Abstract
Objectives
To compare 2006-2007 and projected 2010-2011 advanced pharmacy practice experience (APPE) availability and needs for 4 colleges and schools of pharmacy in Georgia and Alabama and to examine barriers and offer potential solutions to increase APPE site and preceptor availability.
Methods
Data on APPE needs and availability were gathered prospectively and evaluated relative to current and projected enrollment and planned programmatic changes.
Results
Combined 2006-2007 non-community APPE needs and availabilities were 3,590 and 4,427, respectively, with a surplus availability of 837. Combined projected 2010-2011 non-community APPEs were estimated at 4,309. Assuming 2006-2007 non-community availability remained unchanged, the surplus availability declined to 118.
Conclusions
The need for quality experiential education represents a significant barrier and rate-limiting step to the matriculation of the increased numbers of pharmacists. Barriers to expanding APPE availability include: introductory pharmacy practice experience (IPPE) and APPE expansion, growth of new and existing pharmacy programs, financial instability of acute care facilities, and lack of preceptor development resources. Regional experiential education consortiums can provide a constructive approach to improve access to quality sites and preceptors through standardizing processes and leveraging resources.
Keywords: consortium, practice experience, pharmacist shortage, preceptors, advanced pharmacy practice experience, introductory pharmacy practice experience
INTRODUCTION
Many factors have converged over the past several years, resulting in an increasingly difficult environment for identifying, developing, and retaining high-quality APPE sites and preceptors for doctor of pharmacy (PharmD) degree programs.1-3 Since 1998, the United States has been in the midst of a pharmacist shortage.4-6 Although there are current data to suggest the shortage is not as severe as once thought, there is an unmet need for pharmacists in most states.4,6,7 As a result of the current nationwide shortage and predictions of increased future need of pharmacists, there has been rising pressure to expand the number of pharmacy graduates.8,9 This has been achieved by both creating new programs and expanding existing schools and colleges of pharmacy. However, these efforts have also intensified the nationwide shortage of qualified pharmacy faculty members.10
There were 100 accredited schools and colleges of pharmacy in the United States as of January 2008. An additional 6 programs had been granted pre-candidate status.11 Between 2002 and 2007, the number of pharmacy students enrolled in first professional doctor of pharmacy degree programs increased 30.3%, from 38,902 to 50,691. Within this same time period, the number of first professional PharmD degrees conferred rose 59.3%, from 6,158 to 9,812.12 Regional statistics for Georgia and Alabama illustrated similar trends. Between 2002 and 2007, combined pharmacy student enrollment in these 2 states climbed 31.6% (1764 students to 2322 students) and first professional PharmD degrees conferred rose 48.8% (375 to 558).12
Additional pressures on APPE availability resulted from the adoption of the revised ACPE accreditation standards and guidelines for the PharmD degree, also known as Standards 2007.13 These standards require that APPEs comprise a minimum of 25% of the curriculum and be at least 1440 hours in length. They also mandate that IPPEs comprise a minimum of 5% of the curriculum for a minimum of 300 hours. In an effort to comply with the accreditation standards, several institutions have added additional hours of APPE and IPPE instruction to their curriculum, thereby increasing competition for already limited sites and preceptors.
Within Georgia and Alabama, the schools and colleges of pharmacy united to form the Southeastern Pharmacy Experiential Education Consortium (SPEEC) as a means to cooperatively address experiential issues.14 Similar to other US PharmD programs, the experiential programs associated with SPEEC institutions rely heavily on volunteer faculty members to teach the majority of APPEs.15 In addition to the pharmacist shortage affecting our states, challenges exist due to the rural nature of the region. A majority of the counties in Georgia and Alabama are designated as either “medically underserved” areas or “health professional shortage areas,” which compounds the difficulty in securing student training sites in both acute care and interdisciplinary environments.16,17
As of 2008, there were 303 licensed hospitals in Georgia and Alabama.18,19 Similar to hospitals nationwide, these facilities frequently face financial difficulties.20,21 In a nationwide analysis of over 4500 hospitals, more than half were deemed either insolvent or at risk of insolvency.22 As these financially challenged facilities mandate staffing reductions, schools and colleges of pharmacy that are heavily dependent on volunteer faculty members could experience a profound impact on experiential training availability and quality, eventually leading to a decline in graduation rates.
