Abstract
Background
Significant variation in regional utilization of home health (HH) services has been documented. Under Medicare's Home Health Interim and Prospective Payment Systems, reimbursement policies designed to curb expenditure growth and reduce regional variation were instituted.
Objective
To examine the impact of Medicare reimbursement policy on regional variation in HH care utilization and type of HH services delivered.
Research Design
We postulated that the reimbursement changes would reduce regional variation in HH services and that HH agencies would respond by reducing less skilled HH aide visits disproportionately compared with physical therapy or nursing visits. An interrupted time-series analysis was conducted to examine regional variation in the month-to-month probability of HH selection, and the number of and type of visits among HH users.
Subjects
A 100 percent sample of all Medicare recipients undergoing either elective joint replacement (1.6 million hospital discharges) or surgical management of hip fracture (1.2 million hospital discharges) between January 1996 and December 2001 was selected.
Results
Before the reimbursement changes, there was great variability in the probability of HH selection and the number of HH visits provided across regions. In response to the reimbursement changes, though there was little change in the variation of probability of HH utilization, there were marked reductions in the number and variation of HH visits, with greatest reductions in regions with highest baseline utilization. HH aide visits were the source of the baseline variation and accounted for the majority of the reductions in utilization after implementation.
Conclusions
The HH interim and prospective payment policies were effective in reducing regional variation in HH utilization.
Keywords: Medicare, home health care, regional variation
Between 1986 and 1996, there was dramatic growth in Medicare home health (HH) utilization, increasing from $2.6 billion per year (3 percent of Medicare Part A expenditures) to $17.5 billion per year (13 percent of Part A expenditures). This resulted from growth in both the annual number of beneficiaries served (increasing from 1.6 to 3.6 million) and the average number of annual visits per beneficiary (increasing from 23 to 79 visits per beneficiary) (105th Congress United States of America 1998).
At the same time it was noted that there was significant regional variation in utilization of HH services (Kenney and Dubay 1992; Welch, Wennberg, and Welch 1996; McCall et al. 2001;). Welch, Wennberg, and Welch (1996) reported greater variation in utilization of HH services than either skilled nursing days, hospital days, physician services, or hospital admissions, leading the authors to conclude that there was no “national consensus on whether and, if so, how often to use HH care.”
The significant regional variation raised concern within Congress and at the Office of Inspector General (OIG) that much of this regional variation could be attributable to either inefficient or fraudulent practices. Beginning July 1995, the OIG working with other agencies initiated Operation Restore Trust, a five-state (California, Florida, Illinois, New York, and Texas) audit that documented examples of fraud and abuse (Health Care Financing Administration 1995). The program was expanded nationwide in 1997.
In addition to these regulatory efforts, Congress passed the Balanced Budget Act of 1997, and the Centers for Medicare and Medicaid Services (CMS) implemented the HH Interim Payment System (IPS) on October 1, 1997 (with refinements starting October 1, 1998), and the HH Prospective Payment System (PPS) on October 1, 2000 (105th Congress United States of America 1997).
The IPS reduced the aggregate per-visit limit on payments from 112 percent of national mean historical costs to 105 percent of the national median costs. As per-visit limits do little to control the growth in number of visits per beneficiary, per-beneficiary limits were also implemented.
These per-beneficiary limits were partly designed to also reduce regional variation (105th Congress United States of America 1998). This was accomplished by blending agencies' historical mean per-beneficiary cost with standardized regional per-beneficiary costs, thereby driving limits toward regional means. (See Table S1 in the appendix for details.) These policies were phased-in based on each agency's fiscal year end. Under the PPS, implemented on October 1, 2000, HH care was organized into 60-day episodes of care for HH resource groups (HHRGs) (Health Care Financing Administration 2000).
The Congressional Medicare Payment Advisory Commission (MEDPAC) and several independent groups have described reductions in HH care after implementation of the IPS and PPS policies (MEDPAC 1999; McCall et al. 2001, 2003a, 2003b; Komisar 2002; Schwartz et al. 2002; Liu, Long, and Dowling 2003; Murkofsky et al. 2003; Murtaugh et al. 2003; Spector, Cohen, and Pesis-Katz 2004).
In our prior analyses focusing on postacute care HH patients, we reported the reduction in HH utilization for patients undergoing major orthopedic surgery (FitzGerald et al. 2006). We expand upon these prior analyses to examine how these changes in reimbursement policy affected regional variation over time, as well as how the reimbursement changes affected the mix of skilled HH services delivered.
METHODS
Patient Selection
As described in more detail in our prior studies (FitzGerald et al. 2007), we opted to select a 100 percent national sample for two well-defined cohorts that are commonly associated with postacute care. This permitted sufficient power to conduct month-to-month analyses across the various Balanced Budget Act policy periods between 1996 and 2001 so that policy implementation dates could be better correlated with temporal changes in utilization.
We selected patients undergoing elective joint replacement surgery (JR) as a group that ought to be sensitive to policy changes given the high degree of clinical discretion about the venue of postacute care. We also selected patients undergoing surgical repair of hip fracture (FX) as they undergo similar procedures yet are a more vulnerable group of patients. Before implementation of the IPS, 61 percent of JR and 43 percent of FX patients received HH care during the 120-day postoperative period (FitzGerald et al. 2006).
Patients undergoing JR surgery were identified by diagnosis-related groups (DRGs) codes 209 and 471. Verification of surgery and inclusion in the study sample was confirmed by ICD-9 procedure codes 81.51–81.55. Patients undergoing joint replacement for clearly nonelective reasons were excluded from this sample (e.g., infection or major trauma, 12 percent of all JR patients). Sensitivity analyses conducted using the full JR sample did not meaningfully change findings and therefore only results for the clinically defined elective JR sample are presented.
