Abstract
Eighty four heavy drinkers who responded to a newspaper recruitment ad were randomly assigned to receive either: a) training in a moderate drinking protocol via an Internet-based program (www.moderatedrinking.com) and use of the online resources of Moderation Management (MM) (www.moderation.org) or b) use of the online resources of MM alone. Follow-ups are being conducted at 3, 6, and 12 months. Results of the recently completed 3 month follow-up (86% follow-up) indicated both groups significantly reduced their drinking based on these variables: standard drinks per week; percent days abstinent; and mean BAC per drinking day. Both groups also significantly reduced their alcohol-related problems. Relative to the control group the experimental group had better outcomes on percent days abstinent and log Drinks per Drinking Day. These short-term outcome data provide evidence for the effectiveness of both the moderate drinking web application and of the resources available online at MM in helping heavy drinkers reduce their drinking and alcohol-related problems.
Introduction
Problem drinkers: An under-served population
Epidemiological research suggests that there are four times as many individuals with alcohol problems with no evidence of dependence relative to those who meet the criteria for dependence (NIAAA, 2000). A recent report indicates that this group is increasing in size while the prevalence of alcohol dependence is declining (NIAAA, 2004). The Institute of Medicine (1990) described non-dependent problem drinkers as a large but under-served group and identified the need to provide interventions for this group. While moderation training protocols such as Behavioral Self-Control Training (BSCT) have been found to be effective for this population (see Hester, 2003 for a review) there are barriers to its widespread implementation in the U.S. First, traditional alcoholism treatment programs usually see drinkers who are at the most severe end of the dependence spectrum and most providers are resistant to using moderation protocols even with non-dependent clients (Institute of Medicine, 1990). Second, health care settings such as family practices and mental health clinics are not structured to offer drinkers such services (SAMSHA, 2007). On the other hand, an Internet-based or “web application” that is independent of alcohol treatment programs could be an alternative approach for meeting the needs of this under-served population.
Moderation Management (MM)
MM is a mutual-help organization that focuses specifically on this under-served population. Their web site (www.moderation.org) describes MM as a “behavioral change program and national support group network for people concerned about drinking and who desire to make positive lifestyle changes. MM empowers individuals to accept personal responsibility for choosing and maintaining their own path, whether moderation or abstinence.” MM offers an online mutual-help support community, face-to-face meetings, and written materials describing MM’s program of behavioral change. A survey found that most MM members were young to middle-aged, white, and well educated. They reported frequent heavy drinking, but few signs of alcohol dependence (Humphreys & Klaw, 2001).
Behavioral self-control training
Early BSCT protocols focused primarily on changing drinking behaviors to achieve moderation. The basic components of early protocols included goal setting, self-monitoring, and rate control. There have been 46 controlled clinical trials of BSCT, nearly all of which evaluated these early protocols (see Hester, 2003 and Miller, Wilbourne, & Hettema, 2003 for reviews). BSCT, delivered in various formats, has been tested in more controlled clinical trials than any other intervention for alcohol problems and its efficacy has been consistently supported by this empirical research. Heather and colleagues have noted that “BSCT has become the standard moderation-oriented treatment in countries in which the goal is an accepted part of treatment services” (Heather et al., 2000, pg. 562).
Researchers have evaluated BSCT in a wide range of clinical populations and compared it to other effective interventions. BSCT with a goal of moderation is, at least in the U.S., less effective than abstinence-oriented approaches for severely dependent clients (e.g., Foy, Nunn, & Rychtarik, 1984). However, when drinkers who are not alcohol dependent are assigned at random to abstinence or moderation goals, long-term results are consistently comparable (e.g., Sanchez-Craig et al, 1984). Also, less intensive ways of delivering BSCT (e.g., via self-help books) are usually as effective as more intensive ways of delivering BSCT.
Miller and colleagues conducted a long-term (2–8 years) follow-up of individuals who had been involved in BSCT studies at The University of New Mexico (Miller, Leckman, Delaney, & Tinkcom, 1992). They found that many individuals who were initially successful at moderating their drinking eventually stopped drinking entirely; for them, successful moderation was a stepping stone to abstinence. They also found a group of individuals who had consistently moderated their drinking without any signs of alcohol-related problems. The pre-treatment client characteristics predictive of success with BSCT were fewer signs of dependence and a shorter history of alcohol-related problems.
In summary, BSCT procedures with a goal of moderation have been extensively studied. These studies collectively show that some problem drinkers respond favorably to this approach, sustaining moderate and non-problematic drinking over extended periods, whereas others, following BSCT with a moderation goal, eventually opt for total abstinence (some with and some without additional treatment). Some drinkers, however, did not benefit from these early protocols emphasizing moderate drinking skills. Thus we concluded that a more comprehensive protocol (with appropriate segues to an abstinence goal) could be more helpful to heavier drinkers.
Computer-based BSCT
We have found computer-based training in BSCT to be effective in helping individuals reduce their drinking. Fifteen years ago we developed the Behavioral Self-Control Program for Windows (BSCPWIN) and evaluated its effectiveness in a randomized clinical trial (Hester & Delaney, 1997). At pre-treatment, participants were drinking, on average, six standard drinks per day, five days per week, with a weekly estimated peak BAC of 169mg%. At the 10 week follow-up the experimental group who received the BSCPWIN reduced their drinking while the wait-list control group showed only a modest reduction in drinking. The wait-list control group significantly reduced their drinking by the 20 week follow-up after going through the BSCPWIN program. At 12 month follow-up participants on average were drinking less than half that amount with average peak BACs of 53mg%. We compared treatment effect sizes with other BSCT studies and found BSCPWIN to be comparable to BSCT provided in face-to-face individual therapy and in group settings. This protocol, however, needed to be updated to reflect current empirical research. (The details of the new protocol are described in the next section.) We also changed it from a Windows program that had to be downloaded, installed, and was limited to a Windows PC, to a web application that is available online and is independent of the user’s operating system. The Moderate Drinking web application is the result of these revisions.
