Abstract
Objective
To estimate the costs associated with formal and self-managed daily practice teams in nursing homes.
Data Sources/Study Setting
Medicaid cost reports for 135 nursing homes in New York State in 2006 and survey data for 6,137 direct care workers.
Study Design
A retrospective statistical analysis: We estimated hybrid cost functions that include team penetration variables. Inference was based on robust standard errors.
Data Collection
Formal and self-managed team penetration (i.e., percent of staff working in a team) were calculated from survey responses. Annual variable costs, beds, case mix-adjusted days, admissions, home care visits, outpatient clinic visits, day care days, wages, and ownership were calculated from the cost reports.
Principal Findings
Formal team penetration was significantly associated with costs, while self-managed teams penetration was not. Costs declined with increasing penetration up to 13 percent of formal teams, and increased above this level. Formal teams in nursing homes in the upward sloping range of the curve were more diverse, with a larger number of participating disciplines and more likely to include physicians.
Conclusions
Organization of workforce in formal teams may offer nursing homes a cost-saving strategy. More research is required to understand the relationship between team composition and costs.
Keywords: Nursing homes, costs, teams, quality, cost effectiveness
Interdisciplinary and multidisciplinary teams are often viewed as a more effective way to deliver health care (Halstead 1976; Mickan and Rodger 2000; Lawrence 2002; Lemieux-Charles and McGuire 2006;), especially to patients requiring complex services, such as those in need of chronic care (Wagner et al. 2001; Shortell et al. 2004; Wagner 2004;) or in long-term care settings (Heinemann and Zeiss 2002). Such teams have been credited with better patient outcomes, both in acute (Shortell et al. 1994; Gittell et al. 2000;) and long-term care programs (Mukamel et al. 2006), and have been associated with lower error rates and provision of higher quality patient care (Shortell et al. 1994; Edmondson 1996; Rafferty, Ball, and Aiken 2001; West et al. 2002; Alexander et al. 2005; Proudfoot et al. 2007;). Work environments organized around teams have also been found to exhibit better working conditions, including reduced staff turnover and absenteeism, increased staff motivation, and reduced staff conflict (Mitchell et al. 1996; Gittell et al. 2000; Firth-Cozens 2001; Pearson et al. 2006; Proudfoot et al. 2007;).
In nursing homes, interdisciplinary care planning teams are the norm. They are mandated by the clinical guidelines for the Resident Assessment Instrument/Minimum Data Set (RAI/MDS) process, which is required by the Centers for Medicare and Medicaid Services (CMS) of the >90 percent of U.S. nursing homes that are Medicare or Medicaid certified (Forbes-Thompson et al. 2006). It is also a condition of accreditation by the Joint Commission on Accreditation of Healthcare Organizations (JCOAH 2004; Dellefield 2006;). These teams develop residents' care plans, but they do not provide ongoing daily care.
Nursing home staff providing daily care to nursing home residents may or may not be organized in teams. Studies suggest that such teams may lead to better resident outcomes. Rantz et al. (2004) studied 92 Missouri nursing homes and attributed better patient outcomes to team and group processes in the provision of daily care. Yeatts et al. (2004) and Yeatts and Cready (2007) studied five facilities and based on qualitative and quantitative data show that when CNAs are organized in teams there was a modest positive effect on CNAs' empowerment and performance and on residents' care. Scott-Cawiezell et al. (2005) in a purposeful sample of 32 nursing homes attributed better care and resident morale to teamwork based on key informant interviews. Berlowitz et al. (2003) have shown that greater implementation of quality improvement efforts in nursing homes was associated with emphasis on innovation and teamwork. Others have also found an association between organizational processes related to teamwork, such as leadership, communication, and interaction among staff, and better resident outcomes (Sheridan, White, and Fairchild 1992; Anderson, Issel, and McDaniel Jr 2003; Rantz et al. 2003; Scott-Cawiezell et al. 2003;).
While the nursing home literature suggests that teamwork may be associated with better quality of care, much less is known about the cost consequences of teamwork. Burl and Bonner (1991), Burl, Bonner, and Rao (1994), Burl et al. (1998), and Aigner, Drew, and Phipps (2004) found that teams of nurse practitioners and physicians are more cost effective than physicians alone in nursing homes. Vu et al. (2007) provided evidence that specialized teams focused on wound care provide cost-effective care. Rantz et al. (2004) examined the relationship between costs and resident outcomes in 92 nursing homes in Missouri, and while they did not offer direct evidence, they speculated that there might be efficiencies gained from the team approach adopted by homes that experience better outcomes. None of these studies examined the cost implications of employing multidisciplinary teams to provide the full spectrum of daily care in nursing homes.
