Abstract
Objectives
To compare the effectiveness of small-group training in correct inhaler technique with self-directed Internet-based training.
Design
Pharmacy students were randomly allocated to 1 of 2 groups: small-group training (n = 123) or self-directed Internet-based training (n = 113). Prior to intervention delivery, all participants were given a placebo Turbuhaler and product information leaflet and received inhaler technique training based on their group. Technique was assessed following training and predictors of correct inhaler technique were examined.
Assessment
There was a significant improvement in the number of participants demonstrating correct technique in both groups (small group training, 12% to 63%; p < 0.05; and Internet-based training, 9% to 59%; p < 0.05) post intervention, with no significant difference between the groups in the percent change (n = 234, p > 0.05). Increased student confidence following the intervention was a predictor for correct inhaler technique.
Conclusions
Self-directed Internet-based training is as effective as small-group training in improving students' inhaler technique.
Keywords: dry powder inhaler, Turbuhaler, asthma, Internet-based training
INTRODUCTION
Asthma medications are primarily administered via inhalation and delivered directly to the site of action and thereby have greater efficacy with fewer systemic adverse effects.1 However, they are administered through an inhaler device, which adds another dimension to medication regimens as appropriate use of these medications is not only dependant on the optimal medication being prescribed but also on appropriate device administration being practiced.
There are many inhaler devices currently on the Australian and international markets. The most commonly used devices are metered dose inhalers (MDIs), which deliver a measured amount of medication as a mist the patient can inhale. They consist of a pressurized canister of medication in a case with a mouthpiece, commonly used for reliever therapy. Dry powder inhalers (DPIs, eg, the Turbuhaler) are similar to MDIs, but the medication is in powder form, rather than in liquid form, and it is breath activated. These are commonly used for preventer therapy. A high rate of incorrect technique has been reported worldwide (20%-68%) for both MDIs and DPIs.2-7
The implications of incorrect inhaler technique are striking. With the annual cost of asthma medications estimated at about $374 million,1 there are huge economic implications associated with their incorrect use. There are also important clinical ramifications associated with incorrect inhaler use, such as inadequate dose delivery or faulty dispersion of medication in the airways, resulting in suboptimal medication dosing.8
Simple training interventions significantly improve patients' inhaler technique,9-12 thus it is important that pharmacists are aware of the issues associated with inhaler use and are appropriately and adequately trained to deal with them.
Pharmacists obtain inhaler technique training from various sources, such as package inserts and training from pharmaceutical representatives.10,13,14 However, for many pharmacists, their first inhaler educational experience is in pharmacy school,15 possibly suggesting that this is the place where their preliminary knowledge is obtained. Students should therefore be able to demonstrate correct inhaler technique in order to train others. Effective training starts with their initial exposure to inhaler devices in pharmacy school.
At the University of Sydney, Pharmacy Practice 2 is a unit of study delivered in the second year of the bachelor of pharmacy curriculum. The key focus is to enable students to acquire knowledge regarding the therapeutic management of common disease states, and develop and utilize appropriate communication skills and written resources such as Consumer Medicine Information in the provision of drug and disease information to patients. The specific course objectives are associated with therapeutics and communication. However, those objectives within which inhaler device training lies are to “….Apply their knowledge to solve consequential problems in the therapeutic areas of …Respiratory Medicine and …..Communicate their knowledge confidently and effectively..” (A list of objectives is available from the author). In line with these course objectives, students are trained how to appropriately use inhaler devices through physical demonstrations and hands-on practice in small-group workshops.
Though small-group education is effective in this context, it is time consuming. Given the amount of information that needs to be covered in workshops and the trend toward self-directed, more flexible learning methods in higher education, more efficient yet effective methods of inhaler technique training need to be investigated and evaluated. In particular, the use of technology in this area of vocational training needs to be considered. In order to determine the impact of using technology in the training of pharmacy students, this study compared the proportion of pharmacy students able to demonstrate correct inhaler technique following small-group training to that number following self-directed Internet-based training. Also, to better understand ways in which inhaler technique training could be made more effective in the future, predictors of inhaler technique post-training were determined. The most effective and efficient method of training inhaler technique to students was identified and recommended to Pharmacy Practice 2, Respiratory Workshops.