Patients undergoing surgical repair of hip fracture were identified with an ICD-9 diagnosis of 820.xx in any 1 of the 10 diagnostic code positions. Surgical repair of hip fracture was confirmed with the hip replacement codes 81.51–81.53 or pinning codes 79.35, 79.15, or 78.55. Patients treated nonsurgically for hip fracture were excluded.
Descriptors of the patient population are described in the appendix in Table S3.
Data Source
Medicare claims were obtained for all acute care hospital admissions, related skilled nursing facility (SNF), rehabilitation hospital (RH), and HH bills for patients undergoing either joint replacement surgery or surgical repair of hip fracture between January 1, 1996, and December 31, 2001. Acute care hospital, RH, and SNF claims were abstracted from the Medicare Provider Analysis and Review (MEDPAR). HH claims were abstracted from the HH Standard Analytic File.
Dependent Variables
Probability of HH Utilization
Admission to HH care was identified to begin within 7 days of discharge from either the acute care hospital or one of the contiguous postacute care institutions (SNF or RH). Patients meeting the above criteria were defined as receiving HH care. Trends in the probability of HH care were initially analyzed separately for patients discharged directly to HH and for patients receiving HH care following an SNF or RH stay. As there was no difference in change in regional variation by type of HH admission, these patient groups were combined into a single measure (any HH use) for the final models.
Number of HH Visits
To parallel the 60-day PPS reimbursement structure and to capture the majority of postacute HH care provided after inpatient surgery, 60- and 120-day episodes of care were created. Episodes terminated with either the end of the 60- or 120-day interval, rehospitalization, death, or a break in service >7 days. When the HH claim “to” and “from” dates straddled the end date of the episode, the number of visits was prorated proportionally. HH care was completed within 60 and 120 days of HH admission, respectively, for 93 and 98 percent of patients undergoing JR and for 80 and 93 percent of FX patients. As regional and temporal variation based on either the 60- or 120-day episodes were similar, only the latter estimates are presented.
Type of HH Visits
Type of HH visit (physical therapy, nursing service vs. HH aide) was extracted from the HH standard analytic files. Before July 1999, the revenue center line item reported the number of visits corresponding to the type of service. Thereafter the methodology changed to reflect 15-minute intervals and under PPS certain revenue center codes were deleted. For the analysis of service type, we elected to focus on the Interim Payment Policy period (October 1997–October 1998), when the largest reduction in HH services occurred and CMS used a uniform methodology for identifying type of HH service.
Independent Variables
To describe regional variation over time, we first describe detailed regional (state-by-state) variation in HH utilization using select timepoints correlating with change in reimbursement policy (e.g., pre-IPS, IPS, refined IPS, and PPS) presented on maps of the United States.
The 10 CMS regions are used to summarize regional variation in order to describe detailed temporal (month-to-month) variation in HH utilization. Each CMS region includes several states. CMS identifies each region by the city where the regional office is located. (See Figure S1, map of the United States, in the appendix for descriptions of the CMS regions.)
We then describe detailed temporal (month-to-month) variation in HH use for the CMS regions. Monthly trends in regional HH utilization are based on regression analyses that included 67 binary calendar month indicators (March 1996–September 2001) that represent the month of admission to HH care after the inpatient or last contiguous institutional discharge, with March 1996 used as the reference. (As the sample frame was selected based on date of the acute care hospitalization, using 120-day episodes, the first two and last three months of HH data contain incomplete episodes and are dropped from the study.)
Throughout the text and in the tables, results were derived using four spline variables to separately represent each of the four policy periods in place of the monthly calendar variables. (Spline variables describe the average change across the policy period and smooth month-to-month variation; Marsch and Cormier 2001.)
Other Covariates
The analyses controlled for patient, institutional, HH, and regional characteristics as follows.
Patient Covariates
Patient demographic factors included age at the time of surgery (by pentile), gender, and race (Caucasian, African American, or other). Patient socioeconomic status was estimated using the 2000 U.S. Census reported median income in the patient's zipcode of residence after matching patient and Census zip codes. Patient receipt of state aid (e.g., dual eligible patients where states elect to buy into Medicare benefits on behalf of patients) was also included in the models.
Patient medical characteristics included original reason for Medicare entitlement (aged, disabled, end-stage renal disease, or disabled and end-stage renal disease). Medical comorbidities identified from the 10 MEDPAR diagnostic codes were categorized into 19 categories using the Charlson comorbidity index (Deyo, Cherkin, and Ciol 1992).
Surgical characteristics varied by indication. For patients undergoing JR, the indications included hip vs. knee and revision vs. primary replacement. For FX patients, the indications included replacement vs. pinning and whether in-hospital complications were noted (DRG 210 vs. 211).
Institutional Covariates
For probability of selection models, the analyses adjusted for characteristics of the discharging inpatient, SNF, or RH institution. The institutional characteristics included teaching status (acute care hospital only), profit status, day of discharge, relative size (within own venue of care), and rural vs. urban status.
HH Covariates
For the number of HH visit models, the analyses adjusted for characteristics of the HH provider. Characteristics included HH profit status, the age of HH agency, and whether it operated under a certificate of need or simple business licensure.
Other Regional Covariates
Postacute care supply variables by zip code (number of SNF beds, RH beds, HH nurses, and HH aides) were matched to hospital zip codes. All values were per capita adjusted by including the per zip code total population aged 65 years or older in the model using the 2000 U.S. Census data. The county-level Medicare managed care market penetration rates for 1999 reported by the Centers for Medicare and Medicaid Statistics were also included (Centers for Medicare & Medicaid Services 1999).
