Abstract
Background
There is evidence that various meditation practices reduce distress, but little is known about the mechanisms of frequently repeating a mantram—a spiritual word or phrase—on distress reduction. Mantram repetition is the portable practice of focusing attention frequently on a mantram throughout the day without a specific time, place or posture.
Purpose
We examined the hypothesis of whether increases positive reappraisal coping or distancing coping mediated the sustained decreases in anger found following a group-based mantram intervention that was designed to train attention and promote awareness of internal experiences.
Method
A secondary analysis was performed on data collected from a randomized controlled trial that compared a group-based mantram intervention (n=46) to an attention-matched control (n = 47) in a community sample of HIV-positive adults. Positive reappraisal and distancing coping were explored as potential mediators of anger reduction.
Results
Participants in the mantram intervention reported significant increases in positive reappraisal coping over the 5-week intervention period whereas the control group reported decreases. Increases in positive reappraisal coping during the 5-week intervention period mediated the effect of mantram on decreased anger at 22-week follow-up.
Conclusions
Findings suggest that a group-based mantram intervention may reduce anger by enhancing positive reappraisal coping.
Keywords: Acceptance-Based Responding, Anger, Cognitive Coping, HIV Intervention, Meditation, Meta-cognition, Spirituality
There is growing evidence that various group-based meditation interventions reduce perceived stress (Grossman, Niemann, Schmidt & Walach, 2004; Lane, Seskevich & Pieper, 2007; Oman, Hedberg & Thoresen, 2006) and mood disturbance (Speca, Carlson, Goodey & Angen, 2000) in various populations. Meditative techniques are believed to reduce stress in the short-term by initiating the relaxation response, a state of subjective and physiological calm opposite to the fight-or-flight response (Benson, 1983; Benson, 1989; Benson, Beary & Carol, 1974; Benson, Greenwood & Klemchuk, 1975; Jacobs, 2001a, 2001b), but other psychological mechanisms may influence longer-term reductions in distress. Frequently practiced meditation techniques may promote a normalization of the stress response over time (MacLean et al., 1997). In fact, a simple to learn attention focusing strategy like mantram repetition––silently repeating a spiritual word or phrase frequently throughout the day––has been shown to significantly reduce perceived stress (Bormann, Becker et al., 2006; Bormann, Smith et al., 2005; Bormann, Smith, Shively, Dellefield & Gifford, 2007) and symptoms related to posttraumatic stress disorder (PTSD) (Bormann, Thorp, Wetherell & Golshan, 2008). Where individuals may have previously responded reflexively and without awareness, the mantram intervention may slow cognition and allow individuals to attend more fully to a given stressor and their internal responses to that stressor. This increased attention and heightened awareness of one’s cognitive processing that results from repeating a mantram may promote changes in primary appraisals of stressful events or secondary appraisals of resources for coping with those events (Bower, Kemeny, Taylor & Fahey, 1998). Bearing in mind the multiple, uncontrollable stressors inherent in living with human immunodeficiency virus (HIV) infection (Leserman, 2003), the mantram intervention may promote adaptive cognitive coping efforts that have been associated with decreased distress in this population (Carrico et al., 2006b).
Because psychological distress has been associated with decrements in immune status and more rapid HIV disease progression, effectively managing distress such as anger, appears to be an especially salient task for this population (Leserman, 2003). Consequently, a variety of multi-modal stress management interventions have been developed as adjuvant treatments for HIV-positive persons (Antoni, 2003). These stress management interventions are designed to enhance coping skills, improve psychosocial adjustment, and encourage health-promoting behaviors with the hope of attenuating HIV disease progression.
