Abstract
Objective
To design, implement, and evaluate a course on health promotion and literacy.
Design
Course objectives such as the development of cultural competency skills, awareness of personal biases, and appreciation of differences in health beliefs among sociocultural groups were addressed using a team-based learning instructional strategy. Student learning outcomes were enhanced using readiness assessment tests (RATs), group presentations, portfolio reflections, and panel discussions.
Assessment
Comparing precourse and postcourse Inventory for Assessing the Process of Cultural Competence among Healthcare Professionals (IAPCC-R) scores and portfolio responses indicated enhanced progress toward cultural competency. The Student Evaluation of Teaching (SET) provided suggestions for course enhancements.
Conclusions
Evidence supporting enhanced cultural competency after completing the course affirms its value as we prepare pharmacy students to provide patient-centered care in a culturally diverse world.
Keywords: cultural competency, health literacy, health disparities, curriculum
INTRODUCTION
Hepler and Strand's pharmaceutical care model maintains that one of the goals of drug therapy is an improved quality of life.1 Pharmacists must understand their patients', as well as their own, cultural background in order to accomplish these goals.2 By the year 2050, minorities will comprise approximately 50% of the US population.2 Since pharmacy students are living in a multicultural and increasingly diverse world, they must be able to interact and provide patient-centered care in this culturally diverse setting.
The need for including cultural competency training in the pharmacy curriculum has previously been established.3 Guideline 9.1 of the 2007 ACPE accreditation standards states that schools and colleges “must ensure that the curriculum addresses cultural competency, health literacy, health care disparities, and competencies needed to work as a member of or on an inter-professional team.”4 A survey assessing cultural competency content in the curricula found that many schools recognize the need to add curricular content but have not implemented it.5 There have also been reports that have highlighted the effects of elective coursework to enhance cultural competency.6-9
The need for cultural competency also is consistent with the goals of the Southern Illinois University Edwardsville (SIUE) School of Pharmacy. Specifically, the School of Pharmacy aims to inculcate a spirit of respect for diversity. In addition to encouraging faculty members to include these topics across the curriculum, 3 required credits are allocated in the third professional (P3) year to address these curricular needs. The course is titled Health Promotion and Literacy.
The specific objectives of the course were to: (1) develop overall cultural competency; (2) enhance self-awareness of biases; (3) address cultural knowledge such as differences in health beliefs among various sociocultural groups, health disparities, and health literacy issues; and (4) develop skills including health promotion strategies for providing culturally responsive care. This article describes and evaluates the course developing cultural competency in pharmacy students.
DESIGN
A team-based learning approach as described by Larry Michaelson was the primary instructional strategy used for course delivery.10 The essential concept of team-based learning is the development of groups that evolve into cohesive teams by focusing on assignments best developed as teams. In team-based learning, there is minimal use of didactic lectures. Instead, the focus is on students completing preassigned readings and then applying principles to team activities. During the first offering of the course in fall 2007, the class consisted of 81 students organized into 16 teams (15 with 5 members and 1 with 6 members). The teams were organized using a heterogeneous grouping technique. The technique is a random way of assigning students to a group when critical cultural information about students is lacking. It helps to create teams with as much diversity as possible since it is based on a random assignment.10 Teams were assigned to work on specific in-class assignments and exercises throughout the semester, complete Readiness Assessment Tests (RATs) and a summative team project. Team members also were required to provide peer evaluations of each team member's contributions to team assignments. To minimize conflict among individuals, members' peer evaluation scores were the average of points they received from the members of their teams. Points were received for in-class exercises and assignments and for the final project. Students used a rubric for awarding points based on students' preparation for class, contributions to team work, respect for others' ideas, and flexibility when disagreements occurred.