Statistical Analysis
Probability of HH Utilization
The probability of HH utilization accounting for the clustering of patients within the discharging inpatient facility was modeled using nested logistic regression models. (See Figure S2 in appendix.) Upper and lower bounds of the estimates were calculated using bootstrap methodology (500 iterations) (Efron and Tibshirani 1993; Mooney and Duval 1993;).
Number of HH Visits
The numbers of HH visits per 60- or 120-day episode of HH care were modeled using linear regressions with random effects for HH agency. As results from 60- and 120-day analyses were similar, only results from 120-day analyses are presented.
All models adjusted for patient demographic, clinical, socioeconomic, regional, and institutional covariates. Due to the large size of the study cohort, estimates were deemed significant only when p<.0001 or when the absolute upper or lower limits of the bootstrap estimate distribution (as described above) did not include the value tested in the null hypothesis. STATA version 7.0 (STATA 2002) was used to perform all statistical analyses. All cartography was created using ArcGIS version 9.2 (ArcGIS 2007).
RESULTS
Sample Descriptions
From the MEDPAR database, 1,567,779 JR cases (for indication other than hip fracture) with hospital discharge dates between March 1, 1996, and September 30, 2001, were identified. In all, 102 patients died before discharge. A total of 186,659 discharges (12 percent) were excluded where the elective nature of the surgery was unclear from the coded diagnoses (including a majority of revisions). An additional 9,674 patients were excluded who had atypical billings where the type of postacute care could not be easily identified. Sensitivity analyses with and without the above exclusions did not reveal meaningful differences, and results for the more tightly defined cohort are presented. For the number of HH visits, 228 patients were excluded who died either while at SNF or RH or within 7 days of discharge (and no HH care provided). (See Figure S2 in appendix for summary data flow.)
A total of 1,164,946 cases of hip fracture treated surgically were identified. Patients who died before hospital discharge (n=628), whose postacute care venue was unclear (n=6,147), or who died either while at SNF or RH or within 7 days of discharge (n=9,158) were excluded from analysis.
Discharges with missing covariate data (3–6 percent of data depending upon the covariates included) were dropped from analyses.
Probability of HH Selection
Although probability of HH selection varied by region, there was little regional variation in responsiveness to changes in reimbursement policies.
Elective Joint Replacement
Probability of HH selection varied by region with the highest probabilities of selection in March 1996 in Boston, Atlanta, and San Francisco regions (73, 69, and 69 percent, respectively), and the lowest probabilities were in the Chicago, Seattle, and Kansas City regions (52, 53, and 54 percent, respectively), with the national mean at 61 percent (Table 1). As previously reported (FitzGerald et al. 2006), under IPS, the national mean fell from 61 percent in March 1996 to 54 percent in October 1998, thereafter remaining essentially flat through September 2001. There was little variation in responsiveness to the policy across regions. Thus, by September 2001, the same regions occupied the top three and bottom three rankings, with the exception of Dallas surpassing Kansas City in the bottom rankings.
Table 1.
Adjusted* Proportion of Patients Receiving Home Health (HH) Care after Inpatient Orthopedic Surgery†,‡
| After Elective Joint Replacement Surgery |
After Surgical Treatment for Hip Fracture |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mar-96 | Oct-97 | Oct-98 | Oct-00 | Sep-01 | Mar-96 | Oct-97 | Oct-98 | Oct-00 | Sep-01 | |
| National | 0.61 | 0.61 | 0.54 | 0.55 | 0.54 | 0.44 | 0.43 | 0.35 | 0.41 | 0.39 |
| CMS region (Difference from national mean) | ||||||||||
| Boston | 0.73 | 0.74 | 0.66 | 0.70 | 0.67 | 0.46 | 0.46 | 0.39 | 0.45 | 0.45 |
| (+0.12) | (+0.13) | (+0.12) | (+0.14) | (+0.14) | (+0.02) | (+0.03) | (+0.04) | (+0.04) | (+0.05) | |
| Atlanta | 0.69 | 0.67 | 0.59 | 0.62 | 0.60 | 0.50 | 0.47 | 0.38 | 0.47 | 0.45 |
| (+0.08) | (+0.05) | (+0.05) | (+0.07) | (+0.06) | (+0.05) | (+0.05) | (+0.03) | (+0.05) | (+0.05) | |