In the study we report here we take advantage of data that were collected for a study of a large number of nursing homes in New York State (NYS) regarding the organization of their direct care workers into formal and self-managed teams. We merge this information with expenditures data reported in their Medicaid cost reports and use regression techniques to estimate cost functions. We adapt the basic cost function derived from economic principles to include variables describing the penetration of formal and self-managed teams in each nursing home, and thus are able to estimate the relationship between teams and costs.
BACKGROUND: DAILY PRACTICE TEAMS IN NURSING HOMES
Nursing home residents receive a complex set of services, including help with activities of daily living (ADLs) such as eating, bathing, and toileting; rehabilitation; social activities; and medical care. This care is provided by many different disciplines. While the majority of tasks are performed by nursing staff—certified nurses' assistants (CNAs), licensed practical nurses (LPNs), and to a lesser degree, registered nurses (RNs)—others, including therapists, nutritionists, social workers, and physicians, may participate in care provision as well. All these individuals may work independently or in teams. The teams may be formally organized by management, with explicit protocols and procedures, or they may be self-organized by the workers themselves and occur spontaneously. The nature and organization of nursing homes, into multiple units and wings, allows for the simultaneous coexistence of staff in all three modalities: no teams, self-managed teams, and formal teams.
Temkin-Greener et al. (2009) studied the prevalence and the predictors of these teams in a large-scale study in NYS. The data collected in that study are the data used for the study we present here. We, therefore, briefly describe the parent study and summarize its findings vis-à-vis the type of teams in the facilities included in that study, and we refer the reader for further detail to Temkin-Greener et al. (2009). The parent study consisted of a survey of direct care staff (N=7,418) conducted in 2006 in 162 NYS nursing homes with 50 or more beds. Direct care staff were those who self-identified as providing daily, hands-on care to residents. The survey addressed the organization of work environment and the presence of daily practice teams. The survey did not provide a definition of team or teamwork to the respondents. Rather, it guided the respondents through a series of questions. The respondents were asked if they are members of any teams that exist in their facility, and if so, what were these teams' functions (e.g., prepare the plan of care, quality improvement, specialized care such as wound care, etc.). They were also asked whether they were part of a team that provided daily resident care. Those who reported being part of a daily practice team were asked to identify other team members (e.g., RNs, therapists, etc.) and to designate how their teams are organized. They were asked to select whether they practiced in a formally organized team to which they were assigned by management or whether they were part of a self-managed team with staff organizing themselves into specific work teams. The respondents were also asked who their team leaders were and how often such teams met to discuss resident care.
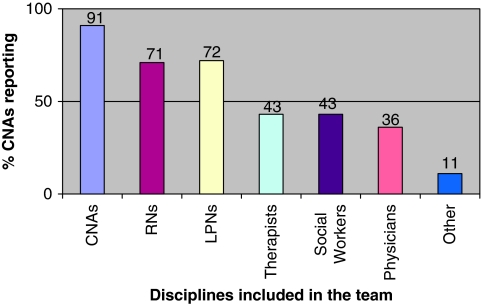
In an average facility, 15.9 percent of the direct care workers reported working in daily practice teams, either formal or self-managed teams (Temkin-Greener et al. 2009). With the exception of three facilities, all nursing homes reported some proportion of daily practice teams, but none reported >44 percent. Figure 1 shows the composition of the teams based on the reports by the CNAs. Similar responses were obtained from other members of the team (e.g., RNs or CNAs). This demonstrates that these teams were indeed largely multidisciplinary and included a variety of personnel, dominated by nursing, but including therapists, social workers, and physicians. There were no substantial differences in composition between self-managed and formal teams. Almost half (46 percent) of responders indicated that they met with their team members daily to discuss patient care and another 27 percent meet at least weekly. These teams were typically led by RNs (reported by 50–60 percent of responders) or LPNs (reported by about 20 percent of responders). It is also interesting to note that primary assignment, that is, assigning staff to the same resident, was as prevalent (averaging about 44 percent) in all facilities, irrespective of whether the work force was organized in teams.
Figure 1.
Composition of Daily Care Teams*
*Information based on the survey question: “Who else is on your team?”
METHODS
Sample and Data
Survey data from the parent study described above were merged with the 2006 NYS Medicaid Cost Reports. The Medicaid cost reports are annual financial reports mandated, audited for accuracy, and used by the state to calculate Medicaid payment rates for nursing homes. They include information about expenditures, outputs (such as inpatient days, home health visits, etc.) and input price (such as wages by staff category), number of beds, and ownership. Case-mix information, measured by the Resource Utilization Groups (RUGs) III for each facility, was obtained separately from the NYS Department of Health. RUGs scores reflect the resource needs of each resident, based on their acuity, frailty, and rehabilitation needs, and are used by NYS to determine payment rates for nursing homes.
The initial sample included 7,418 direct care workers in 162 nursing homes. Due to missing cost report and case-mix data, the final sample included 6,498 direct care workers in 140 facilities.