In this project, 2006-2007 APPE availability and needs for 4 SPEEC-affiliated institutions in Georgia and Alabama were prospectively compared. Needs for 2010-2011 were also forecasted, based on known factors such as expanding student enrollments of existing programs, creation of new regional colleges or schools of pharmacy, and planned programmatic changes designed to meet new accreditation standards. In addition, specific barriers to expanding APPE availability were identified and potential solutions offered.
METHODS
Participating SPEEC institutions included: Auburn University Harrison School of Pharmacy, Mercer University College of Pharmacy and Health Sciences, South University School of Pharmacy, and The University of Georgia College of Pharmacy. Institutional specific APPE availability data for the 2006-2007 academic year were extracted from the Experiential Education Management Systems software and databases (EXP-EMS) in February 2006 and included the following: APPE class size for the 2006-2007 academic year; number of community-based APPEs needed per class; number of non-community-based APPEs needed per class; total community-based APPE availability; total non-community based APPE availability.
Projected needs for the 2010-2011 APPE year were made by the experiential director at each SPEEC institution based upon their knowledge of anticipated changes in class size or professional program (eg, opening additional campuses and adding additional required APPEs to meet Standards 2007.) Information was also gathered from SPEEC and non-SPEEC (actual and proposed) institutions within the southeastern United States to determine their APPE “footprint” for student placement. An overlay of these diagrams was subsequently used to identify key cities where multiple colleges/schools already had established APPE sites.
Normalization of APPE availability was not attempted as assignment length at APPE sites varied from 4 to 5 weeks. Instead, availability was presented only in terms of institutional need, regardless of APPE length. Similarly, types of non-community APPEs (eg, acute care, outpatient, or elective) could not be further delineated due to lack of standardization in school requirements and/or APPE definitions among institutions. All actual and projected needs were multiplied by 115% to determine the total APPEs needed. This overage calculation was based on studies suggesting a 12.5% to 14.8% reassignment rate for APPEs.23
In order to ascertain the potential capacity of APPE sites and preceptors in Georgia and Alabama in 2006, the following data were compiled from state hospital associations and boards of pharmacy: number of licensed pharmacists; number of licensed pharmacist preceptors (applicable only for Alabama); number of licensed hospitals; and number of licensed hospital beds.
RESULTS
For the 2006-2007 academic year, the total APPE need for Alabama and Georgia was 4,133 and the total APPE availability was 6,662 (an excess availability of 2,529 APPEs). When community APPEs were excluded, total needs decreased 13.1% to 3,590 while total availability fell 33.5% to 4,427 (an excess availability of 837). Thus, the surplus of community APPE availability accounted for 67% of the excess APPE availability.
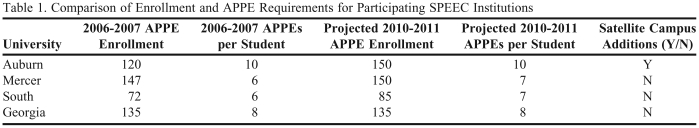
For the 2010-2011 year, APPE needs were projected to be 4,859 experiences. As illustrated in Table 1, these increases were secondary to either higher anticipated enrollment (3 institutions) or additional APPE course requirements (2 institutions). The latter programmatic change was predicted in response to proposed accreditation revisions.13 Assuming that total availability from 2006-2007 remained unchanged at 6,662, an overall excess of 1803 APPEs was calculated for 2010-2011. If community APPE needs and availabilities were removed from consideration, total needs dropped 11.3% to 4,309. When comparing 2010-2011 non-community APPE needs to the 2006-2007 non-community APPE availability of 4427, total excess of non-community APPEs was reduced to 118.
Table 1.
Comparison of Enrollment and APPE Requirements for Participating SPEEC Institutions
Abbreviations: APPE = advanced pharmacy practice experience
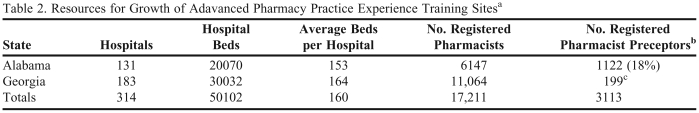
In evaluating the regional overlap for student placement of SPEEC and non-SPEEC institutions within the southeastern United States, 8 cities emerged as areas with the highest potential for site competition among college/schools of pharmacy. These cities were: Atlanta, Augusta, Birmingham, Chattanooga, Columbus, Huntsville, Knoxville, Nashville, and Savannah. Georgia had at least a one-third greater hospital capacity than Alabama in terms of absolute numbers of facilities and hospital beds (Table 2). Furthermore, Georgia had 80% more pharmacists than Alabama. Because Alabama requires registration of preceptors with the Alabama Board of Pharmacy, it was determined that 18% of licensed Alabama pharmacists were registered as preceptors.
