Abstract
Objective
To test how the implementation of new Medicare post-acute payment systems affected the use of inpatient rehabilitation facilities (IRFs), skilled nursing facilities (SNFs), and home health agencies.
Data Sources
Medicare acute hospital, IRF, and SNF claims; provider of services file; enrollment file; and Area Resource File data.
Study Design
We used multinomial logit models to measure realized access to post-acute care and to predict how access to alternative sites of care changed in response to prospective payment systems.
Data Extraction Methods
A file was constructed linking data for elderly Medicare patients discharged from acute care facilities between 1996 and 2003 with a diagnosis of hip fracture, stroke, or lower extremity joint replacement.
Principal Findings
Although the effects of the payment systems on the use of post-acute care varied, most reduced the use of the site of care they directly affected and boosted the use of alternative sites of care. Payment system changes do not appear to have differentially affected the severely ill.
Conclusions
Payment system incentives play a significant role in determining where Medicare beneficiaries receive their post-acute care. Changing these incentives results in shifting of patients between post-acute sites.
Keywords: Medicare, post-acute care, prospective payment, access to care
Post-acute care encompasses a wide range of health care services that share the goal of restoring recently hospitalized patients to their prior level of functioning. Post-acute care is also used to improve the transition from hospital to the community, and post-acute care facilities provide services to patients needing additional support to assist them in recuperating following discharge from an acute care hospital.
Patients can access post-acute care services in many settings, including skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs), and their own homes with services from home health agencies (HHAs). Each of these settings offers a different level of care. IRFs provide intensive care (3 or more hours a day of rehabilitation therapy). SNFs can also provide inpatient rehabilitation under the Medicare benefit, although it is generally less intensive than that provided in an IRF (Gage 1999). HHAs provide therapy, nursing care, and assistance from home health aides.
Between 1988 and 1997, Medicare expenditures for post-acute care increased at an average annual rate of 25 percent (Medicare Payment Advisory Commission [MedPAC] 2003a, b), making it the fastest growing category of Medicare spending. This increase was due to a shift to post-acute care as a way to reduce acute care length of stay after the prospective payment system for acute care hospitals was put in place and to liberalization of the definitions of eligibility for service provision and coverage (Lewis et al. 1987; Neu, Harrison, and Heilbrunn 1989; Manton et al. 1993; Steiner and Neu 1993; Chan et al. 1997; McCall et al. 2003a, b).
However, trends in spending for post-acute care changed after passage of the Balanced Budget Act of 1997 and subsequent Balanced Budget Refinement Act of 1999. These laws altered Medicare's post-acute care payment policies dramatically, shifting payments to post-acute care providers from a cost basis to prospective payment. Between 1997 and 2002, Medicare introduced an interim payment system for HHAs (1997) and prospective payment for SNFs (1998), HHAs (2000), and IRFs (2002). The new payment systems for post-acute care were designed to reduce spending and introduce incentives for efficiency, and early evidence indicates that they have constrained use and contained expenditures (Cotterill and Gage 2002; Komisar 2002; McCall et al. 2003a, b; MedPAC 2003a, b; Street et al. 2003; White 2003; Fitzgerald 2006). After rising from US$14 billion in 1994 to US$35.7 billion in 1996, total Medicare spending for post-acute care declined to US$28.0 billion in 2001, before increasing again to US$42.1 billion in 2005. Between 1996 and 2001, the number of Medicare beneficiaries using post-acute care decreased by 18 percent, from 4.3 million to 3.5 million users (MedPAC 2003a, b, 2007).
The early evidence also suggests that the new payment systems have led to shifts in the types of post-acute care patients receive. The decrease in Medicare spending for post-acute care between 1996 and 2001 was due to a nearly 50 percent decline in spending for home health care, with use of post-acute care other than home health care actually growing during the period. Using the Medicare 1 percent sample, McCall et al. (2003a, b) observed that changes in treatment patterns included more beneficiaries receiving no post-acute care and much lower use of home health care, but slightly higher use of inpatient rehabilitation and long-term care hospitals. MedPAC (2003a, b) examined changes before and after implementation of the prospective payment systems for SNFs and home health care and found substantial declines in the use of home health care but increases in the use of skilled nursing and other post-acute care providers, indicating that, for some diagnoses, skilled nursing may be partly replacing home health care. For example, for patients discharged from acute care with a diagnosis of septicemia, use of home health care declined from 21 to 10 percent while SNF use increased from 21 to 27 percent (MedPAC 2003a, b). Lin et al. (2006) examined changes in PAC use early in the period following the Balanced Budget Act for patients in six categories: stroke, hip and knee procedures, hip fracture, chronic obstructive pulmonary disease, pneumonia, and congestive heart failure. Using a 5 percent sample of Medicare beneficiaries, they found that use of home health care decreased in response to the home health interim payment system and use of skilled nursing decreased in response to prospective payment in SNFs.
Existing studies suggest that the outcomes of post-acute care have not worsened as a result of the new payment systems (Angelelli et al. 2002; McCall et al. 2003a, b), but there is some evidence that quality of care for patients with a skilled nursing stay declined between 2000 and 2004 (Kaplan 2007). Nonetheless, concerns remain that lower use of post-acute care generally, coupled with shifts in sites of care, will eventually have an adverse impact on beneficiary access to appropriate care and health outcomes (DeJong et al. 2002; MedPAC 2002, 2006). These concerns are compounded by the lack of clinical consensus about which patients need post-acute care and what types of post-acute care are appropriate for which patients, which may leave patients particularly exposed to decisions about care that are based on nonclinical factors, including providers' financial incentives (Jette and Keysor 2002). Cotterill and Gage (2002) suggested that some portion of the increase in the use of inpatient rehabilitation between 1997 and 2000 may have been influenced by the incentives to curb use inherent in the interim payment system for home health and prospective payment for SNFs. Buntin et al. (2005) found that the geographical availability of different types of post-acute care facilities affected the probability that Medicare patients discharged from acute care would receive facility-based post-acute care as well as the setting in which they received care.
In this paper, we investigate the effects of four major changes in post-acute care payment systems on Medicare beneficiaries' use of different types of post-acute care, including SNFs, IRFs, and HHAs. We focus on patients discharged from acute care hospitals with a diagnosis of hip fracture, stroke, or lower extremity joint replacement, the three largest categories of patients receiving post-acute care. Together, they make up about 53 percent of inpatient rehabilitation cases and about 14 percent of skilled nursing cases (MedPAC 2008). We focus on these diagnoses in order to isolate homogenous groups of patients to more accurately capture differences over time associated with payment changes. We also examine whether the effects of the payment changes differed between more severely ill patients, who are expected to be more costly, and those who are less severely ill. Our study differs from previous work on this topic in that we use data for the full (non-HMO) Medicare population in a continuous 8-year period (1996–2003), which includes the implementation of the home health interim payment system, skilled nursing prospective payment, home health prospective payment, and inpatient rehabilitation prospective payment, and considers the effects of all the payment changes simultaneously. Because payment systems for alternative sites affect use of each setting, we are fortunate to have data covering the period during which all of the prospective payment systems were put in place. In addition, given the richness of our dataset, we are able to control for more variables, including discharging hospital characteristics, which might change over time. Finally, this is the first study to look for adverse selection against the most severely ill patients in all post-acute settings after the payment changes.