Variables
Penetration of Direct Care Teams
Based on survey responses from all direct care workers we distinguished between those providing daily care in teams assigned by management, which we denote as formal teams, and those who self-organize their daily care work in teams, which we denote as self-managed. We measured the penetration of these teams in each facility by calculating the percent of direct care responders who reported being members of each team type. We note that these definitions recognize the possibility that facilities may accommodate simultaneously workers in formal teams, self-managed teams, and workers who are not working in teams to provide daily resident care. Such organization of work appears to reflect the reality in many nursing homes in which different floors or units are managed differently.
Cost and Other Facility Characteristics
The dependent variable was annual variable costs, that is, those costs that vary with the level of outputs produced by the facility. It was calculated based on the facility's total expenditures, excluding capital costs (depreciation of leases and rentals, depreciation of the major equipment, and interest on capital debt). Outputs included total inpatient days adjusted for case mix by interaction with the RUGs III score for the facility, total number of admissions, total number of outpatient visits, total number of home care visits, and total number of adult day care days. Hourly wages (input price) were derived by labor category as the total compensation (salaries plus benefits) divided by total hours paid. We only included the wages for CNAs and management (i.e., the administrator, the medical director, the director of nursing, etc.) in our model since the wages of RNs, LPN, and CNAs were highly correlated.
Methods
Assuming rational economic behavior and hence cost minimization, cost functions typically model costs as a function of exogenous outputs (e.g., inpatient days and outpatient services) and wages, assuming that the technology is fixed (Silberberg 1978). They may also include other variables expected to shift the cost function, such as region. In this study we are interested in the impact of teams on costs and, therefore, include them to test the hypothesis that the cost function is shifted in facilities with teams. We estimated a hybrid cost function following Nyman (1988) and Mukamel and Spector (2000) as follows:
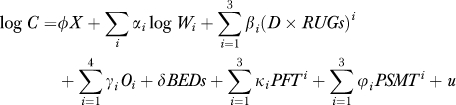 |
where C is annual variable costs; W a vector of wages; D×RUGs case-mix adjusted inpatient days; O a vector of other outputs, including admissions, adult day care days, home health, and outpatient clinic visits; PFT the percent penetration of formal teams; and PSMT the percent penetration of self-managed teams. Beds are included to control for the level of capital because we are estimating a variable cost function. X is a vector of other facility and environmental characteristics that have been shown to shift nursing home cost functions in previous studies, including ownership, competition measured by the Herfindahl–Hirschman Index (HHI) (calculated based on occupied beds and assuming that market boundaries coincide with counties), and New York City location (Mukamel and Spector 2000). All these variables have been defined in the previous section.
Unlike the structural cost function, the hybrid specification that we adopted recognizes the potential for heterogeneity across types of nursing homes (e.g., ownership) and also allows for zero outputs. The latter is important in the context of nursing homes because many nursing homes do not provide all outpatient services and will, therefore, have zero values for some outputs. The structural cost function, which typically specifies outputs as log transforms cannot accommodate zeros, while the hybrid cost function can. Inpatient days and team penetration were entered as linear, squared, and cubed terms to allow for both economies and diseconomies of scale (Grannemann, Brown, and Pauly 1986).
Because the survey responses were biased toward the nonprofits facilities (see “Results”) we also estimated a weighted regression model in which we used probability weights to reflect the ownership distribution of nursing homes in the state as a whole. The results were very similar and, therefore, we report only the results based on the weighted regression.
To account for potential heteroscedasticity across observations, inference was based on robust standard errors. Because of the high collinearity between the linear, squared, and cubed team penetration variables, standard errors are likely to be inflated, and statistical significance was, therefore, inferred based on a joint F test of the hypothesis that all three terms are jointly zero.
We have also performed tests for outliers using Cook's D and excluded five outlier observations for a final sample of 135 nursing homes and 6,137 direct care workers.
To demonstrate the relationship between costs and team penetration we calculated the predicted annual variable cost for all nursing homes, using their actual values for team penetration and sample averages for all other variables. In converting from log(cost) to costs we included the smearing effect (Duan et al. 1982).
RESULTS
Sample and Response Bias
Table 1 provides descriptive statistics for the 135 nursing homes included in the final analysis as well as all 531 nursing homes in NYS who meet the parent study inclusion criteria and have cost report data. The average penetration of both formal and self-managed teams was low, at 8.4 and 7.4 percent, respectively. It was, however, rather variable, with standard deviations of 6.4 percent and 5.5 percent, respectively. The correlation between formal and informal team penetration rates was −0.18 (p=.03). The study sample was not significantly different from all nursing homes in costs, but it was significantly (at the 0.05 level) more likely to include nonprofit facilities (66 vs. 51 percent), to have more inpatient days (by 12 percent), and to report lower management wages (by 13 percent). As noted above, the regression model was weighted to account for the difference in ownership distribution between the sample and population, although the regression estimates were very similar.
Table 1.
