Abstract
Objective
To determine whether variation in the representation of minority physicians across geographical areas in California affects the location decisions of minority physicians.
Data Sources
We analyzed data on 9,806 residents and 53,606 patient-care physicians from the 1997–2003 American Medical Association Masterfiles for California along with data from the California Department of Finance, RAND, and other sources.
Study Design
We estimated departure models using linear probability models and destination models using conditional logit. Each model controlled for physician and county characteristics. Parameters of interest include the interactions of physician race/ethnicity with area-level minority physician representation for the corresponding race/ethnicity.
Principal Findings
Departure models show that black and Hispanic physicians are more likely to remain in an area as the level of representation of physicians from their respective groups worsens. The destination models show that black, Asian, and Hispanic physicians tend to move to areas where the level of representation is similar to that of their previous location.
Conclusions
Black and Hispanic physicians are influenced by the level of representation of physicians from their respective groups in their location decisions and tend to locate where needed.
Keywords: Geographic/spatial factors/small area variations, racial/ethnic differences in health and health care, cohort analysis
Racial diversity has recently been the topic of reports by the Sullivan Commission on Diversity in the Healthcare Workforce and the Institute of Medicine (Institute of Medicine 2004; Sullivan Commission 2004;). These reports emphasize the importance of racial/ethnic physician–patient concordance in the provision of quality patient care.
Health disparities affecting minorities have been traced to many causes, including language and cultural barriers that can deter minorities from seeking care or lead to suboptimal care (Lewin-Epstein 1991; Kaiser Family Foundation 1999; Ma 1999; Morehouse Medical Treatment and Effectiveness Center 1999; Ku and Waidmann 2003; Yeo 2004;). Racial/ethnic concordance in physician–patient relationships has been shown to improve care (Gray and Stoddard 1997; Saha et al. 1999, 2003; LaVeist and Carroll 2002; LaVeist and Nuru-Jeter 2002; Cooper et al. 2003; Garcia et al. 2003; LaVeist, Nuru-Jeter, and Jones 2003). Patients tend to prefer physicians who are of their own race/ethnicity (Gray and Stoddard 1997; Saha et al. 1999; Garcia et al. 2003;), and also tend to use more health care and are less likely to postpone care when they have physicians who are of their own race/ethnicity (LaVeist, Nuru-Jeter, and Jones 2003). Race-concordant visits are longer and characterized by more positive effect (Cooper et al. 2003; Saha et al. 2003;). Patients also report higher satisfaction when they are able to choose their provider (LaVeist and Carroll 2002; LaVeist and Nuru-Jeter 2002;).
Such positive relationships are more likely to occur when an area contains enough physicians of a given race/ethnicity to serve local patients who are of the corresponding race/ethnicity. Economic analysis of the physician labor market adds further evidence that racially/ethnically concordant physician–patient relationships are highly valued. Brown et al. (2007) found that earnings per hour for Hispanic and Asian physicians are higher when practicing in areas where they are more underrepresented relative to the size of the respective Hispanic and Asian populations. This suggests that patients prefer physicians with whom they have language and/or cultural concordance to such an extent that they are willing to pay more to obtain such relationships or preferentially choose health plans where there is a greater likelihood of forming such relationships (Brown et al. 2007).1
Additional research has found that physicians from groups underrepresented in the health professions are more likely to serve minority and economically disadvantaged patients (Cantor et al. 1996; Gartland et al. 2003;). It has also been found that black and Hispanic physicians practice in areas with larger black and Hispanic populations and care for more black and Hispanic patients, respectively, than other physicians (Komaromy et al. 1996).
However, a nuanced understanding of racial/ethnic concordance is important. Not all patients prefer having a physician who is of their own race/ethnicity. Schnittker and Liang (2006), using nationally representative data, find that only 21.7 percent of blacks and only 26.8 percent of Hispanics prefer a physician of the same race/ethnicity and that racial/ethnic concordance promotes better encounters mainly among those who prefer concordance. This suggests that those areas where the representation of black and Hispanic physicians is the lowest may benefit the most from an improved representation of black and Hispanic physicians because such areas are the least likely to have enough black and Hispanic physicians to serve those who prefer concordance. In other words, underrepresentation per se does not imply that minorities who desire concordance are unable to find it. The critical factor is the degree of underrepresentation. An issue not hitherto discussed in the literature is whether physicians move to (or preferentially remain in) areas in which they are underrepresented.
Although price signals (earnings-per-hour premiums) indicate that racial/ethnic concordance is valued (Brown et al. 2007), these signals may not be large enough to influence minority physicians' location choices. Given that other area characteristics play a role in a physician's location decision, we are interested in whether variation in the level of representation of minority physicians across geographical areas affects the location decisions of minority physicians.
To determine the influence that the level of minority physician representation has on the location decisions of minority physicians, location choice is separated into a departure model (the decision to leave an area) and a destination model (the decision to go to an area) (Liaw and Ledent 1987; Frey et al. 1996; Polsky et al. 2000;). We also extend this analysis to physicians just completing residency.
