrollment | Percent person-years by subcategory (sum of each column within each subcategory equals 100%) | ||||
| Age (years) | |||||
| 1–<2 | 22.4 | 21.8 | 21.5 | 21.7 | 21.5 |
| 2–<3 | 21.0 | 20.9 | 20.7 | 20.4 | 20.7 |
| 3–<4 | 19.9 | 20.0 | 20.1 | 19.9 | 19.7 |
| 4–<5 | 18.9 | 19.1 | 19.4 | 19.4 | 19.3 |
| 5–<6 | 17.8 | 18.1 | 18.4 | 18.7 | 18.8 |
| Race/Ethnicity | |||||
| White | 46.9 | 48.1 | 48.4 | 47.7 | 46.5 |
| African American | 24.1 | 22.7 | 21.6 | 20.8 | 20.1 |
| Native American | 2.0 | 2.0 | 2.1 | 2.1 | 2.1 |
| Asian/Pacific Islander | 3.4 | 3.2 | 3.2 | 3.5 | 3.4 |
| Hispanic/Latino | 12.9 | 14.1 | 14.9 | 15.4 | 15.9 |
| Multiracial | 1.8 | 2.0 | 2.2 | 2.3 | 2.3 |
| Unknown | 9.0 | 7.8 | 7.5 | 8.1 | 9.7 |
| Gender | |||||
| Male | 51.2 | 51.1 | 51.3 | 51.1 | 51.2 |
| Female | 48.8 | 48.9 | 48.7 | 48.9 | 48.8 |
In thousands of person-years of enrollment.
Characteristics of Claims Submitted by Medical Care Providers
Before the policy change, there were 3,631 Medicaid claims submitted for FVT. Following the policy change, claims for FVT increased to 28,303, with 38.0 percent submitted by medical care providers. Among claims submitted by medical care providers, the majority were from physicians (54.5 percent) and in terms of specialty the overwhelming majority of claims were from pediatricians (85.7 percent).
Rates of FVT before and after Medicaid Policy Change
Overall, the rates of FVT claims were 0.14 and 0.66 per 100 person-years of enrollment for the prepolicy (2002–2003) and postpolicy (2004–2006) periods (Rate Ratio [RR]=4.69, 95 percent CI: 4.50–4.90) (Table 2). The change in the rate of FVT claims was highest for children between the ages of 1 and 2 years (RR=26.33, 95 percent CI: 21.35–21.48), followed by children 2–<3 years (RR=4.62, 95 percent CI: 4.22–5.06), and lowest for children 5–<6 years old (RR=3.10, 95 percent CI: 2.90–3.32). Males and females displayed almost equal relative improvements in their rate of FVT claims following the policy change. In terms of race/ethnicity, Native Americans displayed the largest change in their rate of FVT claims (RR=24.75, 95 percent CI: 15.13–40.50), followed by whites (RR=8.48, 95 percent CI: 7.73–9.31), and Asians/Pacific Islanders (RR=7.98, 95 percent CI: 5.87–10.87). African Americans exhibited the smallest improvement in their rate of FVT claims (RR=1.73, 95 percent CI: 1.63–1.86).
Table 2.
Wisconsin Medicaid Claims for Fluoride Varnish Treatment
| Rates of Fluoride Varnish Treatment |
|||
|---|---|---|---|
| 2002–2003 | 2004–2006 | Rate Ratio | |
| Characteristic | Prepolicy Rate* | Postpolicy Rate* | (95% CI) |
| Overall† | 0.14 (0.003) | 0.66 (0.006) | 4.69 (4.50, 4.90) |
| Dental providers | 0.12 (0.003) | 0.41 (0.004) | 3.45 (3.28, 3.62) |
| Medical providers | 0 | 0.17 (0.003) | NA |
| Race/ethnicity | |||
| Asian/Pacific Islander | 0.07 (0.012) | 0.59 (0.027) | 7.98 (5.87, 10.87) |
| African American | 0.27 (0.009) | 0.47 (0.010) | 1.73 (1.63, 1.86) |
| Hispanic/Latino | 0.20 (0.009) | 1.12 (0.018) | 5.65 (5.20, 6.14) |
| Multiracial | 0.08 (0.017) | 0.50 (0.033) | 6.49 (4.24, 9.93) |
| Native American | 0.07 (0.018) | 1.73 (0.071) | 24.75 (15.13, 40.50) |
| Unknown | 0.11 (0.006) | 0.48 (0.043) | 4.42 (3.76, 5.20) |
| White | 0.07 (0.003) | 0.59 (0.008) | 8.48 (7.73, 9.31) |
| Age (years) | |||
| 1–<2 | 0.02 (0.002) | 0.47 (0.009) | 26.33 (21.35, 32.48) |
| 2–<3 | 0.10 (0.004) | 0.46 (0.008) | 4.62 (4.22, 5.06) |
| 3–<4 | 0.21 (0.007) | 0.72 (0.011) | 3.38 (3.17, 3.60) |
| 4–<5 | 0.25 (0.007) | 0.91 (0.012) | 3.69 (3.47, 3.93) |
| 5–<6 | 0.12 (0.003) | 0.36 (0.014) | 3.10 (2.90, 3.32) |
| Gender | |||
| Female | 0.14 (0.004) | 0.66 (0.008) | 4.76 (4.48, 5.05) |
| Male | 0.14 (0.003) | 0.65 (0.016) | 4.62 (4.35, 4.91) |
Rates are per 100 person-years of Medicaid enrollment.
