Abstract
Chronic pressure overload (PO) is associated with cardiac hypertrophy and altered autonomic control of cardiac function, in which the latter may involve adaptations in central and/or peripheral cardiac neural control mechanisms. To evaluate the specific remodeling of the intrinsic cardiac nervous system following pressure overload, the descending thoracic aorta artery of the guinea pig was constricted ∼20%, and the animals recovered for 9 wk. Thereafter, atrial neurons of the intrinsic cardiac plexus were isolated for electrophysiological and immunohistochemical analyses. Intracellular voltage recordings from intrinsic cardiac neurons demonstrated no significant changes in passive membrane properties or action potential depolarization compared with age-matched controls and sham-operated animals, but afterhyperpolarization duration was increased in PO animals. Neuronal excitability, as determined by the number of action potentials produced with depolarizing stimuli, was differentially increased in phasic neurons derived from PO animals in response to exogenously applied histamine compared with sham and age-matched controls. Conversely, pituitary adenylate cyclase-activating polypeptide-induced increases in intrinsic cardiac neuron evoked AP frequency were similar between control and PO animals. Immunohistochemical analysis demonstrated a twofold increase in the percentage of neurons immunoreactive for neuronal nitric oxide synthase in PO animals compared with control. The density of mast cells within the intrinsic cardiac plexus from PO animals was also increased twofold compared with preparations from control animals. These results indicate that congestive heart failure associated with chronic pressure overload induces a differential remodeling of intrinsic cardiac neurons and upregulation of neuronal responsiveness to specific neuromodulators.
Keywords: intrinsic cardiac nervous system, histamine, pituitary adenylate cyclase-activating polypeptide, mast cells, nitric oxide synthase, intracellular recording
chronic heart disease induces remodeling of cardiac tissues and the neurohumoral control mechanisms that regulate its function. In response to the stress of chronic pressure overload, the adaptive responses have been well characterized within cardiac myocytes (12, 27, 32, 41) and in the dynamics of collagen matrix reorganization (22, 37), leading to cardiac hypertrophy. However, little attention has been paid to potential changes/remodeling in the peripheral aspects of the intrinsic cardiac nervous system, the final common pathway for control of regional cardiac function (1). During the evolution of cardiac pathology, this nervous system is subject to alterations in neural, circulating, and locally generated signals that have the potential to induce cellular remodeling (2, 3, 15). In that regard, a recent study from our laboratory demonstrated that this intrinsic cardiac plexus demonstrated phenotypic changes and enhanced neuronal excitability following chronic myocardial infarction (21).
The neurons of the intrinsic cardiac plexus integrate information from a variety of sources, including central preganglionic fibers, sensory afferent fibers, local interneurons, sympathetic postganglionic fibers, and local paracrine signals, such as mast cell signals (2, 9, 19, 35, 36, 38). With remodeling, the functional responses of these neurons, including reflex responses to imposed cardiac stress, can be modified, and this can impact disease progression (3, 4, 31). In general, neural adaptive responses that increase heterogeneity in cardiac sympathetic inputs are deleterious (13, 16) and induced changes that augment parasympathetic responses may be protective against hypertrophy, arrhythmia, and sudden cardiac death (11, 18, 24, 40). While both clinical studies in congestive heart failure (CHF) patients (5, 34) and experimental models of CHF (6, 7) indicate diminished indices of parasympathetic function with chronic heart disease, the specific roles of induced changes in central drive (e.g., preganglionic inputs) vs. alterations in peripheral ganglia neuronal integration and function are not well defined.
To evaluate the specific contribution of remodeling of cardiac parasympathetic postganglionic neurons in response to chronic heart disease, the current study examined active and passive electrical properties of the intrinsic cardiac plexus in response to chronic pressure overload induced by aortic constriction. The goal of these experiments was to determine whether the intrinsic cardiac neurons show functional and/or phenotypic alterations associated with the progression into cardiac left ventricular hypertrophy and congestive heart failure. Although several different neuromodulators can modify neuronal excitability of these cells, we focused on specific adaptations in histamine (20, 21) and pituitary adenylate cyclase-activating polypeptide (PACAP) (38, 39) -induced responses.
Within the guinea pig intrinsic cardiac nervous system, the primary source of histamine is cardiac mast cells (35), and chronic heart disease is associated with increased mast cell number and degranulation (22). Histamine increases excitability of intrinsic cardiac neurons via H1-phospholipase C-coupled receptors, leading to opening of nonspecific cation channels and increases in intracellular Ca2+ (20). Release of inflammatory mediators from mast cells has likewise been associated with phenotypic alterations in intrinsic cardiac neurons (e.g., nNOS and iNOS expression; Ref. 21) and at least in the setting of chronic myocardial infarction, an increase in intrinsic cardiac neuronal excitability (21). Therefore, in response to the stress of chronic pressure overload, guinea pig intrinsic cardiac neurons were evaluated for induced changes in neuronal excitability in conjunction with induced changes in mast cell density and NOS expression.
PACAP is colocalized with acetylcholine in virtually all preganglionic neurons innervating the guinea pig intrinsic cardiac ganglia (10). Endogeneous release of PACAP can depolarize and increase excitability of intrinsic cardiac neurons (9, 38), an effect mediated by PAC1 receptors coupled to the hyperpolarization-activated, nonselective cation current Ih (30) via an adenylyl cyclase-dependent signal cascade (39). In consideration of the hypothesized decrease in nicotinic receptor-mediated ganglionic transmission associated with pacing-induced heart failure (6, 7), we also determined whether the heart failure associated with chronic pressure overload altered the functional neuronal responses to PACAP in guinea pig intrinsic cardiac ganglia.
MATERIALS AND METHODS
Animals.