The required textbook was Campinha-Bacote's The Process of Cultural Competence in the Delivery of Healthcare Services. 11 Campinha-Bacote's process of developing cultural competency was used to form the course schedule. The course content was grouped into 7 clusters: (1) creating desire for cultural competency; (2) process of cultural competency in the delivery of healthcare services; (3) cultural awareness; (4) cultural knowledge: health beliefs; (5) cultural skills: communicating; (6) knowledge and skills: health literacy; (7) cultural encounter: team presentations.
A list of the specific readings assigned to cover the variety of course content is available from the author. Students were held accountable for required pre-class readings using the concept of Readiness Assessment Tests (RATs).10
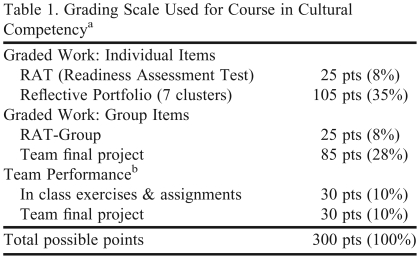
An online Blackboard (Blackboard Academic Suite, Washington, DC) course portfolio was established for the course and all students were taught how to establish their own individual reflective portfolios. Students were required to make the portfolio available to course faculty members for review and grading. Besides RATs, the summative team project, in-class assignments, and portfolio reflections were designed to assess learning of concepts addressed in the various clusters. Faculty members teaching various clusters designed 3 to 5 questions for each cluster reflections. Student portfolio questions are found in Appendix 1. The grading scale used for the course is outlined in Table 1. The criteria used for grading the reflective submissions included knowledge of course content, application of knowledge, and the demonstration of the progression as a journey to cultural competency.
Table 1.
Grading Scale Used for Course in Cultural Competencya
Grading scale: 270 to 300 pts = A; 240 to 269 pts = B; 210 to 239 pts = C; 180 to 209 pts = D; < 180 pts = F
b Peer evaluation scores as assessed by the average of points received from team members
The goal for the first cluster was to create desire for cultural competency training. One challenge was motivating students to want to become culturally competent. The students seemed to be initially apprehensive of the content and value of cultural competency awareness. Some students were unsure about whether enhanced cultural awareness was necessary for pharmacy practice. To motivate students, faculty members presented background information on the benefits of cultural competency and the role of the pharmacist in reducing health disparities and improving health outcomes. The significance of cultural competency due to changing demographics and diversity, as well as key legislation addressing the challenges, were also discussed.
The second cluster addressed the process of cultural competency as described by Campinha-Bacote.11 The process is described as a journey that involves the integration of 5 constructs: cultural desire, cultural awareness, cultural knowledge, cultural skill, and cultural encounters. The journey begins with having a desire to recognize and learn more about various cultures through the process of developing cultural skills to effectively handle a broad spectrum of multicultural settings. Even though the various clusters for the course were organized according to these constructs, the process of cultural competency involves the integration of the different constructs. Organizing the course schedule in clusters according to these constructs was a way of developing the course content. Presentation of the process of cultural competency as a journey was intended to serve as a motivation for life-long learning and continued striving for cultural proficiency.
The third cluster focused on cultural awareness by having students look at their own biases and beliefs. Exercises were adapted from the Center for the Health Professions University of California, San Francisco resource “Toward Culturally Competent Care: A Toolbox for Teaching Communication Strategies.”12 For example, within their team, students examined their own family health beliefs and use of home remedies. Students also examined their attitudes about stereotypes. A short vignette from a Home Box Office (HBO) video, If These Walls Could Talk 2, was also shown in class.13 This vignette depicts the biases and behaviors of the health care system toward an elderly lesbian couple. The student teams were asked to explore their own biases and attitudes after viewing the video.
Differences in health beliefs were explored in cluster 4. Specific health belief models were examined including the health belief model, temporal orientation, trans-theoretical model of change, and the theory of planned behavior.14,15 Culturally diverse case scenarios were also discussed as a way of exploring differences in health beliefs and developing knowledge for communicating in a culturally responsive manner (case scenarios available from authors). Students discussed these cases using the LEARN model for communicating in a culturally responsive manner.16 LEARN signifies (1) Listen with sympathy and understanding to the patient's perception of the problem; (2) Explain your perceptions of the problem; (3) Acknowledge and discuss the differences and similarities; (4) Recommend treatment; and (5) Negotiate agreement.