METHODS
Defining Minority Physician Representation
We follow Brown et al. (2007) and define physician representation for each racial/ethnic group as the difference between the proportion of the local physician workforce comprised of a specific racial/ethnic group and the proportion of the population who are members of the same group (e.g., [proportion of the physician workforce who are Hispanic]−[proportion of population who are Hispanic]). A value of 0 indicates that no under- or overrepresentation is present. A positive value indicates the proportion of physicians in an area that may be in excess of what is needed for members of a given racial/ethnic group to be able to easily see a physician who is of their own race/ethnicity (overrepresentation). A negative value indicates the proportion of the population who may be unable to easily see a physician who is of their own race/ethnicity (underrepresentation).
Departure Model
Departure models relate physicians' decision to leave an area to physicians' characteristics and area characteristics. We specify the departure model as follows:
| (1) |
where depart is equal to 1 if a physician subsequently moved to a different county in the United States and 0 otherwise. Vector P denotes physician characteristics: age and its square, gender, years residing in current location, and indicators of being born in California, being born outside the United States, and of completing at least part of one's residency training in California. Generalist (family practice, general practice, internal medicine, pediatrics, and obstetrics/gynecology) and specialist (all remaining categories) physicians are indicated to account for the fact that generalists require smaller market areas and more frequent patient encounters. Physician specialty was calculated using a previously used algorithm (Newhouse et al. 1982; Escarce et al. 2000; Brown et al. 2007;): physicians reporting only one specialty were counted as 1.0 full-time equivalent (FTE) in the reported specialty; physicians reporting two specialties were counted as 0.6 FTE in their primary specialty and 0.4 FTE in the other.
Indicator variables for the race/ethnicity of each physician (black, Hispanic, and Asian and Pacific Islanders [PI]) are included in R. The reference group in this model contains physicians surveyed in 1997 who are male, white, born in the United States outside of California, completed their residency outside of California (this category is omitted in the residency model), and are generalist physicians.
Vector C contains county characteristics relevant to the health care marketplace: ratios of generalists, specialists, hospital beds, HMO penetration, and per capita income, as well as the proportions of the population who are older than 65, eligible for Medi-Cal, white, black, Hispanic, and Asian/PI. Ratios of generalists and specialists per 100,000 population provide an indication of the size of the local physician workforce. The size of health care infrastructure is measured by hospital beds per 100,000 population. The level of HMO penetration (defined as the ratio of county-level HMO penetration to national-level HMO penetration) is a measure of the relative level of managed care across counties. Per capita income (measured as the ratio of county per capita income to national per capita income) is an indicator of the effect of relative income on the demand for medical care. The relative size of the elderly population will tend to increase the demand for medical care, while the size of the potentially publicly insured population will tend to limit physician revenues.
The vector D includes measures of the level of representation for each group of minority physicians (black, Hispanic, and Asian/PI). We also interact each measure with the corresponding race of the physician (D·R). These interactions are the main variables of interest as they reflect the influence of the level of minority physician representation on minority physicians' decisions to relocate. Finally, vector F contains county- and year-fixed effects.
We employ a fixed-effects linear probability model, which produces unbiased parameter estimates. We incorporate clustering at the physician level and correct for heteroskedasticity using Huber/White estimator and generalized least squares (Huber 1967; White 1980;). We focus our interpretation of parameter estimates only on marginal probabilities, avoiding interpretation of estimates that may occur outside [0, 1].
Destination Model
Given that a physician has chosen to relocate, she must choose a destination from a set of alternative locations. Because we have more comprehensive data about area characteristics of locations within California, we restrict our sample to physicians who have only moved to a different county within California. While this will result in different estimates than would be the case had we included physicians who located outside of California, for policy questions related to the under- or overrepresentation of minority physicians across geographical areas within California this is the more appropriate model.
Assuming a physician chooses to relocate within California (occurring in 7,626 of 12,672 relocation events), a physician must choose a particular California county. The area characteristics associated with different destination choices will be key criteria in selecting a destination. The destination model is specified as a conditional logit model as follows:
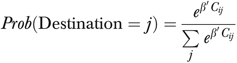 |
(2) |
where j=1, 2, …, J for a total of J alternative destinations (57 less the physician's current county location=56).2 The dependent variable is equal to 1 if a physician moves to a given county, j, in California and 0 otherwise. The vector C contains a physician-level variable indicating whether a physician is a specialist and county-level variables that include the following: per capita income, HMO penetration, specialists per 100,000 population, generalists per 100,000 population, and the proportions of the population who are Medi-Cal eligible, who are aged 65 and older, and who are of the same race/ethnicity as the physician.
In addition, our main variable of interest, the level of representation of minority physicians, is included in C as a set of categorical variables denoting the choice of a destination county where the level of representation is either one (or more) standard deviation higher, one (or more) standard deviation lower, or within one standard deviation of the departure county.
DATA
Data on the individual characteristics and practice locations of physicians who, at any one time, practiced in California were obtained from the American Medical Association (AMA) Masterfile for the years 1997–2003. The AMA Masterfile is the best available data source at this time, but its primary limitation is that updating physician addresses is often done with a lag averaging 2 years (Kletke 2004).
Because physician movement is measured with a lag, this means that in our departure models, the dependent variable is measured with error. If this measurement error has a mean different from 0 due to the average 2-year lag, but is otherwise random across physicians, then there will be no bias to the estimated coefficients (with the exception of the constant term that is biased due to the mean measurement error not being 0—this bias is unimportant here), but the standard errors will be larger (Wooldridge 2006). The assumption of measurement error being random with a mean different from 0 is reasonable given the available evidence.