Twenty-two, 9-wk-old, male Hartley guinea pigs (Charles River), weighing between 500 and 650 g, were used in these chronic studies. Nine animals of the same age and weight were used as a time control (sham) surgeries, in which the heart was visualized, but not disturbed. Twenty additional age-matched male Hartley guinea pigs were used for controls. All procedures were approved by the Institutional Animal Care and Use Committees of East Tennessee State University and Ithaca College and were in accordance with the Guide for the Care and Use of Laboratory Animals (National Academy Press, Washington DC, 1996).
Surgical preparation.
Guinea pigs were pretreated with atropine (0.1 mg/kg sc) and ketamine (80 mg/kg ip). Anesthesia was induced with 3% isoflurane via an induction chamber (VetEquip, Pleasanton, CA). Upon removal from the induction chamber, 2.5% isoflurane was delivered via a conical nose cone (VetEquip) until responses to hindlimb toe pinch stimuli had diminished. Following endotracheal intubation, mechanical ventilation was initiated and maintained with a positive pressure ventilator (SAR-830/P ventilator, IITC, Woodland Hills, CA) using 100% O2. Anesthesia was maintained with isoflurane (1–3%). Core body temperature was maintained at 38.5°C with a circulating water heating pad. Buprenorphine (0.05 mg/kg sc) was administered preoperatively.
Animal identification.
An AVID microchip (AVID MicroChip I.D. Systems, Folsom, LA) was injected subcutaneously using a 12-gauge needle into the interscapular space. A MiniTracker (AVID MicroChip I.D. Systems) scanner was then passed over the implant site to detect the unique identification number for each animal.
Induction of chronic pressure overload.
Using aseptic surgical technique, we performed a left thoracotomy along the 2nd-3rd intercostal space, and the descending thoracic aorta was exposed. Uniform constriction of the thoracic aorta was produced by tying a 3–0 surgical ligature tightly around the vessel and a metal tube ranging from 1 to 2 mm external diameter and ∼1 cm length (made from 18-gauge needle) and then removing the tube. An endocath flexible chest tube was placed into the chest cavity from the caudal aspect of the chest cavity. The chest was then closed, residual air withdrawn, and spontaneous ventilation was resumed. Underlying muscle and subcutaneous tissues were closed with 3–0 absorbable suture (dexon, vicryl), and the skin was closed with 3–0 nonabsorbable suture (nylon). The chest tube was then withdrawn. For sham controls, all of the above procedures were duplicated and time matched to the experimental group with the exception that the ligature was not placed, nor tied around the descending thoracic aorta.
Terminal experiments.
Guinea pigs (14–18 wk of age, 800–1000 g at termination, ∼8–9 wk after surgery), were euthanized by CO2 inhalation and exsanguination. The heart was removed, weighed and placed into ice-cold Krebs Ringer solution (mM: NaCl 121, KCl 5.9, CaCl2 2.5, MgCl2 1.2, NaH2PO4 1.2, NaHCO3 25, glucose 8, aerated with 95% O2/5% CO2 for a pH of 7.4). The cardiac plexus, located in the epicardium of the atria, was dissected as previously described (19, 29). This region is located primarily in the wall of the left atria underlying the area of the coronary sinus and was exposed by opening the atria and removing the overlying muscle and connective tissue. The tissue was pinned to a Sylgard-lined 60-mm Petri dish and continuously superfused (6–8 ml/min) with 35–37°C Krebs Ringer. Histamine (10−4 M in Krebs solution; Sigma, St. Louis, MO) and PACAP 1–27 (50 μM in Krebs solution; American Peptides, Sunnyvale, CA) were applied by local pressure ejection (6–9 psi; Picospritzer, General Valve Corporation, Pine Brook, NJ) through small tip diameter (5–10 μm) glass micropipettes positioned 50–100 μm from individual neurons. For multiple tests of responses in the same cell, the cells were allowed to wash with the circulating Krebs solution for several minutes between drug applications.
Electrophysiological methods.
Intracellular voltage recordings from intracardiac neurons were obtained with an AxoClamp 2B amplifier (Axon Instruments, Union City, CA) from cells impaled with 2M KCl-filled microelectrodes (40–80 MΩ). Data were collected, digitized, and analyzed using pClamp 8.2 (Axon Instruments). Individual neurons were used for an experiment if the membrane potential were −40 mV or less and it produced action potentials with an overshoot of at least 20 mV. The neurons were identified as putative parasympathetic postganglionic neurons by their morphology (∼30 μm in diameter) and their basic electrical properties relative to previous studies (17, 19).
Single action potentials were stimulated by positive current injection (0.3–0.7 nA, 5 ms), averaged (5–6 individual recordings), and analyzed to determine the amplitude and duration of the afterhyperpolarizing potential (AHP). Neuronal excitability was monitored by observing the response to a series of long depolarizing current pulses (0.1–0.6 nA, 500 ms). Neurons were categorized as phasic [1–3 action potentials (APs) at the onset of depolarizing stimuli only], or tonic (multiple APs throughout depolarizing stimuli). The AP frequency vs. stimulus amplitude was determined to assess relative changes in excitability.
For each cell, following characterization of the basic electrophysiological properties, induced changes in evoked AP frequency were assessed immediately following 1–2 s application of either histamine (100 μM) or PACAP (50 μm). Each was applied by local pressure ejection, immediately adjacent (∼50–100 μm) to the recorded neuron, and doses were chosen that produce maximal or near-maximal responses (9, 35). Changes in AP frequency vs. stimulus amplitude were determined to assess relative drug-induced changes in excitability for both phasic and tonic intrinsic cardiac neurons derived from control animals vs. animals with chronic pressure overload.
Immunohistochemistry.