While previous investigations have focused extensively on establishing the efficacy of stress management interventions with HIV-positive persons (Antoni et al., 2006; Chesney, Chambers, Taylor, Johnson & Folkman, 2003; Lechner et al., 2003), isolating the most potent mechanism(s) of distress reduction in these multi-modal treatments is crucial to inform the development of interventions with potentially superior efficacy (Carrico, Antoni, Weaver, Lechner, & Schneiderman, 2005). In prior investigations examining the efficacy of a group-based cognitive behavioral stress management (CBSM) program with HIV-positive gay men, changes in cognitive coping skills were identified as one important pathway for distress reduction. Intervention-related increases in cognitive coping (Carrico et al., 2005; Cruess, Antoni, Kumar & Schneiderman, 2000; Lutgendorf et al., 1997; Lutgendorf et al., 1998) and decreases in cognitive avoidance (Carrico et al., 2006a) may mediate CBSM-related reductions in distress. However, because CBSM is a multi-modal treatment that incorporates both relaxation training and cognitive skills, it is premature to attribute these coping skills changes exclusively to the cognitive-behavioral components of this intervention. In fact, other investigations have highlighted the importance of home relaxation practice as an independent predictor of reductions in distress during CBSM (Cruess et al., 2000; Lutgendorf et al., 1997; Lutgendorf et al., 1998) and increased longevity after the conclusion of this time-limited intervention (Ironson et al., 1994).
It may be that cognitive-behavioral approaches and certain forms of meditation practice share a common change process, meta-cognitive awareness (Teasdale et al., 2002). Rather than changing the content of dysfunctional thoughts, it appears that these treatments may influence distress outcomes by enhancing awareness of one’s relationship to cognitions (Teasdale et al.). By learning to examine cognitive and emotional responses to events in a non-judgmental manner (Grossman et al., 2004; Kabat-Zinn, 2003), individuals may cultivate an enhanced awareness or acknowledgement of internal experiences. This enhanced awareness may provide opportunities for individuals to consider and perform a range of adaptive cognitive-behavioral coping responses to more effectively manage a chronic stressor such as living with HIV infection. For example, previous investigations have observed that this acceptance-based responding is a crucial mechanism whereby substance use disorder treatments achieve positive outcomes (Carrico, Gifford, & Moos, 2007; Gifford, Ritsher, McKellar, & Moos, 2006). It may be that attention-focusing practices, like the mantram intervention alone, are sufficient to raise awareness of alternative options in coping with distress among HIV-positive persons.
Mantram repetition, the practice of silently focusing on a chosen spiritual word or phrase repeated frequently throughout the day (Easwaran, 2001; Oman & Driskill, 2003), has been classified as a form of portable, concentrative meditation (Bormann & Oman, 2007). However, mantram repetition differs from most forms of traditional meditation because it does not require a particular posture, time, or place. It can be repeated almost continuously throughout the day, particularly in emotionally challenging situations (Easwaran). Lending support to this premise, previous studies of the group-based mantram intervention in samples of veterans with chronic illness and/or PTSD and healthcare employees have shown significant reductions in perceived stress, trait-anger and PTSD-related symptoms during the intervention period (Bormann, Becker et al., 2006; Bormann, Oman et al., 2007; Bormann, Smith et al. 2005; Bormann et al., 2008).
Qualitative data further support the efficacy of mantram for reducing trait-anger in both veteran and employee groups (Bormann, Oman, Kemppainen, Becker, Gershwin & Kelly, 2006). Individuals who participated in the group-based mantram intervention indicated that mantram repetition helped them manage a variety of distressing emotions such as “impatience, anger, frustration, upset, disgruntled or feeling out of control” (Bormann, Oman et al., 2006, p. 507). In particular, participants noted that mantram repetition was especially helpful in managing uncontrollable stressors (Bormann, Oman et al.). Thus, it is plausible that this group-based mantram intervention provides participants with an opportunity to develop meta-cognitive skills such as acceptance-based responding that builds the capacity of individuals to cope more effectively in managing the multiple, uncontrollable stressors inherent in living with HIV infection.
In a previously reported study of HIV-positive adults, the group-based mantram repetition intervention reduced trait-anger and enhanced spiritual faith through a 22-week follow-up in comparison to an attention-matched control condition (Bormann, Gifford et al., 2006). For this investigation, based on theoretical and empirical evidence, we conducted a secondary analysis of data that included positive reappraisal coping and trait-anger. We hypothesized that increases in positive reappraisal coping during a 5-week, group-based mantram repetition intervention would mediate sustained reductions in trait-anger through a 22-week follow-up assessment. We also explored distancing as another coping strategy that might explain the effects of mantram on sustained reductions in trait-anger if the mantram intervention served as a distraction (Broderick, 2005; Rusting & Nolen-Hoeksema, 1998). Depression and anxiety were not selected for lack of empirical support from the original study.