DESIGN
This was a repeated measures parallel group design study and was approved by the University of Sydney Human Research Ethics Committee. It was conducted during the respiratory tutorial classes and included all students enrolled in Pharmacy Practice 2, in the second year of the University of Sydney BPharm curriculum. Within this unit of study, students were divided into 10 groups. Each student attended 1 Pharmacy Practice 2 workshop per week for 12 weeks. Over this 12-week period, workshops were conducted in respiratory health, cardiovascular disease (hypertension, ischaemic heart disease, and cardiac failure), endocrinology (diabetes and thyroid disorders), and infectious diseases, and in the areas of communication, barriers to communication, counselling, and patient perspectives to illness. Each tutorial was facilitated by 1 tutor and lasted for 1½ hours. Workshops were spread out through the week and no 2 were held simultaneously. Workshops included case-based, problem-based learning approaches as well as appropriate hands-on and small group activities. Students enrolled in Pharmacy Practice 2 were evaluated through an end-of-semester oral assessment, multiple-choice and written examinations, and throughout semester tutorial participation. Criteria for evaluation were articulated in the Pharmacy Practice Unit of Study Outline, 2008. Logistical issues, such as the required tutorial rooms to conduct the study, computers for the Internet-based part of the intervention, were all addressed prior to study commencement. Inhaler placebos were also made available by AstraZeneca (New South Wales, Australia).
In the fourth week of the semester, following completion of the respiratory lecture material delivery, all students in the second year of the program were invited to participate in the study and asked to sign an informed consent form. Based on 10 predetermined tutorial groups, the researchers randomly allocated 5 groups to group A and 5 to group B.
At the start of the training tutorial, each participant in both groups was given a placebo inhaler device, Turbuhaler, and an information leaflet explaining the use of the device (package insert product information). Each participant was given 10 minutes to practice using the inhaler, referring only to the written resources provided. Participants were not instructed on how or what to do with the placebo device, nor how to use the written information provided. Participants utilized their own learning techniques.
Baseline Assessment
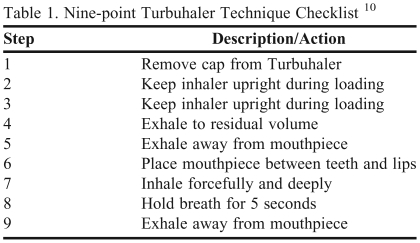
After 10 minutes of self-training, all participants had their inhaler technique assessed by one of 3 assessors who had previously undergone assessor training. All 3 assessors evaluated the inhaler technique of the first participant in each tutorial group and provided feedback to ensure consistency of assessment. From then on, the inhaler technique of each participant was evaluated by 1 assessor only. Assessments were based on a 9-step checklist (Table 1).10 Correct inhaler technique corresponded to a score of 9/9. Demographic data and other characteristics (Turbuhaler use history and level of confidence in demonstrating Turbuhaler technique) were also collected at this point.
Table 1.
Nine-point Turbuhaler Technique Checklist 10
Participants were awarded 1 point for each step they performed correctly, giving them a score out of 9 for Turbuhaler technique. Correct technique = 9/9.
Interventions
Following baseline assessment, participants returned to their assigned tutorial group, in which the intervention took place.
Small Group Workshop.
Group A intervention was 15 minutes in duration and consisted of 2 parts. First, the entire tutorial group received inhaler technique training by watching a step-by-step demonstration by an asthma doctor. Second, the participants worked in pairs and took turns teaching and assessing each other on correct inhaler technique using the 9-step checklist.
Internet-based Tutorial.
Group B intervention was 15 minutes in duration. Participants were assigned to a computer and given the opportunity to work through the tutorial individually. The Internet-based tutorial shows a pharmacist demonstrating the correct use of the inhaler; a checklist of steps for inhaler use that allowed students to practice each step with the placebo inhaler; and an activity requiring students to observe and assess a patient using an inhaler and identify any steps performed incorrectly using the checklist. The Internet-based tutorial allowed students to review any part as often as required.