Whole mounts of the cardiac ganglion preparations were fixed in Zamboni's (2% paraformaldehyde, 0.1% picric acid) overnight at 4°C. The tissue was then washed in PBS and blocked with 0.3% Triton X-100 and 4% donkey serum prior to incubation with the primary antibodies for 12–18 h at 4°C. Preparations were then washed and incubated with secondary antibodies for 90 min at room temperature. Antibodies used included mouse anti-MAP2 (microtubule associated protein 2, 1:500; Sigma), rabbit anti-nNOS (1:500, Cayman), mouse anti-iNOS (1:100, Transduction Labs), goat anti-ChAT (choline acetyltransferase, 1:100; Chemicon, Temecula, CA), rabbit anti-histamine (1:500; Accurate, Westbury, NY), donkey anti-mouse biotin (1:500), streptavidin-AMCA (1:500), donkey anti-rabbit rhodamine (1:500), donkey anti-goat FITC (1:500), and donkey anti-mouse FITC (1:500, all from Jackson Immunoresearch, West Grove, PA).
The percentage of nNOS cells was determined by counting the total number of either MAP2 or ChAT-immunoreactive cells and then determining the number of nNOS-immunoreactive cells. ChAT was used to label neurons in preparations also stained for iNOS, due to species interactions among the primary antibodies. Using MAP2 and ChAT staining also controlled for the variability in the total number of neurons per preparation, which can vary significantly (29).
Mast cell density was determined by histamine-immunoreactivity. Previous studies have demonstrated that histamine labels mast cells in these tissues (35). The numbers of histamine-immunoreactive cells were determined in three separate fields (∼100 mm2 each) on each preparation. The average number of mast cells/mm2 was determined for each sample.
Analysis of ventricle and lung size.
After removing the atria, the ventricular tissue was immediately fixed in 4% paraformaldehyde for 12–24 h at 4°C and then placed in 70% ethanol at 4°C until processing. Subsequently, the ventricles were weighed and cut into 2-mm-thick slices, parallel to the atrioventricular groove. Outlines of the left ventricular (LV) and right ventricular (RV) chambers at each level were traced onto plastic overlays. These areas were then measured using computer-assisted planimetry (Image Research, St. Catharines, Ontario, Canada). RV and LV areas were calculated by multiplying each area by tissue thickness, and their products were summed and expressed in cm3 (means ± SD) for both ventricles. Lungs were removed, weighed (wet weight), dried, and weighed again (dry weight). Lung weights are expressed as % body wt.
Statistical analysis.
Values are expressed as the mean ± SE. Statistical significance was determined by Students t-test or ANOVA, with a P value less than 0.05 considered significant. Best fit lines for the frequency curves were generated using either a linear or exponential relationship, which provided estimates of the adjusted R2 values.
RESULTS
Analysis of cardiac anatomy and effects of chronic pressure overload.
Chronic pressure overload was induced in 22 guinea pigs by banding of the descending aorta (∼20% constriction). Nine animals died within 48 h of aortic constriction. The remaining 13 animals with pressure overload (PO) were maintained for an average of 9 wk following surgery (Table 1). A subset of 9 animals were used as surgical controls (sham surgeries), in which the aorta was visualized, but undisturbed. To determine the effects of the chronic pressure overload on overall cardiopulmonary function, the weight of the heart and lungs as a percentage of body weight were determined at the termination of the experiment (Table 1). Following termination, the ventricular tissue was also fixed, and sections were analyzed to determine wall thickness. Chronic PO resulted in a significant increase in the heart size and, more specifically, an increase in the left ventricular size compared with sham surgery animals. Left ventricular hypertrophy was observed in the PO hearts, with no significant changes in the size of the right ventricular wall relative to sham control animals. In addition, there was a significant increase in the weights of both wet and dried lung tissues in PO animals compared with controls.
Table 1.
Analysis of tissue changes with chronic pressure overload
| Sham | PO | |
|---|---|---|
| Age at termination, wk | 18.4±1.6 | 18.8±1.7 |
| Postsurgical recovery period, wk | 9.4±1.6 | 9.8±1.8 |
| % Heart weight | 0.66±0.09 | 0.90±0.21* |
| % Wet lung weight | 0.51±0.05 | 0.78±0.21* |
| % Dry lung weight | 0.09±0.01 | 0.16±0.06* |
| LV volume, cm3 | 1.01±0.16 | 1.41±0.30* |
| RV volume, cm3 | 0.19±0.06 | 0.25±0.16 |
| N | 9 | 13 |
Values are expressed as means ± SD. PO, pressure overload; LV, left ventricle; RV, right ventricle.
P < 0.003 vs. Sham.
Passive membrane properties.
Parasympathetic postganglionic neurons of the intrinsic cardiac nervous system were identified on the basis of their relative size (∼30 μm) and their membrane properties (17, 19). A total of 13 PO animals were studied with intracellular recordings obtained from 48 individual cells. Of those, 12 neurons were tonic, or accommodating in nature, firing multiple action potentials during a prolonged depolarizing pulse, while 36 were phasic in nature, firing only one or two action potentials at the onset of depolarizing pulses. Sham-operated animals (n = 9) and age-matched controls (n = 20) showed no differences in any of the parameters tested, and the data from these animals were pooled as control data. A total of 76 neurons from control and sham animals were analyzed. Of these, 21 cells were determined to be tonic (16 neurons from control animals and 5 from sham animals) and 55 were phasic (35 neurons from control animals and 20 from sham animals). There was no significant change in the relative percentage of tonic to phasic neurons in the PO animals compared with controls.
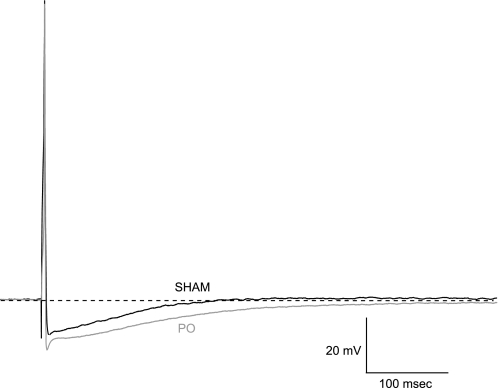
Animals with chronic pressure overload showed no significant changes in resting membrane potential or passive membrane properties (data not shown). However, an analysis of evoked single action potentials showed a significant increase in the duration of the AHP phase of the action potential in PO animals (Fig. 1, mean duration 301 ± 16 ms) compared with neurons from control animals (237 ± 8 ms, P < 0.05). Conversely, the amplitude of the AHP showed no significant change (controls 14.9 ± 0.4 mV; PO 14.5 ± 0.5 mV).