Method
Procedure
Data from a previously conducted randomized trial were used (for more detail see Bormann, Gifford et al., 2006). Human subject’s approval was obtained and HIV-positive participants were recruited from 2003 to 2004 using flyers at HIV clinics and community agencies in San Diego, California. Inclusion criteria consisted of being HIV-positive ≥ 6 months, 18 to 65 years old, clean and sober from drug/alcohol abuse for ≥ 6 months, and ability to comprehend English. Exclusion criteria consisted of significant cognitive impairment as evidenced by a score of ≤ 25 on the Mini-Mental Status Exam; presence of a medical condition that affects cortisol levels (e.g., chronic hepatitis); regular use of medications having immunomodulatory effects (e.g., interferon); bereavement in past 3 months; initiating a new alternative/complementary therapy in past 3 months; current practice of other forms of mantram repetition; and acute infection or a recent change in highly active anti-retroviral therapy (HAART) regimen. Ninety-three HIV-positive persons were block randomized based on current prescription for highly active anti-retroviral therapy HAART (yes or no) and T-helper (CD4) cell counts (< 200 or ≥ 200).
Data were collected at baseline, immediately following the group-based mantram intervention (week 5), after a booster session conducted 5 weeks later (week 10), and at 22-week follow-up. Approximately 71% participants completed the 22-week follow-up assessment. This follow-up rate is comparable to those of other randomized controlled trials of stress management interventions for HIV-positive persons (Antoni et al., 2006; Chesney et al., 2003).
Mantram Intervention
The standardized mantram intervention consisted of information on choosing and using a mantram (Bormann, 2005). It was delivered in 5 weekly classes (90-minutes per week) with homework assignments. Participants were given a list of recommended mantrams representing various spiritual traditions (Bormann, 2005), a copy of The Mantram Handbook (Easwaran, 2001), and a course manual with exercises. Other strategies taught to enhance mantram repetition included the practice of one-pointed attention while engaging in one task at a time and intentionally slowing down mentally and behaviorally. Slowing down and mantram repetition together were discussed as a means for making wiser choices, setting priorities, and decreasing stress from hurried behavior. Each group session consisted of (1) time for questions and answers on the material presented; (2) reporting on homework assignments and sharing strategies for using mantram repetition; (3) group exercises to illustrate application of mantram practice, slowing down, or one-pointed attention; (4) 5 minutes of silent, group mantram repetition to raise meta-cognitive awareness of the thinking process or 5 minutes of writing the mantram as an exercise in one-pointed attention; (5) and instructions for homework assignments. After the 5-week mantram intervention, participants received 4 weekly pre-recorded phone call messages reminding them to practice mantram repetition daily. Participants then attended a 90-minute booster session at week ten.
Attention-Matched Control Condition
Participants in the attention-matched control group viewed videotapes on HIV-topics including medications, treatment issues, wasting syndrome, and nutrition. Following the videos, co-facilitators led group discussions meant to provide group interaction and attention similar to the mantram group but without any specific mantram or skills training. Participants attended 90-minute group sessions once a week for 5 weeks. This was followed by automated phone calls from co-facilitators once a week for 4 weeks and a 90-minute booster session at week 10.
Measures
Demographic and Health-related Variables
Gender, age, sexual orientation, race, income, education, employment status, and months since diagnosis of HIV were assessed by questionnaire.
Ways of Coping Scale-Short Form
Positive reappraisal coping and distancing were assessed using the Ways of Coping Scale-SF (Folkman & Lazarus, 1987; Folkman & Lazarus, 1988). Participants were instructed to choose answers that best reflected the extent to which they used various strategies to cope with day-to-day events related to living with HIV infection. The positive reappraisal coping subscale consisted of five items (e.g., “I looked for the ‘silver lining’, so to speak, tried to look on the bright side of things.”). Distancing was assessed by four items (e.g., “Tried to forget the whole thing.”). Items for each subscale were rated on four-point, Likert-type scales ranging from 0 (not used) to 3 (used a great deal). These coping subscales displayed adequate internal consistency (Cronbach’s alpha for positive reappraisal coping was .86 and distancing was .67).