Immediately following delivery of the intervention to both groups, participants had their inhaler technique assessed by the same researcher who had performed the baseline assessment. Participants were asked to demonstrate the correct use of an inhaler using the placebo device and were assessed using the 9-step checklist.10
EVALAUATION AND ASSESSMENT
Data Analysis
Demographic data, including gender, age, inhaler use history, and confidence in use, were analyzed descriptively. Comparisons between groups were made using chi-square analysis. In order to compare the impact of the intervention between the groups, 2 forms of analysis were performed. To determine the difference in proportion of participants demonstrating correct technique, a chi-square analysis was performed. For comparisons of the change in mean Turbuhaler scores (out of 9), repeated measures general linear analysis was used.
In order to determine predictors of correct inhaler technique following delivery of inhaler technique education, a logistic regression analysis was performed. The dependent variable was correct technique following intervention (score 9/9) and the independent variables were intervention group (group A or group B), technique at baseline (correct or incorrect), gender (male or female), age, previous pharmacy experience (yes or no), previous inhaler use (yes or no), confident to use inhaler before intervention (yes or no) and confident to use inhaler after education (yes or no). Results were considered significant at p ≤ 0.05 and a power of 0.8. All data relating to Turbuhaler scores was normally distributed.
Data Findings
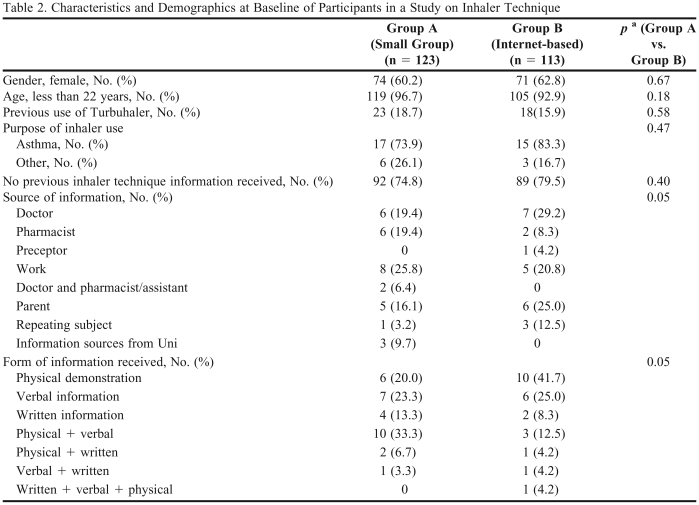
All 236 second-year pharmacy students invited to participate in the study agreed to do so (group A, n=123; group B, n=113). Analysis of participant demographics indicated that there was no significant difference between participants in group A compared with group B (Table 2).
Table 2.
Characteristics and Demographics at Baseline of Participants in a Study on Inhaler Technique
achi-square test
At baseline, there was no significant difference in the proportion of participants with correct Turbuhaler technique in group A compared to group B (12% and 9%, respectively; p = 0.40). Both methods of training inhaler technique within the respiratory workshops of Pharmacy Practice 2 were found to be feasible.
Following delivery of the intervention, there was a significant increase in the proportion of participants with correct inhaler technique for group A (12% vs. 63% respectively; n=123, p = 0.04) as well as group B (9% vs. 59% respectively; p = 0.040) when compared to baseline. The magnitude of increase in proportion of participants with correct inhaler technique following intervention was not significantly different between group A and group B (63% and 59%, respectively; n=236, p = 0.60).
When inhaler technique was expressed as a mean score out of 9 (as per the 9-item checklist), similar results were observed. There was no significant difference in mean Turbuhaler score at baseline for group A (6.7 ± 1.4; Mean ± SEM) vs. group B (6.5 ± 1.4), (Wilks' Lambda = 0.998, p = 0.45). There was a significant yet similar improvement in mean Turbuhaler score following intervention for group A (8.3 ± 1.1, mean ± s.e.m) as well as group B (8.3 ± 1.0) (Wilks' Lambda = 0.425, F(1,234), p < 0.001).