| San Francisco | 0.69 | 0.69 | 0.64 | 0.67 | 0.65 | 0.52 | 0.51 | 0.43 | 0.50 | 0.48 |
| (+0.07) | (+0.08) | (+0.09) | (+0.12) | (+0.12) | (+0.08) | (+0.08) | (+0.08) | (+0.08) | (+0.09) | |
| Philadelphia | 0.67 | 0.67 | 0.62 | 0.62 | 0.58 | 0.44 | 0.43 | 0.38 | 0.43 | 0.41 |
| (+0.06) | (+0.06) | (+0.07) | (+0.06) | (+0.04) | (+0.00)§ | (+0.00)§ | (+0.02) | (+0.01) | (+0.01) | |
| New York | 0.66 | 0.64 | 0.55 | 0.56 | 0.55 | 0.50 | 0.46 | 0.42 | 0.46 | 0.45 |
| (+0.05) | (+0.03) | (+0.01)§ | (+0.00)§ | (+0.01)§ | (+0.06) | (+0.04) | (+0.06) | (+0.04) | (+0.05) | |
| Dallas | 0.57 | 0.56 | 0.47 | 0.46 | 0.45 | 0.43 | 0.42 | 0.33 | 0.37 | 0.35 |
| (−0.05) | (−0.05) | (−0.08) | (−0.09) | (−0.09) | (−0.01) | (−0.01) | (−0.02) | (−0.04) | (−0.05) | |
| Denver | 0.56 | 0.57 | 0.52 | 0.51 | 0.48 | 0.39 | 0.38 | 0.33 | 0.37 | 0.33 |
| (−0.06) | (−0.04) | (−0.03) | (−0.04) | (−0.06) | (−0.05) | (−0.04 | (−0.03) | (−0.04 | (−0.06) | |
| Kansas City | 0.54 | 0.56 | 0.50 | 0.51 | 0.51 | 0.31 | 0.33 | 0.26 | 0.31 | 0.29 |
| (−0.08) | (−0.05) | (−0.04) | (−0.04) | (−0.03) | (−0.13) | (−0.09) | (−0.10) | (−0.10) | (−0.10) | |
| Seattle | 0.53 | 0.54 | 0.49 | 0.50 | 0.48 | 0.45 | 0.44 | 0.37 | 0.43 | 0.41 |
| (−0.08) | (−0.07) | (−0.06) | (−0.06) | (−0.06) | (+0.01) | (+0.01) | (+0.02) | (+0.02) | (+0.02) | |
| Chicago | 0.52 | 0.53 | 0.46 | 0.46 | 0.46 | 0.36 | 0.35 | 0.28 | 0.33 | 0.31 |
| (−0.09) | (−0.09) | (−0.09) | (−0.10) | (−0.07) | (−0.09) | (−0.08) | (−0.08) | (−0.08) | (−0.08) | |
Multivariate analyses adjusted for patient, institutional, HH, and regional covariates as outlined in Methods section.
Regions sorted by proportion of HH utilization after elective joint replacement surgery during March 1996.
All regional monthly estimates significantly different than the corresponding national estimate as assessed by bootstrap except where noted by § symbol.
Hip Fracture
Similar findings were observed for the hip fracture population. There was variation by region in baseline utilization but little variation in response to the policy changes. The highest probabilities of selection were in the San Francisco, New York, and Atlanta regions (52, 50, and 50 percent, respectively) and the lowest probabilities in the Kansas City, Chicago, and Denver regions (31, 36, and 39 percent, respectively), with the national mean at 44 percent. As previously reported, under IPS, the national mean fell to 35 percent, recovering to 41 percent by October 2000 and then falling again slightly to 39 percent by September 2001 (FitzGerald et al. 2006). There was remarkably little variation in response to the policy across regions, so that by September 2001 the regions had the same rank order and only two regions had briefly changed internal rank order during the follow-up before returning to the original rank order.
Number of HH Visits during a 120-Day Episode of Care
Elective Joint Replacement
As documented by other authors, there had been significant variation in utilization of HH services before the reimbursement changes (McCall et al. 2001, 2003a, b; Komisar 2002; Liu, Long, and Dowlingy 2003; Murkofsky et al. 2003; Murtaugh et al. 2003; Schlenker, Powell, and Goodrich 2005).
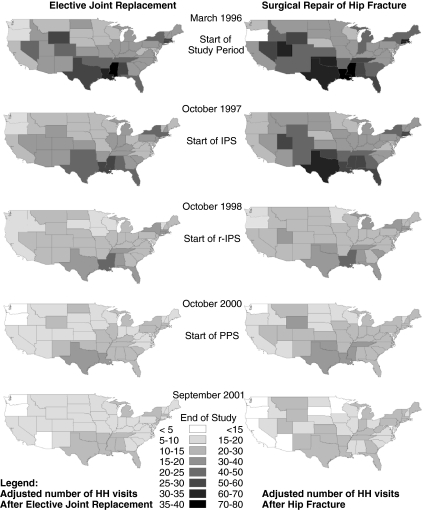
The maps in Figure 1 illustrate that in March 1996, for JR patients HH agencies were providing on average >20 visits per 120-day episode of HH care in 75 percent of illustrated states. There was a significant drop in the mean number of HH visits after implementation of the IPS, with agencies now providing an average of >20 visits per episode in only 21 percent of states. After implementation of PPS, there was further reduction, so that no states had an average of 20 or more visits per episode of HH care.
Figure 1.
Adjusted Number of Visits among Home Health Users during 120-Day Episode of Care by State
Looking at the variation across regions defined by CMS, in March 1996, the adjusted mean number of HH visits per 120-day episode of HH care was 31.4 in the Dallas region but only 14.9 in the Seattle region (Table 2 and Figure 2a). In other words, the Dallas HH agencies were providing an additional 7.4 visits over the national mean of 24.0 visits (1.31 times greater), while Seattle HH agencies were providing 9.0 fewer visits than the national mean (0.62 times lower).