The findings of our BSCPWIN study are consistent with a rapidly growing body of literature demonstrating the effectiveness of computer-based (i.e., Windows programs) and online interventions for addictions, mental health disorders, and health-related diseases. As one indication of this body of research, the Journal of Medical Internet Research (www.jmir.org) is in its 10th year of online publication, publishing four issues online per year with 44 articles in 2008 (through November), including three reviews of the literature.
Carroll and colleagues (2008) evaluated the efficacy of a computer-based cognitive behavioral program for addictions in a randomized clinical trial (RCT) with 77 individuals seeking treatment for substance abuse. Using an additive design they found that individuals receiving the computer-based intervention showed greater improvement based on negative urine screens and longer continuous periods of abstinence during treatment compared to those who received only the treatment program as usual. They concluded that the program is an effective adjunct to outpatient treatment.
Walters and colleagues developed and evaluated a brief motivational intervention for heavy drinking college students, the electronic Check-up To Go (eCHUG). Results indicated significantly greater reductions in drinking at 8 week follow-ups for the eCHUG group in comparison to the control group, but between group differences were no longer significant by the 16 week follow-up (Walters, Vader, & Harris, 2007). Walters, Miller, and Chiauzzi (2005) also have reviewed the commercially available web applications for college students.
Calbring and Smit (2008) combined an Internet-based program with minimal therapist contact (email and brief weekly phone calls) for problem gamblers. They found significant improvements in both gambling measures, anxiety, depression, and quality of life at follow-ups. Large effect sizes were reported at follow-ups up to 36 months.
Norman and colleagues (2008) reported evidence from a RCT for the effectiveness of a web application for smoking prevention and cessation in schools. They found both an increase in negative attitudes towards smoking and a reduction in smoking behaviors in current adolescent smokers. However, not all web-assisted tobacco interventions are found to be as effective as this study. A systematic review of this topic by Bock and colleagues (2008) concluded that while the quality of interventions has improved, there is “substantial room for further improvements to ensure that smokers are offered high-quality, evidence-based treatments” (www.jmir.org/2008/5/e39/html).
The Moderate Drinking web application
The protocol upon which we based our web application is similar to that advocated by MM (Rotgers, Kern, & Hoeltzel, 2003). The protocol is divided into modules which focus on the following topics (modules followed by an * have been developed since the original moderation training protocols in the 1970’s): Building motivation and self-confidence*; setting drinking goals/limits; “doing a 30” (an initial month long period of abstinence)*; self-monitoring drinking (with personalized feedback relative to the goals the drinker has set); rate control; setting personal drinking rules*; self-monitoring urges to drink (with personalized feedback)*; identifying and managing triggers; developing alternatives; general problem solving*; dealing with lapses and/or relapses*; considering abstinence*; and self-monitoring one’s own mood using the Positive and Negative Affect Scale* (with feedback relative to baseline levels) (Watson, Clark & Tellegen, 1988).
When users register on the site, the MD program recommends first choosing a goal (abstinence or moderation), building motivation for change, “doing a 30,” setting moderate drinking goals/limits (if that is the desired goal), and then self-monitoring one’s drinking. Users are prompted to enter their self-monitoring data each time they log back onto the site, and then get feedback about their progress towards their goals. If their goal is moderation, their drinking feedback is cumulative and compared to their goals. If their goal is abstinence, the program asks them to enter their urges to drink self-monitoring data. Users can go through the program’s modules in order or they can pick and choose which modules might best meet their needs. Readers interested in viewing the program online can contact the senior author for access.
Moderation Management
MM is, to our knowledge, the only mutual-help group supportive of moderation in drinking as opposed to other groups that focus solely on abstinence. While MM is also supportive of abstinence, they are aware of the research finding that most non-dependent drinkers cut back on their drinking when they decide to change (Klingemann & Sobell, 2007). They offer face-to-face meetings in a number of sites around the U.S. and abroad as well as online meetings and a listserv, and will soon offer a forum. Their web site also provides the basic steps of moderation guidelines, the Rotgers et al. (2003) self-help book, an interactive program that allows users to report their abstinence and moderate drinking days in a calendar online (for others to see), and help in subscribing to the MM support group listserv.
Objectives
The purpose of this study was to evaluate the effectiveness of both the Moderate Drinking (MD) web application as an adjunct to participation in the online activities offered by MM, and the effectiveness of those activities and resources available online at MM by themselves.
Hypotheses
Both experimental and control groups will reduce their consumption and alcohol-related problems relative to baseline levels at follow-ups.
The experimental group will show a greater reduction in consumption and alcohol-related problems relative to the control group at all follow-ups.
Institutional Review Board
This study was approved by our designated Institutional Review Board at Presbyterian Healthcare Systems, Albuquerque, NM.
Methods
Planned study population
We planned this study as an effectiveness trial to maximize its external validity. Toward that end we limited the exclusion criteria (discussed below) to mainly exclude alcohol dependent drinkers. Based on our previous moderate drinking study, we planned to recruit a 50-50 split of men and women and 25% Hispanics (consistent with their prevalence in the Albuquerque, NM metro area). Our primary recruitment tool was a display ad in the weekly TV guide section of the local newspaper.
Inclusion criteria
We had six inclusion criteria: 1. Alcohol Use Disorder Identification Test (AUDIT) (Saunders et al, 1993)scores >7; 2. Drinking 10+ standard (14 grams) drinks per week; 3. Not currently abstaining; 4. Interest in moderating their consumption; 5. Minimum age 21; and 6. A computer with Internet access at home.
AUDIT scores of 8 or more suggest the presence of alcohol-related problems or at least risk for alcohol-related problems (Saunders et al, 1993). A minimum of 10 drinks per week is somewhat arbitrary. However, our experience and that of other moderation training trials suggest that individuals drinking less than this amount per week are less likely to benefit from a moderate drinking protocol. Individuals who are currently abstaining were advised to continue to do so and were referred to abstinence-oriented resources in our community. We only recruited adults because we felt that a moderate drinking program for minors would need to be tailored specifically to their developmental stages. We required participants to have a computer with Internet access at home so that they could access the online MM community and the MD web application from there.