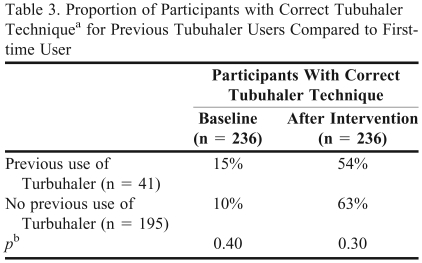
With regards to previous inhaler use, 41 out of 236 (17%) participants had previously used a Turbuhaler. There was no significant difference in the proportion of participants with correct technique at baseline (p = 0.40) or after the intervention (p = 0.30) for participants who had previously used a Turbuhaler compared with those who had never used it (Table 3). The most common reason for previous use was for asthma treatment.
Table 3.
Proportion of Participants with Correct Tubuhaler Techniquea for Previous Tubuhaler Users Compared to First-time User
Correct Turbuhaler technique as defined by a score of 9/9 on checklist used at baseline and after intervention.10
bComparison of correct Turbuhaler technique between participants in small-group training and self-directed Internet-based training.
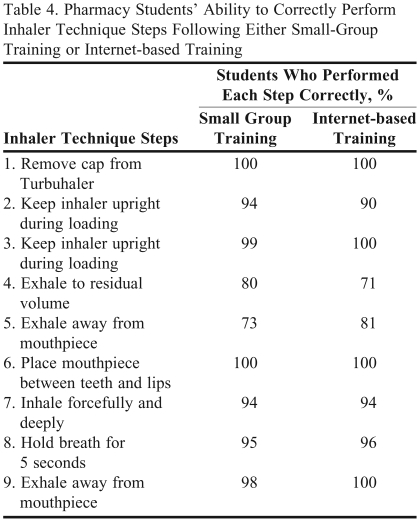
Analysis of the most common error in the technique indicated that step 4 (Exhale to residual volume) and Step 5 (Exhale away from the mouthpiece) were most commonly performed incorrectly. There was no significant differences between group A and group B (p > 0.05 for all steps) with regards to the proportion of participants demonstrating correct technique for each one of the 9 Turbuhaler steps (Table 4).
Table 4.
Pharmacy Students' Ability to Correctly Perform Inhaler Technique Steps Following Either Small-Group Training or Internet-based Training
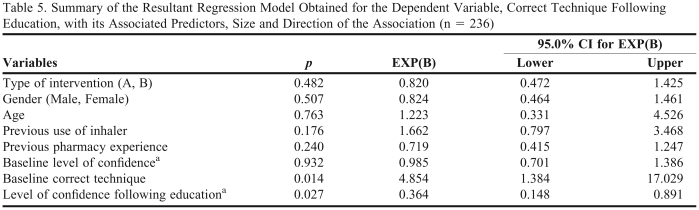
Logistic regression modeling identified “correct technique at baseline” and “level of confidence following intervention” to be significantly associated with correct technique following education (p = 0.014, R2 = 0.079; Table 5).
Table 5.
Summary of the Resultant Regression Model Obtained for the Dependent Variable, Correct Technique Following Education, with its Associated Predictors, Size and Direction of the Association (n = 236)
aLevel of confidence (1 = confident, 2 = not sure, 3 = not confident). Beta is the standardized regression coefficient. Beta values with their p values show whether each variable is making a statistically unique contribution to the model (p < 0.05) or not. The EXP(B) values are the odds ratios, which is the increase (or decrease if less than 1) in the odds of being in 1 outcome category when the value of the predictor increases by 1 unit. A 95% confidence interval (CI) is displayed for each of the odds values giving a lower and an upper value.
DISCUSSION
This study investigated the effectiveness of small-group training compared with self-directed Internet-based training to train undergraduate pharmacy students on Turbuhaler technique. Both self-directed Internet-based training and small-group training are equally effective in improving inhaler technique.
The Turbuhaler was chosen despite there being several respiratory devices currently available on the Australian and international markets. The Turbuhaler is one of the most commonly prescribed devices for preventer therapy; hence, its use has important implications for overall asthma management.1 Also, Turbuhalers were readily available for use in this study.