Table 2.
Resources for Growth of Adavanced Pharmacy Practice Experience Training Sitesa
References 24-27
b Alabama Board of Pharmacy requires specific licensure for preceptors
c Estimate based on using similar proportion for preceptors in Georgia as in Alabama (18%)
DISCUSSION
Although initial evaluation of the results suggests that the institutions examined should have minimal difficulty in placing students on APPEs through the 2010-2011 academic year, when community-based APPEs are removed from the equation, a more realistic picture of APPE availability appears. In actuality, each institution has noted increasing difficulties securing adequate numbers of quality APPE sites and preceptors for their PharmD students. These differences between perception and reality underscore the limitation in simply counting numbers to evaluate the status of a complex system. The tally of availability does not accurately represent the true ability to place students in APPE s.
APPE availability must be considered within the context of type, preceptor, site, quality, location, and timing. Additionally, the impact of outside institutions must be taken into account. Although not readily apparent, the grouping of non-community APPE s, rather than subdividing them into required and elective experiences, actually overestimates the true number of APPE s available when scheduling and rescheduling students. This non-community aggregate group includes the following APPE types: general hospital, internal medicine, medicine subspecialty, primary care, home health, long-term care, and drug information, as well as elective APPE experiences in administration, academia, industry, and nuclear medicine, and experiences abroad. To fully understand the scope of the problem, additional focus must be placed on calculating needs and availability for required APPEs, such as primary care, acute care/internal medicine, and health-system practice.28 Future studies should further subdivide APPE types in order to better characterize APPE availability.
Although a 15% buffer calculation was added to the actual calculated APPE needs, this may not have been sufficient.23 In practice, once APPE schedules are distributed to preceptors, all remaining availability is often reallocated to other programs soliciting for student placement. As such, all availability remaining after the schedule is completed, is not promised to any given program. Given that over 12% of rescheduling is due to factors other than student requests, this practice creates a huge administrative burden for experiential faculty and staff members to locate replacement APPEs that satisfy the curricular needs of individual students.23
Barriers to Expanding APPE Availability
A variety of barriers exist with regards to expanding APPE availability. These include escalation of student numbers through new and existing programs, static or reduced hospital availabilities secondary to financial pressures, high dependence on volunteer faculty members to precept students, competition from regional IPPE placements, and scarcity of tangible and intangible resources necessary for adequate preceptor development.
Although this study only examines the impact of APPE needs and availabilities relative to the 4 participating programs, there are many more schools in the Southeast that play a role in determining future regional availability. Expansion campuses and new schools in Georgia, Tennessee, South Carolina, Florida, Kentucky, and Virginia will add to the competition for sites and may soon dramatically impact APPE availability utilized by SPEEC-affiliated institutions. Between 2006 and 2008, the following pharmacy college/school additions have occurred in Georgia, Alabama, or their adjoining states: 1 new school/college admitted its first class, 2 schools/colleges opened satellite campuses, and 3 schools/colleges applied for (or have been granted) precandidate status. Two additional colleges/schools are actively recruiting deans in order to begin the process of school development and eventual application for precandidate status. While the full impact will not be realized until all of the students matriculate into APPEs, it is expected to be significant. These new programs more than likely will target both IPPE and APPE placement within the identified key areas used by the SPEEC-affiliated institutions, including Atlanta, Augusta, Birmingham, Chattanooga, Columbus, Huntsville, Knoxville, Nashville, and Savannah.
Institutional sites and clinics represent the greatest need for required APPEs.23 Given the economic crisis facing the majority of healthcare systems, the number of hospitals or hospital beds probably will not increase significantly in the short term.20-22 Therefore, most new acute care APPEs must be developed at existing sites. Between 2006 and 2008, the number of hospital facilities within Alabama and Georgia actually declined from 314 to 303.18,19,26,27 Although some of this decrease may have been the result of hospital consolidation, it is likely that some facilities have closed. In addition, within individual hospitals, there are limited capacities for integrating students in advanced clinical APPEs since only a fraction of employed pharmacists have the required skills, training, and established practice sites needed for student training. Even with small increases in staffing, the capacity would not change substantially in most cases. For these reasons, no increase in non-community APPE availability was projected between academic year 2006-2007 and academic year 2010-2011.
