Abstract
Objective
To assess whether a raised serum troponin T concentration would be an independent predictor of death in patients with an acute ischaemic stroke.
Design
Observational study.
Setting
Auckland Hospital, Auckland, New Zealand.
Subjects
All 181 patients with an acute ischaemic stroke admitted over nine months in 1997-8, from a total of 8057 patients admitted to the acute medical service.
Main outcome measures
Blood samples for measuring troponin T concentration were collected 12-72 hours after admission; other variables previously associated with severity of stroke were also recorded and assessed as independent predictors of inpatient mortality.
Results
Troponin T concentration was raised (>0.1 μg/l) in 17% (30) of patients admitted with an acute ischaemic stroke. Thirty one patients died in hospital (12/30 (40%) patients with a raised troponin T concentration v 19/151 (13%) patients with a normal concentration (relative risk 3.2 (95% confidence 1.7 to 5.8; P=0.0025)). Of 17 possible predictors of death, assessed in a multivariate stepwise model, only a raised troponin T concentration (P=0.0002), age (P=0.0008), and an altered level of consciousness at presentation (P=0.0074) independently predicted an adverse outcome.
Conclusions
Serum troponin T concentration at hospital admission is a powerful predictor of mortality in patients admitted with an acute ischaemic stroke.
Introduction
Stroke is the third commonest cause of death in Western industrialised countries1 and is a major cause of long term morbidity.2 The link between heart disease and acute stroke is already established. Cardioembolism accounts for 15-20% of all strokes,3 and conversely, after a stroke, patients are at increased risk of developing electrocardiographic changes, cardiac arrhythmias, and myocardial cell damage.4 Creatine kinase concentrations rise in some patients after a stroke, and the myocardial subfraction (creatine kinase MB) is a predictor of early death.5 Troponin T and I are highly sensitive and specific markers of cardiac damage and are more predictive than creatine kinase of adverse outcomes in patients presenting with unstable angina or myocardial infarction.6 We hypothesised that a raised serum troponin T concentration would be an independent predictor of early death in patients with an acute ischaemic stroke.
Subjects and methods
From 8 July 1997 to 8 March 1998, all patients with an acute ischaemic stroke presenting to the acute medical service at Auckland Hospital (n=181) were identified at the daily general medical “handover” meetings and from the hospital admission database. These patients were followed until hospital discharge. Intracerebral or subarachnoid haemorrhage was ruled out by computed tomography at the time of admission in 172 patients. The other nine patients were included without computed tomography because haemorrhage was thought to be unlikely on clinical grounds. These nine patients came from both groups of subjects (those with and without a raised troponin T concentration), and their inclusion did not alter the outcome of the study.
Blood samples were collected 12-72 hours after admission. Information about symptoms of heart disease, cardiac history, and risk factors was collected in all patients. The severity of stroke was measured on admission by assessing (according to the Scandinavian stroke scale7) the level of consciousness; eye movements; strength in the hand, arm, leg, and face; speech, orientation, and gait. Other variables previously associated with stroke severity—serum glucose concentration, temperature, and blood pressure at admission—were recorded.8,9 Patient outcomes were recorded as death in hospital, return home, or discharge to a rest home or private hospital (institutional care).
Serum cardiac troponin T concentration was measured using the Elecsys 2010 immunoassay system (Roche-Boehringer, Mannheim). Concentrations over 0.1 μg/l were deemed raised.10
The local ethics committee approved the study.
Analysis
Continuous variables were compared by unpaired t tests, and binomial variables were compared using Fisher's exact test. Actuarial curves were constructed using the Kaplan-Meier method, and comparisons were made by the log rank method. Logistic regression was done using the SAS/STAT package, version 6 (SAS Institute).
Results
Of 8057 patients admitted to the acute medical service at Auckland hospital, 181 patients (mean age 75 years; 89 women) presented with an acute ischaemic stroke; 174 of these cases involving the anterior circulation and seven involving the posterior circulation. Fifty seven patients had a history of ischaemic heart disease, but none was known to have had an acute myocardial infarction or unstable angina in the three weeks before admission.
Thirty (17%) patients had a raised troponin T concentration (3.29 (SD 6.19) μg/l). These patients were older than those with a normal troponin concentration (78.9 (8.3) years v 74.1 (10.6) years; P<0.01), but there were no other differences in baseline characteristics between the two groups. Proportions of patients with a history of ischaemic heart disease were similar in both those with and those without a raised troponin T concentration (10/30 v 47/151 respectively; P=0.83).