This data limitation also suggests that there is some error in the measure of minority physician representation in our departure models. In this case, the parameter bias resulting from such error depends on the ratio of the variance of the true measure of representation and the variance of representation when it is measured with error (Wooldridge 2006). If this ratio is close to 1, then any bias to the parameter will be small. In the current case measurement error will be very small since in our data only 6.9 percent of physicians relocate (or leave practice) on average over the entire period examined.3 Note that the true percentage of physicians who migrate (or leave practice) in any given year may be somewhat greater or less than the long-run 6.9 percent figure depending on the specific configuration of lags in any given year, with the long-run measured migration percentage becoming more accurate the longer the period is that is being examined. This suggests that reporting lags regarding physician location will result in an average error rate of much less than 6.9 percent (because only some observations will be in error). This further suggests that the parameters of the physician representation measures may be slightly biased toward 0 as well as there being some relatively small but unpredictable effects on the parameter estimates of the other covariates to the degree that they are correlated with the measure of representation (Nugent, White, and Basham 2000; Wooldridge 2006;).
This data limitation also implies that there is also some small measurement error in the destination models. There are two concerns about measurement error in these models. The first is that some physicians did not move at the time that the data states: there may be a mismatch between the timing of the dependent variable and with some of the time-varying independent variables, which is equivalent to a small amount of measurement error in each of these independent variables to the extent that they change over time. Because most of these variables change very little over time, this measurement error is likely to be quite small.
The second concern is with regard to the physician representation variables in the destination model. In these variables there is, on average, <6.9 percent measurement error and we use interval measures that will mask much of this already very small error. Thus, in each of the two concerns above with respect to measurement error in the destination model, any resulting biases to the estimated parameters are likely to be small and thus of little consequence depending on the correlation of the independent variables with each other (Stefanski and Carroll 1985; DeVaro and Lacker 1995;).
An additional issue is the geographical level at which to measure minority physician representation. There will necessarily be more variation in minority physician representation across geographical units as the geographical unit used becomes smaller. We must determine whether to measure minority physician representation only in the area where a patient lives or also to include the area where they work. The first approach assumes that patients do not access medical care outside of the area where they live. If patients access a significant amount of medical care outside of this area, and the levels of minority physician representation differ between areas, then measuring minority physician representation only in the area where patients live may result in an inaccurate measure.
The second approach assumes that patients may access medical care across larger areas, such that the heterogeneity in minority physician representation between smaller areas is unimportant. In other words, the second approach assumes that patients may access medical care around their home, around their place of employment, and anywhere in between. In this situation, the average level of minority physician representation across this larger area may be a more accurate measure. Someone living in an area where there are few physicians who are racially/ethnically concordant to them will often be able to access such physicians who are nearby but outside of the area around their home.
The fundamental issue in deciding which geographical measure to use is how convenient it is to access the medical resources that exist between patients' regular travel destinations. The level of convenience depends on the most common mode of transportation used in an area. If this is public transportation, then the convenience factor is low and assuming that most patients will access medical resources anywhere between their home and workplace is inappropriate. However, if private vehicles are the most common mode, then the convenience factor is high and the assumption that most patients will access medical resources anywhere between their home and workplace is warranted.
In a “car culture” such as California the convenience factor is high. In 2002, 92 percent of housing units had one or more vehicles available, 96 percent of employed individuals commuted to work (mean time: 27 minutes) with only 5.2 percent using public transportation (other than taxicabs) (U.S. Census Bureau 2002a,b;). Thus, in California the average level of physician representation as measured across a larger area that likely includes most patients' home and workplace appears to be more meaningful.
Additional information on the demographic and socioeconomic characteristics of California was obtained from the California Department of Finance and RAND (Department of Finance 2004; RAND California 2005;). Information on county HMO penetration was obtained from Cattaneo and Stroud (2003, 2004).
The 53,606 physicians included in this analysis represent active patient-care physicians with known race/ethnicity (approximately 70 percent) and valid zip codes. We include physicians who are white, black, Hispanic, and Asian/PI.
We also model the departure and destination choices for 9,806 recently graduated California residents. These models exclude the variable measuring the number of years residing in one's current location. Tables 1 and 2 report descriptive statistics.
Table 1.
Descriptive Statistics for Individuals
| Physicians |
Residents |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | 53,606 | 9,806 | ||
| Male | 41,207 | 76.9 | 5,647 | 57.6 |
| Female | 12,399 | 23.1 | 4,159 | 42.4 |
| Age | Mean=50.79, SD=11.9 | Mean=33.65, SD=4.87 | ||
| Specialty* | ||||
| Generalist FTEs† | 21,625.8 | 40.3 | 4,727.0 | 48.2 |
| Specialist FTEs | 31,921.4 | 59.5 | 5,079.0 | 51.8 |
| Race/ethnicity | ||||
| White | 38,094 | 71.1 | 5,138 | 52.4 |
| Black | 1,718 | 3.2 | 407 | 4.2 |
| Hispanic | 2,356 | 4.4 | 681 | 6.9 |
| Asian | 11,438 | 21.3 | 3,050 | 31.1 |
| Born in CA | 11,151 | 20.1 | 2,839 | 29.0 |
| Born in a country outside the United States | 15,240 | 28.4 | 3,240 | 33.0 |
| Completed some medical residency in CA | 34,243 | 63.9 | NA | NA |
| Number of years in departure location | Mean=13.00, SD=7.62 | NA | ||
Totals do not add up to 100% because some physicians' specialties are unspecified.