Comparison of Study Sample to All New York State Study Eligible Nursing Homes
| Sample (N=135) |
All NYS Study Eligible Nursing Homes (N=531) |
|||
|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |
| Percent of direct care staff organized in formal teams | 8.4 | 6.4 | NA | NA |
| Percent of direct care staff in self-managed teams | 7.4 | 5.5 | NA | NA |
| Annual variable costs ($1000) | 20,135 | 17,949 | 17,988 | 16,896 |
| Inpatient days | 77,071* | 48,273 | 68,709 | 40,942 |
| Inpatient admissions | 408 | 334 | 367 | 303 |
| Average RUG scores | 1.18 | 0.12 | NA | NA |
| Adult day care days | 2,481* | 5,041 | 3,530 | 17,125 |
| Number of beds | 215 | 136 | 196 | 113 |
| Home health care visits | 7,964 | 42,580 | 8,281 | 59,039 |
| Outpatient clinics | 1,083 | 7,572 | 499 | 4,720 |
| Management hourly wage | 43.35* | 14.39 | 49.12 | 26.72 |
| CNA hourly wage | 18.29 | 4.70 | 19.04 | 5.29 |
| Nonprofit ownership (%) | 66%* | 51% | ||
Significant difference at the 0.05 level.
Cost Function
Table 2 shows the estimated cost function. As expected, costs significantly increase with outputs—case-mix adjusted days, admissions, adult day care days, home health visits, and outpatient clinic visits. The functional dependence on case-mix adjusted days is the typical one, exhibiting first increasing returns to scale and then decreasing returns to scale. Costs also increase significantly with wages. They are higher in nonprofit nursing homes, possibly reflecting higher quality care in those facilities. Costs were not significantly associated with either competition or upstate location (at the 0.1 level), and therefore the final model we are presenting excludes these variables.
Table 2.
Estimated Annual Variable Cost Function with Probability Weights (Dependent Variable: Log of Variable Cost)
| Independent Variables | Coefficient | Robust Standard Error | p Value* |
|---|---|---|---|
| % direct care staff in formal teams | |||
| Linear | 0.012 | 0.968 | .99** |
| Squared | −2.332 | 7.626 | .76** |
| Cubed | 11.956 | 15.768 | .49** |
| % of direct care staff in self-managed teams | |||
| Linear | −0.487 | 1.124 | .67*** |
| Squared | 11.449 | 13.352 | .39*** |
| Cubed | −38.929 | 37.744 | .30*** |
| Beds | 0.214 × 10−2 | 0.254 × 10−3 | .00 |
| Case-mix adjusted days/1,000 | |||
| Linear | 0.226 | 0.192 × 10−2 | .00 |
| Squared | −0.115 × 10−3 | 0.123 × 10−4 | .00 |
| Cubed | 1.76 × 10−7 | 0.248 × 10−9 | .00 |
| Admissions | 0.213 × 10−3 | 0.433 × 10−4 | .00 |
| Adult day care days/1,000 | 0.010 | 0.231 × 10−2 | .00 |
| Home health care visits/10,000 | 0.027 | 0.349 × 10−2 | .00 |
| Outpatient clinic visits/1,000 | 0.007 | 0.928 × 10−3 | .00 |
| Log management wages | 0.170 | 0.058 | .00 |
| Log CNA wages | 0.535 | 0.077 | .00 |
| Nonprofit facility | 0.093 | 0.027 | .00 |
| Constant | 12.620 | 0.225 | .00 |
N=135.
R2=0.97.
Based on robust standard errors.
p value for the hypotheses that the linear, squared, and cubed terms are jointly significant is .004 (F3, 117=4.77).
p value for the hypotheses that the linear, squared, and cubed terms are jointly significant is .426 (F3, 117=0.94).
The individual variables of team penetration are not significantly associated with costs. However, because we include linear, squared, and cubed terms, they are highly collinear and standard errors tend to be inflated. An F test of the hypothesis that all three terms are jointly significant has a p value of .004 for penetration of the formal teams, indicating that costs are associated with formal teams. However, for self-managed team penetration, the p value is .426, indicating that these types of teams do not have an impact on costs. Similar results were obtained when we estimated models with only formal or self-managed teams variables.
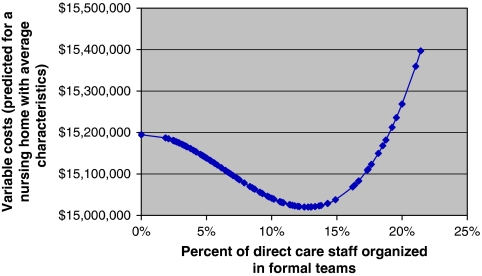
Figure 2 demonstrates the relationship between costs and penetration of formal teams. The figure is based on actual values for formal team penetration, and those are indicated by the dots in the graphs. Most observations are in the range between 4 and 13 percent penetration and in this range costs are declining as team penetration increases. For team penetration of 15 percent and above, costs are increasing as penetration increases. We note that in this range, there are many fewer observations. Only 30 of the 135 (22 percent) nursing homes in our sample have team penetration above this level.