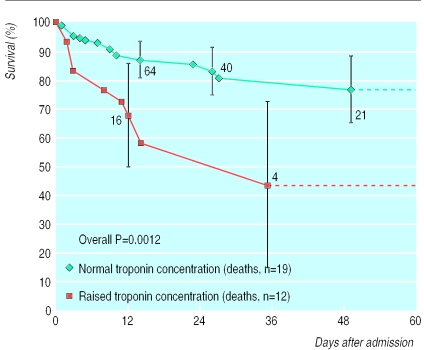
Thirty one patients died in hospital (12/30 (40%) patients with a raised troponin T concentration v 19/151 (13%) with a normal concentration); the relative risk for inpatient mortality in the patients with a raised concentration was 3.2 (95% confidence interval 1.7 to 5.8; P=0.0025). Overall, 40% of all inpatient deaths were among the 30 patients with a raised troponin T concentration. At 60 days a significant mortality difference between the two groups persisted (figure). If a combined end point of death in hospital and discharge to institutional care was considered, troponin T was still a powerful predictor of outcome (1.9; 1.4 to 2.5 (P=0.0108)). Renal failure is a recognised cause of raised troponin T concentration,11 but the results were not altered by exclusion of patients with a serum creatinine concentration >0.2 mmol/l.
Seventeen factors that may predict death were assessed in a multivariate stepwise model. These factors were history of ischaemic cardiac disease, treatment for hypertension, diabetes mellitus, smoking, atrial fibrillation, impaired renal function, age, all nine clinical indicators used to measure stroke severity, and a positive troponin T result. Only a raised troponin T concentration (P=0.0002), age (P=0.0008), and an altered level of consciousness at presentation (P=0.0074) predicted an adverse outcome.
Three patients with incomplete data on stroke severity were excluded from further analysis. There was a non-significant trend for patients with a raised troponin T concentration to have an abnormality in any one of the nine categories we used to assess stroke severity. Fifty patients had an altered level of consciousness at presentation (11/30 (37%) patients with a raised troponin T concentration v 39/148 (26%) with a normal concentration (P=0.27)). Neither the individual categories nor the combined prognostic score predicted mortality in a multivariate analysis.
Forty one patients had a serum glucose concentration >8 mmol/l at admission,9 and this was significantly more common in patients with a raised troponin T concentration than in those with a normal concentration (12/30 v 29/151; P=0.018). There was no significant difference between the two groups of subjects in terms of mean temperature (36.3°C v 36.6°C; P=0.40), systolic blood pressure (155 mm Hg v 163 mm Hg; P=0.22), or diastolic blood pressure (91 mm Hg v 93 mm Hg; P=0.55) at admission. When serum glucose concentration, temperature, and systolic and diastolic blood pressure at admission were included in the multivariate analysis, none of these factors predicted death or discharge to institutional care.
Discussion
This study has shown that a raised serum concentration of troponin T is a major predictor of death after an acute ischaemic stroke (with a threefold increase in mortality). The use of the more sensitive troponin T assay has shown a greater frequency of myocardial damage and was more predictive of death than studies using creatine kinase or its myocardial subfraction (creatine kinase MB).5 Previous studies have suggested that cardiac damage after a stroke is neurally mediated through abnormal autonomic discharges.4,12 Noradrenaline concentrations are raised after a stroke, and higher concentrations have been associated with myocardial changes.13 Our results are consistent with this mechanism, although there are other possible explanations, including that a prior cardiac event resulted in the subsequent stroke. However, in our cohort, which included 57 patients with known ischaemic heart disease, no previous cardiac events had been identified and hence any myocardial damage was asymptomatic. Further studies are needed to determine if the cause of death differs between patients with raised troponin T concentration and those with a normal concentration.
What is already known on this topic
An acute stroke may be followed by electrocardiographic changes, cardiac arrhythmias, and a rise in creatine kinase concentration
Troponin T concentration is a more sensitive and specific marker for cardiac damage than creatine kinase concentration
What this study adds
This study used the troponin T assay to investigate the frequency of unsuspected cardiac damage among patients presenting with an ischaemic stroke
It found both a high incidence of cardiac damage (17%) and a strong association with inpatient mortality (a threefold increase in the risk of death) in patients presenting with an ischaemic stroke
Myofibrillar degeneration and electrocardiographic abnormalities are more likely in patients with an acute increase in intracranial pressure. Therefore, cardiac complications and a raised troponin T concentration would be expected to be more common in patients with severe ischaemic strokes. In this study there was a non-significant trend for a raised troponin T concentration to be associated with more severe strokes, as assessed by the Scandinavian stroke scale. However, we could not correlate computed tomography data with clinical outcomes. Computed tomography was usually performed in the first 24 hours to differentiate between ischaemic and haemorrhagic strokes. In the first 48 hours, however, the extent of an acute infarct is often poorly defined on computed tomography. A previous study found that infarct volume measured by computed tomography was poorly correlated with clinical measures of stroke severity and outcome.14
Troponin T concentration was measured in a single serum sample obtained 12 to 72 hours after admission to hospital. Serial measurement of troponin T concentration and creatine kinase MB over the following few days would be needed to determine the time course of myocardial damage after an ischaemic stroke.