Includes family practice, general practice, internal medicine, pediatrics, and obstetrics/gynecology.
FTE, full-time equivalent; CA, California; SD, standard deviation.
Table 2.
Descriptive Statistics for California Counties*
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Proportion of population Medi-Cal eligible | 0.15 | 0.06 | 0.04 | 0.32 |
| Proportion of population age 65 and older | 0.13 | 0.03 | 0.07 | 0.21 |
| Specialists/100,000 | 88.18 | 54.56 | 11.19 | 297.52 |
| Generalists/100,000 | 75.14 | 29.26 | 8.35 | 181.25 |
| Hospital beds/100,000 | 292.98 | 274.14 | 56.34 | 1,798.71 |
| HMO penetration ratio (county/US) | 1.14 | 0.76 | 0.05 | 2.96 |
| Per capita income ratio (county/US) | 0.79 | 0.28 | 0.44 | 2.04 |
| Race/ethnicity of population | ||||
| Proportion of population who are white | 0.66 | 0.18 | 0.20 | 0.94 |
| Proportion of population who are black | 0.04 | 0.04 | 0.00 | 0.17 |
| Proportion of population who are Hispanic | 0.22 | 0.15 | 0.03 | 0.72 |
| Proportion of population who are Asian | 0.06 | 0.07 | 0.00 | 0.33 |
| Physician representation | ||||
| (White physicians−white population) | 0.11 | 0.11 | −0.13 | 0.39 |
| (Black physicians−black population) | −0.02 | 0.04 | −0.13 | 0.14 |
| (Hispanic physicians−Hispanic population) | −0.18 | 0.13 | −0.55 | 0.18 |
| (Asian physicians−Asian population) | 0.08 | 0.09 | −0.16 | 0.32 |
| Climate | ||||
| Average temperature in January (°F) | 44.74 | 6.57 | 28.60 | 55.20 |
| Average temperature in July (°F) | 71.58 | 7.45 | 56.30 | 92.00 |
| Average precipitation in January (in.) | 4.62 | 2.82 | 0.37 | 13.50 |
| Average precipitation in July (in.) | 0.73 | 0.12 | 0.00 | 0.64 |
Data from 57 of California's 58 counties is included. Alpine County has no physicians listed in the data and so was excluded from the analysis.
RESULTS
Departure Model
During the period under analysis there were 12,762 relocation events of which 5,136 involved leaving the state. On average, 4.6 percent (0.046) physicians relocate each year (excluding those who leave practice). Table 3 reports coefficients for the departure model that represent marginal probabilities.
Table 3.
Marginal Probabilities That a Physician Will Leave a California County†
| Coefficient | Robust t-Statistics | |
|---|---|---|
| Physician characteristics | ||
| Age | −0.005 | (−15.04)** |
| Age2 | 0.00005 | (15.78)** |
| Female | −0.001 | (−0.49) |
| Born in CA | −0.008 | (−7.34)** |
| Foreign born | −0.008 | (−7.02)** |
| Was a CA medical resident | −0.002 | (−2.23)* |
| Years residing in departure location | −0.004 | (−41.33)** |
| Specialist physician | 0.004 | (4.10)** |
| Black physician | 0.021 | (3.18)** |
| Hispanic physician | 0.019 | (2.68)** |
| Asian physician | −0.006 | (−3.55)** |
| County characteristics | ||
| Generalists/100,000 | 0.001 | (2.41)* |
| Specialists/100,000 | 0.0005 | (2.14)* |
| Hospital beds/100,000 | 0.000 | (−0.02) |
| Proportion of population eligible for Medi-Cal | 0.215 | (2.78)** |
| Proportion of population aged 65+ | −0.151 | (−0.32) |
| Proportion of population that is white | 0.317 | (0.90) |
| Proportion of population that is black | −0.026 | (−0.05) |
| Proportion of population that is Hispanic | 1.031 | (2.18)* |
| Proportion of population that is Asian | 0.111 | (0.30) |
| HMO penetration (US) | −0.010 | (−1.36) |
| Per capita income (US) | 0.006 | (0.56) |
| Concordance measures and interactions | ||
| (Proportion physicians black−proportion population black) | 0.163 | (0.72) |
| (Proportion physicians Hispanic−proportion population Hispanic) | 0.048 | (0.28) |
| (Proportion physicians Asian−proportion population Asian) | −0.039 | (−0.55) |
| Black physician × (proportion physicians black−proportion population black) | 0.251 | (2.39)* |
| Hispanic physician × (proportion physicians Hispanic−proportion population Hispanic) | 0.059 | (2.62)** |
| Asian physician × (proportion physicians Asian−proportion population Asian) | 0.004 | (0.30) |
| Year-fixed effects | ||
| 1998 | −0.008 | (−3.53)** |
| 1999 | 0.015 | (4.21)** |
| 2000 | −0.011 | (−1.93) |
| 2001 | −0.019 | (−2.48)* |
| 2002 | −0.014 | (−1.47) |
| Constant | −0.19342 | (−0.52) |
| Observations | 266,714 | |
| F-statistic | 60.85** | |
| R2 | 0.0294 | |
Significant at 1%.