Exclusion criteria
We chose these criteria to exclude participants who were most unlikely to benefit from the protocols, given prior research in moderation: 1. History of treatment for substance abuse; 2. History of hospitalization for alcohol or drug dependence or detoxification; 3. Past or current diagnosis of drug abuse or dependence; 4. Evidence of past or present physical dependence (major withdrawal symptoms: DTs, seizures, hallucinations); 5. Current indication of psychosis or bipolar disorder based on self-report; 6. Evidence of significant cognitive impairment from brain dysfunction (based on self-report and observation during screening interviews); 7. Evidence of health oriented contraindications to any further drinking (e.g., taking MAOIs, Hepatitis C, pregnancy, congestive heart failure); 8. English reading level below the 8th grade (assessed using the Slosson Oral Reading Test, (Slosson, 1990)); 9. Unwilling or unable to be available for follow-ups; 10. Unwilling or unable to provide one significant other (SO) for corroboration of their self-report of drinking; and 11. Currently a member of MM.
Experimental design
There are a number of ways we could have evaluated the effectiveness of the MD application. After considering them we chose an additive design that compares the MD + MM programs in combination to MM alone. While it cannot tell us the absolute impact that MD alone would have, it can tell us how much outcomes will improve above and beyond involvement in MM itself. This design maximizes external validity because this is how we envision the two resources will be used: the MD program as an adjunct to participation in MM.
We chose follow-up points at 3, 6, and 12 months from baseline. On the basis of previous BSCT studies, we anticipated that participants in the experimental condition would have received the majority of the benefit from using the MD web application in the first 3 months following intake.
Power analysis and sample size
There are no published outcome data for participation in MM from which we could calculate an effect size. BSCT protocols on the other hand, which is a component of MM, have published effect sizes. Since we do not know the extent to which members of MM use the BSCT protocol, we considered it prudent to assume that the estimated effect size of MM was probably less than that found in BSCT studies. After lengthy discussions with MM Board member Dr. Fred Rotgers, we estimated that the effect of the online MM support group was modest and around .4 (Cohen’s d, between Cohen’s cutoffs for “small” and “moderate” effect sizes). This is the effect size we used for the control condition in the power analysis.
In estimating the effect size of the experimental condition (MD + MM), we again considered the effect size of BSCT. We calculated an average effect size of BSCT based on a series of six studies by Miller and colleagues from 1982 to 1997 (Hester & Delaney, 1997). These studies had follow-up intervals ranging from 3 months to 2 years. The effect sizes had a mean of 1.11 (Range .89 – 1.36) for the variable of the mean weekly alcohol consumption at the final follow-up period compared to pretreatment levels. In our BSCPWIN trial we used the software as a stand-alone intervention and the mean standardized effect across three alcohol-consumption measures from pretreatment to a 12-month follow-up was 1.09. Between-group effect sizes, which could also be computed in our BSCPWIN trial for our initial follow-up, averaged 1.28 on these measures at the 10-week follow-up and averaged .67 at the 20-week follow-up, for an overall mean of .975. Because the MD condition in the current proposal will be an adjunct to MM involvement, we anticipated that its supplementary effect over and above the MM effect would be somewhat smaller than this. Thus, sample sizes for this study were determined by a power analysis based on a between-group effect size of .8, which indicated that a sample size of 27 per group would result in a power of .80 for detecting the effect hypothesized in our second experimental hypothesis at α = .05. We conservatively estimated that perhaps as many as 10% of participants who completed an Informed Consent form would not participate sufficiently to be considered treated, and another 10% would be lost or fail to come in for follow-ups by the 12 month follow-up. To compensate for this, our initial target was to recruit 27/.8 = 34 subjects per condition, for a total of 68 participants, in order to end up with 27 subjects per group at the end of the 12 month follow-up. In terms of the analyses of the separate within-group changes projected in our first experimental hypothesis, using procedures outlined in Maxwell and Delaney (2000, p. 568) and assuming a correlation across time periods of .5 consistent with that observed in Hester and Delaney (1997), it was determined that 27 subjects per group would yield a power greater than .95 in the MD group and a power greater than .65 in the MM group for detecting the anticipated within-group changes.
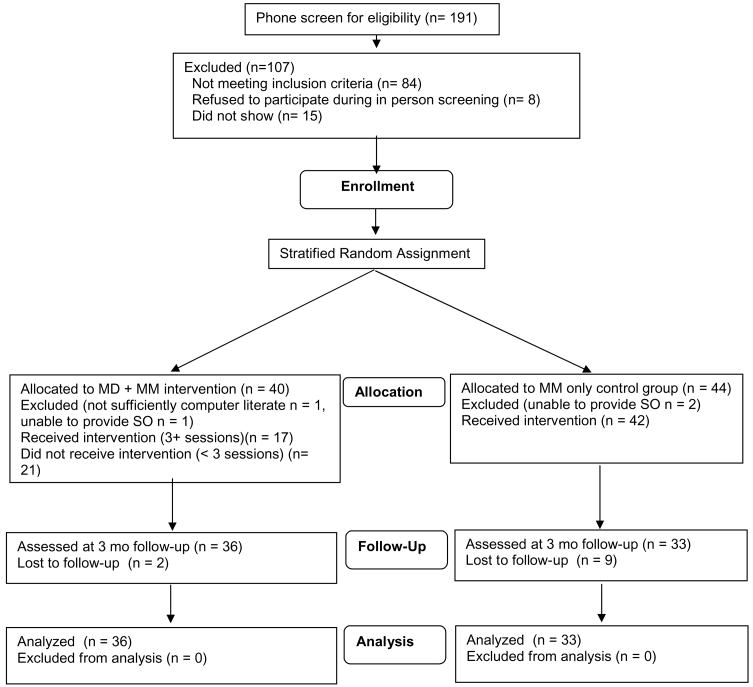
We revisited this power analysis after we had collected some of our initial 3 month follow-up data. Those initial data suggested a smaller difference in outcomes between the two groups and as a result we increased our sample size goal to 98. However we were not able to reach this goal by the time our recruitment window closed. Our final sample size is 80. See Figure 1 for a flow-chart of participants in the clinical trial.