Spielberger Trait-Anger Inventory-Short Form
Trait-anger, instead of state-anger, was chosen because it measures how one generally responds to situations over time and has been used in previous mantram studies. Trait-anger was chosen instead of state-anger which measures feelings at the time of questionnaire administration and therefore, has demonstrated floor-effects (Bormann, Becker et al., 2006; Bormann et al., 2005). Trait-anger was assessed using 10 items (e.g., “When I get mad I say nasty things.”) rated on a 4-point Likert-type scale ranging from 1 (almost never) to 4 (almost always). Concurrent validity has been supported by correlations with measures of hostility, neuroticism, and anxiety (London & Spielberger, 1983; Spielberger, Jacobs, Russel & Crane, 1983). For the present study, this measure displayed good internal consistency (Cronbach’s alpha = .91).
Statistical Analyses
We conducted a series of split-plot, repeated measures analysis of variance (ANOVA) analyses using the principle of intent-to-treat. It was determined that missing data were missing at random. Therefore, multiple imputation procedures using the Expectation-Maximization algorithm in SPSS were applied to assign missing values based on group assignment. The expectation of the likelihood of a missing value was calculated using variables inferred through a mathematical model from variables that were observed; then the maximum likelihood estimates of the parameters were computed by maximizing the expected likelihood found in the first calculation.
As a conservative measure, we replicated the analysis on data without replacing missing values using a group by time mixed-model approach. Both of these methods have been shown to produce comparable parameter estimates and have been determined to be superior to other statistical methods for analyzing longitudinal data (Enders, 2006). We tested for mediation using hierarchical linear regression and the Sobel variance estimate of the mediated effect (Baron & Kenny, 1986; MacKinnon & Dwyer, 1993).
Results
Participant Demographics
A majority of participants were male (81%) and gay/lesbian (52%). Although a majority of participants were non-Hispanic white (52%), a sizeable minority were African American (31%) and Hispanic (15%). Mean age was 42.9 (SD = 6.8) years, and the sample was largely well-educated with 69% of participants having completed at least some college. The majority of participants (62%) reported that they were working at study entry. The modal income reported by 55% of participants was $5,001 to $17,000 per year.
Analyses
As reported by Bormann, Gifford et al. (2006), there was no differential drop-out between the mantram and attention-matched control group. It was determined that participants in the mantram group had been diagnosed with HIV for fewer years (M = 8.4 SD = 5.3) than attention-matched controls (M = 11.1 SD = 6.2), and mantram participants were more likely to be working greater than 20 hours per week (41% vs. 17%). Neither of these demographic variables, however, was related to changes in measures of coping (i.e., positive reappraisal and distancing) or trait-anger over the 22-week investigation (p > .20). There were no baseline differences in positive reappraisal coping or trait-anger between the study conditions (p > .20); however, the attention-matched control participants reported marginally greater use of distancing at baseline (p = .07).
Mantram Effects on Coping and Anger
Over the 5-week, group-based mantram intervention period, a significant group by time interaction for positive reappraisal coping (F (1, 91) = 20.82, p < .01; Cohen’s d = .48) was observed but not for distancing (F (1, 91) = 2.58, p > .10; Cohen’s d = .09). Participants in mantram reported significant increases in positive reappraisal coping over the 5-week intervention period (F (1, 45) = 17.97, p < .01), while those in the attention-matched control reported significant decreases (F (1, 46) = 3.98, p = .05). On average, participants in mantram reported a 25% increase in the use of positive reappraisal coping from baseline. Means and standard deviations for positive reappraisal coping and distancing over the 5-week intervention period are reported in Table 1.
Table 1.