In cluster 5, communication within families and the role of families in health care decisions as a specific sociocultural group were discussed. For this cluster, the film In the Gloaming was viewed in class.17 This film features a son dying of AIDS who comes home to share his final days with his mother but, in the process, shuts out his father and sister. During team discussions, students reflected on how communication occurred within this family.
Cluster 6 was dedicated to developing knowledge and skills for addressing health literacy concerns. The objectives for this cluster were to (1) develop awareness of the problem of health literacy; (2) recognize the consequences and implications of low health literacy; (3) discuss various tools available to test health literacy; (4) assess the suitability of materials for patients with low health literacy; and (5) discuss the comprehension process with adult learners. Students were asked to assess the suitability of patient education materials using the Suitability Assessment Method (SAM) criteria, and also were asked to determine from non-health-care professionals their understanding of patient information content from magazines or online sources. Videos demonstrating how patients with low literacy levels understand medication information and how they interact with their providers were viewed during class. (These videos are available from the American Medical Foundation and are targeted for developing health care providers' awareness of the extent of understanding of health care information in low literacy patients.18)
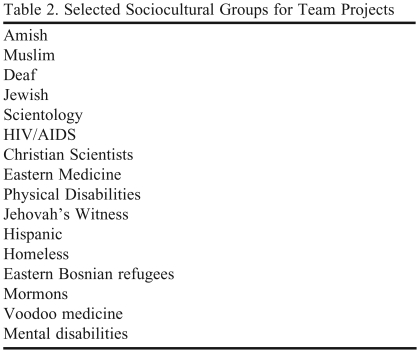
The final cluster was designed to address outcomes expected in cultural encounters given the constraints of a didactic course and lack of access to an experiential component. The purpose of cultural encounter is for direct interaction with people of culturally diverse backgrounds. Course constraints did not permit this direct interaction with various cultural groups. Cluster 7 was designed to simulate cultural encounters using students' team project presentations. The goal of the projects was to address outcomes expected in a cultural encounter. Student teams selected a specific sociocultural group from a provided list of groups. The specific groups selected during the fall 2007 offering are listed in Table 2. Many of the teams interviewed people from the various groups as part of their preparation for their team presentations. Teams were allotted a portion of 3 class sessions during the semester to work on their projects. During the final 3 weeks of the course, each team presented a 20-minute report that highlighted the specific project outcomes (guidelines available from authors). The project was intended for students to identify differences in health beliefs, community strengths, and potential barriers for access to health care; identify knowledge and skills necessary to foster health promotion in a culturally responsive manner; and recommend health promotion strategies for providing culturally responsive care. A written report about the presentation also was required.
Table 2.
Selected Sociocultural Groups for Team Projects
To assess the effectiveness of the course in increasing cultural competency in students, a precourse and postcourse survey instrument was administered called the Inventory for Assessing the Process of Cultural Competence among Healthcare Professionals (IAPCC-R). The IAPCC-R is a 25-item survey instrument that measures the 5 constructs of Campinha-Bacote's model of cultural competency, including cultural awareness, cultural knowledge, cultural skill, cultural encounter, and cultural desire.11 This instrument has been previously shown to be reliable and valid in assessing the process of cultural competency.11 The IAPCC-R was administered to students during the first and final weeks of the course. The results of the IAPCC-R provided students with self-reflection on their level of cultural competency at the beginning and conclusion of the course. The SIUE Institutional Review Board granted exempt status for administration of the IAPCC-R survey as a research tool and for the course evaluation. Administering the IAPCC-R as a precourse and postcourse survey instrument provided data for assessing the impact of the course on the 5 constructs of cultural competency.