Table 2.
| After Elective Joint Replacement Surgery |
After Surgical Treatment for Hip Fracture |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mar-96 | Oct-97 | Oct-98 | Oct-00 | Sep-01 | Mar-96 | Oct-97 | Oct-98 | Oct-00 | Sep-01 | |
| National | 24.0 | 21.5 | 18.0 | 15.6 | 14.1 | 47.1 | 43.7 | 33.6 | 28.9 | 24.3 |
| CMS region (Difference from national mean) | ||||||||||
| Dallas | 31.4 | 28.3 | 21.2 | 19.5 | 17.1 | 72.5 | 69.2 | 49.1 | 44.4 | 37.3 |
| (+7.4) | (+6.7) | (+3.2) | (+3.9) | (+3.0) | (+25.4) | (+25.5) | (+15.5) | (+15.4) | (+13.1) | |
| Boston | 28.1 | 24.8 | 19.5 | 16.8 | 15.3 | 56.6 | 50.7 | 36.7 | 29.2 | 24.7 |
| (+4.1) | (+3.2) | (+1.5) | (+1.2) | (+1.2) | (+9.5) | (+7.1) | (+3.1) | (+0.3) | (+0.4) | |
| Atlanta | 27.1 | 23.8 | 19.8 | 16.8 | 14.8 | 52.7 | 48.0 | 35.8 | 29.9 | 22.6 |
| (+3.2) | (+2.3) | (+1.8) | (+1.2) | (+0.7) | (+5.6) | (+4.4) | (+2.2) | (+0.9) | (−1.6) | |
| Denver | 27.3 | 25.6 | 21.0 | 17.6 | 15.9 | 48.8 | 44.0 | 32.0 | 27.4 | 21.5 |
| (+3.4) | (+4.0) | (+3.0) | (+2.0) | (+1.8) | (+1.7) | (+0.4) | (−1.6) | (−1.5) | (−2.8) | |
| New York | 23.2 | 20.2) | 16.8 | 14.4 | 13.5 | 40.8 | 39.2 | 30.9 | 27.0 | 24.0 |
| (−0.7) | (−1.3) | (−1.2) | (−1.2) | (−0.6) | (−6.2) | (−4.5) | (−2.7) | (−1.9) | (−0.3) | |
| San Francisco | 21.4 | 19.1 | 16.8 | 14.8 | 13.5 | 39.2 | 33.4 | 26.7 | 21.9 | 19.5 |
| (−2.5) | (−2.5) | (−1.2) | (−0.8) | (−0.6) | (−7.8) | (−10.2) | (−6.9) | (−7.0) | (−4.7) | |
| Chicago | 20.3 | 19.0 | 16.2 | 14.6 | 13.9 | 39.1 | 36.4 | 29.2 | 25.6 | 21.8 |
| (−3.6) | (−2.6) | (−1.8) | (−1.0) | (−0.2) | (−8.0) | (−7.2) | (−4.4) | (−3.3) | (−2.5) | |
| Kansas City | 20.7 | 19.7 | 17.5 | 15.3 | 13.6 | 37.5 | 35.6 | 27.1 | 23.9 | 20.9 |
| (−3.2) | (−1.8) | (−0.5)§ | (−0.3)§ | (−0.5)§ | (−9.6) | (−8.1) | (−6.5) | (−5.0) | (−3.3) | |
| Philadelphia | 19.7 | 17.7 | 14.5 | 11.7 | 10.9 | 35.6 | 34.6 | 29.0 | 24.8 | 21.3 |
| (−4.3) | (−3.8) | (−3.5) | (−3.9) | (−3.2) | (−11.5) | (−9.1) | (−4.6) | (−4.1) | (−3.0) | |
| Seattle | 1.9 | 13.1 | 11.1 | 10.1 | 9.8 | 28.0 | 25.4 | 21.2 | 18.4 | 18.3 |
| (−9.0) | (−8.5) | (−6.9) | (−5.5) | (−4.3) | (−19.0) | (−18.2) | (−12.4) | (−10.5) | (−6.0) | |
Multivariate analyses adjusted for patient, institutional, HH, and regional covariates as outlined in methods section.
Regions sorted by proportion of HH utilization after elective joint replacement surgery during March 1996.
All regional monthly estimates significantly different than the corresponding national estimate as assessed by bootstrap except where noted by § symbol.
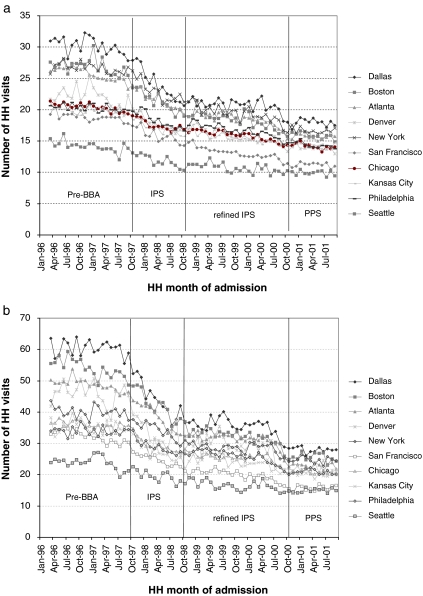
Figure 2.
(a) Adjusted Mean Number of Home Health (HH) Visits per 120-Day Episode after Elective Joint Replacement Surgery by Region. (b) Adjusted Mean Number of HH Visits per 120-Day Episode after Surgical Management of Hip Fracture by Region
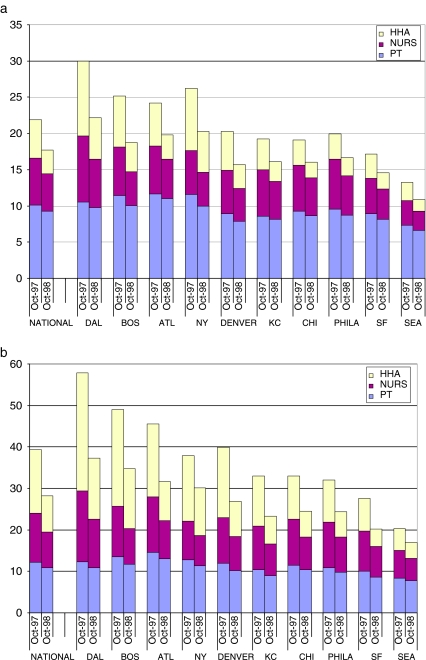
(a) Reduction in Home Health Visits between October 1997 and October 1998 by Type of Visit for Patient Undergoing Elective Joint Replacement Surgery. (b) Reduction in Home Health Visits between October 1997 and October 1998 by Type of Visit for Patient Undergoing Surgical Repair of Hip Fracture
As the graph indicates (Figure 2a), the significant regional variation in the mean number of HH visits decreased over time, with the greatest reduction in variation occurring under IPS and during the transition to PPS. As a measure of change in regional variation, we examined the difference between the national mean and each of the region's mean number of visits per episode across the time periods. The magnitude of the absolute difference from the national mean fell in all 10 of the CMS regions across the time periods, while the relative magnitude of the deviation from national fell in 6 out of 10 regions.