Means and Standard Deviations for Measures of Coping and Anger over Time
| Mantram (n = 46) | Control (n = 47) | |
|---|---|---|
| Positive Reappraisal Coping | ||
| Baseline | 8.0 (4.7) | 9.0 (4.1) |
| 5 Weeks | 10.0 (3.7) | 8.2 (3.9) |
| Distancing Coping | ||
| Baseline | 4.8 (2.5) | 5.8 (2.9) |
| 5 Weeks | 5.2 (2.4) | 5.3 (2.2) |
| Trait-Anger | ||
| Baseline | 19.2 (6.6) | 19.9 (6.8) |
| 5 Weeks | 17.3 (6.0) | 19.5 (6.0) |
| 10 Weeks | 16.8 (4.7) | 19.5 (6.5) |
| 22 Weeks | 16.7 (5.4) | 19.1 (6.5) |
We observed a significant group by time interaction for trait-anger through the 22-week follow-up (F (3, 91) = 2.74, p < .05; Cohen’s d = .41). Participants in mantram reported significant reductions in trait-anger through the 22-week follow-up (F (3, 45) = 10.12, p < .01), while those in the attention-matched control reported no changes (F (3, 46) = 0.88, p > .40). On average, participants in mantram reported a 13% decrease in trait-anger from baseline. Means and standard deviations for trait-anger over the 22-week investigation period are reported in Table 1. We replicated all split-plot repeated measures ANOVA analyses using a mixed-model methodology with data that were not imputed.
Mediation Analyses
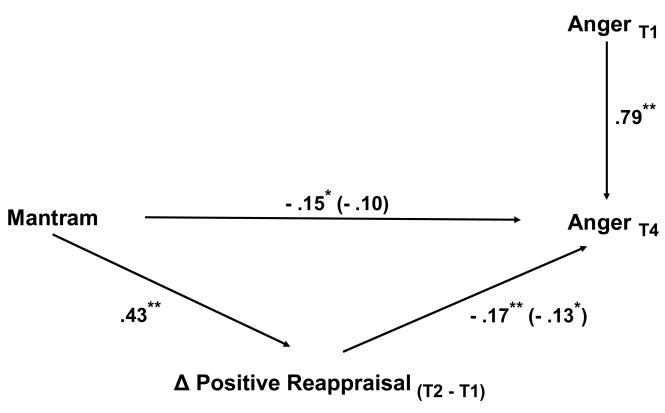
We conducted a series of hierarchical linear regression analyses in order to test whether 5-week changes in positive reappraisal coping (T2-T1) mediated the effect of mantram on lower levels of trait-anger at 22-week follow-up (T4), after controlling for baseline levels of trait-anger (T1). First, we observed that participants in mantram reported increases in positive reappraisal coping over the 5-week intervention period (B = .43, p < .01). Next, we determined that 5-week changes in positive reappraisal coping were a significant predictor of trait-anger at 22-week follow-up, after accounting for baseline values (B = −.17, p < .01). Then, we observed that participants in mantram reported significantly lower levels of trait-anger at 22-week follow-up, after accounting for baseline levels (B = −.15, p < .01). Finally, we regressed trait-anger at 22-week follow-up on baseline levels of trait-anger in the first block, and experimental condition and 5-week changes in positive reappraisal coping were included as predictors in the second block. We observed that the previously significant effect of mantram on lower levels of trait-trait-anger at 22-week follow-up became non-significant (B = −.10, p > .10) while 5-week changes in positive reappraisal coping continued to be a significant predictor (B = −.13, p = .05). Figure 1 summarizes these hierarchical linear regression analyses. Overall, this pattern of results is consistent with mediation. Lending further support to this conclusion, we observed that Sobel’s variance estimate of the indirect effect was marginally significant (Zindirect = 1.81, p = .07).
Figure 1.
Mediation diagram summarizing hierarchical linear regression analyses. *p ≤ .05 **p < .01.