Fig. 1.
Afterhyperpolarizing potential (AHP) duration is increased in neurons from pressure overload-treated (PO) animals. Single action potentials, produced by injection of a brief depolarizing current (0.6 nA, 5 ms), were recorded from intracardiac neurons in both sham (black trace) and PO animals (gray trace). The duration of the afterhyperpolarization phase (AHP) of the action potential was significantly greater in neurons from PO animals. Resting membrane potentials: −52 mV (Sham) and −54 mV (PO).
Effects of neuromodulators on evoked action potential frequency.
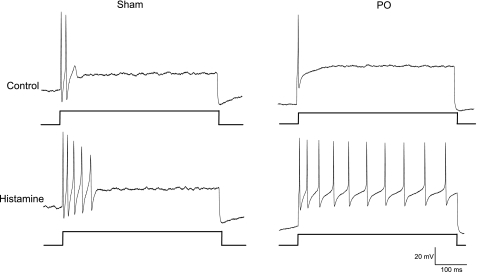
Previous studies have shown that the frequency of APs produced by these neurons in response to prolonged depolarizing stimuli can be regulated by exposure to neuromodulators. Specifically, brief application of histamine to neurons produces a rapidly reversible increase in the frequency of evoked APs (35). In animals with chronic pressure overload, the neuronal response to histamine was enhanced, such that histamine application resulted in a significant increase in the number of action potentials produced in response to depolarization compared with sham surgical animals (Fig. 2).
Fig. 2.
Histamine induces a higher frequency of evoked APs in neurons from animals with chronic pressure overload. Action potentials were produced by injection of long depolarizing currents (500 ms) prior to (top traces) and after (bottom traces) a 1-s application of histamine. The frequency of APs produced in neurons from sham (A) and chronic pressure overload animals (B) prior to histamine application were not different. However, following exogenous application of histamine, the frequency of APs produced in the PO-treated cell was greater than that observed in neurons from sham tissues. Resting membrane potentials: −42 mV sham, −47 mV PO; current stimulation: 0.5 nA sham, 0.4 nA PO.
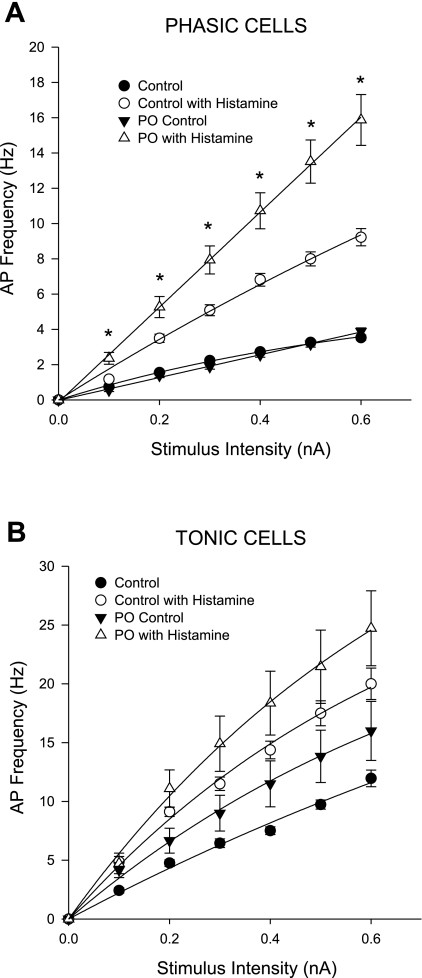
A detailed analysis of the frequency of action potentials produced in response to injection of a series of depolarizing currents in phasic and tonic neurons derived from PO animals was examined in the presence and absence of histamine (Fig. 3). AP frequency responses were indistinguishable between control and PO neurons in the absence of histamine. Application of histamine to control neurons results in a greater AP frequency at each stimulus amplitude in both phasic (Fig. 3A) and tonic (Fig. 3B) neurons. In the PO animals, the histamine-induced increase in AP frequency is significantly greater than the histamine-induced response in control animals at all stimulus amplitudes in the phasic neurons. However, there was no significant change in the AP frequency produced by tonic neurons from PO animals with histamine application compared with controls.
Fig. 3.
Up-regulation of the histamine-induced increase in neuronal excitability is observed in phasic intrinsic cardiac neurons with pressure overload. The frequency of evoked APs (means ± SE) as a function of increasing stimulus intensity (0.1–0.6 nA, 500-ms duration) was determined in intracardiac neurons derived from control and PO models prior to and following histamine application. Data from control (untreated) and sham surgical animals were not significantly different and were pooled. Neurons were categorized as either phasic (A, top) or tonic (B, bottom), based on their firing responses to a prolonged stimulus. There were no significant differences in the frequency of evoked APs in either phasic or tonic cells from PO vs. control tissues prior to histamine application. Histamine application induces a significant increase in AP frequency in both phasic and tonic neurons. However, the histamine-induced increase was significantly greater in phasic neurons from PO tissues compared with the histamine-induced responses in phasic neurons from control preparations. Conversely, there was no significant difference in the histamine-induced responses in the tonic neurons from PO and control preparations. The frequency vs. stimulus curves for the phasic neurons from PO preparations were best fit with a linear equation (R2 > 0.99 for both), while the remaining curves were best with a single exponential curve (R2 > 0.99). Statistical significance was evaluated at each stimulus intensity for a given treatment (i.e., control with histamine vs. PO with histamine) by t-test, *P < 0.05.