Figure 1.
Flowchart of Participation through Trial.
Screening
Potential participants were screened over the phone using the Quick Screen from Project MATCH, and a questionnaire addressing inclusion criteria 2–6 and exclusion criteria 2–5, 8, 10, 11, and 12. We invited those who passed the phone screening to schedule an appointment for a face-to-face meeting for the remaining screening items, to discuss the clinical trial in more detail, and to review and sign the Informed Consent. The in-person screening included the Michigan Alcohol Screening Test (Selzer, 1971), the AUDIT, the Brief Symptom Inventory (BSI) (Derogatis, 2000), a brief medical history questionnaire, and the gathering of demographic data.
Significant Others (SOs)
We asked participants for the name of a SO we could interview to corroborate the participant’s self-report. We also asked the SO to contact us if he or she became aware that the participant’s drinking was increasing or that the participant was experiencing new or worsening alcohol-related problems.
Assessment
We chose the following instruments for the baseline and follow-up assessments: the AUDIT (baseline & 12 mo.); the Brief Drinker’s Profile (BDP) which measures quantity/frequency of drinking and drug use, family history, and other risk factors (baseline, 3, 6, & 12 mo.) (Miller & Marlatt, 1987a); the Drinker’s Inventory of Consequences (DrInC) which measures both lifetime and recent (previous 3 months) consequences of drinking (baseline, 3, 6, & 12 mo.) (Miller et al., 1995); the Severity of Alcohol Dependence (community sample) (SADQ-C) which measures symptoms of alcohol dependence (baseline, 6, & 12 mo.) (Stockwell et al., 1994); the Stages of Change and Readiness and Treatment Eagerness Scale (SOCRATES) which measures motivation for change (baseline, 3, 6, & 12 mo.) (Miller & Tonigan,1996); demographic data; and additional questions from the Form 90 (Miller, 1996) that ask about any additional treatment outside of the study they have received during follow-up. Social Support was also assessed at 6 and 12 months using the Interpersonal Support Evaluation List (ISEL) (Cohen, 1985) to examine whether participants’ social resources varied along with drinking outcomes.
The BDP quantity/frequency data allows us to calculate drinks per week, drinks per drinking day, mean peak BACs per week, highest peak BAC per week, and hours of BACs > 80mg% (on the descending curve of the drinking episode). BACs and hours > 80mg% were calculated from the drinking data taking into consideration time spent drinking, gender, and weight.
We collected SO data using the Collateral Interview Form (CIF) (Miller & Marlatt, 1987b). The CIF is a parallel instrument to the BDP for use with collaterals at baseline and follow-up. It is a paper and pencil measure the Research Assistant (RA) used in phone interviews with SOs and subsequently entered into the Drinker’s Evaluation program, a separate web application developed to collect baseline and follow-up data directly from the participants.
Planned interventions & timing
Upon signing the Informed Consent, participants were administered the baseline assessment. While they were answering the baseline questionnaires, the RA scored the AUDIT and assigned the participant to a treatment group based on the randomization schedule discussed below. Once participants completed the baseline assessment the RA informed them of their group assignment.
For the control group, the RA showed participants the resources on the MM web site and helped them sign up for the online support group discussions via the listserv. This also involved helping them set up a separate Google mail account to manage the large amount of email that the MM listserv generates. This concluded the assistance provided to the control group. To receive a minimum dose of exposure we asked participants to read and/or post to the listserv at least twice a week for at least the first 12 weeks of the study.
The experimental group received the same training in using the online MM resources after the baseline assessment. In addition, we gave participants in the experimental group the web site address for accessing the MD web application at home, and then registered them on the site. We asked each group participant to use the MD web application at least once weekly for the first 9 weeks. We originally considered this a sufficient number of sessions and time to be exposed to each of the modules in the MD program, and classified such individuals as having completed treatment. We considered individuals who logged into the program once or twice to not have received a sufficient dose of the intervention. This latter decision was based on the senior author’s clinical experience with using BSCPWIN with clients in the past: three sessions seemed to be the minimum exposure for clients to understand the basic elements of setting goals and self-monitoring their drinking. As the clinical trial progressed, however, participants’ reports of their use of the program at follow-up varied widely. The implications of these varying patterns of use are presented in the Discussion section.
Randomization
Groups were formed by stratified random assignment. Participants were classified into blocks based on the three control factors of gender (male or female), ethnicity (Anglo, Hispanic, or Other), and problem severity as measured by the AUDIT (low [<16] or high [16+]). Within each block, participants were randomly assigned to either the experimental or control group.
Results
Study participant characteristics
Data were available on 80 participants at baseline. These included approximately equal numbers of females (n = 45, 56% of sample) and males (n = 35, 44%). Participants included 63 (79%) non-Hispanic Caucasians, 15 (19%) Hispanics, and 2 (2%) other. Mean age of participants was 50 years, and mean number of years of education was 15. Participants did not differ across groups on demographic variables or, as shown in Table 1, on any of the continuous measures assessed at baseline.
Table 1.
Means of Continuous Measures at Baseline
| Measure | Group | |
|---|---|---|
| MD | MM | |
| Age | 48.7 | 52.1 |
| Education in Years | 15.7 | 15.1 |
| MAST | 14.1 | 13.2 |
| Drinks (SECs)/Week | 33.0 | 35.4 |
| Percent Days Abstinent | 16.3 | 16.2 |
| Mean Drinks per Drinking Day | 5.5 | 6.1 |
| Mean Peak BAC per Drinking Day | 111.2 | 119.5 |
| Hours Over 80 mg | 21.9 | 26.1 |
| DrNC Recent Total | 24.3 | 21.3 |
| AUDIT | 17.7 | 18.3 |
Transformation of skewed variables
Several of the measures of drinking were very positively skewed. In particular, two critical measures of quantity of drinking, Mean Drinks per Drinking Day and Mean Peak BAC for Drinking Days, had skewness at baseline of 2.0 and 2.4, respectively. Certain other variables (e.g. Hours over 80mg% in the previous month) were even more extremely skewed (skewness > 2.5). Thus, such measures were log transformed before analysis. This resulted in reducing the skewness for the log transformation of the baseline variables, such as log Mean Drinks per Drinking Day and log Mean Peak BAC for Drinking Days, to less than 1.0 in absolute value.