When examining the potential for recruiting new preceptors, the assumption that a majority of all licensed pharmacists within a given state would be willing and able to serve as APPE or IPPE preceptors is tempting. However, with the ongoing pharmacist shortage, some practitioners may not feel capable of precepting students because of lack of time or educational background. Other pharmacists may feel that it is not their responsibility to offer practice experiences or that their practice is not conducive to education.29,30 Lastly, there may be a geographical mismatch with willing preceptors located in sites not readily accessible to students. Alabama's requirement for preceptors to hold a separate license in order to sign for experiential training hours allowed for a true assessment of the percentage of licensed Alabama pharmacists who were active preceptors. Surprisingly, this was only 18%. This percentage not only demonstrates how misleading it is to simply count the number of registered pharmacists when estimating the availability of future preceptors, but also illustrates how difficult it is to find a solution to the preceptor shortage when a large proportion of practicing pharmacists do not participate in training the next generation in our profession.3,28,30,31 To compound the situation, the majority of APPEs nationwide are taught by volunteer faculty members.15 For the 4 participating institutions within this study, the proportion of APPEs taught by volunteer faculty members ranged from 68% to 91%.
To meet the needs of expanding pharmacy education endeavors, new preceptors and sites must be developed to ensure adequate quantity and quality of experiences. Experiential education directors define attracting, developing, and retaining qualified preceptors as the area most worrisome to them.32 Many feel they have insufficient resources (eg, time, staff, travel budget) to provide preceptor development. As a result, the AACP Preceptor Development Task Force deduced that only 30% of seasoned preceptors and less than 50% of new preceptors receive training.33 Since some administrators, even within the academy, do not fully understand the intricacies and complexities of directing an experiential program and the various factors affecting APPE availability, adequate resources may not be allotted to the identification, establishment, and ongoing development of high quality sites and preceptors.15,28
In addition to the consideration of needs for and availability of APPEs, many programs must also further develop sites, preceptors, and IPPE experiences to satisfy ACPE Standards 2007 requirements.13 This new mandate creates additional competition for already limited availability, especially given the recent expansion of pharmacy programs. A majority of programs compensate preceptors or institutions for APPEs and the market forces of increased demand for APPEs in the face of inadequate supply may drive up expectations for this compensation. This is a situation that would greatly disadvantage programs relying on limited state funding. If a “bidding war” for APPEs ensues, some programs may not survive.
Solutions for Expanding APPE Availability
Potential strategies to address many of the identified barriers have been found within a multistate or regional experiential pharmacy program consortium.14 Through alignment of expectations and administrative tasks across several schools and colleges of pharmacy, the process of experiential education can be streamlined for preceptors and sites, while obtaining more consistent desired student experiences and outcomes. Standardization of the preceptor application form, course objectives and syllabi, APPE preceptor manuals, and student orientations all help new preceptors orient rapidly to precepting for multiple institutions. Common evaluation tools for students, preceptors, and site visits further enhance consistency of outcomes for students and efficiency of preceptors. Sharing policies on attendance and a uniform APPE schedule, along with an online electronic system for student profiles, immunization verification, and evaluations among all institutions simplify many of the administrative responsibilities for preceptors. Collectively, these initiatives may give preceptors more confidence that they are indeed capable of precepting students.
Preceptor development may be achieved more efficiently within a consortium as well. Both traditional and nontraditional formats may be used effectively to reach busy preceptors, while consuming only a fraction of the resources when shared among institutions. SPEEC has developed live programs at local, state, and regional meetings on the basics of precepting and online training modules including topics such as Professionalism, Structuring the Student Experience, Motivating Students in the Clinical Arena, Achieving Synergy in Clinical Teaching, and Assessment and Evaluation. These all serve to improve the quality of existing sites and preceptors and assist in the development of new sites and preceptors with little or no background in teaching.14 In addition, these training programs provide an opportunity for sites and preceptors to learn how to integrate students more effectively into their practice while deriving significant benefit in terms of extending services or developing new services that may not otherwise be feasible.34 As a result, preceptors may better recognize their role in ensuring the future of our profession.30,31
By using a cooperative approach to scheduling within a consortium, a more accurate evaluation of APPE availability becomes possible. Sharing availability and considering the group's needs makes it more likely that each institution will meet its current and future APPE (and IPPE) needs. Collaboration and pooling of resources is vital to the successful design and implementation of the approaches already described here. The uniform policies and procedures, evaluation tools, and preceptor development programs benefit not only the sites and preceptors but also the consortium members as well in terms of overcoming the scarcity of resources allotted to experiential programs. By working together to increase the availability of APPEs, a consortium could shift the market to a more favorable balance of APPE supply and demand.