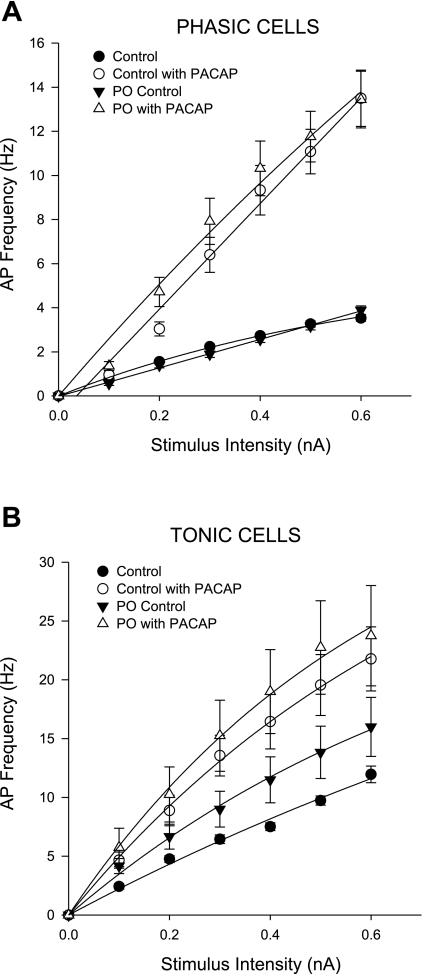
Pituitary adenylate cyclase-activating polypeptide (PACAP) is localized in parasympathetic preganglionic fibers (10) and normally increases the evoked AP frequency in the intrinsic neurons with both exogenous application and preganglionic fiber stimulation (9, 38). In contrast to the results seen with histamine, the ability of PACAP to increase AP frequency was unchanged in neurons from PO animals compared with controls in both phasic and tonic neurons (Fig. 4).
Fig. 4.
The PACAP-induced increase in neuronal excitability is unchanged with pressure overload. Cells from PO preparations showed no change in the responses to exogenous PACAP application compared with control preparations. PACAP application induces an increase in the frequency of evoked APs in both phasic (A, top) and tonic (B, bottom) neurons. There was no significant difference in the frequency of APs produced at increasing stimulus intensities in PO vs. control preparations in the absence of PACAP. Similarly, there were no significant differences in the frequency of APs produced following PACAP application in untreated cells from PO preparations compared with controls. All frequency vs. stimuli curves were best fit with a single exponential curve, with R2 > 0.99.
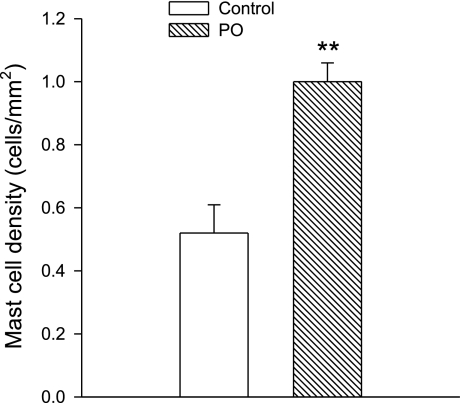
Mast cell density analysis.
Chronic heart disease has been shown to increase cardiac mast cell density (8, 22). Previous studies from our laboratory demonstrated a three-fold increase in mast cell density in the intrinsic cardiac plexus with chronic myocardial infarction (21). To determine whether chronic pressure overload also affects mast cell density, whole mounts of cardiac ganglia were fixed and analyzed with antibody staining for histamine to assess mast cell number. As shown in Fig. 5, the density of mast cells approximately doubled in the tissues from PO animals compared with controls (P < 0.003).
Fig. 5.
Pressure overload induces an increase in mast cell density in the cardiac plexus. Whole mounts of the cardiac plexus from control and pressure overload-treated animals were fixed and stained for immunohistochemical analysis. Mast cell density was determined with antibody labeling for histamine (rabbit anti-histamine, 1:500 and donkey anti-rabbit-Cy3, 1:500). The number of histamine-immunoreactive cells in a 100-mm2 area was determined in five different preparations and the mean ± SD is shown (open bars, control preparations; striped bar, PO preparations). There was a significant (**P < 0.003) increase in mast cell density in the PO tissues.
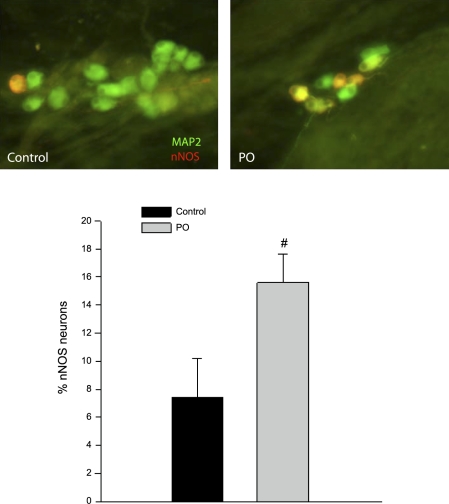
Analysis of nitric oxide synthase expression.
Heart disease induces changes in the expression of nitric oxide synthase (NOS) in both myocytes and neurons (12, 15, 21, 31). Two isoforms of NOS, neuronal NOS (nNOS) and inducible NOS (iNOS), were examined in cardiac ganglia from PO animals. Tissue was examined using immunohistochemical labeling for either microtubule associated protein 2 (MAP2) or choline acetyltransferase (ChAT) (to label all of the neurons) and either nNOS or iNOS. Previous studies have demonstrated that both MAP2 and ChAT staining can be used equally to quantify the number of neurons in a preparation (29). The number of nNOS-immunoreactive neurons expressed as a percentage of the total number of neurons in the tissue showed a twofold increase in the tissue from PO animals compared with controls (P < 0.001, Fig. 6). There was no evidence of iNOS immunoreactivity in any of the PO tissues tested (n = 3, data not shown).
Fig. 6.