Includes providers of unknown type.
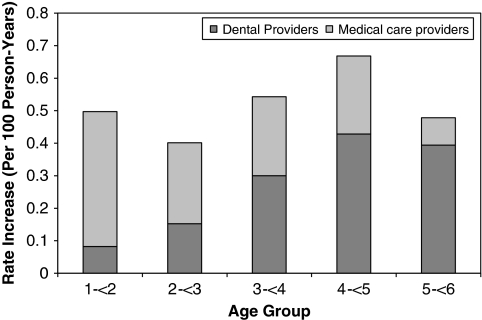
Overall, the rate of FVT claims by dentists increased by over 300 percent (RR=3.45, 95 percent CI: 3.28–3.62) following the inclusion of medical care providers. The relative contributions of dentists and medical care providers to the increase in the rate of FVT claims following the policy change are shown in the Figure 1. Medical care providers were responsible for much of the increase observed for the youngest children, accounting for 83.5 percent of the increase in children between 1 and <2 years of age. In contrast, dentists were responsible for 82.4 percent of the rate increase observed among children between the ages of 5 and <6 years.
Figure 1.
The Relative Contributions of Dental Providers and Medical Care Providers to the Increase in Fluoride Varnish Claims Post Policy Change by Age Group
DISCUSSION
This study is the first to examine the impact of a change in Medicaid policy that allows for reimbursing medical care providers for FVT to help prevent dental caries. Overall, we found a significant increase in the rate of FVT claims for Medicaid-enrolled children. This result is particularly important on two fronts. First, there was a significant involvement of medical care providers, as they accounted for slightly under 40 percent of the FVT claims submitted after 2004. This would appear to indicate the willingness of medical care providers to support the prevention of dental caries in children. Possible reasons for this participation of medical care providers in the provision of FVT include its ease of application, patient acceptance, and a reduced risk for toxicity. Second, we also observed an increase in the rate of FVT claims by dentists. This was in spite of the fact that the size of Medicaid-enrolled population in Wisconsin continued to grow over the study period. This result is particularly promising given reports indicating that there is a decline in the dentist to patient ratio and a maldistribution of dentists, especially in communities where their services are needed the most.
Children ages 1–2 years appeared to benefit the most from the involvement of medical care providers in the application of FVT. We found that medical care providers were responsible for over three quarters of the increase in FVT for children in this age range. This finding is not surprising given that children within the ages of 1–2 years usually see their pediatrician and family physicians for early preventive procedures such as immunizations and other health care checks. This finding also supports a recent study that reports that 74 percent of pediatricians who responded to a national survey would be willing to accept reimbursement for applying FVT to children's teeth in their practices (Lewis et al. 2000).
One very intriguing result was that the rate of FVT for children ages 3–6 years provided by dentists substantially increased following the policy change. Based on our data, it is not immediately clear why such an increase would be observed in conjunction with a policy change affecting medical care providers. The reimbursement rate for FVT did not change over the study period, and in fact, Wisconsin has one of the lowest reimbursement rates ($12.76 per application) out of states that currently allow medical care providers to bill for FVT (Cantrell 2008). The Wisconsin Dental Association was initially concerned with this policy because it did not create an atmosphere of long-term, sustainable preventive care by facilitating access to a dental home (Weber 2004). It addition, the policy did not include a component designed to address the Medicaid population's need for basic restorative care. Despite these initial concerns, it is conceivable that this policy led to an increased focus on preventive services among dental providers in Wisconsin, leading to the observed increase in FVT.