Significant at 5%.
County-level fixed effects included but not reported.
Our main variables of interest are physician race/ethnicity, the level of representation of each group of physicians by race/ethnicity, and their interaction. Relative to white physicians and assuming no over- or underrepresentation, Asian/PI physicians are slightly less likely to leave an area (−0.006, p<.01), whereas black (0.021, p<.01) and Hispanic (0.019, p<.01) physicians are both more likely to leave an area.
With regard to the interaction of physician race/ethnicity with the corresponding level of physician representation, we find that black physicians (0.251, p<.05) and Hispanic physicians (0.059, p<.01) were more (less) likely than white physicians to leave their current county when physicians in their respective groups were overrepresented (underrepresented).
With respect to other physician characteristics, we find that as physicians age, they are less likely to move (−0.005, p<.01), but that this effect diminishes until age 50 (−0.005/2(0.00005)) and then rises again as physicians move closer to retirement age, as shown by the positive parameter on the square of age (0.00005, p<.01). We do not find any statistically significant difference between males and females. We do find that physicians born in California (−0.008, p<.01), who had done their residency in California (−0.002, p<.05) or who were born outside of the United States (−0.008, p<.01), were less likely to move. Also, specialists are more likely to move than generalists (0.004, p<.01).
Physicians were more likely to depart in the presence of more generalists (0.001, p<.05) and more specialists (0.0005, p<.05). Additionally, physicians were more likely to leave given higher proportions of Medi-Cal eligibles (0.215, p<.01) or higher proportions of Hispanics in the population (1.031, p<.05).
In comparing these results with residents, physicians who are just entering the larger workforce, these “new” labor market entrants were overall less sensitive to individual-level and area-level characteristics (results not shown). There were no statistically significant effects from the interaction between physicians' race/ethnicity and the corresponding level of minority physician representation.
However, older residents were less likely to depart (−0.032, p<.01) with a turning point occurring at age 53.3 (−0.32/2(0.0003)). Residents trained as specialists were more likely to leave (0.017, p<.01). In addition, residents were more likely to stay in areas with a greater density of hospital beds (−0.001, p<.05) and higher relative income (0.161, p<.05).
Destination Model
Table 4 reports the estimated odds ratios (OR) from the conditional logit regressions of the destination model. We include the results for white physicians for comparison purposes, but we do not discuss them. Separate regressions were estimated for each racial/ethnic group of physicians and recently graduated residents. Our fundamental interest is whether, after physicians have left an area, they move to an area where they are more needed by members of their own racial/ethnic group (an area one standard deviation or more lower in physician representation). Note that many counties are very close to concordance. For example, although in 2000 black physicians were underrepresented in 48 of 57 counties and overrepresented in 9 of 57 counties, in 18 counties underrepresentation was <1 percent and in 4 counties overrepresentation was <1 percent. In this same year, Hispanic physicians were underrepresented in 56 of 57 counties, with underrepresentation being <1 percent in only 1 county. Finally, in 2000 Asian/PI physicians were underrepresented in 10 of 57 counties and overrepresented in 47 of 57 counties, although in 6 counties underrepresentation was <1 percent and in 4 counties overrepresentation was <1 percent.
Table 4.
Odds Ratios of Physicians Choosing Particular County Characteristics When Relocating
| White Physicians | Black Physicians | Hispanic Physicians | Asian Physicians | |
|---|---|---|---|---|
| Specialist physician | 0.99 | —† | 1.82 | 0.86 |
| (−0.03) | (0.41) | (−0.24) | ||
| January temperature | 1.13 | 1.13 | 1.17 | 1.24 |
| (25.14)** | (6.23)** | (7.93)** | (24.66)** | |
| July temperature | 0.98 | 0.96 | 0.97 | 1.04 |
| (−5.72)** | (−2.30)* | (−2.37)* | (6.16)** | |
| January precipitation | 0.92 | 0.84 | 0.81 | 0.90 |
| (−6.34)** | (−2.75)** | (−3.82)** | (−4.03)** | |
| July precipitation | 3.11 | 0.98 | 25.93 | 53.05 |
| (3.58)** | (−0.01) | (2.56)** | (6.55)** | |
| Per capita income (US) | 1.17 | 1.23 | 1.42 | 1.23 |
| (1.75) | (0.49) | (1.04) | (1.27) | |
| HMO penetration (US) | 2.99 | 2.59 | 3.63 | 3.52 |
| (32.18)** | (5.08)** | (8.70)** | (19.10)** | |
| Proportion of population Medi-Cal eligible | 1.18 | 40.18 | 42.49 | 19.10 |
| (0.37) | (2.22)* | (2.62)** | (4.83)** | |
| Proportion of population aged 65+ | 3.35 | 1.00 | 0.00 | 0.00 |
| (1.18) | (−1.98)* | (−1.91) | (−6.45)** | |
| Specialists/100,000 | 1.00 | 1.00 | 1.00 | 1.00 |
| (−0.47) | (0.92) | (−0.04) | (−0.93) | |
| Generalists/100,000 | 1.01 | 1.00 | 1.01 | 1.01 |
| (10.32)** | (0.53) | (2.25)* | (4.65)** | |
| Hospital beds/100,000 | 1.00 | 1.00 | 1.00 | 1.00 |
| (−9.25) | (0.54) | (−1.36) | (−3.31)** | |
| Proportion of population who are white | 0.38 | — | — | — |
| (−4.98)** | ||||
| Proportion of population who are black | — | 157.16 | — | — |
| (2.38)* | ||||
| Proportion of population who are Hispanic | — | — | 1.70 | — |
| (0.51) | ||||
| Proportion of population who are Asian | — | — | — | 150.20 |
| (9.07)** | ||||
| One standard deviation‡,§ or higher in racial/ethnic physician representation (corresponding to the physician's race) | 0.64 | 0.77 | 0.23 | 0.29 |
| (−9.51)** | (−1.46) | (−7.76)** | (−16.93)** | |
| One standard deviation‡,§ or lower in racial/ethnic physician representation (corresponding to the physician's race) | 1.38 | 1.16 | 0.52 | 0.47 |
| (7.67)** | (0.64) | (−2.77)** | (−9.54)** | |
| Observations | 336,471 | 16,017 | 27,759 | 131,157 |
z-Statistics are given in parentheses.