Figure.
Actuarial survival after admission of 181 patients (151 with normal concentration of troponin T; 30 with raised troponin) to hospital with acute stroke (error bars show 95% confidence intervals). Numbers indicate numbers of patients still at risk in hospital (that is, excluding those who have died and those who have recovered and left hospital)
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Bonita R, Beaglehole R. Cerebrovascular disease: explaining stroke mortality trends. Lancet. 1993;341:1510–1511. doi: 10.1016/0140-6736(93)90640-3. [DOI] [PubMed] [Google Scholar]
- 2.Anderson NE, Bonita R, Broad JB. Early management and outcome of acute stroke in Auckland. Aust N Z Med J. 1997;27:561–567. doi: 10.1111/j.1445-5994.1997.tb00965.x. [DOI] [PubMed] [Google Scholar]
- 3.Brickner ME. Cardioembolic stroke. Am J Med. 1996;100:465–474. doi: 10.1016/s0002-9343(97)89525-3. [DOI] [PubMed] [Google Scholar]
- 4.Samuels MA. Neurally induced cardiac damage: definition of the problem. Neurol Clin. 1993;11:273–292. [PubMed] [Google Scholar]
- 5.Norris JW, Hachinski VC, Myers MG, Callow J, Wong T, Moore RW. Serum cardiac enzymes in stroke. Stroke. 1979;10:548–553. doi: 10.1161/01.str.10.5.548. [DOI] [PubMed] [Google Scholar]
- 6.Donnelly R, Millar-Craig MW. Cardiac troponins: IT upgrade for the heart. Lancet. 1998;351:537–539. doi: 10.1016/S0140-6736(05)78549-4. [DOI] [PubMed] [Google Scholar]
- 7.Scandinavian Stroke Study Group. Multicenter trial of hemodilution in ischemic stroke: background and study protocol. Stroke. 1985;16:885–890. doi: 10.1161/01.str.16.5.885. [DOI] [PubMed] [Google Scholar]
- 8.Reith J, Jorgensen HS, Pedersen PM, Nakayama H, Raaschow HO, Jeppersen LL, et al. Body temperature in acute strokes: relation to stroke severity, infarct size, mortality and outcome. Lancet. 1996;347:422–425. doi: 10.1016/s0140-6736(96)90008-2. [DOI] [PubMed] [Google Scholar]
- 9.Weir JW, Gordon DM, Alexander GD, Kennedy RL. Is hypoglycaemia an independent predictor of poor outcome after acute stroke? Results of a long term follow up study. BMJ. 1997;314:1303–1306. doi: 10.1136/bmj.314.7090.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christenson RH, Duh SH, Newby LK, Ohman EM, Califf RM, Granger CB, et al. Cardiac troponin T and cardiac troponin I: relative values in short term risk stratification of patients with acute coronary syndromes. Clin Chem. 1998;44:494–501. [PubMed] [Google Scholar]
- 11.McNeil AR, Marshall M, Ellis CJ, Hawkins RC. Why is troponin T increased in the serum of patients with end-stage renal disease? Clin Chem. 1998;44:2377–2378. [PubMed] [Google Scholar]
- 12.Myers MG, Norris JW, Hachinski VC, Weingert ME, Sole MJ. Cardiac sequelae of acute stroke. Stroke. 1982;13:838–842. doi: 10.1161/01.str.13.6.838. [DOI] [PubMed] [Google Scholar]
- 13.Myers MG, Norris JW, Hachinski VC, Sole MJ. Plasma norepinephrine in stroke. Stroke. 1981;12:200–204. doi: 10.1161/01.str.12.2.200. [DOI] [PubMed] [Google Scholar]
- 14.Saver JL, Johnston KC, Homer D, Wityk R, Koroshetz W, Truskowski LL, et al. Infarct volume as a surrogate or auxiliary outcome measure in ischemic stroke clinical trials. Stroke. 1999;30:293–298. doi: 10.1161/01.str.30.2.293. [DOI] [PubMed] [Google Scholar]