Although Native American children constitute the lowest percentage of the Medicaid-enrolled children in Wisconsin, this population experienced the largest increase in its rate of FVT claims. This finding for Native American children is particularly important given the increased caries risk for this minority population (Niendorff and Jones 2000; Nash and Nagel 2005;). For example, data from the Make Your Smile Count Survey, conducted by the Wisconsin Department of Health and Family Services (DHFS) in 2001–2002, indicated that 64 percent of third-grade Native American children screened had untreated decay compared with 25 percent of white children (Oral Health Program Division of Public Health, WI DHFS 2001–2002). Therefore, the involvement of medical care providers could be one way to address the observed oral health disparities among Native American populations especially in Wisconsin. In contrast, African American children displayed the lowest absolute rate of FVT claims as well as the smallest change in rates following the policy change. One possible explanation for this phenomenon is that African American children are also particularly susceptible to inadequate access to medical care (National Center for Health Statistics Health, United States 2006). This would imply that promoting preventive oral health services among African American children is invariably tied with the large task of improving their access to the health care system in general.
Despite the observed increase in the rate of FVT, the absolute rates following the policy change still indicate a need to improve access to preventative oral health care for Medicaid-enrolled children. Given that the ADA advocates FVT twice a year for high-risk children, which includes children from low socioeconomic backgrounds, the rates shown in Table 2 clearly show a large deficit in the receipt of FVT. As an example, even if we conservatively say that only 50 percent of Medicaid-enrolled children in Wisconsin should be receiving FVT twice a year, this implies that the rate per 100 person-years of enrollment should be on the order of 100. However, the highest rate observed for any population subgroup was 1.73 for Native Americans. This suggests that (1) further monitoring should be done to examine whether the rate of FVT continues to rise and (2) that the involvement of medical care providers will likely not be sufficient to meet the preventive oral health care needs of underserved populations.
Implication for Policy and Practice
The findings from this study serve as an important baseline for future Medicaid policies regarding the delivery of preventive oral health services. At a minimum, our results provide an argument in favor of allowing medical care providers to be reimbursed for FVT by Medicaid in states yet to implement such a policy. However, the absolute rate of FVT claims following the policy change also suggests that there is still much to be done to improve the oral health of high-risk populations.
LIMITATIONS
Certain potential study limitations should be noted. The primary limitation is that the pre–post study design suffers from a lack of comparison data from a state yet to allow reimbursement for FVT to medical care providers. Therefore, it is unclear whether one can directly attribute the rise in FVT, particularly among dentists, to the policy change. While it will be important to investigate this increase to further improve access, we do not believe this limitation negates the primary conclusion that the provision of FVT by medical care providers is a significant improvement in preventive oral health care delivery. We examined only Wisconsin Medicaid enrollees; therefore, it is possible that our findings do not generalize to other states. However, given that Wisconsin's Medicaid population consists of a racially/ethnically diverse population with both urban and rural poor, we believe our results should extend to other states. Medicaid claims data can be subject to coding errors and inconsistently recorded provider information, leading to a potential study bias. Finally, we did not have access to individual-level provider data, and so we were unable to tabulate the number of FVT claims submitted per provider. Therefore, we are unable to infer whether the observed increases resulted from a small number of providers substantially increasing their provision of FVT, or whether it resulted from smaller increases from a larger number of providers.
CONCLUSION
A state-level Medicaid policy change was followed by both a significant involvement of nondental providers and an overall increase in FVT. Children 1–2 years old appeared to benefit the most from involvement of medical care providers. Similar policy changes in other states may also lead to increased access to children's primary preventive dental services.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Dr. Okunseri was supported by Health Resources and Services Administration (HRSA) Maternal and Child Health Bureau R40MC08955 grant to the Marquette University, and Dr. Garcia was supported by NIH grants K24 DE000419, U54 DE014264, U54 DE019275, and U54 RR024381. We thank David Ebert for helping us with accessing the database. We are also very grateful to the anonymous reviewers, whose helpful comments improved the quality of the manuscript.
Disclaimers/Financial and Other Disclosures: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- American Academy of Pediatrics. Policy Statement. Oral Health Risk Assessment Timing and Establishment of the Dental Home. Pediatrics. 2003;111:1113–6. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics, Committee on Practice and Ambulatory Medicine. Recommendations for Preventive Pediatric Health Care (RE9939) Pediatrics. 2000;105:645–6. [Google Scholar]
- American Dental Association Council on Scientific Affairs. Professionally Applied Topical Fluoride: Evidence-Based Clinical Recommendations. Journal of the American Dental Association. 2006;137:1151–9. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- Cantrell C. The Role of Physicians in Children's Oral Health. State Health Policy Monitor. National Academy for State Health Policy. 2008;2(5):1–5. [Google Scholar]
- Casamassimo P. Bright Futures in Practice: Oral Health. Arlington, VA: National Center for Education in Maternal and Child Health; 1996. [Google Scholar]
- Chu M, Sweis LE, Guay AH, Manski RJ. The Dental Care of U.S. Children: Access, Use and Referrals by Nondentist Providers, 2003. Journal of the American Dental Association. 2007;138:1324–31. doi: 10.14219/jada.archive.2007.0047. [DOI] [PubMed] [Google Scholar]
- Dela Cruz GG, Rozier RG, Slade G. Dental Screening and Referral of Young Children by Pediatric Primary Care Providers. Pediatrics. 2004;114:e642–e652. doi: 10.1542/peds.2004-1269. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. Medicaid at-a-Glance. A Medicaid Information Source. Department of Health and Human Services, Center for Medicare and Medicaid Services [accessed on February 13, 2008]. Available at http://www.cms.hhs.gov/MedicaidGenInfo/downloads/MedicaidAtAGlance2005.pdf.