Participant flow & follow-ups
Figure 1 summarizes the sample sizes at various stages throughout the study. The overall follow-up rate (69 of 80) was 86%. However, the follow-up rate in the MD group (95%) was substantially higher than that in the MM group (79%), a difference which approached statistical significance (Fisher’s exact p = .051).
Participants lost to follow-up
Comparisons of participants not assessed at 3 months (lost to follow-up, LTF) with those assessed at 3 months suggested that LTFs tended to have more of a binge drinking pattern. The one test of 13 conducted to reach significance at .05 was that for log Mean Peak BAC for Drinking Days, t(78) = 2.59, p = .012. Although tests of differences on baseline variables between LTFs and those who completed the follow-up generally did not reach significance, they had low power given there were only 11 LTFs. The pattern of means suggest that LTFs tended to exhibit a binge drinking typology. That is, they tended to report a higher percentage of days abstinent at baseline (26.7% vs 14.6%), but also tended to report heavier drinking on indicators of binge drinking such as Mean Peak BAC per Drinking Day (167mg% vs. 107mg%), Mean Drinks per Drinking Day (6.6 vs. 5.7), and Hours over 80mg% in the previous month (32.8 vs. 22.7). Thus, in the primary analyses we controlled for binge drinking status using NIAAA’s definition of binge drinking: a mean number of drinks per drinking day of 5 or more for males and of 4 or more for females.
Results of primary analyses
The following results are based on the intent to treat sample. We did compare outcomes of experimental group participants according to whether or not they had received what we considered to be a minimum exposure to the MD program (3 or more sessions) but did not find any differences. Consequently we combined the two groups for analyses. To test our hypotheses regarding alcohol consumption, we considered three dependent measures to be of primary importance: Percent Days Abstinent (PDA), selected in part for its sensitivity to the MD goal of cutting down one’s drinking by reducing the number of days on which one drinks; and two measures of the intensity of drinking on days when participants were not abstinent, namely, log Mean Drinks per Drinking Day, and log Mean Peak BAC for Drinking Days. The DrInC Recent Total score was the sole measure of alcohol-related problems. Thus, the primary analyses involved multivariate tests for alcohol consumption and univariate tests for alcohol problems in a between × within design, with between-subject factors of Treatment Condition and Binge Drinking Status, and a within-subject factor of Time, with all factors having two levels.
Hypothesis 1
The multivariate test of the overall reduction in alcohol consumption averaging across both groups was highly significant, F(3, 63) = 15.84, p < .001, with the univariate tests showing highly significant effects on all three measures: PDA, F(1, 65) = 17.28, p < .001, d = .52; log Mean Drinks per Drinking Day, F(1, 65) = 41.40, p < .001, d =.99; and log Mean BAC per Drinking Day, F(1, 65) = 28.64, p < .001, d = .85. (Effect sizes are computed by dividing differences in means over a pooled standard deviation reflecting between-subject variability, the conservative procedure recommended by Maxwell & Delaney, 2004, pp. 315, 549.) The improvement in PDA was from a mean of 14.5% at Baseline to 27.2% at the 3-month follow-up. Similarly, Mean Drinks per Drinking Day declined from 5.7 to 3.7, and Mean BAC on Drinking Days declined from 107.4mg% to 66.7mg%.
The overall reduction in alcohol-related problems was also highly significant, F(1, 65) =19.37, p < .001, d = .54. The DrInC Recent Total score declined from a mean of 22.70 at baseline to a mean of 16.47 at the 3-month follow-up.
Hypothesis 2
To test our hypothesis #2 regarding effects on alcohol consumption we conducted a multivariate test of the Time × Treatment interaction. This was significant, F(3, 63) = 3.22, p = .029, indicating that the MD + MM interventions resulted in greater improvement over time than did the MM intervention by itself. Univariate tests were significant for PDA F(1, 65) =5.44, p = .023, d = .59; significant for log Mean BAC on Drinking Days, F(1, 65) = 4.62, p = .035, d = .69; and non-significant for log Drinks per Drinking Day, F(1, 65) = 2.00, p = .162, d = .43. Results indicating the form of the two-way Time × Treatment interaction for Percent Days Abstinent are displayed in Figure 2.
Figure 2.
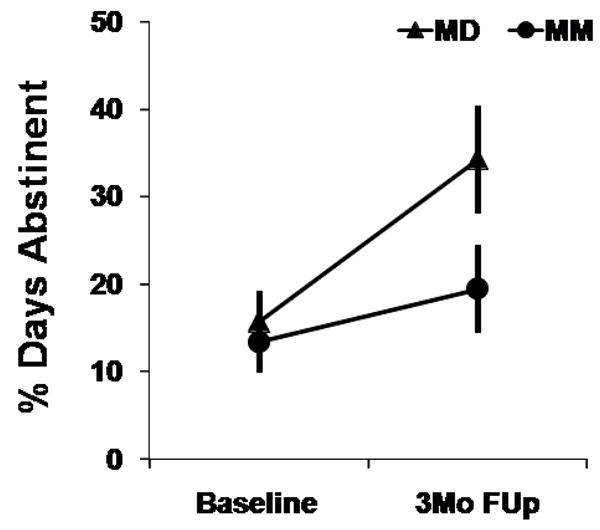
Percent Days Abstinent as a function of Time and Treatment Condition.
For alcohol-related problems the improvement in the MD group over time tended to be greater than that in the MM group. However, the test of the Time × Treatment interaction on the DrInC Recent Total did not reach significance, F(1, 65) =3.48, p = .067, d = .46.