EVALUATION AND ASSESSMENT
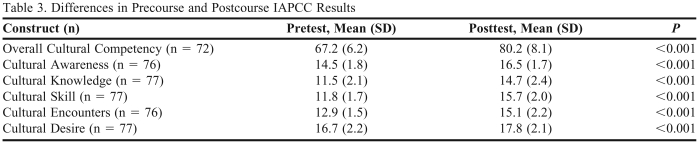
The course was evaluated by assessing the achievement of course objectives. The first objective was to develop overall cultural competency. Development of overall cultural competency was assessed by comparing the precourse and postcourse IAPCC-R scores. The results of the precourse-postcourse IAPCC-R are given in Table 3. The precourse overall cultural competency mean score of 67.2 ± 6.2 indicated that students were culturally aware (see Table 3 for the level of cultural competency ratings).10 Upon completing the course, the overall cultural competency score of 80.2 ± 8.1 indicated that students had achieved cultural competency.10 For each of the 5 constructs of Campinha-Bacote's model of cultural competency, significant improvements in mean scores were noted between precourse and postcourse scores (Table 3). The second course objective was to enhance students' self-awareness of biases. An end-of-semester course evaluation was administered. Results are noted in Table 4. The mean (SD) for the question, “The course enhanced my awareness of my own biases toward people who are different than me,” was 4.6 (1.0) on a scale where 1 = strongly disagree and 6 = strongly agree. Additionally, scores on the “cultural awareness” construct of the IAPCC-R improved significantly (p < 0.001) from a pretest score of 14.5 ± 1.8 to a posttest score of 16.5 ± 1.7 (Table 3).
Table 3.
Differences in Precourse and Postcourse IAPCC Results
Abbreviations: IAPCC = Inventory for Assessing the Process of Cultural Competence among Healthcare Professionals
Note: (a) The response options are different for each of the 25 items on the IAPCC-R.9 (b) Levels of Cultural Competency for Overall scores on the IAPCC-R (Possible range 25-100): Culturally Proficient 91-100; Culturally Competent 75-90; Culturally Aware 51-74; Culturally Incompetent 25-50. (c) Possible Range for all Constructs: Cultural Awareness, Cultural Knowledge, Cultural Skill, Cultural Encounters, and Cultural Desire is 5-20
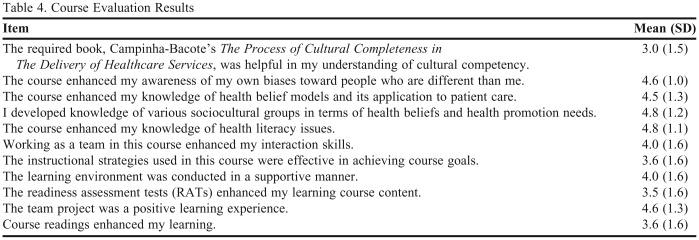
Table 4.
Course Evaluation Results
Note: Responses were obtained on the following scale 1 = strongly disagree, 2 = disagree, 3 = slightly disagree, 4 = slightly agree, 5 = agree, 6 = strongly agree
The course evaluation results presented in Table 4 indicate that the course enhanced knowledge of health belief models (4.5 ± 1.3), developed knowledge of various sociocultural groups in terms of health beliefs and health promotion needs (4.8 ± 1.2), and enhanced students' knowledge of health literacy issues (4.8 ± 1.1). Furthermore, the scores on the cultural knowledge construct also improved significantly in the IAPCC-R (p < 0.001) from a pretest score of 11.5 ± 2.1 to a posttest score of 14.7 ± 2.4 (Table 3).
Students indicated that the team project was a positive learning experience (4.6 ± 1.3) during the course evaluation at the end of the semester (Table 4). Also, the scores on the cultural skill and cultural encounters constructs in the IAPCC-R improved significantly from pretest to posttest (Table 3).