CHANGES IN MEDICARE PAYMENT FOR POST-ACUTE CARE
The post-acute care payment system changes we study are the home health interim payment system, implemented in October 1997; the skilled nursing prospective payment system, implemented in July 1998; the home health prospective payment system, implemented in October 2000; and the inpatient rehabilitation prospective payment system, implemented in January 2002. These payment systems markedly vary in their design. The interim payment system for home health limited payments by reducing the per-visit cost limits that were in place and adding an aggregate per-beneficiary payment limit (McCall et al. 2003a, b). The skilled nursing prospective payment system uses per-diem payments to encourage providers to limit cost per day, but it does not provide incentives to limit length of stay. Payments amounts are case mix adjusted; prospective payments were initially considered less generous than payments under the previous system because they did not reimburse for the actual cost of providing care, especially ancillary services. Home health prospective payment provides incentives to limit expenditures per episode by reimbursing providers using 60-day pay periods. The Balanced Budget Act required prospective payment for home health to be budget neutral to the interim payment system, with 15 percent rate cuts. However, the Balanced Budget Refinement Act postponed the cuts until the fiscal year 2002, when rates were cut by 15 percent. The inpatient rehabilitation prospective payment system uses per-discharge payments to provide incentives for limiting costs per rehabilitation stay. Payment amounts are based on payment categories defined by the patient's rehabilitation impairment (e.g., stroke, hip fracture), functional status, and comorbidities and are, therefore, case mix adjusted (Carter et al. 2002; Stineman 2002).
The payment systems also varied in the degree to which they aimed to reduce Medicare spending. The American Hospital Association (AHA) (1998) projected that the home health interim payment system would save US$3.1 billion in 1998 and 1999, whereas the Centers for Medicare and Medicaid Services estimated that the prospective payment system for SNFs would save US$30 million in 1998 (AHA 1998). By contrast, prospective payment for inpatient rehabilitation was designed to be budget neutral. Nonetheless, all of the prospective payment systems share the feature that providers who deliver care that costs less than the payments they receive can keep the difference as profit.
HYPOTHESES
Based on the design and goals of the different payment systems, we formulated the following hypotheses for the study:
The immediate effects of the home health interim payment system and the skilled nursing prospective payment system, which were intended to constrain cost growth, would be to reduce the use of home health and skilled nursing, respectively. Further, reductions in use would differentially affect more severely ill patients because their costs would not be fully captured by case-mix systems. In addition, over time, the home health and skilled nursing payment systems would lead to greater use of alternative sites of post-acute care.
The home health prospective payment system would continue to reduce the use of home health care overall because it was designed to continue the interim payment system cuts. It would, however, increase use by severely ill patients because, unlike under the previous payment system, the home health prospective payments are case-mix adjusted. In addition, over time, prospective payment would result in greater use of alternative sites of post-acute care.
The inpatient rehabilitation prospective payment system, which was designed to be budget neutral, would have little effect on the use of inpatient rehabilitation care overall. However, the prospective payment system would increase use by more severely ill patients because, unlike under the previous payment system, prospective payments are case-mix adjusted.
DATA AND METHODS
Study Sample
We have data on all elderly Medicare patients discharged from hospitals between January 1996 and June 2003. Within this group, we chose to focus on the three largest patient groups using all types of post-acute care: stroke patients, hip fracture patients, and lower extremity joint replacement patients. These conditions account for approximately 7 percent of Medicare acute care discharges and one quarter of discharges to post-acute care. Our sample, exclusions, and measures are described in further detail in prior work (Buntin et al. 2005).
Variables
We conducted multivariate regression analyses in which we modeled the type of post-acute care as function changes in post-acute care payment systems and a wide array of covariates that affect the use of post-acute care. The dependent variable in the analyses was the first post-acute care site used after discharge from an acute care hospital. We chose to use the first site because a substantial majority of the patients discharged from acute care use only one site for post-acute care. (Ninety-three percent of all acute care discharges who receive post-acute care use only one site, whereas 72 percent of patients with the three study conditions use only one site.) For the study, we defined use of post-acute care use as use of inpatient rehabilitation, skilled nursing, or home health care that began within 30 days of discharge from the acute care hospital and was covered by Medicare.
The key independent variables were intended to capture the effects of the changes in post-acute care payment systems, which we assumed would be superimposed on an underlying trend in the use of post-acute care. Therefore, we included a linear time trend and indicator variables for the seasons in the models to account for the underlying trend and for seasonal variations in use. (Seasonal variations can arise as a result of seasonal patterns in the illness severity of patients with the study conditions [Laake and Sverre 1996; Aronow and Ahn 2004;].) To capture the shift in the proportion of patients going to each post-acute care site that was associated with the implementation of each new payment policy, we included indicator variables for the implementation of each of the four payment systems. These variables were set to 0 before the fourth quarter of 1997, the third quarter of 1998, the fourth quarter of 2000, and the first quarter of 2002, respectively, and to 1 beginning in those quarters. Last, we included interactions between each of the payment policy indicator variables and the linear time trend in order to capture changes in the slope of the time trend resulting from the changes in the payment policies.
The covariates in the models included demographic and clinical characteristics of the patients as well as characteristics of the acute care hospital that might affect post-acute care choices. Post-acute care supply characteristics play a key role in post-acute care use as well (Neu, Harrison, and Heilbrunn 1989; Swan and Benjamin 1990; Kenney and Dubay 1992; Dubay 1993; Steiner and Neu 1993; Young 1997; Liu, Wissoker, and Rimes 1998; MedPAC 2003a, b). However, because these effects can themselves be altered by payment system changes, we do not include them in our models because developing models to account for endogenous effects of this type was beyond the scope of this project. We identified a number of demographic characteristics that affect the use of post-acute care and type of post-acute care used, including age, gender, Medicaid coverage, race, and place of residence, defined as a metropolitan statistical area (MSA), an area adjacent to an MSA, or rural area/not adjacent to an MSA (Neu, Harrison, and Heilbrunn 1989; Manton et al. 1993; Steiner and Neu 1993; Kane et al. 1996; Lee, Huber, and Stason 1997; Liu, Wissoker, and Rimes 1998; Gage 1999; Bronskill, Normand, and McNeil 2002; Finlayson 2002; Shatto 2002; MedPAC 2003a, b; Buntin et al. 2005). To allow for nonlinear effects of age on the use of post-acute care, we classified patients into 3-year age bands.