Figure 2.
Predicted Variable Annual Costs as Function of Formal Teams Penetration (Based on the Estimated Cost Function)
The magnitude of the savings associated with formal teams is not large compared with the total annual expenditures level of nursing homes. The largest savings that can be realized by increasing formal team penetration to the minimum of the cost curve point is 1.16 percent.
DISCUSSION
In this paper we examine data for nursing homes in NYS and find that prevalence of teams is associated with cost savings when such teams are formally organized, but not when they are self-managed. While the association is highly statistically significant, with a p value of .004, it is not very large in terms of its monetary impact. The most that can be saved by instituting formal teams is around $174,000 per year, which is roughly equivalent to the cost of two residents stays. Nevertheless, the cost savings we are measuring are net costs, reflecting the total savings that can be achieved after any investments in team creation and maintenance, suggesting that formal teams are a cost-saving strategy for nursing homes. Coupled with the information from other studies (see our review in the introduction section) that suggests that teams may result in better patient outcomes, formally organized direct care teams should be considered as an important strategy leading to both better quality care and lower costs.
Despite these encouraging findings, the analysis also raises a puzzling question. We find cost savings over only a relatively low range of penetration of direct care teams, of no more than 13 percent. In fact, at penetration of around 15 percent, we observe increasing costs, that is, diseconomies of scale. While it is not unreasonable to expect that the benefits of teams will level off at some point and perhaps even that diseconomies of scale will set in at really high penetration levels, it is surprising to find that costs are increasing at relatively low levels of penetration. What might explain these findings? Below we consider several hypotheses and compare nursing homes in the downward and upward sloping regimes of the cost curve to offer potential explanations.
One possibility is that the nursing homes in the upward sloping part of the curve are facilities in which teams contribute to higher quality care but at a higher cost. For example, teamwork might increase quality by making it easier for staff to perform some duties, such as transferring or turning a patient. Frequent turning is important for prevention of pressure ulcers. This task is easier to accomplish if performed by two individuals and is, therefore, likely to be done more often when staff is working in teams. Working in teams also increases oversight, by both peers and supervisors, making it more likely that staff will not shirk, adhere to protocol, and perform all tasks as expected. Such increased activities are likely to result in better care and improved patient outcomes, and also higher costs, as staff spends more time on the same activities helping each other, or performing activities that otherwise may not be undertaken at all because of shirking. To test this hypothesis we compared the average number of deficiency citations per bed (all health deficiencies, quality-of-life deficiencies only, and quality-of-care deficiencies only) and the average score of each of the 19 quality measures (QMs) published in the Nursing Home Compare in the fourth quarter of 2006 across the nursing homes in the downward and the upward sloping parts of the cost curve. We found no significant differences (at the 0.05 level) between the two groups, suggesting that the difference in the relationship between costs and team penetration is not likely explained by processes that lead to higher quality. We should, however, note that the measures of quality that were available to us to test this hypothesis are rather crude. The variation in deficiency citations is known to depend on policies of the local state office issuing the citations (Mukamel 1997), and the QMs in the Nursing Home Compare report card are not risk adjusted for the most part, and have been shown to lead to different quality ranking than QMs with a more extensive risk adjustment (Mukamel et al. 2008). It is, therefore, possible that our inability to detect a difference in quality between the two groups of nursing homes is due to the inadequacy of the QMs that were available to us.
Another potential explanation is that nursing homes with teams above 15 percent penetration are those that push teams “too far,” imposing this type of work organization on staff that is not inclined, motivated, or comfortable working in teams. Teamwork is associated with both costs and benefits. There are costs, such as meeting times and training of members in team processes that are necessary for the management and maintenance of the team. In a well-functioning team we expect these costs to be more than offset by savings due to increased efficiencies and better patient outcomes. Prior studies, in settings other than the nursing home, have shown that patients treated by better functioning teams experience better health outcomes (Rantz et al. 2004; Shortell et al. 2004; Mukamel et al. 2006;) and that better patient outcomes can be associated with lower costs (Mukamel and Spector 2000). Not all teams, however, are well-functioning teams (Temkin-Greener et al. 2004) and the benefits of teamwork may not accrue to teams that are not cohesive and do not work well together. Thus, perhaps nursing homes with higher team penetration are those where management is imposing team structures on staff that do not welcome it and hence those teams incur only the costs and not the benefits of teamwork. To examine this possibility we compared staff satisfaction with their work unit as expressed in their response to the survey question “If I had a chance to change my unit in this facility for the same pay and the same work, I would not want to.” We found no significant differences (at the 0.05 level) between responders in facilities in the upward and the downward parts of the cost curve, suggesting that this may not explain the higher costs when team penetration increases above 15 percent.