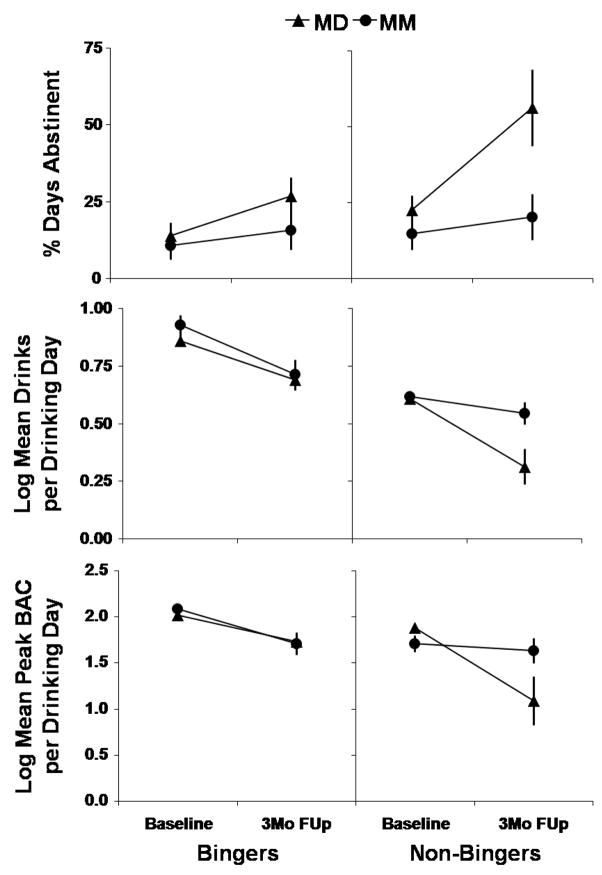
One unanticipated result was that the form of the Time × Treatment interaction differed as a function of Binge Drinking Status. In particular, the multivariate test of the Time × Treatment × Binge Drinking Status three-way interaction was significant for the alcohol consumption variables, F(3, 63) = 2.64, p = .042. The test of this interaction did not reach significance for the DrInC Recent Total, F(1, 65) =1.46, p = .232. On the alcohol-consumption measures, the univariate test was non-significant for PDA, F(1, 65) =1.31, p = .256, but was significant for log Mean Drinks per Drinking Day, F(1, 65) =4.68, p = .034, and highly significant for log Mean BAC per Drinking Day, F(1, 65) =7.81, p = .007. As shown in Figure 3, the form of the three-way interaction was the same for all these consumption measures, namely, the advantage of the experimental group (MD + MM involvement) over the control group (MM involvement only) in promoting improvement over time was much more pronounced for the non-binge drinkers than for the binge drinkers.
Figure 3.
Means as a function of Time, Treatment Condition, and Binge Drinking Status for Percent Days Abstinent (top panel), log Drinks per Drinking Day (middle panel), and log Peak BAC per Drinking Day (bottom panel).
Follow-up tests of the simple two-way Treatment × Time interaction within levels of Binge Drinking indicated that there was no evidence of a difference in amount of improvement over time as a function of Treatment condition for binge drinkers, F’s< 1.0, p’s > .50. On the other hand, for non-binge drinkers, as suggested by Figure 3, the amount of improvement from baseline to the 3 month follow-up was significantly greater for the MD group than for the MM group on all 3 primary alcohol consumption variables: PDA, F(1, 65) = 4.06, p = .048, d = .87; log Mean Drinks per Drinking Day, F(1, 65) = 5.38, p = .024, d = 1.10; and log Mean BAC per Drinking Day, F(1, 65) =9.48, p = .003, d = 1.58.
Significant Others (SOs)
Reports were available from SOs for 75 participants at baseline and for 58 participants at the 3-month follow-up. The pattern of results reported by the SOs was generally in accord with the pattern of self-reports of participants. For example, in terms of Mean Drinks per Drinking Day, the overall mean reported by participants was 5.83 at baseline and 3.54 at follow-up, while for SOs the means were 5.82 and 3.70, respectively. However, correlations between the two sets of reports, while significant, were only moderate in size: r = .343, p = .003 at baseline and r = .305, p = .020 at follow-up. In terms of effects of the factors of Time, Group, and Binge drinking status, the strongest effect for the SOs, like for the participants, was the effect of Time. For example, for log Mean Drinks per Drinking Day, the effect of Time was very highly significant, F(1,54) = 13.21, p = .001. In terms of interactions, the SO data revealed a consistent two-way interaction of Time × Group, F(1,54) = 5.56, p = .022. The form of this interaction was that, for both bingers and non-bingers, the magnitude of improvement from baseline to follow-up was greater for the MD group than for the MM group.
Discussion
These outcome data support both experimental hypotheses: 1. Both groups reduced their consumption and alcohol-related problems relative to baseline levels at follow-up; and 2. The experimental group showed a greater reduction in consumption and a trend towards a greater reduction in alcohol-related problems relative to the control group at follow-up. The magnitude of the reductions in the drinking measures corresponded to medium-to-large effect sizes. In addition the experimental group, compared to the control group, showed even greater reductions in consumption as measured by PDA and log Mean peak BAC per Drinking Day.
These results provide the first scientific evidence from a randomized clinical trial of the potential benefits of the effectiveness of our new web application, Moderate Drinking, when used in conjunction with MM and the resources available online at Moderation Management. It also provides evidence for the effectiveness of the resources MM offers online.
We did not see a clear, positive dose-response relationship between the use of the MD program and outcomes. An analysis of outcomes in the experimental group based on the frequency of logging into the program was non-significant. At one end of the spectrum, some participants who logged in only once or twice had positive outcomes while others did not benefit from their minimal use of the program. Others used the program frequently and had positive outcomes but not all frequent users of the program were successful in reducing their drinking.