The covariates in the models also included a large number of clinical variables intended to capture the case mix, or clinical complexity, of patients at the time of discharge from the acute care hospital. Thus, we included a set of comorbidities, complications of acute care, and condition-specific measures tailored to stroke, hip fracture, and joint replacement patients and derived from the diagnoses reported on the hospital discharge records. The comorbidities used in the analyses were the chronic conditions identified by Iezzoni et al. (1994) as conditions that are nearly always present before hospital admission and hence are extremely unlikely to represent complications arising during the hospitalization. The comorbidities we included in the models were as follows: cancer with a poor prognosis, metastatic cancer, chronic pulmonary disease, coronary artery disease, congestive heart failure, peripheral vascular disease, severe chronic liver disease, diabetes with end organ damage, chronic renal failure, nutritional deficiencies, dementia, functional impairment, and diabetes without end organ damage.
The complications were conditions and problems that were likely to have arisen during the acute care hospital stay. To develop the list of complications, we adapted the complication list developed by Iezzoni et al. (1994) to reflect only those complications that were likely to have a continued effect after hospital discharge and, therefore, to potentially influence the choice of site for post-acute care. We augmented the list to include some important complications for the Medicare population that had been omitted from the original list. The complications we included in the models were postoperative pulmonary compromise, postoperative gastrointestinal hemorrhage or ulceration, cellulitis or decubitus ulcer, septicemia, mechanical complications due to device or implant, miscellaneous complications, shock or cardiorespiratory arrest, infections, postoperative heart attack, postoperative cardiac abnormalities other than heart attack, postoperative derangement, coma, pneumonia, venous thrombosis or pulmonary embolism, hemorrhage, hip fracture, wound infection, iatrogenic complications, sentinel events, acute renal failure, stroke, and delirium. We also created several condition-specific clinical variables, listed in Table 1, including the type of fracture, stroke, or replacement.
Table 1.
Means of Characteristics
| Hip Fracture |
Stroke |
Joint Replacement |
||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Mean | SD |
| Demographics | ||||||
| Female | 0.783 | 0.412 | 0.598 | 0.490 | 0.652 | 0.476 |
| White | 0.936 | 0.245 | 0.843 | 0.364 | 0.927 | 0.261 |
| Black | 0.036 | 0.186 | 0.117 | 0.322 | 0.047 | 0.213 |
| Hispanic | 0.008 | 0.090 | 0.013 | 0.112 | 0.008 | 0.090 |
| 65≤age≤67 | 0.026 | 0.160 | 0.072 | 0.258 | 0.122 | 0.327 |
| 68≤age≤70 | 0.037 | 0.189 | 0.089 | 0.285 | 0.152 | 0.359 |
| 71≤age≤73 | 0.057 | 0.231 | 0.111 | 0.314 | 0.170 | 0.376 |
| 74≤age≤76 | 0.083 | 0.276 | 0.129 | 0.335 | 0.172 | 0.378 |
| 77≤age≤79 | 0.114 | 0.318 | 0.138 | 0.345 | 0.152 | 0.359 |
| 80≤age≤82 | 0.140 | 0.347 | 0.135 | 0.342 | 0.109 | 0.311 |
| 83≤age≤85 | 0.155 | 0.362 | 0.120 | 0.325 | 0.068 | 0.252 |
| 86≤age≤88 | 0.149 | 0.357 | 0.094 | 0.292 | 0.035 | 0.183 |
| Age>88 | 0.238 | 0.426 | 0.111 | 0.315 | 0.019 | 0.138 |
| Lives in an MSA | 0.713 | 0.452 | 0.711 | 0.453 | 0.692 | 0.462 |
| Lives adjacent to an MSA | 0.157 | 0.363 | 0.160 | 0.367 | 0.166 | 0.372 |
| Beneficiary is covered by Medicaid | 0.211 | 0.408 | 0.207 | 0.405 | 0.082 | 0.275 |
| Complications | ||||||
| Postoperative pulmonary compromise | 0.010 | 0.102 | 0.013 | 0.112 | 0.005 | 0.067 |
| Postoperative GI hemorrhage or ulceration | 0.007 | 0.082 | 0.010 | 0.098 | 0.003 | 0.051 |
| Cellulitis or decubitus ulcer | 0.021 | 0.143 | 0.017 | 0.130 | 0.005 | 0.072 |
| Septicemia | 0.003 | 0.059 | 0.008 | 0.088 | 0.001 | 0.037 |
| Mechanical complications due to device or implant | 0.008 | 0.091 | 0.006 | 0.077 | 0.014 | 0.116 |
| Miscellaneous complications | 0.023 | 0.149 | 0.002 | 0.043 | 0.032 | 0.176 |
| Shock or cardiorespiratory arrest | 0.001 | 0.038 | 0.002 | 0.041 | 0.001 | 0.030 |
| Infections | 0.000 | 0.018 | 0.001 | 0.030 | 0.000 | 0.008 |
| Postoperative heart attack (AMI) | 0.010 | 0.100 | 0.009 | 0.095 | 0.004 | 0.061 |
| Postoperative cardiac abnormalities other than AMI | 0.001 | 0.037 | 0.002 | 0.046 | 0.001 | 0.025 |
| Postoperative derangement | 0.001 | 0.037 | 0.000 | 0.018 | 0.001 | 0.034 |
| Coma | 0.003 | 0.057 | 0.006 | 0.080 | 0.002 | 0.040 |
| Pneumonia | 0.036 | 0.187 | 0.048 | 0.215 | 0.008 | 0.087 |
| Venous thrombosis or pulmonary embolism | 0.008 | 0.091 | 0.005 | 0.072 | 0.008 | 0.092 |
| Hemorrhage | 0.015 | 0.122 | 0.003 | 0.050 | 0.013 | 0.115 |
| Hip fracture | — | — | 0.005 | 0.073 | — | — |
| Wound infection | 0.002 | 0.047 | 0.001 | 0.027 | 0.002 | 0.046 |
| Iatrogenic complications | 0.047 | 0.212 | 0.003 | 0.053 | 0.050 | 0.218 |
| Sentinel events | 0.001 | 0.033 | 0.001 | 0.034 | 0.001 | 0.036 |
| Acute renal failure | 0.007 | 0.086 | 0.008 | 0.088 | 0.004 | 0.060 |
| Stroke | 0.006 | 0.075 | — | — | 0.002 | 0.041 |
| Delirium | 0.020 | 0.141 | 0.013 | 0.115 | 0.012 | 0.108 |
| Comorbidities | ||||||
| Cancer with a poor prognosis | 0.010 | 0.099 | 0.009 | 0.093 | 0.003 | 0.054 |
| Metastatic cancer | 0.006 | 0.075 | 0.008 | 0.090 | 0.001 | 0.031 |
| Chronic pulmonary disease | 0.172 | 0.377 | 0.126 | 0.332 | 0.100 | 0.300 |
| Coronary artery disease | 0.207 | 0.405 | 0.244 | 0.429 | 0.155 | 0.362 |
| Congestive heart failure | 0.169 | 0.375 | 0.162 | 0.368 | 0.055 | 0.228 |
| Peripheral vascular disease | 0.041 | 0.198 | 0.060 | 0.237 | 0.019 | 0.136 |
| Severe chronic liver disease | 0.004 | 0.064 | 0.003 | 0.052 | 0.002 | 0.039 |
| Diabetes with end organ damage | 0.015 | 0.120 | 0.033 | 0.178 | 0.008 | 0.087 |
| Chronic renal failure | 0.008 | 0.091 | 0.009 | 0.095 | 0.002 | 0.043 |