The mean response to the item regarding the helpfulness of the required textbook in understanding the process of cultural competency was (3.0 ± 1.5; Table 4). Changing the required textbook was one of the most common recommendations provided by the students to help improve the course.
Students perceived the use of specific instructional strategies in the course like readiness assessment tests (RATs), and the readings with somewhat of a neutral attitude. Twenty-three percent of students (11 out of 47) stated that the content could have been covered effectively in a smaller credit-hour course, for example, a 2-credit course versus the existing 3-credit course.
DISCUSSION
The design of the course achieved results in developing cultural competency. However, IAPCC-R scores showed that students did not achieve cultural proficiency.11 Campinha-Bacote affirms that the development of cultural competency is a journey that continues with students interacting with patients from culturally diverse backgrounds. Students agreed that the course improved their self awareness of their biases and also perceived that it improved their cultural awareness. This suggests that students agreed that the second course objective was achieved. Addressing cultural knowledge, such as differences in health beliefs among various sociocultural groups and health disparities, was the third objective. As stated earlier, the group project was implemented so students could identify differences in health beliefs, community strengths, and potential barriers for access to health care; identify knowledge and skills necessary to foster health promotion in a culturally responsive manner; and recommend health promotion strategies for providing culturally responsive care. Therefore, evidence was obtained that the third course objective was addressed. The fourth course objective was to develop skills, including health-promotion strategies, for providing culturally responsive care. The group projects along with the summative team projects were aimed to address this objective and were structured to simulate a cultural encounter and foster health promotion in a culturally responsive manner. The summative team projects addressed differences between various sociocultural groups; however, the students' reflections affirmed that there may be more diversity within a specific group than between groups. The knowledge gained from the health literacy cluster also helped for recommending appropriate health promotion strategies for providing culturally responsive care. Based on the positive comments obtained for the summative team projects and the improvement in scores for cultural skill and cultural encounters constructs, there is evidence that this fourth course objective was addressed.
The textbook was not well received by the students. This is evidenced by the open-ended comments regarding Campinha-Bacote's The Process of Cultural Competence in the Delivery of Healthcare Services, published by Transcultural C.A.R.E. Associates.11 This book focused on the process of development of cultural competency as a journey. It does not relate the concepts to the practice of pharmacy and does not address health care differences among various cultural groups. Halbur's Essentials of Cultural Competence in Pharmacy Practice, published by the American Pharmacists Association was used as the required textbook during the second offering of this course.2 The Halbur book applies the concepts of cultural competency to the practice of pharmacy, and could be useful as a resource for differences among various cultures after students graduate.
The second offering of the course has involved numerous changes to enhance the course. These include incorporation of additional applications to pharmacy practice. The use of common Spanish words and phrases to help communicate with Spanish-speaking patients has also been incorporated because of the projected population growth of Hispanics in the United States. A role-playing exercise that simulated a pharmacist and Spanish-speaking patient interaction has been included. Some students commented that they wanted representatives of various cultural groups to participate in question and answer sessions. To address this request, a Gay-Lesbian-Bisexual-Transgender (GLBT) panel was included to help students learn more about this sociocultural group and help address common stereotypes and biases. For their group presentations, students were encouraged to have a representative from their sociocultural group join them to share their stories. If students were not able to find a suitable representative, course faculty members were often able to connect them with one since many faculty members had contacts through previous courses or clinical settings. Students also were asked to relate their sociocultural team presentations to pharmacy practice by designing a pharmacy-patient case. Additional content on health disparities including financial concerns also have been included.
The instructional techniques such as the RATs and readings received a neutral response from the students. Part of the reason for this somewhat ambivalent attitude is that this course was not conducted as a traditional lecture course. Some students did not like the RATs that assessed whether the students had completed the course readings. This may be partly due to the idea that students had to complete the course readings prior to class and often felt that they needed to focus on specific details in the readings as opposed to a general understanding. The course evaluation did not specifically include a question asking about the effectiveness of the reflective portfolios. A question of this nature will be included in the future to help gauge the usefulness of the reflective portfolio. Also, more clearly defined rubrics for evaluating the written reflections will be developed. While a minority of the students suggested reducing the credit hours for the course, there are no plans to implement such a change immediately, however, it may be considered in the future.