Another possible explanation is that the composition of the teams is different in facilities where penetration is higher. Nursing homes with higher team penetration may be those that have progressed further in team development and have created teams that are more extensive and encompass more disciplines, going beyond just nursing staff to include therapists and physicians. Such teams, because of their more specialty-oriented composition, may provide a more extensive and expensive array of services, as the literature on care by specialists versus primary care physicians has demonstrated in other settings (Greenfield et al. 1992). To test this hypothesis we compared the nursing homes in the two regimes of the cost curve on two measures. We find that physicians are more likely to be members of teams in nursing homes in the upward sloping regime of the cost curve, with 31 percent of direct care workers reporting a physician in their team, compared with only 26 percent of workers in homes in the downward sloping regime of the curve (p=.03). We also find that the teams in the homes in the upward sloping part of the cost curve are more likely to have more discipline represented (p=.02), that is, have more specialists.
We should note that these last observations, while possibly explaining the higher costs associated with teams in these nursing homes, when taken together with the prior observation of no differences in quality, raise questions about the benefits of having teams that are more disciplinarily diverse. Further research is clearly needed: to determine whether these results are replicable in other nursing homes; to better understand the differences in team compositions between nursing homes in the two cost curve regimes; and to investigate more carefully the hypotheses we suggest and the cost and quality implications for the use of formal teams in nursing homes.
We should also note several limitations of this study. First, the sample available to us of 135 was small relative to the number of explanatory variables of 16, raising the possibility that the power to detect significant associations might be limited. However, we do find a significant relationship between all the basic cost function variables as well as the formal team penetration variables and costs. Thus, this concern remains only with respect to the self-managed team findings. Furthermore, in a model that included only self-managed team variables and, therefore, had acceptable power (with 13 variables and hence a ratio of 10 between independent variables and observations) we also failed to find a significant relationship between self-managed team penetration and costs (p=.25), contributing to the robustness of our main finding.
We should also note that this study focused on nursing homes in NYS and did not include any proprietary chain facilities. Therefore, the results may not generalize directly to nursing homes nationally. Further research, including different types of facilities, is required.
In summary, this study provides for the first time empirical evidence based on a large sample that formal teams in nursing homes can be cost saving. This conclusion is tempered, however, by the possibility that the composition of the team might be an important factor contributing to its cost effectiveness.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors gratefully acknowledge funding from the National Institute on Aging, Grant # R01 AG23077. We also wish to thank seminar participants at the Center for Health Policy Research, University of California, Irvine, for helpful comments.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Aigner MJ, Drew S, Phipps J. A Comparative Study of Nursing Home Resident Outcomes between Care Provided by Nurse Practitioners/Physicians Versus Physicians Only. Journal of the American Medical Directors Association. 2004;5(1):16–23. [PubMed] [Google Scholar]
- Alexander JA, Lichtenstein R, Jinnett K, Wells R, Zazzali J, Liu D. Cross-Functional Team Processes and Patient Functional Improvement. Health Services Research. 2005;40(5 Pt 1):1335–55. doi: 10.1111/j.1475-6773.2005.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RA, Issel LM, McDaniel RR., Jr Nursing Homes as Complex Adaptive Systems: Relationship between Management Practice and Resident Outcomes. Nursing Research. 2003;52(1):12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlowitz DR, Young GJ, Hickey EC, Saliba D, Mittman BS, Czarnowski E, Simon B, Anderson JJ, Ash AS, Rubenstein LV, Moskowitz MA. Quality Improvement Implementation in the Nursing Home. Health Services Research. 2003;38(1 Pt 1):65–83. doi: 10.1111/1475-6773.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burl JB, Bonner AF. A Geriatric Nurse Practitioner/Physician Team in a Long-Term Care Setting. HMO Practice. 1991;5(4):139–42. [PubMed] [Google Scholar]