| Nutritional deficiencies | 0.022 | 0.146 | 0.020 | 0.138 | 0.002 | 0.049 |
| Dementia | 0.226 | 0.418 | 0.115 | 0.319 | 0.012 | 0.108 |
| Functional impairment | 0.047 | 0.212 | 0.297 | 0.457 | 0.009 | 0.096 |
| Diabetes without end organ damage | 0.134 | 0.341 | 0.232 | 0.422 | 0.126 | 0.332 |
| Composite measure of severity | 0.255 | 0.436 | 0.263 | 0.440 | 0.258 | 0.438 |
| Discharging hospital characteristics | ||||||
| Nonprofit hospital | 0.750 | 0.433 | 0.732 | 0.443 | 0.779 | 0.415 |
| Government hospital | 0.116 | 0.320 | 0.132 | 0.339 | 0.094 | 0.292 |
| Average daily census of hospital | 177.509 | 159.335 | 184.425 | 167.794 | 197.276 | 165.114 |
| Resident to ADC ratio of hospital | 0.100 | 0.204 | 0.112 | 0.227 | 0.129 | 0.234 |
| Percentage of low-income patients | 0.130 | 0.090 | 0.137 | 0.098 | 0.120 | 0.083 |
| % Medicare days | 0.492 | 0.124 | 0.495 | 0.131 | 0.480 | 0.123 |
| Case mix index of hospital | 1.440 | 0.227 | 1.435 | 0.247 | 1.520 | 0.242 |
| Condition-specific factors | ||||||
| Pertrochanteric fracture | 0.492 | 0.500 | — | — | — | — |
| Total hip replacement | 0.029 | 0.169 | — | — | 0.290 | 0.454 |
| Partial hip replacement | 0.332 | 0.471 | — | — | 0.019 | 0.138 |
| Total knee replacement | — | — | — | — | 0.582 | 0.493 |
| Knee revision | — | — | — | — | 0.051 | 0.220 |
| Hip revision | 0.002 | 0.040 | — | — | 0.059 | 0.235 |
| Hip replacement | — | — | — | — | 0.367 | 0.482 |
| Knee replacement | — | — | — | — | 0.632 | 0.482 |
| Bilateral procedure | — | — | — | — | 0.042 | 0.200 |
| Basilar artery infarct | — | — | 0.003 | 0.055 | — | — |
| Carotid, verterbral, or multiple artery | — | — | 0.063 | 0.243 | — | — |
| Hemorrhagic stroke | — | — | 0.073 | 0.261 | — | — |
ADC, average daily census; GI, gastrointestinal; MSA, metropolitan statistical area; SD, standard deviation.
The covariates in the models also included characteristics of the acute care hospital that can influence patterns of care and approaches to discharge planning in the hospital and, consequently, post-acute care use (Neu, Harrison, and Heilbrunn 1989; Steiner and Neu 1993; Blewett, Kane, and Finch 1995; Bronskill, Normand, and McNeil 2002;). These characteristics include size (average daily census [ADC]), teaching status (resident to ADC ratio), ownership status (government, private nonprofit, or for-profit), Medicare patient percentage, case mix index of the hospital, and low-income patient percentage.
Finally, to assess whether the changes in post-acute care payment systems had differential effects by patient severity, we also estimated versions of our models that interacted the payment policy indicator variables and time trends with a single indicator variable for the most severely ill patients, defined as those who have a high probability of death. We constructed this indicator variable using demographic and clinical variables to predict each patient's probability of death (top quartile of the distribution for their condition). We also included the indicator variable for the most severely ill patients in our models as a case-mix measure.
Statistical Analysis
Our regression analyses were based on estimating multinomial logistic regression models, which enabled us to incorporate multiple sites into a single choice model and estimate them jointly. The model was of the form
where  is the probability that a patient used post-acute care of type m given the vector of explanatory variables x,
is the probability that a patient used post-acute care of type m given the vector of explanatory variables x,  is the probability that a patient did not use any Medicare-covered post-acute care given the vector of explanatory variables x (i.e., b is the reference category), and βm|b are vectors of estimated coefficients. As discussed above, the vector of explanatory variables included a set of variables to capture the effects of the changes in payment policies superimposed on the underlying trend in use, patient demographic and clinical variables, and characteristics of the acute care hospital.
is the probability that a patient did not use any Medicare-covered post-acute care given the vector of explanatory variables x (i.e., b is the reference category), and βm|b are vectors of estimated coefficients. As discussed above, the vector of explanatory variables included a set of variables to capture the effects of the changes in payment policies superimposed on the underlying trend in use, patient demographic and clinical variables, and characteristics of the acute care hospital.
Because the results of multinomial regression models are difficult to visualize and interpret, we used the estimated coefficients to compute standardized predictions in which only payment system effects were varied across all the patients in the study and then predicted the probabilities of using IRF care, SNF care, and home health care (Lane and Nelder 1982).
RESULTS
Patients in our hip fracture, stroke, and joint replacement samples use post-acute care at high rates. In 2002, over 85 percent of hip fracture and joint replacement patients and about 70 percent of stroke patients used some type of Medicare-covered post-acute care. Roughly 22 percent of hip fracture patients and 33 percent of joint replacement patients used inpatient rehabilitation care. Hip fracture patients were much more likely to use skilled nursing care than stroke or joint replacement; stroke patients received home health care at a higher rate than hip fracture patients.
In examining the means of the variables we controlled for in the models, we found some key differences between the populations. The hip fracture sample is older—over half of the hip fracture patients are age 80 or older—and more heavily female, as expected. None of the three groups have a high level of complications, but all three groups have a substantial rate of comorbidities. These results are presented in Table 1.