CONCLUSION
There is a growing problem in meeting the demands of experiential training for the ever-increasing numbers of pharmacy students. A simple accounting of the numbers of needed experiences versus the total possible availability of sites does not provide educators and administrators with an accurate picture of the challenges faced. The difficulty in placing all students in quality sites exists despite what appears on paper to be a surplus of available APPEs. Based on projections of future needs, the challenges facing experiential educators will only increase.
Many of the barriers contributing to these struggles are systemic and occur at a very broad level that includes problems with our nation's overall healthcare system. Nonetheless, there are several local and regional solutions that can help schools meet their needs in the short term and help them more adequately plan for the long term. In our experience, these challenges are best addressed when schools join together in regional consortia, allowing for open and honest communication and cooperation.
REFERENCES
- 1. O'Sullivan T, Hammer DP, Manolakis PG, Skelton JB, Weber SS, Dawson KN, Flynn AA. Pharmacy experiential education present and future: realizing the Janus vision. A background paper for the AACP APPI summit to advance experiential education in pharmacy. June 2005. http://courses.washington.edu/pharm560/APPI/Background_Paper.pdf Accessed April 24, 2009.
- 2.Talley CR. Experiential s for pharmacy students. Am J Health-Syst Pharm. 2006;63(11):1029. doi: 10.2146/ajhp060190. [DOI] [PubMed] [Google Scholar]
- 3.Traynor K. Experiential education requirements squeeze schools, sites. Am J Health-Syst Pharm. 2004;61(15):1537–8. doi: 10.1093/ajhp/61.15.1537. [DOI] [PubMed] [Google Scholar]
- 4.Knapp KK, Quist RY, Walton SM, Miller LM. Update on the pharmacist shortage: national and state date through 2003. Am J Health-Syst Pharm. 2005;62(5):492–499. doi: 10.1093/ajhp/62.5.492. [DOI] [PubMed] [Google Scholar]
- 5.Cooksey JA, Knapp KK, Walton SM, Cultice JM. Challenges to the pharmacist professional from escalating pharmaceutical demand. Health Aff. 2002;21(5):182–188. doi: 10.1377/hlthaff.21.5.182. [DOI] [PubMed] [Google Scholar]
- 6.Walton SM, Knapp KK, Miller LM, Schumock GT. Examination of state-level changes in the pharmacist labor market using Census data. J Am Pharm Assoc. 2007;47(3):348–357. doi: 10.1331/JAPhA.2007.06081. [DOI] [PubMed] [Google Scholar]
- 7. Pharmacy Manpower Project. Aggregate Demand Index. http://www.pharmacymanpower.com. Accessed April 24, 2009.
- 8.Cohe JL, Kabat HF, Knapp DA, Koda-Kimble MA, Rutledge CO. Pharmaceutical education and the pharmacy workforce. Should we expand our programs? Report of the AACP Argus Commission 1999-2000. Am J Pharm Educ. 2000;64(suppl):4S–7S. [Google Scholar]
- 9.Knapp DA. Professionally determined need for pharmacy services in 2020. Am J Pharm Educ. 2002;66(Suppl):421–9. [Google Scholar]
- 10.Roche VF. Tucson, Arizona: American Association of Colleges of Pharmacy; 2000. Challenges and Opportunities for schools and colleges of Pharmacy in the next decade. Paper presented at NABP/AACP Combined District 7 and 8 Meeting. [Google Scholar]
- 11. American Association of Colleges of Pharmacy. Academic pharmacy's vital statistics. http://www.aacp.org/about/Pages/Vitalstats.aspx, Accessed July 15, 2009.