PO induces an increase in neuronal nitric oxide synthase (nNOS)-expressing neurons in the cardiac plexus. Whole mounts of the cardiac plexus from control and PO animals were fixed and stained for immunohistochemical analysis. The percentage of nNOS neurons was determined by antibody labeling for nNOS (rabbit anti-nNOS 1:500 and donkey anti-rabbit-Cy3 1:500, red) and MAP2 (mouse anti-MAP2 1:500 and donkey anti-mouse FITC 1:500, green). Neurons with colocalization appear yellow or orange in color. Top: an example of nNOS staining in a control ganglia vs. a ganglia from a PO animal is shown. The percentage of neurons that stained positively for both MAP2 and nNOS was calculated in six preparations from control and PO tissues, and the means ± SD are shown in the bottom panel (black bar, controls; gray bar PO) with a significant increase (#P < 0.001) in the percentage of nNOS cells observed in the PO preparations.
DISCUSSION
The results from this study clearly demonstrate that neurons of the intrinsic cardiac plexus in the guinea pig undergo both phenotypic and functional remodeling with chronic pressure overload. The cells show selective upregulation in their responses to histamine, while responses to another excitatory neuromodulator, PACAP, are unchanged. In addition, there was significant proliferation in cardiac mast cells within the plexus and an increase in the percentage of neurons expressing nNOS.
Chronic pressure overload, induced by banding of the descending dorsal aorta, resulted in significant left ventricular hypertrophy in these animals, with no significant alteration in right ventricular size compared with controls. In addition to the hypertrophy, the PO animals also showed signs of developing cardiac failure, as evidenced by the increase in lung tissue mass. The increased wet/dry lung ratios demonstrate the development of pulmonary edema. Thus, these animals showed significant cardiac stress and were undergoing cellular remodeling in ventricular tissues, as has been described by others (12, 27, 32, 41), along with the remodeling of the intrinsic cardiac nervous system described here.
The physiological recordings from individual neurons in the cardiac ganglion showed no changes in resting membrane properties compared with control or sham surgical animals. The relative number of phasic neurons to tonic neurons was also unchanged. However, single evoked action potentials did show a significant increase in the duration of the afterhyperpolarization in the cells from PO animals. This suggests an underlying change in the ion channels responsible for this portion of the response. The duration of the AHP in guinea pig intracardiac neurons is due primarily to activation of the small, calcium-activated potassium channels (SK channels, 23). Because the activity of SK channels is dependent on the influx of calcium through voltage-gated channels, the observed change is most likely due to either a change in calcium channel function or a change in the potassium channels. PO has been shown to induce functional changes in both calcium and potassium currents in ventricular cells, with increased AP durations due to increases in Ca2+ function (41, 42) and decreases in K+ channel function (27). We observed no change in the amplitude of the AHP in the intrinsic cardiac neurons from PO animals. The amplitude of the AHP in these neurons is due to the activation of large-conductance calcium-activated potassium channels (BK channels, Ref. 23). If the PO-induced alterations were due to changes in calcium channel function, this should produce a concomitant change in both the BK and the SK channel function. Because the difference was only seen in the AHP duration, it suggests that the change is specific to SK channel activity, but further experiments would be needed to confirm this hypothesis. Our previous studies in guinea pigs with chronic myocardial infarction showed no change in AHP durations (21). Thus, the increase in AHP duration appears to be specific to the PO model.
Both histamine and PACAP have been shown to increase the frequency of evoked APs in intrinsic cardiac neurons (9, 35, 38). Neurons from PO animals showed a similar increase in evoked AP frequency following PACAP application to that seen in control animals. However, the frequency of APs was significantly increased following histamine application in the phasic neurons from PO animals compared with controls. Tonic neurons, in contrast, did not show any differences in histamine responses. The ionic mechanisms underlying the histamine-induced responses and the PACAP-induced responses are known to use different ion channels (20, 30), suggesting that the changes observed are due to specific alterations associated with the histamine response pathway. A similar increase in histamine-induced excitability was observed in animals with chronic MI (21). This suggests that cardiac disease may produce a generalized upregulation in the sensitivity of the parasympathetic nervous system to inflammatory signals, such as histamine.
In addition to the physiological changes, there were also significant phenotypic changes within the cardiac plexus. The proliferation of mast cells with chronic heart disease has been previously described (8) and may represent a generalized upregulation in the inflammatory responses within the heart. In ventricular tissues, the increase in cardiac mast cells is thought to contribute to alterations in extracellular matrix through increased activation of collagen degradation pathways (22, 37). In the intrinsic cardiac nervous system, the role of mast cells is less clear, but given their ability to release histamine, a known excitatory neuromodulator, and cytokines that can alter neuronal protein expression (26, 32), they could be a significant stimulus in the overall remodeling response.
The increase in nNOS-expressing neurons is also consistent with previous studies. Although the full functional role of NO in the cardiac neuronal plexus is still unknown, it is thought to potentiate synaptic release at the preganglionic terminals (14, 15, 33). Thus, an increase in NO may also mediate an overall increase in parasympathetic function. Previous studies suggest that an upregulation of NOS with chronic heart disease may be both protective and maladaptive (12, 28). For example, in iNOS knockout mice, remodeling of the left ventricle is exacerbated, and it has been hypothesized that NOS activity may be necessary to reduce overactivation of sympathetic elements (12, 25). In another study, increasing nNOS expression with gene transfection in guinea pigs with acute MI increased ACh release from parasympathetic terminals, suggesting an increase in parasympathetic function (15). Further studies are needed to quantify the specific changes in NOS expression and activity in these chronic heart disease models to evaluate the significance of this potential upregulation.