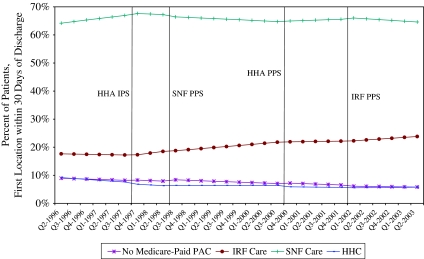
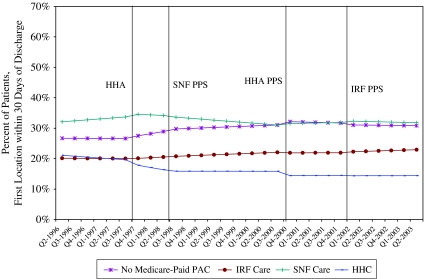
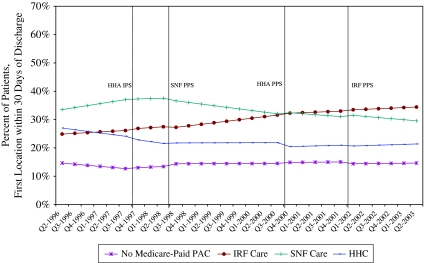
Table 2 presents the detailed results from our logistic regressions using pooled data for the period January 1996 through June 2003 for each condition. Because the signs and magnitudes of the effects are difficult to interpret from the multinomial logit regression output, we provide corresponding estimates of the changes in the probability of going to each post-acute location and standard errors on these estimates (in parentheses). A negative percentage in these columns indicates that the patient was less likely to go to that post-acute location after the payment system change noted in the row title. The implementation effect rows should be interpreted as the shift due to implementation while the time trend effects show the predicted change in the probability of going to that site in the postimplementation period, evaluated at the quarter following the implementation. The asterisks indicate significance levels, as footnoted on the table. In addition, we constructed Figures 1, 2, and 3 displaying case-mix-adjusted probabilities of use that visually display the effects of the payment systems.
Table 2.
Change in Predicted Probability to Site
| Hip Fracture Patients |
Stroke Patients |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | No Medicare- Paid PAC (Std. Error) | IRF (Std. Error) | SNF (Std. Error) | HHC (Std. Error) | No Medicare- Paid PAC (Std. Error) | IRF (Std. Error) | SNF (Std. Error) | HHC (Std. Error) |
| HHA interim payment system implementation effect (10/97) | 0.18% | 0.13% | 0.11% | −0.42%** | 0.85%** | 0.07% | 0.51% | −1.44%** |
| (0.0016) | (0.002) | (0.0026) | (0.0013) | (0.0023) | (0.0022) | (0.0026) | (0.0023) | |
| HHA interim payment system time trend effect | −0.02% | 0.68%** | −0.67%** | 0.01% | 0.73%** | 0.24%* | −0.53%** | −0.44%** |
| (0.001) | (0.0012) | (0.0013) | (0.0006) | (0.0013) | (0.0013) | (0.0016) | (0.0011) | |
| SNF prospective payment system implementation effect (7/98) | 0.59%* | −0.31% | −0.59%* | 0.31%* | 0.12% | 0.05% | −0.37% | 0.20% |
| (0.0024) | (0.0024) | (0.0033) | (0.0017) | (0.0031) | (0.0028) | (0.0034) | (0.0027) | |
| SNF prospective payment system time trend effect | 0.00% | −0.24%* | 0.00% | 0.23%** | −0.53%** | −0.06% | −0.16% | 0.75%** |
| (0.001) | (0.0011) | (0.0013) | (0.0008) | (0.0013) | (0.0012) | (0.0015) | (0.0014) | |
| HHA prospective payment system implementation effect (10/00) | 0.28%* | −0.23% | 0.38% | −0.44%** | 0.82%** | −0.28%* | 0.97%** | −1.51%** |
| (0.0014) | (0.0017) | (0.0023) | (0.0011) | (0.0019) | (0.0018) | (0.0022) | (0.0017) | |
| HHA prospective payment system time trend effect | −0.02% | −0.27%** | 0.34%** | −0.05% | −0.27%** | −0.16%** | 0.43%** | 0.00% |
| (0.0005) | (0.0005) | (0.0008) | (0.0003) | (0.0006) | (0.0006) | (0.0007) | (0.0006) | |
| IRF prospective payment system implementation effect (1/02) | −0.30%* | 0.05% | 0.34% | −0.08% | −0.47%* | 0.27% | 0.34% | −0.14% |
| (0.0016) | (0.0019) | (0.0027) | (0.0014) | (0.0021) | (0.0023) | (0.0026) | (0.0021) | |
| IRF prospective payment system time trend effect | 0.09%* | 0.20%** | −0.39%** | 0.10%* | 0.06% | 0.12% | −0.19%* | 0.01% |
| (0.0005) | (0.0007) | (0.0009) | (0.0004) | (0.0006) | (0.0008) | (0.0009) | (0.0006) | |
| Pseudo R2 | 0.0747 | 0.0865 | ||||||
| Percentage of PAC patients at this location (%) | 7.47 | 20.24 | 65.68 | 6.6 | 29.65 | 21.3 | 32.54 | 16.51 |
| Sample size (N) | 1,326,515 | 1,603,706 | ||||||
| Joint Replacement Patients |
||||||||
| Variable | No Medicare- Paid PAC (Std. Error) | IRF (Std. Error) | SNF (Std. Error) | HHC (Std. Error) | ||||
| HHA interim payment system implementation effect (10/97) | 0.54%** | 0.54%* | −0.51%* | −0.56%** | ||||
| (0.0011) | (0.0025) | (0.0026) | (0.0017) | |||||
| HHA interim payment system time trend effect | 0.48%** | 0.12% | −0.57%** | −0.04% | ||||
| (0.0008) | (0.0015) | (0.0016) | (0.0009) | |||||
| SNF prospective payment system implementation effect (7/98) | 0.58%** | −0.35% | −0.98%** | 0.75%** | ||||
| (0.0019) | (0.003) | (0.0032) | (0.0025) | |||||
| SNF prospective payment system time trend effect | −0.13%* | 0.27%* | −0.75%** | 0.60%** | ||||
| (0.0007) | (0.0013) | (0.0015) | (0.0009) | |||||
| HHA prospective payment system implementation effect (10/00) | 0.22%* | −0.04% | 1.06%** | −1.24%** | ||||
| (0.0009) | (0.0017) | (0.0019) | (0.0013) | |||||
| HHA prospective payment system time trend effect | 0.02% | −0.36%** | 0.26%** | 0.08%* | ||||
| (0.0003) | (0.0006) | (0.0007) | (0.0004) | |||||
| IRF prospective payment system implementation effect (1/02) | −0.49%** | 0.09% | 0.83%** | −0.43%* | ||||
| (0.001) | (0.0022) | (0.0025) | (0.0018) | |||||
| IRF prospective payment system time trend effect | 0.01% | 0.02% | −0.06% | 0.03% | ||||
| (0.0003) | (0.0007) | (0.0008) | (0.0005) | |||||
| Pseudo R2 | 0.0699 | |||||||
| Percentage of PAC patients at this location (%) | 14.29 | 30.13 | 33.41 | 22.17 | ||||
| Sample size (N) | 1,787,094 | |||||||
Notes: The comparison group is No Medicare-Paid PAC.