Discussion
Findings from the present investigation indicated that a 5-week mantram intervention reduced trait-anger in HIV-positive persons by enhancing positive reappraisal coping. To our knowledge, this is the first investigation to determine that a mantram intervention may reduce trait-anger by enhancing the utilization of cognitive coping efforts. We did not observe concurrent effects of mantram on use of distancing coping, although participants randomized to the attention-matched control group reported marginally greater use of distancing at baseline and this may have obscured any effect of the mantram intervention. Taken together, however, these findings highlight that the mantram intervention appears to reduce trait-anger by decreasing the likelihood that individuals respond reflexively with anger to a given stressor.
This group-based mantram intervention was designed to promote enhanced attention and awareness that might result in making well-informed choices, setting priorities, and decreasing stress. It may be that mantram practice encourages individuals to attend more fully to various aspects of a stressor and to one’s internal responses, increasing the likelihood of a shift in cognitive appraisals. Consistent with the results of prior investigations of meta-cognitive awareness as a common change process (Teasdale et al., 2002), it appears that the mantram intervention may cultivate meta-cognitive awareness of internal experiences. Thus, mantram may provide individuals with a strategy that assists with examining cognitive and emotional responses to stressors in a non-judgmental, more accepting manner. Where individuals previously might have been quick to react to a negative event with anger, this acceptance-based responding may allow for exploration of a range of potentially adaptive cognitive-behavioral coping responses (Gifford et al., 2006). By learning to more effectively manage feelings of anger, mantram may assist HIV-positive individuals with increasing and maintaining supportive social relationships as well as meeting important treatment-related goals such as achieving adequate levels of adherence to antiretroviral therapy. Although findings from the present study are provocative, further experimental investigations are needed to more carefully examine the effects of the mantram intervention on attention, cognitive processing, and acceptance-based responding. These outcomes should be examined in future investigations.
Because of its simplicity, the mantram intervention has a wide variety of applications (Bormann & Oman, 2007). For example, mantram may assist individuals in managing reactivity in order to derive the maximum benefit from other cognitive-behavioral and coping skills training elements of multi-modal stress management interventions designed for HIV-positive persons. Bearing in mind that anger and interpersonal conflict have also been identified as potent predictors of relapse (Litt, Cooney & Morse, 2000; Witkiewitz & Marlatt, 2004), the mantram intervention may also be an efficacious adjuvant treatment for individuals with substance use disorders. Individuals with active or recent substance abuse were excluded from the present trial, and future trials should examine the efficacy of mantram in more representative samples of HIV-positive persons. Finally, it is also noteworthy that we did not observe concurrent effects of the mantram intervention on depressive symptoms and anxiety despite the fact that participants presented with clinically significant levels at baseline (Bormann, Gifford et al., 2006). This suggests that there may be important aspects of stress management and other psychosocial interventions for HIV-positive persons that reduce depression and anxiety. Because it is a simple, effective strategy for managing feelings of anger, the mantram intervention may assist with retention in these more extensive cognitive-behavioral treatments.
Findings from the present trial must be interpreted in context of some unique strengths and limitations. One strength is that the present trial utilized an attention-matched control condition rather than a wait-list control, thus demonstrating that mantram effects on positive reappraisal coping and anger cannot be explained by differences in contact time or non-specific group support. In terms of limitations, the follow-up rate for this trial was modest, but it is consistent with those reported in other randomized controlled trials of stress management interventions for HIV-positive persons (Antoni et al., 2006; Chesney et al., 2003). Although results of the present investigation suggest a causal chain of events where intervention related increases in positive reappraisal mediate subsequent reductions in distress, this should be replicated in future trials. Taken together, results of the present study provide preliminary support for the efficacy of the mantram intervention and highlight that it may reduce anger by increasing the utilization of cognitive coping skills. These findings support the need for more research on the mantram intervention using larger randomized trials. More intensive interventions that combine group-based mantram intervention with other active treatments may have the most promise.
Acknowledgments
This work was supported by a grant from the NIH/NCCAM (R21AT01159-01A) with additional support from the UCSD General Clinical Research Center (#1637), NIH/National Center for Research Resources (M01RR008), Ruth L. Kirschstein National Research Service Award (T32-MH019391), the San Diego Veterans Medical Research Foundation and the Department of Veterans Affairs, VA San Diego Healthcare System, San Diego, CA.