The highly varied patterns of use of the MD protocol are to be expected of any self-directed intervention, especially one designed for a clinical issue that may present in such a variety of ways. Unfortunately, this makes it difficult to identify specific mechanisms of change in the application. In order to better understand the pattern of participant use of the MD program, we analyzed outcomes in the experimental group in relation to their use of the various components of the protocol. Within MD, there are 21 modules with material representing the basic components of the BSCT protocol: goal setting, self-monitoring and rate control, as well as some motivational components. Of the 38 participants in the experimental group, 29 actually used the MD application. The average number of modules tapped by those participants who used the site was 8.9, with a trend towards higher number of modules used correlating with better outcomes. The most commonly engaged module involved setting drinking goals (used 22 times), and the next most frequently used components involved gauging one’s chance for success at moderation, and considering “Doing a 30” (used 16 times). In general, motivational components were used relatively frequently, as were components focusing on rate control. Eleven participants entered their self-monitoring of their drinking and received feedback relative to their goals. We will examine these data in more detail once we’ve completed the 12 month follow-ups.
Participant use of Moderation Management resources was not directly monitored during the study. We consciously did this to minimize the assessment burden and to avoid altering what would otherwise be a typical pattern of use. Unfortunately, this makes it difficult to assess precisely which participants in the experimental group benefited more from MM, and which from MD or some combination of the two. Using both monthly email surveys that queried participants about their use of the materials, as well as a structured exit interview at the 12 month follow-up (in progress), we are attempting to further parse the differential use and effects of the two interventions. We will report those findings with the 12 month follow-up results. While this is a limitation of the study, it stems from our choice to maximize external validity. An integration of the two protocols was how we envisioned they would be used in practice.
Another factor that likely affected outcomes was additional assistance participants may have been receiving outside of the study. Twenty-six participants (11 experimental, 15 control) reported seeking help in addition to the interventions in the study: in the experimental group one participant reported attending one Alcoholic Anonymous meeting, eight sought help from some other self-help group, seven went to their doctor about their drinking, six sought help in their social support group and five reported going to their doctor for some other reason. Of the 15 control participants who sought additional help, seven reported attending a self help meeting, two went to their doctors about their drinking, one sought help in their social support network, one entered a RCT of a pharmacological intervention and seven saw their doctor for some other reason.
An unanticipated result emerged from the interaction between participants’ baseline levels of drinking and outcomes in the experimental group. Participants whose drinking, on average, did not meet NIAAA’s definition of binge drinking (5 or more for men, 4 or more for women), had better outcomes in the experimental group which had access to more resources and more opportunities to learn moderate drinking skills. Furthermore, within the experimental group, non-bingers were more likely (7 of 11 or 70%) to participate in 3 or more sessions than were bingers, of whom only 40% (11 of 27) logged into the site 3 or more times.
A consistent finding in the moderate drinking research literature is that those with greater symptoms of dependence benefit less from moderation protocols than do problem drinkers with lower levels of dependence (see Hester, 2003 for a review). This may be the case in our study. Examination of the baseline characteristics of these two groups indicates that the heavier drinking sub-group (that we have labeled Binge Drinkers) had higher mean MAST scores (14.8 vs 11.2, p = .046), and higher scores on the SADQ which measures dependence (4.9 vs. 3.1, p = .037) when compared to the problem drinkers who did not, on average, meet NIAAA’s definition of binge drinking.
Another explanation for this interaction is that there may be a “sleeper” effect in the heavier drinkers that manifests itself in later follow-ups. It may take them longer to acquire the necessary skills to change their drinking. Our 6 and 12 month follow-up data will shed light on this question.
There is a third possible explanation of this interaction between treatment groups and heavy drinking status. As discussed in the Participant flow and follow-up section above, we did see a trend toward better retention in the MD condition, and those lost to follow-up overall tended to be heavier drinkers. Perhaps the interactive nature of the MD program provided more motivation for the less dependent participants who may not think they have as serious a drinking problem as some who are contributing to the MM listserv.
External validity
We expect the results of this study to have high external validity for three reasons. First, the intervention given here will be the same intervention that will be available to future users of both Moderation Management and the Moderate Drinking protocols. Second, a computer-based treatment, by its nature, interacts with users in the same way over time. There is no “drift” from the protocol. From the perspective of this trial, there was no therapist variability in the delivery of the intervention. Third, the study sample was representative of non-treatment seeking and non-dependent, but problematic drinkers based on the baseline measures. This increases the generalizability of our findings. The study sample was diverse, including a large proportion of women (50%) and Hispanics (19%). The study participants were representative of ‘at-risk’ drinkers in that they reported medical conditions and psychological symptoms frequently observed among problem drinking populations.
Limitations
Our study has several limitations. First, it is difficult to determine whether future users of these protocols will have the same level of motivation or commitment that is required of participants entering and following through with a clinical trial. Some future users will come upon the interventions in a more casual fashion, perhaps with as little difficulty as a Google search requires, and may not have the same level of motivation as participants in this clinical trial. In addition, our anecdotal evidence suggested that participating in study follow-ups had some degree of intervention effect. However, since we had neither a delayed assessment nor a no-intervention control group, our conclusions about the effectiveness of MM alone are tempered. These limitations, however, would still not account for the better outcomes in the experimental group.
Another limitation to the generalizability of these results pertains to the general make-up of the study sample. The participants were, on average not only less alcohol dependent, but also somewhat older (M= 50 years) and better educated (M= 15 years of education) than one might expect from a typical sample of problem drinkers. They were also all relatively computer literate. Still, this is the population that has been drawn to MM in the past, and the population we expect to achieve the most benefit from the MD web application in the future.
A fourth limitation of this report is that the data are based on self-report. However, analyses of the collateral data from significant others were correlated and consistent with the findings of overall pre-post changes, and between group differences over time. A final caveat with regards to the current findings is that they are as short-term (3 month) outcomes. It remains to be seen if the significant reductions in drinking and alcohol-related problems, as well as the difference between the groups, persist for the long term. Our expectation, based on past results, is that some drinkers will relapse to heavier drinking, but while others will continue to decrease drinking further and some will become abstinent. We will report these and related outcomes once our 12 month follow-ups are completed.