Perspectives and Significance
The remodeling of the intrinsic cardiac plexus with chronic pressure overload demonstrates a potential protective adaptation within the autonomic nervous system. Enhanced parasympathetic function, in the setting of compromised cardiac function, has been shown to protective against hypertrophy, arrhythmia formation and the risk of sudden cardiac death (18, 24, 40). Yet other studies have suggested that intrinsic cardiac ganglionic function is compromised in congestive heart failure (6). Our results demonstrate changes in intracardiac neuron function that may enhance parasympathetic output, particularly with inflammatory signals. Additionally, the phenotypic changes in nNOS staining and mast cell density may represent a mechanism to facilitate increased parasympathetic postganglionic function. Further experiments are needed to confirm this hypothesis. Taken together, these data suggest that, in addition to alterations in cardiac muscle, chronic stressors can also induce alterations in the integrative control centers that regulate cardiac function.
GRANTS
This work was supported by National Institutes of Health Grants R15 HL60619 to J. Hardwick and HL71830 to J. L. Ardell.
REFERENCES
- 1.Ardell JL Intrathoracic neuronal regulation of cardiac function. In: Basic and Clinical Neurocardiology, edited by Armour JA and Ardell JL. New York: Oxford University, 2004, p. 118–152.
- 2.Armour JA Cardiac neuronal hierarchy in health and disease. Am J Physiol Regul Integr Comp Physiol 287: R262–R271, 2004. [DOI] [PubMed] [Google Scholar]
- 3.Armour JA Potential clinical relevance of the 'little brain' on the mammalian heart. Exp Physiol 93: 165–176, 2008. [DOI] [PubMed] [Google Scholar]
- 4.Arora RC, Cardinal R, Smith FM, Ardell JL, Dell'Italia LJ, Armour JA. Intrinsic cardiac nervous system in tachycardia induced heart failure. Am J Physiol Regul Integr Comp Physiol 285: R1212–R1223, 2003. [DOI] [PubMed] [Google Scholar]
- 5.Azevedo ER, Parker JD. Parasympathetic control of cardiac sympathetic activity: normal ventricle versus congestive heart failure. Circulation 100: 274–279, 1999. [DOI] [PubMed] [Google Scholar]
- 6.Bibevski S, Dunlap ME. Ganglionic mechanisms contribute to diminished vagal control in heart failure. Circulation 99: 2958–2963, 1999. [DOI] [PubMed] [Google Scholar]
- 7.Bibevski S, Dunlap ME. Prevention of diminished parasympathetic control of heart rate in experimental heart failure. Am J Physiol Heart Circ Physiol 287: H1780–H1785, 2004. [DOI] [PubMed] [Google Scholar]
- 8.Bidri M, Féger F, Varadaradjalou S, Hamouda NB, Guillosson JJ, Arock M. Mast cells as a source and target for nitric oxide. Int Immunopharmacol 1: 1543–1558, 2001. [DOI] [PubMed] [Google Scholar]
- 9.Braas KM, May V, Harakall SA, Hardwick JC, Parsons RL. Pituitary adenylate cyclase-activating polypeptide expression and modulation of neuronal excitability in guinea pig cardiac ganglia. J Neurosci 18: 9766–9779, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calupca MA, Vizzard MA, Parsons RL. Origin of pituitary adenylate cyclase-activating polypeptide (PACAP)-immunoreactive fibers innervating guinea pig parasympathetic ganglia. J Comp Neurol 423: 26–39, 2000. [PubMed] [Google Scholar]
- 11.Cardinal R, Ardell JL, Linderoth B, Vermeulen M, Foreman RD, Armour JA. Spinal cord activation differentially modulates ischemic electrical responses to different stressors in canine ventricles. Auton Neurosci Basic Clin 111: 37–47, 2004. [DOI] [PubMed] [Google Scholar]
- 12.Casadei B The emerging role of neuronal nitric oxide synthase in the regulation of myocardial function. Exp Physiol 91: 943–955, 2006. [DOI] [PubMed] [Google Scholar]
- 13.Chen LS, Zhou S, Fishbein MC, Chen PS. New perspectives on the role of autonomic nervous system in the genesis of arrhythmias. J Cardiovas Electrophysiol 18: 123–127, 2007. [DOI] [PubMed] [Google Scholar]
- 14.Choate JK, Danson EJF, Morris JF, Paterson DJ. Peripheral vagal control of heart rate is impaired in neuronal NOS knockout mice. Am J Physiol Heart Circ Physiol 281: H2310–H2317, 2001. [DOI] [PubMed] [Google Scholar]
- 15.Dawson TA, Woodward T, Barber Z, Wang L, Paterson DJ. Cardiac cholinergic NO-cGMP signaling following acute myocardial infarction and nNOS gene transfer. Am J Physiol Heart Circ Physiol 295: H990–H998, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dell'Italia LJ, Ardell JL. Basic and Clinical Neurocardiology, edited by Armour, JA and Ardell JL. New York: Oxford University Press, 2004, p. 340–367.