SUMMARY
A required cultural competency course utilizing a team-based learning strategy enhanced cultural competency in pharmacy students. Development and implementation of a cultural competency course presents challenges to faculty members in terms of developing appropriate in-class activities applicable to a non-scientific topic. Some students may not understand or value the course as the nature of the content is outside of students' normal comfort zones and can be met with disinterest or ambivalence as stated in some of the open-ended comments on the course evaluations. Although some students approached the course apprehensively at the onset, when the course was completed, students appreciated many aspects. Students became more aware of their personal biases, believed that their knowledge of health-belief models and their application to patient care was enhanced, and believed that their knowledge of several sociocultural groups as well as health literacy issues improved as a result of the course.
Evidence supporting enhanced cultural competency after completing the course reaffirms the value of the course in moving them forward in their journey toward cultural proficiency.
Appendix 1. Reflective Portfolio Questions
Cluster l – Creating Desire for Cultural Competency
1. What is the value of developing cultural competency?
2. What cultural group do you desire to learn more about in terms of health beliefs? Why?
3. In what ways do you think you could help to decrease health disparities?
4. Based on your self-assessment score on the IAPCC-R survey, what did you learn about your level of cultural competency?
5. What do you perceive will be the challenges with learning to work with your group as an effective team?
Cluster 2 – Process of Cultural Competency in the Delivery of Healthcare Services
6. What was a key concept (s) you learned about the process of cultural competency?
7. What experiences have you had learning with people from different sociocultural groups than yourself?
8. Explain what was satisfying and what was discouraging about these experiences?
9. What personal qualities do you have that will help you establish interpersonal relations with persons from other cultures?
Cluster 3 – Cultural Awareness
10. How have your health beliefs influenced your understanding and acceptance of others?
11. Provide an example where you witnessed an individual being stereotyped. Explain the harmful effects that resulted.
12. How might working in a diverse environment challenge your beliefs and values?
Cluster 4 – Cultural Knowledge: health beliefs
13. What was one of the key concept(s) you learned about different health beliefs among various cultural groups?
14. Select a health belief that is contrary to your own and explain how this will change your communication methods?
15. JB Taylor is a 45-year-old African American man who is in your pharmacy to pick up a new asthma medication for his 8-year-old daughter. You know that JB Taylor has not filled his own prescription for Toprol XL 100mg in over six months. He had filled it twice in three months previous to that. How would you approach this subject with JB Taylor? Include in your response any variables from the Health Belief Model that you could address with JB Taylor.
16. Ramona Conseulo is a 62-year-old Hispanic woman. She is in your pharmacy today to fill a prescription for Augmentin from her dentist. You notice that Ramona has not filled her insulin or metformin prescriptions for 3 months. When you ask her about this, she states that she has stopped using anything but what her herbalist recommends. Romana appears to have lost weight (10-20 lbs) since you saw her last. How do you approach this subject with Ramona? Include in your response any variables from the Theory of Planned Behavior that you might address with Ramona.
Cluster 5 – Cultural Skills: communicating
17. Assuming that you accept the premise that all behavior is rooted in relationships, explain how understanding this concept will help you provide better care to patients.
18. What connections do you see between interpersonal communication and intercultural communication?
19. How could understanding the patterns of communication in your family of origin help you to be a better pharmacist?
Cluster 6 – Knowledge and Skills: literacy
20. As a practicing pharmacist, how will this awareness of the issues related to health literacy affect your interaction with patients?
21. You learned about several instruments used to test for health literacy in order to identify low literacy patients. Which instrument would you prefer to use and why? What specific questions related to pharmacy would you add to one or more of those instruments?