Correct technique rather than a Turbuhaler score out of 9 was chosen as the primary outcome variable as future health care professionals will be expected to perform all steps associated with Turbuhaler administration correctly in order to educate patients properly on correct inhaler technique. Hence, mean Turbuhaler technique score was used to describe the extent to which the technique had improved.
Prior to baseline assessment, students were given written information and a placebo inhaler device. This part of the study was aimed at mimicking the real-life scenario in which pharmacists would have access to information about device technique through the product information leaflet and would be required to study this independently.
Only a small proportion of students (10%) were able to use the Turbuhaler correctly after reading the written information provided. This is consistent with the literature that indicates that when it comes to device technique training, verbal instruction and written information are not effective in improving technique.7 Physical demonstration is the most effective method of educating both students and patients on correct inhaler technique.10,16 Based on this data, it is logical that a physical demonstration should be part of small-group training for device technique in the second year (as per group A intervention). Hence, when the self-directed Internet-based training (group B intervention) was developed, a physical demonstration identical to that received by the students in the small-group training was incorporated into the training program. Where the groups differed was mainly in the flexibility of the self-directed Internet-based training, which allowed students to replay it as often as needed, and in the small-group that allowed members to obtain peer feedback. The content of both interventions was identical in all other aspects.
Although results suggested that both interventions were equally effective at educating pharmacy students on Turbuhaler technique, about 40% of students still continued to demonstrate incorrect technique following the intervention. This suggests that neither intervention may be considered sufficiently effective. It is important to consider why this may be the case when studies have clearly shown that educating people with asthma on the correct use of an inhaler, can result in 100% of patients using their device correctly.7 The difference in achieving correct technique with undergraduate students compared with studies with patients might be due to several factors, including that (1) the motivation for learning technique is different for students than for patients; (2) patients receive individual feedback from trained professionals, whereas students received feedback from primarily inexperienced peers; and (3) as patients are regular users of these devices, it might be that achieving correct technique is somewhat easier for them than for students, a majority of whom have never before held an inhaler.
The results were further analyzed to determine the mean Turbuhaler technique scores at baseline and after the intervention for group A and group B to determine whether students with incorrect technique at least showed improvement in their scores. Despite the high proportion of students with incorrect technique, there was a significant improvement in mean scores after the intervention. This suggests that even though a significant proportion of students continued to demonstrate incorrect technique after the intervention, their inhaler technique had improved. The most problematic steps demonstrated by the majority of students were failure to exhale to residual volume and to exhale away from the mouthpiece (Table 1). This is consistent with other studies in which patients found these same 2 steps most problematic.17 The consistency with which these particular steps continue to be a problem suggests that perhaps educational interventions should highlight these particular steps.
Seventeen percent of students had used a Turbuhaler prior to the study; however, these students did not show better results at baseline or after the intervention compared to students who had never previously used one. Although this is disappointing, this may be due to a range of factors, such as not receiving effective counselling from their health care professionals when they were first prescribed their inhalers, or not having their technique reviewed regularly as device technique declines over time following education.18
Following education, confidence and correct inhaler technique were correlated. In contrast, the same was not observed for pre-education confidence and technique. This may be due to the fact that prior to the intervention, students did not completely grasp the notion of what correct technique entails; hence, they were not able to reasonably or realistically judge their own competency or confidence in using the inhaler. Hence, asking an individual as to whether he or she feels confident to use the inhaler may not elicit a reliable response unless the individual knows what correct inhaler technique is. This regression analysis, however, most importantly demonstrates that inhaler technique prior to education was not a predictor of inhaler technique post education. This suggests that no matter what the initial inhaler technique is, individuals can be taught how to use these inhalers.