Variable automatically dropped by Stata due to no within-group variance.
Standard deviations for each group relative to their current location are as follows: blacks, SD: 0.05; Hispanics, SD: 0.18–0.19; Asians, SD: 0.12–0.14; whites, SD: 0.14–0.16.
Measured as a greater than a one-standard deviation (SD) reduction relative to their current location (see SDs above).
Significant at 1%.
Significant at 5%.
We find that, relative to the level of representation in their departure county, both Hispanic and Asian/PI physicians are more likely to stay in a county with similar levels of representation (Hispanic physicians: move to county with greater representation, OR: 0.23, p<.01; move to county with lesser representation, OR: 0.52, p<.01; Asian/PI physicians: move to county with greater representation, OR: 0.29, p<.01; move to county with lesser representation, OR: 0.47, p<.01).
Destination models for newly graduated California residents also yielded similar results (results not shown). All minority residents were less inclined to move to areas where physicians from their respective groups had higher levels of representation (blacks: OR 0.17, p<.01; Hispanics: OR 0.10, p<.01; Asian/PIs: OR 0.04, p<.01). Furthermore, black residents (OR 3.22, p=.065) were more likely to move to areas where black physicians had lower levels of representation.
DISCUSSION
Previous work has also shown that racially/ethnically concordant relationships are valued in the health care market and their value is at least partially embodied in earnings per hour premiums for minority physicians in areas where they are underrepresented (Brown et al. 2007). Economic theory predicts that these price signals should work to distribute physicians more evenly across geographical areas as the supply of minority physicians equilibrates with the demand for them in areas where they are relatively more needed.
It is important to note that these market signals will be present even in a state where minority physicians are underrepresented in most counties. It is the relative underrepresentation that matters in this case. Market signals work when they vary from place to place. These signals will vary to the degree that underrepresentation varies and as shown in Table 2 there is a large variation around the mean level of physician representation for each racial/ethnic group.
Our departure models found that black and Hispanic physicians (but not residents) are more likely to remain in an area as the level of underrepresentation of physicians from their respective groups worsens relative to other areas. Our destination models found that black, Asian/PI, and Hispanic physicians tend to move to areas where the level of representation is similar to that of their previous location. Our destination models of residents just entering the job market showed that black residents are more likely to move to areas where they are more underrepresented.
In sum, Hispanic and black physicians tend to not leave areas in which physicians from their racial/ethnic group are underrepresented once they settle in such areas, and when they move, they tend to move to areas similar to those that they are from. While we found that only black physicians just completing residency move to areas where they are more underrepresented, the fact that Hispanic physicians are underrepresented in all but one California county and have the greatest average underrepresentation suggests that anywhere they move to is unlikely to improve or worsen the situation of Hispanic patients.
These patterns show, with respect to California, that current market forces and individual preferences will likely move black and Hispanic physicians to where they need to be. However, a large increase in the number of black and Hispanic physicians will be required before these market forces and individual preferences will make a substantial difference. The distribution of Asian/PI physicians across California provides a lesson for how we may expect black and Hispanic physicians to finally distribute themselves, given adequate numbers and facing the same market forces. The data suggest that if black and Hispanic physicians behave similarly to Asian/PI physicians, then large increases in the numbers of black and Hispanic physicians would be expected to solve the problem of underrepresentation of these two groups across California almost completely without any other changes in policy. As of 2000, Asian/PI physicians were underrepresented by more than 1 percent in only four counties in California. Every other county had adequate representation.
Limitations of this study include some potentially small biases in our findings due to measurement errors in the AMA Masterfile, which are extensively discussed in the data section above. An important additional limitation is that the conclusions in the above discussion of measurement error are based on the assumption that measurement error occurs at random. The degree to which measurement error is correlated with race/ethnicity is the degree to which the conclusions of the earlier discussion will cease to hold. However, we are unaware of available data that would allow us to test whether any measurement error in the AMA Masterfile is correlated with race/ethnicity.