Footnotes
This research was supported by a Small Business Innovative Research grant from the National Institute of Alcohol Abuse and Alcoholism # R44 AA014305 to the senior author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bock BC, Graham AL, Whiteley JA, Stoddard AL. A review of web-assisted tobacco interventions. Journal of Medical Internet Research. 2008;10 (5):e39. doi: 10.2196/jmir.989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calbring P, Smit F. Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology. 2008;76 (6):1090–1094. doi: 10.1037/a0013603. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, et al. Computer-assisted delivery of cognitive-behavioral therapy for addiction: A randomized trial of CBT4CBT. American Journal of Psychiatry. 2008;165 (7):881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Applications. Dordrecht, The Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- Derogatis LR. BSI-18: Administration, Scoring and Procedures Manual. National Computer Systems, Inc; Minneapolis, MN: 2000. [Google Scholar]
- Foy DW, Nunn BL, Rychtarik Broad-spectrum behavioral treatment for chronic alcoholics: Effects of training controlled drinking skills. Journal of Consulting and Clinical Psychology. 1984;52 (2):218–230. doi: 10.1037//0022-006x.52.2.218. [DOI] [PubMed] [Google Scholar]
- Heather N, Brodie J, Wale S, Wilkinson G, Luce A, Webb E, et al. A randomized controlled trial of moderation-oriented cue exposure. Journal of Studies on Alcohol. 2000;61(4):561–70. doi: 10.15288/jsa.2000.61.561. [DOI] [PubMed] [Google Scholar]
- Hester RK. Self-control training. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches: Effective alternatives. 3. Needham Heights, MA: Allyn & Bacon; 2003. pp. 152–164. [Google Scholar]
- Hester RK, Delaney HD. Behavioral Self-Control Program for Windows: Results of a controlled clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:685–693. doi: 10.1037//0022-006x.65.4.686. [DOI] [PubMed] [Google Scholar]
- Humphries K, Klaw E. Can targeting non-dependent problem drinkers and providing Internet based services expand access to assistance for alcohol problems? Journal of Studies on Alcohol. 2001;62 (4):528–532. doi: 10.15288/jsa.2001.62.528. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Broadening the base of treatment for alcohol problems. Washington, D.C: National Academy Press; 1990. [PubMed] [Google Scholar]
- Klingeman H, Sobell LC, editors. Promoting self-change from addictive behaviors. New York, NY: Springer; 2007. [Google Scholar]
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: A model comparison perspective. Mahwah, NJ: Lawrence Erlbaum; 2000. [Google Scholar]
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: A model comparison perspective. 2. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- Miller WR. Form 90. Project MATCH Monograph Series 5. NIHPubNo. 96–4004 1996 [Google Scholar]
- Miller WR, Wilbourne PL, Hettema JE. What works? A summary of treatment outcome research. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches: Effective alternatives. 3. Needham Heights, MA: Allyn & Bacon; 2003. pp. 13–64. [Google Scholar]
- Miller WR, Leckman AL, Delaney HD, Tinkcom M. Long-term follow-up of behavioral self-control training. Journal of Studies on Alcohol. 1992;53:249–261. doi: 10.15288/jsa.1992.53.249. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual supplement for Brief Drinker’s Profile, Follow-up Drinker Profile, and Collateral Interview Form. 1987a b Retrieved from the Center on Alcoholism, Substance Abuse and Addictions assessments instruments page at http://casaa.unm.edu/inst.html.
- Miller WR, Tonigan S. Assessing drinkers’ motivation for change: The stages of change readiness and treatment eagerness scale (SOCRATES) Psychology of Addictive Behaviors. 1994;10(2):81–89. [Google Scholar]
- Miller WR, Tonigan S, Longabaugh R. The drinker inventory of consequences (DrInC) Project MATCH Monograph Series 4. NIHPubNo. 95–3911 1995 [Google Scholar]
- Miller WR, Wilbourne PL, Hettema JE. What works? A summary of alcohol treatment outcome research. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches: Effective alternatives. 3. Needham Heights, MA: Allyn & Bacon; 2003. pp. 13–63. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Tenth special report to the U.S. Congress on alcohol and health: Highlights from current research. NIH pub no. 00–1583 2000 [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol abuse increases, dependence declines across decade. 2004 Retrieved June 16, 2004 from http://www.niaaa.nih.gov/press/2004/NESARCNews.htm.
- Norman CD, Maley D, Li X, Skinner HA. Using the internet to assist smoking prevention and cessation in schools: A randomized, controlled trial. Health Psychology. 2008;27 (6):799–810. doi: 10.1037/a0013105. [DOI] [PubMed] [Google Scholar]
- Rotgers F, Kern M, Hoeltzel R. Responsible drinking: The path to moderation. Berkeley, CA: New Harbinger; 2003. [Google Scholar]
- SAMSHA. [accessed February 9, 2009];Screening, brief intervention, and referral to treatment. 2007 http://www.sbirt.samhsa.gov/about.htm.
- Sanchez-Craig M, Annis HM, Bornet AR, MacDonald KR. Random assignment to abstinence and controlled drinking: Evaluation of a cognitive-behavioural program for problem drinkers. Journal of Consulting and Clinical Psychology. 1984;52:390–403. doi: 10.1037//0022-006x.52.3.390. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aaasland OB, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol User Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. Am J Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Slosson RL. Slosson Oral Reading Test – Revised. Slosson Educational Publications, Inc; 1990. [Google Scholar]
- Stockwell T, Sitharthan T, McGrath D, Lang E. The measurement of alcohol dependence and impaired control in community samples. Addiction. 1994;89:167–174. doi: 10.1111/j.1360-0443.1994.tb00875.x. [DOI] [PubMed] [Google Scholar]
- Walters ST, Miller E, Chiauzzi E. Wired for wellness: e-Interventions for addressing college drinking . Journal of Substance Abuse Treatment. 2005:139–145. doi: 10.1016/j.jsat.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris T. A controlled trial of web-based feedback for heavy drinking college students. Prevention Science. 2007;82(2):83–88. doi: 10.1007/s11121-006-0059-9. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]