Surgical Repair of Hip Fracture
Among FX patients, there was greater variation across CMS region in the baseline number of HH visits per episode. In March 1996, the adjusted mean number of HH visits provided in the Dallas region was 72.5 but only 28.0 in the Seattle region; these figures, respectively, represented 25.4 visits over and 19.0 visits under (or 1.54 times as high and 0.60 times as low) as the national mean (Table 2 and Figure 2b).
The magnitude of this difference diminished dramatically over the following years, with the greatest absolute reductions occurring under the IPS. By September 2001, the adjusted mean number of HH visits in the Dallas region was 37.3 (13.1 visits over, remaining 1.54 times as high as the national mean), while the number of visits in Seattle fell to 18.3 (6.0 visits under and 0.75 times as low as the national mean). The absolute magnitude of the deviation from the national mean fell in 9 out of 10 regions, and the relative magnitude of the deviation from national fell in 7 out of 10 regions.
Regional Variation in HH Visits by Type of HH Service
Variation in Type of HH Service before IPS (October 1997)
The significant regional variation in number of HH visits before IPS was largely attributable to regional variation in the number of HH aide visits, with less variability in the number of physical therapy or nursing visits.
As noted above, among JR patients before IPS, there was significant variation in total number of HH visits ranging from 30.3 to 13.7. (Slightly different means are noted as a result of differences in spline modeling for this smaller temporal sample frame.) The mean number of HH aide visits across regions ranged 10.3–2.5; with less variation in the mean number of PT visits (range 11.6–7.3) or nursing visits (range 9.1–3.4). (All differences were significantly different by bootstrap estimation.)
Among FX patients admitted to HH agency in October 1997, the mean number of visits ranged from 57.9 to 20.3. The majority of this variation in care was again attributable to variation in the number of HH aide visits, ranging between 28.5 and 5.3 visits per region, with less variation in the number of PT visits (range 14.6–8.4) or nursing visits (range 17.2–6.6). (All differences were significantly different by bootstrap estimation.)
Change in Variation in Type of HH Service after IPS (October 1997–October 1998)
The large reductions in total number of visits following the introduction of the IPS were explained primarily by greater reductions in HH aide visits and to a lesser extent nursing visits.
Among JR patients, the total adjusted mean number of visits per episode under IPS fell from 21.9 to 17.7 (a 19 percent reduction) between October 1997 and October 1998. By type of visit, the number of HH aide visits fell from 5.3 to 3.3 (39 percent reduction), while nursing visits fell from 6.5 to 5.1 (21 percent reduction) and physical therapy visits fell from 10.1 to 9.3 (8 percent reduction). By visit type, the 2.1 fewer HH aide visits, 1.3 fewer nursing visits, and 0.8 fewer physical therapy visits, respectively, accounted for 52, 29, and 18 percent of the 4.3 fewer total HH visits provided. (All differences were significantly different by bootstrap estimation.)
Among FX patients, the total adjusted mean number of visits under IPS fell from 39.3 to 28.2 (a 28 percent reduction). By type of visit, the number of HH aide visits fell from 15.3 to 8.8 (42 percent reduction), while nursing visits fell from 11.8 to 8.6 (28 percent reduction) and physical therapy visits fell from 12.2 to 10.9 (11 percent reduction). By visit type, the 6.5 fewer HH aide visits, 3.3 fewer nursing visits, and 1.4 fewer physical therapy visits, respectively, accounted for 58, 29, and 12 percent of the 11.1 fewer total HH visits provided. (All differences were significantly different by bootstrap estimation.)
DISCUSSION
Before implementation of the BBA, there was significant regional variation in HH usage with greater variation in the number of HH visits per beneficiary than variation in number of beneficiaries selected for HH care after major orthopedic surgery. This variation in number of HH visits was driven primarily by variation in the number of HH aide visits.
These results reported herein support the earlier IPS findings by McCall et al. (2003a,b); and related findings by Murtaugh et al. (2003), who reported that between 1997 and 2001 among a 1 percent sample of all HH users (both chronic and postacute care patients), there was a 79 percent reduction in HH aide visits but only a 42 percent reduction in skilled visits (physical therapy and nursing).
Before the BBA, the number of visits per beneficiary had been unconstrained. As elucidated by McKnight (2006), with the IPS per-beneficiary limits based on a blend of agency and regional historical costs, agencies with high average historical costs relative to national average costs faced greater pressure to restrain costs per beneficiary than agencies with lower historical costs. Because number of visits is highly correlated with costs, this translated to greater pressure to reduce visits per user on agencies with high utilization. Porrell, Liu, and Brungo (2006) correlated agency low historical per beneficiary limits with subsequent market share expansion and high limits with market share contraction. Owing to the regional variation in utilization and the differential effect of blended per beneficiary limits, it is not surprising to see greater reductions in regions with greater HH utilization.