Significant at the 0.05 level.
Significant at the 0.001 level.
HHA, home health agency; IFR, inpatient rehabilitation facility; SNF, skilled nursing facility; Std. Error, standard error.
Figure 1.
Predicted Probabilities of Hip Fracture Patients Going to Each PAC Location, 1996–2003
Figure 2.
Predicted Probabilities of Stroke Patients Going to Each PAC Location, 1996–2003
Figure 3.
Predicted Probabilities of Joint Replacement Patients Going to Each PAC Location, 1996–2003
From the figures, we can see that the probability of patients with a hip fracture being discharged without Medicare-covered post-acute care versus inpatient rehabilitation, skilled nursing, or home health is falling over this time period, while increasing for stroke patients and remaining about the same for joint replacement patients. The probability of going to inpatient rehabilitation increased over time for all three conditions but was especially strongly for joint replacement patients. The probability of going to skilled nursing peaked at the beginning of 1998 for all three conditions, but it fell overall. The probability of using home health care declined for all three conditions, with notable declines associated with the implementation of the home health interim payment system and home health prospective payment.
The predictions from our multinomial logit models show significant changes in where patients went after discharge from acute care and how use was affected by the various post-acute payment systems implemented between 1996 and 2003. When the Balanced Budget Act mandated the implementation of the home health interim payment system in October 1997, the use of home health care went down for all three conditions immediately and continued to decline for stroke patients in the periods following implementation. The interim payment system was associated with an immediate reduction in the probability of hip fracture and joint replacement patients going to home health care of 0.4 and 0.6 percentage points, respectively. The interim payment system reduced the likelihood of a stroke patient going to home health by about 1.4 percent immediately and an additional 0.4 percent in the quarter after the payment system changed. There is evidence of a decrease in the use of skilled nursing on implementation of the home health interim payment system for joint replacement patients and for both stroke and joint replacement patients in the period following implementation.
With the implementation of the prospective payment in SNFs in July 1998 there was an immediate decline in skilled nursing use, which was significant for hip fracture and joint replacement patients. After the implementation, there was an increase in home health use for all three conditions.
The implementation of prospective payment for HHAs in October 2000 was associated with a large decrease in the use of home health care for all three conditions. The likelihood of going to home health after prospective payment decreased by 0.4 percent for hip fracture patients, 1.5 percent for stroke patients, and 1.2 percent for joint replacement patients. It was also associated with a decline in inpatient rehabilitation use for all conditions in the period following implementation and an increase in stroke and joint replacement patients' use of skilled nursing.
The implementation of the inpatient rehabilitation prospective payment system in January 2002 was associated with a decrease in the probability of not receiving post-acute care for all three conditions. The likelihood of going to an SNF increased immediately by 0.8 percent in joint replacement patients. For hip fracture patients, prospective payment was associated with a subsequent increase in the use of inpatient rehabilitation and a decline in use of skilled nursing.
We also ran a model that included interactions for more severely ill patients, with the payment system variables to see if their access was differentially affected by the changes in payment systems. Including these 10 interaction variables across three PAC location choices resulted in only a few weakly significant effects. The changes in the other coefficients, including the payment change variables, when these interactions were included were very small in magnitude and the effects were not qualitatively different. The results from these models are, therefore, not shown in the tables.
DISCUSSION
Our study found that choice of post-acute care site does react to Medicare payment system changes and that different post-acute settings do, to some extent, substitute for one another when incentives for admission are changed. However, these payment changes did not result in reduced post-acute care access for the severely ill. Our findings indicate that policy makers need to view post-acute care as one integrated market and plan payments and incentives accordingly. CMS has begun this process with the Post Acute Care Payment Reform Demonstration, the goal of which is to standardize patient assessment information across PAC settings and to use these data to guide payment policy in the Medicare program. Our analysis shows that many patients fall into a clinical gray area, where there is not an obvious medical choice for post-acute care site, and these patients are shifted across post-acute sites based on nonclinical factors, including payments and provider supply. We hope that the demonstration will produce data on which types of patients might benefit most from each post-acute care setting and what the cost differentials are between settings.
Although the effects of the payment systems on the use of post-acute care varied, most were as predicted and were consistent with the earlier literature. There was a marked decline in the use of home health care, with the implementation of the home health interim payment system, and another decline after implementation of the prospective payment system. These patients were mostly being shifted from skilled nursing and home health to no formal care during this time period, resulting in reduced Medicare expenditures. This marked continued decline in home health use after the implementation of the interim payment system, which was highly significant for stroke patients, can be explained by the following three factors. The interim payment system involved substantial fiscal cuts; it was implemented first and relatively quickly, leaving providers little time to adjust to it in advance; and there was a perception that the Balanced Budget Act foretold a general crackdown on all post-acute care. The prospective payment in SNFs was associated with lower use of skilled nursing care for hip fracture and joint replacement patients and increases over time in home health use for stroke and joint replacement patients. Some of the payment changes appeared to have immediate consequences for alternative sites, including the home health interim payment system, which was associated with less skilled nursing use for all conditions. Across the entire time period examined, the proportion of hip fracture and joint replacement patients receiving no formal care was relatively flat, but the proportion of stroke patients receiving no formal post-acute care increased. In addition, it is also interesting to note that the shifts in care described above were least significant and pronounced for hip fracture patients and most pronounced for stroke patients. These findings may be a cause for concern because stroke patients are the group for whom there is the most evidence that aggressive post-acute rehabilitation produces better outcomes (Kane et al. 1996, 1998; Kramer et al. 1997; Kane, Lin, and Blewett 2002).
Of course, there were unanticipated effects. For example, the decreases in SNF use around the home health care interim payment system (which were contrary to our hypothesis) were possibly due to over-expansion in the SNF industry and anticipatory effects of skilled nursing prospective payment. In addition, the declines in use of IRFs for hip fracture patients after skilled nursing prospective payment and the declines in all patients' use of inpatient rehabilitation after the home health prospective payment system was implemented were unexpected. Our models do not capture post-acute payment changes other than the major implementations of new payment systems, such as the Balanced Budget Refinement Act or the Benefits Improvement and Protection Act. Thus, the effects of these Acts may be partially captured by other indicators. In particular, the increases in skilled nursing use around the time of the home health and inpatient rehabilitation prospective payment systems or the decline in use of IRFs after the early payment changes may have resulted from these Acts and their payment supplements to SNFs.