In addition, the external validity of this study only extends to states with large proportions of racial/ethnic minority groups in their population such that physicians may be influenced to locate among groups racially/ethnically concordant to themselves. While not all states have proportions of each racial/ethnic group similar to California, many states have large proportions of one or more racial groups. Twenty-four states have black populations equal to or larger than California. Arizona, Colorado, Florida, Nevada, New Mexico, and Texas all have large Hispanic populations. Hawaii also has a large Asian/PI population. In addition, the results of this study may have been somewhat different if a smaller geographical unit was used.
Future work should examine how many black and Hispanic physicians would need to be produced, based on our understanding of minority physician migration within California, in order for there to be minimal (<1 percent) underrepresentation of black and Hispanic physicians in any California county. While it is unlikely that perfect representation can be achieved in the near future, future work should ascertain a reasonable threshold to guide policy.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This project was funded by the California Program on Access to Care, Office of the President, University of California.
Disclosures: None.
Disclaimers: None.
NOTES
Brown et al. (2007) did not find similar results for black physicians, but their paper suggested that similar findings may be found for black physicians when an oversampling of black physicians is used. We assume that this would be true in this paper.
No physicians were recorded in Alpine County during any year, and no physicians were recorded in Sierra County during 2001 and 2002.
Although we do not include physicians who leave practice in our models, any error in reporting this type of practice change would also affect our measures of physician representation. The overall 6.9 percent figure varies by race/ethnicity: 8.3 percent (blacks), 7.6 percent (Hispanics), 6.7 percent (Asian/PIs), and 6.9 percent (whites).
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Brown TT, Scheffler RM, Tom S, Schulman K. Does the Market Value Racial and Ethnic Concordance in Potential Physician–Patient Relationships? Health Services Research. 2007;42(2):706–26. doi: 10.1111/j.1475-6773.2006.00634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor JC, Miles EL, Baker LC, Barker DC. Physician Service to the Underserved: Implications for Affirmative Action in Medical Education. Inquiry. 1996;33:167–80. [PubMed] [Google Scholar]
- Cattaneo and Stroud. Statewide HMO and Special Programs Enrollment Study. Burlingame, CA: Cattaneo & Stroud Inc; 2003. [Google Scholar]
- Cattaneo and Stroud. Statewide HMO & Special Programs Enrollment Study. Burlingame, CA: Cattaneo & Stroud Inc; 2004. [Google Scholar]
- Cooper LA, Roter DJ, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-Centered Communication, Ratings of Care, and Concordance of Patient and Physicians Race. Annals of Internal Medicine. 2003;139:907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Department of Finance. Population Projections by Race/Ethnicity for California and Its Counties 2000–2050. Sacramento, CA: State of California; 2004. Available at http://www.dof.ca.gov/HTML/DEMOGRAP/ReportsPapers/Projections/P3/P3.php[accessed on July 15, 2008] [Google Scholar]
- DeVaro JL, Lacker JM. Errors in Variables and Lending Discrimination. Federal Reserve Bank of Richmond Economic Quarterly. 1995;81:19–32. [Google Scholar]
- Escarce JJ, Polsky D, Wozniak GD, Kletke PR. HMO Growth and the Geographic Redistribution of Generalist and Specialist Physicians, 1987–1997. Health Services Research. 2000;35:825–48. [PMC free article] [PubMed] [Google Scholar]
- Frey WH, Liaw KL, Xie Y, Carlson MJ. Interstate Migration of the U.S. Poverty Population: Immigration ‘Pushes’ and Welfare Magnet ‘Pulls’. Population and Environment. 1996;17:491–536. [Google Scholar]
- Garcia JA, Paterniti DA, Romano PS, Kravitz RL. Patient Preferences for Physician Characteristics in University-Based Primary Clinics. Ethnicity and Disease. 2003;13:259–67. [PubMed] [Google Scholar]
- Gartland JJ, Hoja M, Christian EB, Callahan CA, Nasca TJ. African American and White Physicians: A Comparison of Satisfaction with Medical Education, Professional Careers, and Research Activities. Teaching and Learning in Medicine. 2003;15:106–12. doi: 10.1207/S15328015TLM1502_06. [DOI] [PubMed] [Google Scholar]
- Gray B, Stoddard J. Physician–Patient Pairing: Does Racial and Ethnic Congruity Influence Selection of a Regular Physician? Journal of Community Health. 1997;22:247–59. doi: 10.1023/a:1025148302636. [DOI] [PubMed] [Google Scholar]
- Huber PJ. The Behavior of Maximum Likelihood Estimates under Nonstandard Conditions. In: Le Cam Lucien M, Neyman Jerzy., editors. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Vol. 1. Berkeley, CA: University of California Press; 1967. pp. 221–223. [Google Scholar]