With the implementation of PPS, the number of visits per episode and regional variation fell even further. For these physical therapy–intense HH episodes of care, reimbursement under PPS was generous, with average payments per visit higher under PPS than IPS or even before IPS implementation. Therefore, the reduction in number of visits after orthopedic surgery under PPS was attributable to the incentive structure of prospective payments rather than reimbursement cuts.
Policy makers have long been concerned that regional variation was attributable to fraudulent or inefficient care (Brown 1997). While it is clear that the IPS and PPS reduced regional variation and that under IPS, this was largely accomplished by reduction in utilization of HH aide visits, it is not clear if these reductions were primarily reductions in inefficient services. Some authors have reported that reductions in HH care use, in general, were not associated with poorer patient clinical outcomes or satisfaction (McCall et al. 2004; Schlenker, Powell, and Goodrich 2005;). However, McCall et al. (2002) did report that for HH patients between 1997 and 1999, there was increased use of SNF, emergency room use, and mortality after HH admission, though no change in hospital readmission rates.
Peng, Navaie-Waliser, and Feldman (2003) reported that at time of HH discharge, patients had a significant number of dependencies, as well as anxiety and depression. Brega et al. (2005) reported that African American and nonwhite Hispanic HH patients had poorer functional outcomes than Caucasian patients at discharge.
With reductions in HH visits and in particular HH aide services, it is likely there would be increased burdens upon informal care from family members, which may disproportionately burden vulnerable HH patients. Peng, Navaie-Waliser, and Feldman (2003) reported that Hispanic and Asian patients reported greater disabilities at time of discharge, and that African American patients were less likely to have informal care available than Caucasian patients. McKnight (2006) reported that reductions in HH utilization were partly offset by increased out-of-pocket payments, and that low-income beneficiaries experienced larger reductions in HH care after implementation of IPS, arguing for potential loss in welfare though no poorer outcomes were noted. Schwartz et al. (2002) reported that in rural HH agencies 81 percent of HH beneficiaries reported increased demands on informal care and heightened concern about older and frail beneficiaries (Lin and Meit 2005). For certain vulnerable patient groups, particularly those with limited informal care options, earlier discharge under these BBA policies could have adverse effects.
Our findings need to be interpreted carefully. Only two conditions were studied, although these represent a significant proportion of postacute care services. Caution should be used extrapolating these findings to other groups of HH patients.
Furthermore, several other policies were concurrently implemented, which either directly (Operation Restore Trust, HH surety bonds, civil penalties for physicians inappropriately prescribing HH services and a 6-month moratorium on new HH agencies) or indirectly (SNF PPS, Short Stay Transfer Policy) impacted HH utilization and might explain some of the observed changes over time. (See Tables S1 and S2 for summary.) However, with the exception of Operation Restore Trust, no policies had differential regional implementation or regulation, so any potential temporal–regional bias is unlikely to be substantial. Furthermore, the above month-to-month analyses demonstrate that changes in utilization correlate well with BBA implementation dates.
In summary, the IPS and PPS reduced regional variation in HH services after major orthopedic surgery. Under IPS, this was largely attributable to reductions in lesser skilled services. Other authors have documented no concurrent reductions in patient outcomes. However, reducing services could result in increased burden on informal care, and for those beneficiaries with little social support, this could have adverse implications. To the extent that these reductions may have reduced ineffective care, these findings suggest that tailoring policies to target areas of high utilization may be an effective strategy to reduce program costs while minimizing potential untoward adverse outcomes.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Drs. FitzGerald and Boscardin's effort was partly supported by K08 HS13168 from the Agency for Healthcare Research and Quality. Dr. FitzGerald and Dr. Ettner's effort was partly supported by an Arthritis Investigator Award from the Arthritis Foundation.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Figure S1. Map of CMS Regions.
Figure S2. Conceptual Model for Nested Logistic Statistical Model.
Table S1. Home Health Reimbursement and Related Policy Changes.
Table S2. Other Concurrent Policies.
Table S3. Elective Joint Replacement and Hip Fracture Patient Characteristics before Implementation of Home Health Policy Changes.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- ArcView. Redlands, CA: ESRI; “ArcGIS” (9.2) [Google Scholar]
- Brega AG, Goodrich GK, Powell MC, Grigsby J. Racial and Ethnic Disparities in the Outcomes of Elderly Home Care Recipients. Home Health Care Service Quarterly. 2005;24(3):1–21. doi: 10.1300/J027v24n03_01. [DOI] [PubMed] [Google Scholar]
- Brown JG. Washington, DC: Department of Health and Human Services; “Results of the Operation Restore Trust Audit of Medicare Home Health Services in California, Illinois, New York and Texas” (A-04-96-02121) [Google Scholar]
- Centers for Medicare & Medicaid Services. “Medicare Managed Care Market Penetration for All Medicare Plan Contractors.” Quarterly State/County Data Files.
- Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. New York: Chapman & Hall; An Introduction to the Bootstrap. [Google Scholar]
- FitzGerald JD, Boscardin WJ, Hahn BH, Ettner SL. Impact of the Medicare Short Stay Transfer Policy on Patients Undergoing Major Orthopedic Surgery. Health Services Research. 2007;42(1):25–44. doi: 10.1111/j.1475-6773.2006.00606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FitzGerald JD, Mangione CM, Boscardin J, Kominski G, Hahn B, Ettner SL. Impact of Changes in Medicare Home Health Care Reimbursement on Month-To-Month Home Health Utilization between 1996 and 2001 for a National Sample of Patients Undergoing Orthopedic Procedures. Medical Care. 2006;44(9):870–8. doi: 10.1097/01.mlr.0000220687.92922.64. [DOI] [PubMed] [Google Scholar]
- Health Care Financing Administration. Medicare Program; Additional Supplier Standards; Final Rule. Federal Register. 1995;60(237):63440–4. [PubMed] [Google Scholar]
- Health Care Financing Administration. Medicare Program; Prospective Payment Systems for Home Health Agencies. Federal Register. 2000;42(CFR Parts 409, 410, 411, 413, 424, 484):41128–214. [PubMed] [Google Scholar]
- Kenney GM, Dubay LC. Explaining Area Variation in the Use of Medicare Home Health-Services. Medical Care. 1992;30(1):43–57. doi: 10.1097/00005650-199201000-00004. [DOI] [PubMed] [Google Scholar]
- Komisar HL. Rolling Back Medicare Home Health. Health Care Financial Review. 2002;24(2):33–55. [PMC free article] [PubMed] [Google Scholar]
- Lin CJ, Meit M. Changes in Medicare Home Health Care Use and Practices in Rural Communities: 1997 to 2001. Journal of Aging Health. 2005;17(3):351–62. doi: 10.1177/0898264305276288. [DOI] [PubMed] [Google Scholar]
- Liu K, Long SK, Dowling K. Medicare Interim Payment System's Impact on Medicare Home Health Utilization. Health Care Financial Review. 2003;25(1):81–97. [PMC free article] [PubMed] [Google Scholar]
- Marsch CL, Cormier DR. Thousand Oaks, CA: Sage; Spline Regression Models, no. 137. In Quantitative Applications in the Social Sciences (Series) [Google Scholar]
- McCall N, Komisar HL, Petersons A, Moore S. Medicare Home Health before and after the BBA. Health Affairs. 2001;20(3):189–98. doi: 10.1377/hlthaff.20.3.189. [DOI] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Constraining Medicare Home Health Reimbursement: What Are the Outcomes? Health Care Financial Review. 2002;24(2):57–76. [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Reforming Medicare Payment: Early Effects of the 1997 Balanced Budget Act on Postacute Care. Milbank Quarterly. 2003a;81(2):277–3. doi: 10.1111/1468-0009.t01-1-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Decreased Home Health Use: Does It Decrease Satisfaction? Medical Care Research and Review. 2003b;61(1):64–88. doi: 10.1177/1077558703260183. [DOI] [PubMed] [Google Scholar]
- McCall N, Petersons A, Moore S, Korb J. Utilization of Home Health Services before and after the Balanced Budget Act of 1997: What Were the Initial Effects? Health Services Research. 2004;38(1 Pt 1):85–106. doi: 10.1111/1475-6773.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight R. Home Care Reimbursement, Long-Term Care Utilization, and Health Outcomes. Journal of Public Economics. 2006;90(1):293–323. [Google Scholar]
- Medicare Payment Advisory Commission (MEDPAC). “Medicare Payment Policy.” Report to the Congress: 1–98.
- Mooney C, Duval R. Bootstrapping. Newbury Park, CA: Sage; 1993. A Nonparametric Approach to Statistical Inference. [Google Scholar]
- Murkofsky RL, Phillips RS, McCarthy EP, Davis RB, Hamel MB. Length of Stay in Home Care before and after the 1997 Balanced Budget Act. Journal of the American Medical Association. 2003;289(21):2841–8. doi: 10.1001/jama.289.21.2841. [DOI] [PubMed] [Google Scholar]
- Murtaugh CM, McCall N, Moore S, Meadow A. Trends in Medicare Home Health Care Use: 1997–2001. Health Affairs (Millwood) 2003;22(5):146–56. doi: 10.1377/hlthaff.22.5.146. [DOI] [PubMed] [Google Scholar]
- 105th Congress of the United States of America. “Balanced Budget Act of 1997.” H.R. 2015-147 4401-11723.
- 105th Congress of the United States of America. “Payment Systems for Medicare's Home Health Benefit.” Serial 105–109.
- Peng TR, Navaie-Waliser M, Feldman PH. Social Support, Home Health Service Use, and Outcomes among Four Racial-Ethnic Groups. Gerontologist. 2003;43(4):503–13. doi: 10.1093/geront/43.4.503. [DOI] [PubMed] [Google Scholar]
- Porell FW, Liu K, Brungo DP. Agency and Market Area Factors Affecting Home Health Agency Supply Changes. Health Services Research. 2006;41(5):1847–75. doi: 10.1111/j.1475-6773.2006.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker RE, Powell MC, Goodrich GK. Initial Home Health Outcomes Under Prospective Payment. Health Services Research. 2005;40(1):177–93. doi: 10.1111/j.1475-6773.2005.00348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MR, Davis LA, Leon J, Davitt JK, Marainen J. Center for Rural Pennsylvania: Pennsylvania State College; The Effect of New Medicare Reimbursement Methodologies on Rural Home Health Agencies and Their Beneficiaries. [Google Scholar]
- Spector WD, Cohen JW, Pesis-Katz I. Home Care before and after the Balanced Budget Act of 1997: Shifts in Financing and Services. Gerontologist. 2004;44(1):39–47. doi: 10.1093/geront/44.1.39. [DOI] [PubMed] [Google Scholar]
- STATA. College Station, TX: “Stata.” (Intercooled 7.0 for Windows 98/95/NT) [Google Scholar]
- Welch HG, Wennberg DE, Welch WP. The Use of Medicare Home Health Care Services. New England Journal of Medicine. 1996;335(5):324–9. doi: 10.1056/NEJM199608013350506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.