There were virtually no differential effects for severely ill patients associated with any of the payment system changes. This is an important finding on its own as an unintended consequence of prospective payment may be selection (i.e., discrimination) against the sickest patients within a diagnosis group (Ellis and McGuire 1996). This finding went against our hypotheses and may be proof that the payment systems risk-adjust fairly well for case mix. While this is good news, continued attention should be given to this issue in the future.
There is room to improve on the methods we have used here in future research and to pursue the next logical steps in this line of inquiry. We investigated what happened with Medicare post-acute care nationally, but there were undoubtedly differential effects of the payment systems by market and provider type given the dramatic geographic variations in care patterns. It is also important to note that because these payment systems were implemented nationally, we are limited to an uncontrolled pre/postanalysis. Our data and methods thus allow us to look only at associations between payment changes and changes in realized access. In other words, we are not able to draw strong conclusions about the causal effects of payment changes on care use. Our findings apply to Medicare-funded post-acute care services and do not account for post-acute services paid for by Medicaid, private insurance, community resources, or patients. An important extension of these analyses will be to study the effect of prospective payment on varying types of providers (e.g., freestanding versus hospital-based providers) in different markets (e.g., by level of competition or rural status).
In addition, our model specification is based on a number of assumptions. It assumes that a linear time trend and seasonal dummies can capture prechange effects. Most importantly, it assumes that the payment system changes have ongoing, incremental, linear effects in all the periods after they are implemented. Thus, for example, it assumes that the effects of later payment changes such as the IRF PPS should be measured only after controlling for the implementation and unfolding effects of all of the prior PPSs. It also assumes that the payment changes we did not include in the model, such as the outpatient hospital PPS, do not affect the care patterns we examined. In addition, we do not control for changes in post-acute provider supply over time because changes in supply may be endogenous in our models.
This study demonstrates the fact that post-acute care should be viewed as one market and incentives introduced in one setting may affect other post-acute care sites. It is thus important that all of the changes associated with the PAC payment reforms be studied in the context of changes in patient costs and outcomes. For example, declines in the use of any given post-acute site would be of greatest concern if they were associated with poorer patient outcomes overall. In addition, it should be noted that these analyses cover only the early stages of the implementation of the new PAC payment systems. Ongoing monitoring of their effects is also warranted.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors would like to acknowledge comments and assistance from Mark Totten, Dan Relles, Susan Paddock, Barbara Wynn, and the rest of the IRF PPS project team at RAND. The analyses on which this publication is based were performed under Contract 500-2004-00033C, entitled “Inpatient Rehabilitation Facility Prospective Payment System Monitoring, Access, and Refinements,” funded by the Centers for Medicare and Medicaid Services, Department of Health and Human Services. The contents of this publication do not necessarily reflect the views or policies of the Department of Health and Human Services nor does the mention of trade names, commercial products, or organizations imply endorsement by the U.S. government. The author assumes full responsibility for the accuracy and completeness of the ideas presented. The RAND Corporation is a nonprofit research organization providing objective analysis and effective solutions that address the challenges facing the public and private sectors around the world. RAND's publications do not necessarily reflect the opinions of its research clients and sponsors. No other disclosures.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- American Hospital Association (AHA) Statement by the Payment Systems for Medicare's Home Health Benefit. Hearing before the Subcommittee on Health of the Committee on Ways and Means, House of Representatives, August 6, 1998. 105th Congress, second session, serial no. 105–109, p. 174.
- Angelelli J, Gifford D, Intrator O, Gozalo P, Laliberte L, Mor V. Access to Postacute Nursing Home Care before and after the BBA. Balanced Budget Act. Health Affairs. 2002;21(5):254–64. doi: 10.1377/hlthaff.21.5.254. [DOI] [PubMed] [Google Scholar]
- Aronow WS, Ahn C. Elderly Nursing Home Patients with Congestive Heart Failure after Myocardial Infarction Living in New York City Have a Higher Prevalence of Mortality in Cold Weather and Warm Weather Months. Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59A:146–7. doi: 10.1093/gerona/59.2.m146. [DOI] [PubMed] [Google Scholar]
- Blewett LA, Kane RL, Finch M. Hospital Ownership of Post-Acute Care: Does it Increase Access to Post-Acute Care Services? Inquiry. 1995;32(4):457–67. [PubMed] [Google Scholar]
- Bronskill SE, Normand SL, McNeil BJ. Post-Acute Service Use Following Acute Myocardial Infarction in the Elderly. Health Care Financing Review. 2002;24(2):77–93. [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Datar Garten A, Paddock S, Saliba D, Totten M, Escarce JJ. How Much Is Post-Acute Care Use Affected by Its Availability? Health Services Research. 2005;40(2):413–34. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter GM, Buntin MB, Hayden O, Paddock SM, Relles DA, Ridgeway G, Totten MA, Wynn BO. Analyses for the Initial Implementation of the Inpatient Rehabilitation Facility Prospective Payment System. Santa Monica, CA: RAND; 2002. [Google Scholar]
- Chan L, Koepsell TD, Deyo RA, Esselman PC, Haselkorn JK, Lowery JK, Stolov WC. The Effect of Medicare's Payment System for Rehabilitation Hospitals on Length of Stay, Charges, and Total Payments. New England Journal of Medicine. 1997;337(14):978–85. doi: 10.1056/NEJM199710023371406. [DOI] [PubMed] [Google Scholar]
- Cotterill PG, Gage BJ. Medicare Post-Acute Care Since the Balanced Budget Act of 1997. Health Care Financial Review. 2002;24(2):1–6. [PMC free article] [PubMed] [Google Scholar]
- DeJong G, Palsbo SE, Beatty PW, Jones GC, Kroll T, Neri MT. The Organization and Financing of Health Services for Persons with Disabilities. Milbank Quarterly. 2002;2:261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubay LC. Comparison of Rural and Urban Skilled Nursing Facility Benefit Use. Health Care Financial Review. 1993;14(4):25–37. [PMC free article] [PubMed] [Google Scholar]