- Edelstein BL. Evidence-Based Dental Care for Children and Age 1 Dental Visits. Pediatric Annals. 1998;27:569–74. doi: 10.3928/0090-4481-19980901-09. [DOI] [PubMed] [Google Scholar]
- Lewis CW, Grossman DC, Domoto PK, Deyo RA. The Role of the Pediatrician in the Oral Health of Children: A National Survey. Pediatrics. 2000;106:e84. doi: 10.1542/peds.106.6.e84. [DOI] [PubMed] [Google Scholar]
- Mertz EA, Grumbach K. Identifying Communities with Low Dentist Supply in California. Journal of Public Health Dentistry. 2001;61:172–7. doi: 10.1111/j.1752-7325.2001.tb03386.x. [DOI] [PubMed] [Google Scholar]
- Nash DA, Nagel RJ. Confronting Oral Health Disparities among American Indian/Alaska Native Children: The Pediatric Oral Health Therapist. American Journal of Public Health. 2005;95:1325–9. doi: 10.2105/AJPH.2005.061796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics Health, United States. With Chartbook on Trends in the Health of Americans Hyattesville, MD [accessed on February 14, 2008]. Available at http://www.cdc.gov/nchs/data/hus/hus06.pdf.
- Newacheck PW, McManus M, Fox HB, Hung YY, Halfon N. Access to Health Care for Children with Special Health Care Needs. Pediatrics. 2000a;105:760–6. doi: 10.1542/peds.105.4.760. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The Unmet Health Needs of America's Children. Pediatrics. 2000b;105:989–97. [PubMed] [Google Scholar]
- Niendorff WJ, Jones CM. Prevalence and Severity of Dental Caries among American Indians and Alaska Natives. Journal of Public Health Dentistry. 2000;60(suppl 1):243–9. doi: 10.1111/j.1752-7325.2000.tb04069.x. [DOI] [PubMed] [Google Scholar]
- Okunseri C, Bajorunaite R, Abena A, Self K, Iacopino AM, Flores G. Racial/Ethnic Disparities in the Acceptance of Medicaid Patients in Dental Practices. Journal of Public Health Dentistry. 2008;68:149–53. doi: 10.1111/j.1752-7325.2007.00079.x. [DOI] [PubMed] [Google Scholar]
- Oral Health Program Division of Public Health, WI Department of Health and Family Services. 2002. Overview of Children's Oral Health in Wisconsin, Youth Oral Health Data Collection Report.
- Schafer TE, Adair SM. Prevention of Dental Disease: The Role of the Pediatrician. Pediatric Clinics of North America. 2000;47:1021–42. doi: 10.1016/s0031-3955(05)70256-x. [DOI] [PubMed] [Google Scholar]
- Sonis A, Zaragoza S. Dental Health for the Pediatrician. Current Opinions in Pediatrics. 2001;13:289–95. doi: 10.1097/00008480-200106000-00013. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- Valdes XL, Greenwell A, Theriot J, Franco S. Access Barriers to Dental Care for Medicaid Patients. Journal of Kentucky Medical Association. 2007;105:491–95. [PubMed] [Google Scholar]
- Vargas CM, Monajemy N, Khurana P, Tinanoff O. Oral Health Status of Preschool Children Attending Head Start in Maryland, 2000. Pediatric Dentistry. 2002;24:257–63. [PubMed] [Google Scholar]
- Vargas CM, Crall JJ, Schneider DA. Socio-Demographic Distribution of Pediatric Dental Caries: NHANES III, 1988–1994. Journal of the American Dental Association. 1998;129:1229–38. doi: 10.14219/jada.archive.1998.0420. [DOI] [PubMed] [Google Scholar]
- Vargas CM, Ronzio CR. Disparities in Early Childhood Caries. BMC Oral Health. 2006;6(suppl 1):S3. doi: 10.1186/1472-6831-6-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber C. Gov. Doyle Announces Fluoride Varnish Reimbursement for MA Pediatrics. Wisconsin Dental Association Journal. 2004;8 [Google Scholar]
- Zeger S, Liang KY, Albert P. Models for Longitudinal Data: A Generalized Estimating Equation Approach. Biometrics. 1988;44:1049–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.