22. Discuss the comprehension deficit findings of your homework assignment and possible revisions of your selected patient education material.
Cluster 7 – Cultural Encounter
23. As cultural competency is a journey, what do you plan to do in order to further develop your competency?
24. How effective did your team work together?
25. How was conflict among the team resolved?
26. How did the team build on individual's member strengths for accomplishing the team project?
REFERENCES
- 1.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–534. [PubMed] [Google Scholar]
- 2.Vess Halbur K, Halbur DA. Washington, DC: The American Pharmacists Association; 2008. Essential of cultural competence in pharmacy practice. [Google Scholar]
- 3.Shaya FT, Gbarayor CM. The case for cultural competence in health professions Education. Am J Pharm Educ. 2006;70(6) doi: 10.5688/aj7006124. Article 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soller RW. An integrated approach to teaching health literacy in the clinical pharmacy curriculum. J Pharm Teach. 2006;13(1):17–28. [Google Scholar]
- 5.Onyoni EM, Ives TJ. Assessing implementation of cultural competency content in the curricula of colleges of pharmacy in the United States and Canada. Am J Pharm Educ. 2007;71(2) doi: 10.5688/aj710224. Article 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Assemi M, Cullander C, Hudmon KS. Implementation and evaluation of cultural competency training for pharmacy students. Ann Pharmacother. 2004;38:781–786. doi: 10.1345/aph.1D402. [DOI] [PubMed] [Google Scholar]
- 7.Brown B, Heaton P, Wall A. A service-learning elective to promote enhanced Understanding of civic, cultural, and social issues and health disparities in pharmacy. Am J Pharm Educ. 2007;71(1) doi: 10.5688/aj710109. Article 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westberg SM, Bumgardner MA, Lind PR. Enhancing cultural competency in a college of pharmacy curriculum. Am J Pharm Educ. 2005;69(5) Article 82. [Google Scholar]
- 9.Evans E. An elective course in cultural competence for healthcare professionals. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700355. Article 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michaelsen LK, Knight AB, Fink LD. Sterling, VA: Stylus Publishing; 2004. Team-based learning. [Google Scholar]
- 11.Campinha-Bacote J. The Process of Cultural Competence in the Delivery of Healthcare Services. 5th Ed. Cleveland, OH: Transcultural C.A.RE. Associates; 2007. [DOI] [PubMed] [Google Scholar]
- 12.Mutha S, Allen C, Welch M. Toward Culturally Competent Care: A Toolbox For Teaching Communication Strategies. San Francisco: Center for the Health Professions, University of California; 2002. [Google Scholar]
- 13.Kane M. New York (NY): HBO Home Video; 2000. producer. If These Walls Could Talk 2. [CD-ROM]. Heche A, Director. [Google Scholar]
- 14.Plake KS. Behavior Change. In: Richardson M, Chant C, Cheng JWM, Chessman KH, Hume AL, Hutchinson LC, et al., editors. Pharmacotherapy Self-Assessment Program 6th ed. Health Promotion and Maintenance. Lenexa, KS: American College of Clinical Pharmacy; 2008. pp. 1–13. [Google Scholar]
- 15.Brown CM, Segal R. Ethnic differences in temporal orientation and its implications for hypertension management. J Health Soc Behav. 1996;37:350–361. [PubMed] [Google Scholar]
- 16.Berlin EA, Fowkes WC. Teaching framework for cross-cultural care: application in family practice. West J Med. 1983;139(6):934–938. [PMC free article] [PubMed] [Google Scholar]
- 17.Zollo F. New York: HBO Home Video; 1997. producer. In the Gloaming. [videocassette]. Reeve C, director. [Google Scholar]
- 18.Weiss BD. 2nd edition. Chicago: AMA Foundation; 2007. Health Literacy and Patient Safety: Help Patients Understand. [CD-ROM] [Google Scholar]