This study would have been improved if the assessors had been blinded to group allocations. Due to time and resource constraints, experienced inhaler technique assessors were engaged in the evaluation of student technique. Practically, this resulted in 2 of the 3 assessors not being blinded to the group allocations. The implications of this on the actual study outcome, however, are considered minimal, mainly because each assessor was required to evaluate a large number of students in a short timeframe, and both blinded and unblinded assessors were consistent in their assessments. This was explored at the beginning of each assessment session. Furthermore, the Internet-based training was conducted during the tutorial, in a controlled environment rather than at home, so it was difficult to predict how students would use the Internet-based program at home on their own time. These limitations could be overcome in future studies. Further, the impact of individualized inhaler technique feedback as well as group education would be worth exploring in this undergraduate student sample.
This study showed that, when it comes to training undergraduate pharmacy students on correct inhaler technique, Internet-based training is equally as effective as face-to-face training. This is consistent with published studies conducted in other arenas.15,19-26 Given the popularity of Internet-based training,21,22 this provides tertiary educators with another effective option for training students with several advantages. The Internet is usually easily accessible for college students and training is usually self-paced and highly interactive. It also involves reduced costs in terms of tutor-led workshops and is more efficient, enabling more complex topics to be covered in workshops. The content available online also is readily and easily updated and altered. Internet-based training also provides an ideal format for continuing professional education for practicing health care professionals. Future studies, however, should continue to focus on the exploration and evaluation of educational methods that are sustainable and universally effective in inhaler technique training, given the significance and monopoly of inhaler use among a broad range of respiratory patients.
SUMMARY
Internet-based training appears equally effective as face-to-face training in educating pharmacy students on inhaler device technique. However, neither method appears sufficiently effective, with 40% of students still having difficulty in demonstrating incorrect inhaler technique after the training sessions. Identifying strategies to improve the success of training large cohorts of students with minimal resources and within a fixed timeframe need to be further explored. Strategies that incorporate individualized feedback and reinforcement over time also need to be developed.
ACKNOWLEDGMENTS
The authors would like to acknowledge the contribution of the students who participated in this research and Dr. Vicky Kritikos for allowing access to her tutorial group during the teaching semester.
REFERENCES
- 1. National Asthma Council Australia. Asthma management handbook. 2006. Available at http://www.nationalasthma.org.au/cms/index.php Accessed August 2009.
- 2.Shrestha M, Parupia HMF, Andrews B, Kim SW, Martin TS, Park D, Gee E. Metered-dose inhaler technique of patients in an urban ED: prevalence of incorrect technique and attempt at education. Am J Emerg Med. 1996;14(4):380–384. doi: 10.1016/s0735-6757(96)90054-6. [DOI] [PubMed] [Google Scholar]
- 3.Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Resp Care. 2005;50(10):1360–1374. [PubMed] [Google Scholar]
- 4.Crompton GK. The adult patient's difficulties with inhalers. Lung. 1990;(168 Suppl):658–62. doi: 10.1007/BF02718191. [DOI] [PubMed] [Google Scholar]
- 5.Epstein S, Maidenberg A, Hallett D, Khan K, Chapman K. Patient handling of a dry-powder inhaler in clinical practice. Chest. 2001;120(5):1480–1484. doi: 10.1378/chest.120.5.1480. [DOI] [PubMed] [Google Scholar]
- 6.Molimard M, Rahersion C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16(3):249–254. doi: 10.1089/089426803769017613. [DOI] [PubMed] [Google Scholar]