- 12. American Association of Colleges of Pharmacy. Institutional trend data. http://www.aacp.org/resources/research/institutionalresearch/Pages/TrendData.aspx, Accessed July 15, 2009.
- 13. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed April 24, 2009.
- 14.Duke LJ, Unterwagner WL, Byrd DC. Establishment of a multi-state experiential pharmacy program consortium. Am J Pharm Educ. 2008;72(03) doi: 10.5688/aj720362. Article 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harralson AF. Financial, personnel, and curricular characteristics of advanced practice experience programs. Am J Pharm Educ. 2003;67(1) Article 17. [Google Scholar]
- 16. Demographic and Economic Profile: Georgia. Updated July 2006. Rural Policy Research Institute. http://www.rupri.org/Forms/Georgia.pdf Accessed April 24, 2009.
- 17. Demographic and Economic Profile: Alabama. Updated July 2006. Rural Policy Research Institute. http://www.rupri.org/Forms/Alabama.pdf Accessed April 24, 2009.
- 18. Georgia Department of Human Resources. Office of Regulatory Services. Hospital Facility Search. http://www.ors.dhr.state.ga.us May 16, 2008.
- 19. Alabama Department of Public Health. Hospital Facility Search. http://ph.state.al.us/FacilitiesDirectory Accessed April 24, 2009.
- 20. Cavendish de Moura H. Financial Crisis at Atlanta's Grady Hospital. Georgia Public Broadcasting Health Desk. 2007. http://www.gpb.org/healthdesk/financial-crisis-at-atlantas-grady-hospital Accessed April 24, 2009.
- 21. Malhotra HB. Financial crisis looms over healthcare industry. The Epoch Times. May 3, 2008. http://en.epochtimes.com/news/8-5-3/70150.html. Accessed April 24, 2009.
- 22. Alarez & Marsal Healthcare Industry Group. Hospital insolvency: the looming crisis. March 2008. http://www.alvarezandmarsal.com/en/docs/am_hospital_insolvency_survey_03.2008.pdf. Accessed April 24, 2009.
- 23.Kawahara NE, Cannon BC, Harper-Brown D, Spunt AL. Reasons Behing the Need for Senior Advanced Practice Experiences Reassignment and the Associated Workload: One Institution's Experience. Am J Pharm Educ. 1999;63(4):406–409. [Google Scholar]
- 24. Georgia Board of Pharmacy. Georgia Secretary of State. http://sos.georgia.gov/Plb/Pharmacy/ Accessed April 24, 2009.
- 25. Alabama Board of Pharmacy. State of Alabama. FAQ - licensure statistics. http://www.albop.com/ Accessed April 24, 2009.
- 26. Alabama Hospital Association. http://www.alaha.org/directory.aspx Accessed April 24, 2009.
- 27. Georgia Hospital Association. http://www.gha.org/directory.html Accessed April 24, 2009.
- 28.Plaza CM, Draugalis JR. Implications of advanced practice experience placement: a 5-year update. Am J Pharm Educ. 2005;69(3) Article 45. [Google Scholar]
- 29.Chase P. Rethinking experiential education (or does anyone want a pharmacy student?) Am J Pharm Educ. 2007;71(2) doi: 10.5688/aj710227. Article 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trovato JA, Edwards JM. Education and training of pharmacy students. Am J Health-Syst Pharm. 2004;61(18):1956–1967. doi: 10.1093/ajhp/61.18.1956. [DOI] [PubMed] [Google Scholar]
- 31.Marriott J. Tough challenge…rewarding results…be a preceptor! Aust Pharmacist. 2006;25(8):604–9. [Google Scholar]
- 32. American Association of Colleges of Pharmacy. Academic practice partnership initiative: summit to advance experiential education in pharmacy. Edition 1, June 2005. http://www.aacp.org/resources/education/APPI/Documents/SummitFinalReport.pdf Accessed July 15, 2009.
- 33.Boyle CJ, Carr-Lopez S, Kawahara NE, Kieser MA, See CJ, Smith GB. Report of the Preceptor Development Task Force Subcommittee Two. Am J Pharm Educ. 2002;66(suppl):42S–3S. [Google Scholar]
- 34.Turner CJ, Ellis S, Giles J, et al. A strategy to develop advanced pharmacy practice experiences. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710346. Article 46. [DOI] [PMC free article] [PubMed] [Google Scholar]