- Burl JB, Bonner A, Rao M. Demonstration of the Cost-Effectiveness of a Nurse Practitioner/Physician Team in Long-Term Care Facilities. HMO Practice. 1994;8(4):157–61. [PubMed] [Google Scholar]
- Burl JB, Bonner A, Rao M, Khan AM. Geriatric Nurse Practitioners in Long-Term Care: Demonstration of Effectiveness in Managed Care. Journal of the American Geriatric Society. 1998;46(4):506–10. doi: 10.1111/j.1532-5415.1998.tb02475.x. [DOI] [PubMed] [Google Scholar]
- Dellefield ME. Organizational Correlates of the Risk-Adjusted Pressure Ulcer Prevalence and Subsequent Survey Deficiency Citation in California Nursing Homes. Research in Nursing and Health. 2006;29(4):345–58. doi: 10.1002/nur.20145. [DOI] [PubMed] [Google Scholar]
- Duan N, Manning WG, Morris CN, Newhouse JP. A Comparison of Alternative Models for the Demand for Medical Care. Santa Monica, CA: RAND; 1982. [Google Scholar]
- Edmondson A. Learning from Mistakes Is Easier Said Than Done: Group and Organizational Influences on the Detection and Correction of Human Error. Journal of Applied Behavioral Science. 1996;32(1):5–28. [Google Scholar]
- Firth-Cozens J. Multidisciplinary Teamwork: The Good, Bad, and Everything in Between. Quality in Health Care. 2001;10(2):65–6. doi: 10.1136/qhc.10.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes-Thompson S, Gajewski B, Scott-Cawiezell J, Dunton N. An Exploration of Nursing Home Organizational Processes. Western Journal of Nursing Research. 2006;28(8):935–54. doi: 10.1177/0193945906287053. [DOI] [PubMed] [Google Scholar]
- Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, Laskin R, Lipson S, Siliski J, Thornhill T, Zuckerman J. Impact of Relational Coordination on Quality of Care, Postoperative Pain and Functioning, and Length of Stay: A Nine-Hospital Study of Surgical Patients. Medical Care. 2000;38(8):807–19. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- Grannemann W, Brown S, Pauly MV. Estimating Hospital Costs: A Multiple Output Analysis. Journal of Health Economics. 1986;5(2):107–27. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Greenfield S, Nelson EC, Zubkoff M, Manning W, Rogers W, Kravitz RL, Keller A, Tarlov AR, Ware JE., Jr Variations in Resource Utilization among Medical Specialties and Systems of Care. Results from the Medical Outcomes Study. Journal of the American Medical Association. 1992;267(12):1624–30. [PubMed] [Google Scholar]
- Halstead LS. Team Care in Chronic Illness: A Critical Review of the Literature of the Past 25 Years. Archives of Physical Medicine and Rehabilitation. 1976;57(11):507–11. [PubMed] [Google Scholar]
- Heinemann GD, Zeiss AM. Team Performance in Health Care: Assessment and Development. New York: Kluwer Academic/Plenum Publishers; 2002. [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations (JCOAH) Comprehensive Accreditation Manual for Long-Term Care. Oakbrook Terrace, IL: Joint Commission Resources Inc; 2004. [Google Scholar]
- Lawrence D. From Chaos to Care: The Promise of Team-Based Medicine. Cambridge, MA: Perseus Publishing; 2002. [Google Scholar]
- Lemieux-Charles L, McGuire WL. What Do We Know about Health Care Team Effectiveness? A Review of the Literature. Medical Care Research Review. 2006;63(3):263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- Mickan S, Rodger S. Characteristics of Effective Teams: A Literature Review. Australian Health Review. 2000;23(3):201–8. doi: 10.1071/ah000201. [DOI] [PubMed] [Google Scholar]
- Mitchell PH, Shannon SE, Cain KC, Hegyvary ST. Critical Care Outcomes: Linking Structures, Processes, and Organizational and Clinical Outcomes. American Journal of Critical Care. 1996;5(5):353. [PubMed] [Google Scholar]
- Mukamel D, Glance LG, Li Y, Weimer D, Spector WD, Zinn JS, Mosqueda L. Does Risk Adjustment of the CMS Quality Measures for Nursing Homes Matter? Medical Care. 2008;46(5):532–41. doi: 10.1097/MLR.0b013e31816099c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB. Risk Adjusted Outcome Measures and Quality of Care in Nursing Homes. Medical Care. 1997;35(4):367–85. doi: 10.1097/00005650-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD. Nursing Home Costs and Risk Adjusted Outcome Measures of Quality. Medical Care. 2000;38(1):78–89. doi: 10.1097/00005650-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Temkin-Greener H, Delavan R, Peterson DR, Gross D, Kunitz S, Williams TF. Team Performance and Risk-Adjusted Health Outcomes in the Program of All-Inclusive Care for the Elderly (PACE) Gerontologist. 2006;46(2):227–37. doi: 10.1093/geront/46.2.227. [DOI] [PubMed] [Google Scholar]
- Nyman JA. The Marginal Cost of Nursing Home Care, New York 1983. Journal of Health Economics. 1988;7(4):393–412. doi: 10.1016/0167-6296(88)90022-7. [DOI] [PubMed] [Google Scholar]