- Ellis RP, McGuire TG. Hospital Response to Prospective Payment: Moral Hazard, Selection, and Practice-Style Effects. Journal of Health Economics. 1996;15(3):257–77. doi: 10.1016/0167-6296(96)00002-1. [DOI] [PubMed] [Google Scholar]
- Finlayson M. Changes Predicting Long-Term Care Use among the Oldest-Old. Gerontologist. 2002;42(4):443–53. doi: 10.1093/geront/42.4.443. [DOI] [PubMed] [Google Scholar]
- FitzGerald JD, Mangione CM, Boscardin J, Kominski G, Hahn B, Ettner SL. Impact of Changes in Medicare Home Health Care Reimbursement on Month-to-Month Home Health Utilization between 1996–2001 for a National Sample of Patients Undergoing Orthopedic Procedures. Medical Care. 2006;44(9):870–8. doi: 10.1097/01.mlr.0000220687.92922.64. [DOI] [PubMed] [Google Scholar]
- Gage B. Impact of the BBA on Post-Acute Utilization. Health Care Financial Review. 1999;20(4):103–26. [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI, Daley J, Heeren T, Foley SM, Fisher ES, Duncan C, Hughes JS, Coffman GA. Identifying Complications of Care Using Administrative Data. Medical Care. 1994;32(7):700–15. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- Jette AM, Keysor JJ. Uses of Evidence in Disability Outcomes and Effectiveness Research. Milbank Quarterly. 2002;2:325–45. doi: 10.1111/1468-0009.t01-1-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane RL, Chen Q, Finch M, Blewett L, Burns R, Moskowitz M. Functional Outcomes of Posthospital Care for Stroke and Hip Fracture Patients under Medicare. Journal of the American Geriatrics Society. 1998;46(12):1525–33. doi: 10.1111/j.1532-5415.1998.tb01537.x. [DOI] [PubMed] [Google Scholar]
- Kane RL, Finch M, Blewett L, Chen Q, Burns R, Moskowitz M. Use of Post-Hospital Care by Medicare Patients. Journal of the American Geriatrics Society. 1996;44(3):242–50. doi: 10.1111/j.1532-5415.1996.tb00909.x. [DOI] [PubMed] [Google Scholar]
- Kane RL, Lin WC, Blewett LA. Geographic Variation in the Use of Post-Acute Care. Health Services Research. 2002;37(3):667–82. doi: 10.1111/1475-6773.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan S. Growth and Payment Adequacy of Medicare Postacute Care Rehabilitation. Archives of Physical Medicine and Rehabilitation. 2007;88(11):1494–9. doi: 10.1016/j.apmr.2007.08.112. [DOI] [PubMed] [Google Scholar]
- Kenney GM, Dubay LC. Explaining Area Variation in the Use of Medicare Home Health Services. Medical Care. 1992;30(1):43–57. doi: 10.1097/00005650-199201000-00004. [DOI] [PubMed] [Google Scholar]
- Komisar HL. Rolling Back Medicare Home Health. Health Care Financial Review. 2002;24(2):33–55. [PMC free article] [PubMed] [Google Scholar]
- Kramer AM, Steiner JF, Schlenker RE, Eilertsen TB, Hrincevich CA, Tropea DA, Ahmad LA, Eckhoff DG. Outcomes and Costs after Hip Fracture and Stroke. A Comparison of Rehabilitation Settings. Journal of the American Medical Association. 1997;277(5):396–404. [PubMed] [Google Scholar]
- Laake K, Sverre JM. Winter Excess Mortality: A Comparison between Norway and England Plus Wales. Age and Ageing. 1996;25(5):343–8. doi: 10.1093/ageing/25.5.343. [DOI] [PubMed] [Google Scholar]
- Lane PW, Nelder JA. Analysis of Covariance and Standardization as Instances of Prediction. Biometrics. 1982;38:613–21. [PubMed] [Google Scholar]
- Lee AJ, Huber JH, Stason WB. Factors Contributing to Practice Variation in Post-Stroke Rehabilitation. Health Services Research. 1997;32(2):197–221. [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Leake B, Leal-Sotelo M, Clark V. The Initial Effects of the Prospective Payment System on Nursing Home Patients. American Journal of Public Health. 1987;77(7):819–21. doi: 10.2105/ajph.77.7.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin W, Kane RL, Mehr DR, Madsen RW, Petroski GF. Changes in the Use of Postacute Care during the Initial Medicare Payment Reforms. Health Services Research. 2006;41(4):1338–56. doi: 10.1111/j.1475-6773.2006.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Wissoker D, Rimes C. Determinants and Costs of Medicare Post-Acute Care Provided by SNFs and HHAs. Inquiry. 1998;35(1):49–61. [PubMed] [Google Scholar]
- Manton KG, Woodbury MA, Vertrees JC, Stallard E. Use of Medicare Services before and after Introduction of the Prospective Payment System. Health Services Research. 1993;28(3):269–92. [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Reforming Medicare Payment: Early Effects of the 1997 Balanced Budget Act on Post-Acute Care. Milbank Quarterly. 2003a;81(2):277–303. doi: 10.1111/1468-0009.t01-1-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall N, Petersons A, Moore S, Korb J. Utilization of Home Health Services before and after the Balanced Budget Act of 1997: What Were the Initial Effects? Health Services Research. 2003b;38(1):85–106. doi: 10.1111/1475-6773.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC; 2002. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Variation and Innovation in Medicare. Washington, DC: MedPAC; 2003a. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC; 2003b. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC; 2006. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: MedPAC; 2007. [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) A Data Book: Healthcare Spending and the Medicare Program. Washington, DC: MedPAC; 2008. [Google Scholar]
- Neu CR, Harrison SC, Heilbrunn JZ. Medicare Patients and Postacute Care: Who Goes Where? Santa Monica, CA: RAND; 1989. [Google Scholar]
- Shatto A. Comparing Medicare Beneficiaries, by Type of Post-Acute Care Received: 1999. Health Care Financial Review. 2002;24(2):137–42. [PMC free article] [PubMed] [Google Scholar]
- Steiner A, Neu CR. Monitoring the Changes in Use of Medicare Posthospital Services. Report Prepared for the Health Care Financing Administration. Santa Monica, CA: RAND; 1993. [Google Scholar]
- Stineman MG. Prospective Payment, Prospective Challenge. Archives of Physical Medicine and Rehabilitation. 2002;83:1802–5. doi: 10.1053/apmr.2002.36067. [DOI] [PubMed] [Google Scholar]
- Street D, Quadagno J, Parham L, McDonald S. Reinventing Long-Term Care: The Effect of Policy Changes on Trends in Nursing Home Reimbursement and Resident Characteristics—Florida, 1989–1997. Gerontologist. 2003;43(2):118–31. doi: 10.1093/geront/43.suppl_2.118. [DOI] [PubMed] [Google Scholar]
- Swan JH, Benjamin AE. Medicare Home Health Utilization as a Function of Nursing Home Market Factors. Health Services Research. 1990;25(3):479–500. [PMC free article] [PubMed] [Google Scholar]
- White C. Rehabilitation Therapy in Skilled Nursing Facilities: Effects of Medicare's New Prospective Payment System. Health Affairs. 2003;22(3):214–23. doi: 10.1377/hlthaff.22.3.214. [DOI] [PubMed] [Google Scholar]
- Young DA. Princeton, NJ: Post-Acute Care. Paper Presented at the Princeton Conference on Medicare Reform. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.