- Institute of Medicine. In the Nation's Compelling Interest: Ensuring Diversity in the Health-Care Workforce. Washington, DC: National Academies Press; 2004. Available at http://books.nap.edu/catalog/10885.html[accessed on July 15, 2008] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Race, Ethnicity & Medical Care: Survey of Public Perceptions and Expectations. Menlo Park, CA: Henry J. Kaiser Family Foundation; 1999. Available at http://www.kff.org/minorityhealth/19991014a-index.cfm[accessed on July 15, 2008] [Google Scholar]
- Kletke PR. Physician Workforce Data: When the Best Is Not Good Enough. Health Services Research. 2004;39:1251–5. doi: 10.1111/j.1475-6773.2004.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, Bindman A. The Role of Black and Hispanic Physicians in Providing Health Care for Underserved Populations. New England Journal of Medicine. 1996;334:1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- Ku L, Waidmann T. How Race/Ethnicity, Immigration Status and Language Affect Health Insurance Coverage, Access to Care and Quality of Care among the Low-Income Population. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2003. Available at http://www.Kff.org/uninsured/loader.cfm?url=/commonsport/security/getfile.cfm&PAGEID=22103[accessed on July 15, 2008] [Google Scholar]
- LaVeist TA, Carroll T. Race of Physician and Satisfaction with Care among African-American Patients. Journal of National Medical Association. 2002;94:937–43. [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A. Is Doctor–Patient Race Concordance Associated with Greater Satisfaction with Care? Journal of Health and Social Behavior. 2002;43:296–306. [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A, Jones KE. The Association of Doctor–Patient Race Concordance with Health Services Utilization. Journal of Public Health Policy. 2003;24:312–23. [PubMed] [Google Scholar]
- Lewin-Epstein N. Determinants of Regular Source of Health Care in Black, Mexican, Puerto Rican, and Non-Hispanic White Populations. Medical Care. 1991;29:543–7. doi: 10.1097/00005650-199106000-00013. [DOI] [PubMed] [Google Scholar]
- Liaw KL, Ledent J. Nested Logit Models and Maximum Quasi-Likelihood Method: A Flexible Methodology for Analyzing Interregional Migration Patterns. Regional Science and Urban Economics. 1987;17:676–88. doi: 10.1016/0166-0462(87)90069-x. [DOI] [PubMed] [Google Scholar]
- Ma GX. Between Two Worlds: The Use of Traditional and Western Health Services by Chinese Immigrants. Journal of Community Health. 1999;24:421–37. doi: 10.1023/a:1018742505785. [DOI] [PubMed] [Google Scholar]
- Morehouse Medical Treatment and Effectiveness Center. A Synthesis of the Literature: Racial and Ethnic Differences in Access to Medical Care. Menlo Park, CA: Henry J. Kaiser Family Foundation; 1999. Available at http://www.kff.org/minorityhealth/1526-index.cfm[accessed on July 15, 2008] [Google Scholar]
- Newhouse JP, Williams AP, Bennett BW, Schwarz WB. Does the Geographical Distribution of Physicians Reflect Market Failure? Bell Journal of Economics. 1982;13:493–505. [Google Scholar]
- Nugent WR, White LG, Basham R. A ‘Devil’ Hidden in the Details: The Effects of Measurement Error in Regression Analysis. Journal of Social Service Research. 2000;27:53–75. [Google Scholar]
- Polsky D, Kletke PR, Wozniak GD, Escarce JJ. HMO Penetration and the Geographic Mobility of Practicing Physicians. Journal of Health Economics. 2000;19:793–809. doi: 10.1016/s0167-6296(00)00053-9. [DOI] [PubMed] [Google Scholar]
- RAND California. California Statistics [Database Online] Santa Monica, CA: RAND California; 2005. Available at http://www.kff.org/minorityhealth/1526-index.cfm[accessed on July 15, 2008] [Google Scholar]
- Saha S, Komaromy M, Koepsell T, Bindman A. Physician–Patient Racial Concordance and the Perceived Quality and Use of Health Care. Archives of Internal Medicine. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Saha S, Taggart SH, Komaromy M, Bindman AB. Do Patients Choose Physicians of Their Own Race? Health Affairs. 2003;19:76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- Schnittker J, Liang K. The Promise and Limits of Racial/Ethnic Concordance in Physician – Patient Interaction. Journal of Health Politics, Policy and Law. 2006;31(4):811–38. doi: 10.1215/03616878-2006-004. [DOI] [PubMed] [Google Scholar]
- Stefanski LA, Carroll RJ. Covariate Measurement Error in Logistic Regression. Annals of Statistics. 1985;13:1335–51. [Google Scholar]
- Sullivan Commission. “Missing Persons: Minorities in the Health Professions” [accessed on July 15, 2008]. Available at http://ca.rand.org/stats/statistics.html.
- U.S. Census Bureau. “Selected Housing Characteristics, 2002. American Community Survey Summary Tables” [accessed on July13, 2008]. Available at http://www.jointcenter.org/healthpolicy/docs/SullivanExecutiveSummary.pdf.
- U.S. Census Bureau. “Selected Economic Characteristics, 2002. American Community Survey Summary Tables” [accessed on July 13, 2008]. Available at http://www.census.gov/acs/www/Products/Ranking/2002/R04T040.htm.
- White H. A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48:817–30. [Google Scholar]
- Wooldridge JM. Introductory Econometrics: A Modern Approach. Mason, OH: Thomson South-Western; 2006. [Google Scholar]
- Yeo S. Language Barriers and Access to Care. Annual Review of Nursing Research. 2004;22:59–73. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