- 7.Basheti I, Reddel HK, Armour CA, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol. 2007;119(6):1537–1538. doi: 10.1016/j.jaci.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 8.Togger DA, Brenner PS. Metered dose inhalers: When it comes to knowing how to use these devices effectively, nurses and patients alike have been found wanting. Demonstrate each step to ensure your patients are getting all they can from their inhaled medications. Am J Nurs. 2001;101(10):26–32. doi: 10.1097/00000446-200110000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Armour C, Bosnic-Anticevich SZ, Brilliant M, et al. Pharmacy asthma care program (PACP) improves outcomes for patients in the community. Thorax. 2007;62(6):496–592. doi: 10.1136/thx.2006.064709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Counseling about Turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir Care. 2005;50(5):617–623. [PubMed] [Google Scholar]
- 11.Sestini P, Cappiello V, Alliani M, et al. Prescription bias and factors associated with improper use of inhalers. J Aerosol Med. 2006;19(2):127–136. doi: 10.1089/jam.2006.19.127. [DOI] [PubMed] [Google Scholar]
- 12.Steier J, Trammer T, Cloes RM, Petro W. Optical feedback of inhalation with Autohaler and Turbuhaler in COPD patients. Lung. 2003;181(4):183–192. doi: 10.1007/s00408-003-1018-x. [DOI] [PubMed] [Google Scholar]
- 13.Kesten S, Zive K, Chapman KR. Pharmacist knowledge and ability to use inhaled medication delivery systems. Chest. 1993;104(6):1737–1742. doi: 10.1378/chest.104.6.1737. [DOI] [PubMed] [Google Scholar]
- 14.Erickson SR, Landino HM, Zarowitz BJ, Kirking DM. Pharmacists' understanding of patient education on metered-dose inhaler technique. Ann Pharmacother. 2000;34(11):1249–1256. doi: 10.1345/aph.19227. [DOI] [PubMed] [Google Scholar]
- 15.Erickson SR, Chang A, Johnson C, Gruppen LD. Lecture versus web tutorial for pharmacy students' learning of MDI technique. Ann Pharmacother. 2003;37(4):500–505. doi: 10.1345/aph.1C374. [DOI] [PubMed] [Google Scholar]
- 16.Lee-Wong M, Mayo PH. Results of a programme to improve house staff use of metered dose inhalers and spacers. Postgrad Med J. 2003;79(930):221–225. doi: 10.1136/pmj.79.930.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Counseling. 2008;72(1):26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Petro W, Schuppenies A. Inhalation therapy by dose-inhalers: analysis of patients' performance and possibilities for improvement (abstract) Pneumologie. 2005;59(5):316–320. doi: 10.1055/s-2004-830213. [DOI] [PubMed] [Google Scholar]
- 19.Calderon Y, Haughley M, Bijur P, leider J, Moreno-Walton L, Torres S, Gennis P, Bauman L. An Educational HIV Pretest Counseling Video Program for Off-Hours Testing in the Emergency Department. Ann Emerg Med. 2006;48(1):21–27. doi: 10.1016/j.annemergmed.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Ryan G, Lyon P, Kumar K, Bell J, Barnet S, Shaw T. Online CME: An effective alternative to face-to-face delivery. Med Teach. 2007;29(8):251–257. doi: 10.1080/01421590701551698. [DOI] [PubMed] [Google Scholar]
- 21.Curran VR, Hoekman T, Gulliver W, Landells I, Hatcher L. Web-based Continuing Medical Education. Evaluation study of computer-mediated continuing medical education. J Continuing Educ Health Prof. 2000;20(2):106–119. doi: 10.1002/chp.1340200207. [DOI] [PubMed] [Google Scholar]
- 22.Hedaya MA, Collins P. Pharmacokinetic teaching utilizing the world wide web: a Flashlight assessment. Am J Pharm Educ. 1999;63(4):415–421. [Google Scholar]
- 23.Kay EJ, Silkstone B, Worthington HV. Evaluation of computer aided learning in developing clinical decision-making skills. Br Dent J. 2001;190(10):554–557. doi: 10.1038/sj.bdj.4801033. [DOI] [PubMed] [Google Scholar]
- 24.Vanderveen RP, Abate MA, Haxby D. A literature evaluation course delivered via computer assisted instruction, electronic mail, and teleconferences: a case description. Am J Pharm Educ. 1999;63(2):178–182. [Google Scholar]
- 25.Wade WE, Cobb HH, Spruill WJ, Chisholm MA. Assessment of student performance in an advanced pharmacokinetics course taught by three methods of instruction delivery. Am J Pharm Educ. 2000;63(1):15–18. [Google Scholar]
- 26.Sowinski KM, Scott SA, Carlstedt BC. An internet training module for traditional and non-traditional doctor of pharmacy students: Content and evaluation. Am J Pharm Educ. 2000;64(1):15–8. [Google Scholar]