- 17.Edwards FR, Hirst GDS, Klemm MF, Steele PA. Different types of ganglion cell in the cardiac plexus of guinea-pigs. J Physiol 486: 453–471, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freeling J, Wattier K, LaCroix C, Li YF. Neostigmine and pilocarpine attenuated tumor necrosis factor α expression and cardiac hypertrophy in the heart with pressure overload. Exp Physiol 93: 75–82, 2007. [DOI] [PubMed] [Google Scholar]
- 19.Hardwick JC, Mawe GM, Parsons RL. Evidence for afferent fiber innervation of parasympathetic neurons of the guinea-pig cardiac ganglion. J Auton Nerv Syst 53: 166–174, 1995. [DOI] [PubMed] [Google Scholar]
- 20.Hardwick JC, Kotarski AF, Powers MJ. Ionic mechanisms of histamine-induced responses in guinea pig intracardiac neurons. Am J Physiol Regul Integr Comp Physiol 290: R241–R250, 2006. [DOI] [PubMed] [Google Scholar]
- 21.Hardwick JC, Southerland EM, Ardell JL. Chronic myocardial infarction induces phenotypic and functional remodeling in the guinea pig cardiac plexus. Am J Physiol Regul Integr Comp Physiol 295: R1926–R1933, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janicki JS, Brower GL, Gardiner JD, Forman MF, Steward, JA Jr, Murray DB, Chancey AL. Cardiac mast cell regulation of matrix metalloproteinase-related ventricular remodeling in chronic pressure or volume overload. Cardiovasc Res 69: 657–665, 2006. [DOI] [PubMed] [Google Scholar]
- 23.Jelson GS, DeMasi GM, Sager KL, Hardwick JC. Modulation of guinea pig intrinsic cardiac neurons by prostaglandins. Am J Physiol Regul Integr Comp Physiol 285: R682–R689, 2003. [DOI] [PubMed] [Google Scholar]
- 24.La Rovere MT, Bersano Gnemmi C, Specchia MG, Schwartz PJ. Exercise-induced increase in baroreflex sensitivity predicts improved prognosis after myocardial infarction. Circulation 106: 945–949, 2002. [DOI] [PubMed] [Google Scholar]
- 25.Liu YH, Carretero OA, Cingolani OH, Liao TD, Sun Y, Xu J, Li LY, Pagano PJ, Yang JJ, Yang XP. Role of inducible nitric oxide synthase in cardiac function and remodeling in mice with heart failure due to myocardial infarction. Am J Physiol Heart Circ Physiol 289: H2616–H2623, 2005. [DOI] [PubMed] [Google Scholar]
- 26.Marone G, deCresenzo G, Adt M, Patella V, Arbustini E, Genovese A. Immunological characterization and functional importance of human heart mast cells. Immunopharmacology 31: 1–18, 1995. [DOI] [PubMed] [Google Scholar]
- 27.Marionneau C, Brunet S, Flagg TP, Pilgram TK, Demolombe S, Nerbonne JM. Distinct cellular and molecular mechanisms underlie functional remodeling of repolarizing K+ currents with left ventricular hypertrophy. Circ Res 102: 1406–1415, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Massion PB, Balligand JL. Relevance of nitric oxide for myocardial remodeling. Curr Heart Fail Rep 4: 18–25, 2007. [DOI] [PubMed] [Google Scholar]
- 29.Mawe GM, Talmage EK, Lee KP, Parsons RL. Expression of choline acetyltransferase immunoreactivity in guinea pig cardiac ganglia. Cell Tissue Res 285: 281–286, 1996. [DOI] [PubMed] [Google Scholar]
- 30.Merriam LA, Barstow KL, Parsons RL. Pituitary adenylate cyclase-activating polypeptide enhances the hyperpolarization-activated nonselective cationic conductance, Ih, in dissociated guinea pig intracardiac neurons. Regul Pept 123: 123–133, 2004. [DOI] [PubMed] [Google Scholar]
- 31.Olshansky B, Sabbah HN, Hauptman PJ, Colucci WS. Parasympathetic nervous system and heart failure. Pathophysiology and potential implications for therapy. Circulation 118: 863–871, 2008. [DOI] [PubMed] [Google Scholar]
- 32.Ono K, Matsumori A, Shioi T, Furukawa Y, Sasayama S. Cytokine gene expression after myocardial infarction in rat hearts: Possible implication in left ventricular remodeling. Circulation 98: 149–156, 1998. [DOI] [PubMed] [Google Scholar]
- 33.Paton JF, Kasparaov S, Paterson DJ. Nitric oxide and autonomic control of heart rate: a question of specificity. Trends Neurosci 25: 626–631, 2002. [DOI] [PubMed] [Google Scholar]
- 34.Porter TR, Eckberg DL, Fritsch JM, Rae RF, Beightol LA, Schmedtje JF, Jr, Mohanty PK. Autonomic pathophysiology in heart failure patients. Sympathetic-cholinergic interrelations. J Clin Invest 85: 1362–1371, 1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Powers MJ, Peterson BA, Hardwick JC. Regulation of parasympathetic neurons by mast cells and histamine in the guinea pig heart. Autonom Neurosci 87: 37–45, 2001. [DOI] [PubMed] [Google Scholar]
- 36.Steele PA, Gibbons IL, Morris JL, Mayer B. Multiple populations of neuropeptide-containing neurons in the guinea-pig heart. Neuroscience 62: 241–250, 1994. [DOI] [PubMed] [Google Scholar]
- 37.Stewart JA, Wei CC, Brower GL, Rynders PE, Hankes GH, Dillon AR, Lucchesi PA, Janicki JS, Dell'Italia LJ. Cardiac mast cell- and chymase-mediated matrix metalloproteinase activity and left ventricular remodeling in mitral regurgitation in the dog. J Mol Cell Cardiol, 35: 311–319, 2003. [DOI] [PubMed] [Google Scholar]
- 38.Tompkins JD, Ardell JL, Hoover DB, Parsons RL. Neurally released pituitary adenylate cyclase-activating polypeptide enhances guinea pig intrinsic cardiac neurone excitability. J Physiol 582: 87–93, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tompkins JD, Parsons RL. Identification of intracellular signaling cascades mediating PACAP-induced increase in guinea pig cardiac neuron excitability. J Mol Neurosci 36: 292–298, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vanoli E, Adamson PB, Foreman RD, Schwartz PJ. Prediction of unexpected death among healthy dogs by a novel marker of autonomic neural activity. Heart Rhythm 5: 300–305, 2007. [DOI] [PubMed] [Google Scholar]
- 41.Wang Y, Tandan S, Cheng J, Yang C, Nouyen L, Sugianto J, Johnstone JL, Sun Y, Hill JA. Ca2+/calmodulin-dependent protein kinase II-dependent remodeling of Ca2+ current in pressure overload heart failure. J Biol Chem 28: 25524–25532, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yasui K, Niwa N, Takemura H, Opthol T, Muto T, Horiba M, Shimizu A, Lee JK, Honjo H, Kamiya K, Kodama I. Pathophysiological significance of T-type Ca2+ channels: Expression of T-type Ca2+ channels in fetal and diseased hearts. J Pharm Sci 99: 205–210, 2005. [DOI] [PubMed] [Google Scholar]