- Pearson A, Porritt K, Doran D, Vincent L, Craig D, Tucker D, Long L, Henstridge V. A Comprehensive Systematic Review of Evidence on the Structure, Process, Characteristics and Composition of a Nursing Team That Fosters a Healthy Work Environment. International Journal of Evidence-Based Healthcare. 2006;4(2):118–59. doi: 10.1111/j.1479-6988.2006.00039.x. [DOI] [PubMed] [Google Scholar]
- Proudfoot J, Jayasinghe UW, Holton C, Grimm J, Bubner T, Amoroso C, Beilby J, Harris MF. Team Climate for Innovation: What Difference Does It Make in General Practice? International Journal of Quality in Health Care. 2007;19(3):164–9. doi: 10.1093/intqhc/mzm005. [DOI] [PubMed] [Google Scholar]
- Rafferty AM, Ball J, Aiken LH. Are Teamwork and Professional Autonomy Compatible, and Do They Result in Improved Hospital Care? Quality in Health Care. 2001;10(Suppl 2):ii32–7. doi: 10.1136/qhc.0100032... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz MJ, Grando V, Conn V, Zwygart-Staffacher M, Hicks L, Flesner M, Scott J, Manion P, Minner D, Porter R, Maas M. Getting the Basics Right. Care Delivery in Nursing Homes. Journal of Gerontological Nursing. 2003;29(11):15–25. doi: 10.3928/0098-9134-20031101-07. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Hicks L, Grando V, Petroski GF, Madsen RW, Mehr DR, Conn V, Zwygart-Staffacher M, Scott J, Flesner M, Bostick J, Porter R, Maas M. Nursing Home Quality, Cost, Staffing, and Staff Mix. Gerontologist. 2004;44(1):24–38. doi: 10.1093/geront/44.1.24. [DOI] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Main DS, Vojir CP, Jones K, Moore L, Nutting PA, Kutner JS, Pennington K. Linking Nursing Home Working Conditions to Organizational Performance. Health Care Manage Review. 2005;30(4):372–80. doi: 10.1097/00004010-200510000-00011. [DOI] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Schenkman M, Moore L, Vojir C, Connolly RP, Pratt M, Palmer L. Exploring Nursing Home Staff's Perception of Communication and Leadership to Facilitate Quality Improvement. Journal of Nursing Care Quality. 2003;19(3):242–52. doi: 10.1097/00001786-200407000-00011. [DOI] [PubMed] [Google Scholar]
- Sheridan JE, White J, Fairchild TJ. Ineffective Staff, Ineffective Supervision, or Ineffective Administration? Why Some Nursing Homes Fail to Provide Adequate Care. Gerontologist. 1992;32(3):334–41. doi: 10.1093/geront/32.3.334. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Marsteller JA, Lin M, Pearson ML, Wu SY, Mendel P, Cretin S, Rosen M. The Role of Perceived Team Effectiveness in Improving Chronic Illness Care. Medical Care. 2004;42(11):1040–8. doi: 10.1097/00005650-200411000-00002. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Zimmerman JE, Rousseau DM, Gillies RR, Wagner DP, Draper EA, Knaus WA, Duffy J. The Performance of Intensive Care Units: Does Good Management Make a Difference? Medical Care. 1994;32(5):508–24. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- Silberberg E. The Structure of Economics: A Mathematical Analysis. New York: McGraw-Hill; 1978. [Google Scholar]
- Temkin-Greener H, Cai S, Katz P, Mukamel D. Daily Practice Teams in Nursing Homes: Evidence from New York State. Gerontologist. 2009;49(1):68–80. doi: 10.1093/geront/gnp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temkin-Greener H, Gross D, Kunitz S, Mukamel DB. Measuring Interdisciplinary Team Performance in a Long-Term Care Setting. Medical Care. 2004;42(5):472–81. doi: 10.1097/01.mlr.0000124306.28397.e2. [DOI] [PubMed] [Google Scholar]
- Vu T, Harris A, Duncan G, Sussman G. Cost-Effectiveness of Multidisciplinary Wound Care in Nursing Homes: A Pseudo-Randomized Pragmatic Cluster Trial. Family Practice. 2007;24(4):372–9. doi: 10.1093/fampra/cmm024. [DOI] [PubMed] [Google Scholar]
- Wagner EH. Effective Teamwork and Quality of Care. Medical Care. 2004;42(11):1037–9. doi: 10.1097/01.mlr.0000145875.60036.ed. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, Carver P, Sixta C. Quality Improvement in Chronic Illness Care: A Collaborative Approach. Joint Commission Journal on Quality Improvement. 2001;27(2):63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- West M, Borrill C, Dawson J, Scully J, Carter M, Anelay S, Patterson M, Waring J. The Link between the Management of Employees and Patient Mortality in Acute Hospitals. International Journal of Human Resource Management. 2002;13(8):1299–310. [Google Scholar]
- Yeatts DE, Cready C, Ray B, DeWitt A, Queen C. Self-Managed Work Teams in Nursing Homes: Implementing and Empowering Nurse Aide Teams. Gerontologist. 2004;44(2):256–61. doi: 10.1093/geront/44.2.256. [DOI] [PubMed] [Google Scholar]
- Yeatts DE, Cready CM. Consequences of Empowered CNA Teams in Nursing Home Settings: A Longitudinal Assessment. Gerontologist. 2007;47(3):323–39. doi: 10.1093/geront/47.3.323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.