We acknowledge the contributions of Patricia Bone, BS, RN; Wendy Belding, MA; Ann Kelly, MSN, APRN; Sheryl Becker, MSN, RN; Madeline Gershwin, MA, RN; and Laureen Pada, MSN/MBA, RN for their contributions to study procedures and coordination, and also to Walter Boyle for technical support.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the official views of the Department of Veterans Affairs or the National Center for Complementary and Alternative Medicine, National Institutes of Health.
Contributor Information
Jill E. Bormann, Veterans Affairs San Diego Health Care System, San Diego State University School of Nursing
Adam W. Carrico, University of California, San Francisco
References
- Antoni MH. Stress management and psychoneuroimmunology in HIV infection. CNS Spectrums. 2003;8:40–51. doi: 10.1017/s1092852900023440. [DOI] [PubMed] [Google Scholar]
- Antoni MH. Behavioural interventions and psychoneuroimmunology. In: Vedhara K, Irwin M, editors. Human Psychoneuroimmunology. Oxford, UK: Oxford University Press; 2005. [Google Scholar]
- Antoni MH, Carrico AW, Duran RE, Spitzer S, Penedo F, Ironson G, et al. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosomatic Medicine. 2006;68:143–151. doi: 10.1097/01.psy.0000195749.60049.63. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benson H. The relaxation response: Its subjective and objective historical precedents and physiology. Trends in Neurosciences. 1983;6(7):281–284. [Google Scholar]
- Benson H. The relaxation response and norepinephrine: A new study illuminates mechanisms. Australian Journal of Clinical Hypnotherapy & Hypnosis. 1989;10(2):91–96. [Google Scholar]
- Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37(1):115–120. doi: 10.1080/00332747.1974.11023785. [DOI] [PubMed] [Google Scholar]
- Benson H, Greenwood MM, Klemchuk H. The Relaxation Response: Psychophysiologic aspects and clinical applications. Psychiatry Medicine. 1975;6(1–2):87–98. doi: 10.2190/376W-E4MT-QM6Q-H0UM. [DOI] [PubMed] [Google Scholar]
- Bormann JE. Frequent, silent mantram repetition: A Jacuzzi for the mind. Topics in Emergency Medicine. 2005;27(2):163–166. [Google Scholar]
- Bormann JE, Becker S, Gershwin M, Kelly A, Pada L, Smith TL, Gifford AL. Relationship of frequent mantram repetition to emotional and spiritual well-being in healthcare workers. Journal of Continuing Education in Nursing. 2006;37:218–224. doi: 10.3928/00220124-20060901-02. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Gifford AL, Shively M, Smith TL, Redwine L, Kelly A, Becker S, Gershwin M, Bone P, Belding Effects of spiritual mantram repetition on HIV outcomes: A randomized controlled trial. Journal of Behavioral Medicine. 2006;29:359–376. doi: 10.1007/s10865-006-9063-6. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Oman D. Mantram or holy name repetition: Health benefits from a portable spiritual practice. In: Plante TG, Thoresen C, editors. Spirit, science and health: How the spiritual mind fuels physical wellness. Westport, CT: Praeger; 2007. pp. 94–112. [Google Scholar]
- Bormann JE, OmanDKemppainen JK, Becker S, Gershwin M, Kelly A. Mantram repetition for stress management in veterans and employees: A critical incident study. J Adv Nurs. 2006;53:502–512. doi: 10.1111/j.1365-2648.2006.03752.x. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Smith TL, Becker S, Gershwin M, Pada L, Grudzinski AH, Nurmi E. Efficacy of frequent mantram repetition on stress, quality of life, and spiritual well-being in veterans: A pilot study. Journal of Holistic Nursing. 2005;23:394–413. doi: 10.1177/0898010105278929. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Smith TL, Shively M, Dellefield ME, Gifford AL. Self-monitoring of a stress reduction technique using wrist-worn counters. Journal for Healthcare Quality. 2007;29(1):47–55. doi: 10.1111/j.1945-1474.2007.tb00175.x. [DOI] [PubMed] [Google Scholar]
- Bormann J, Thorp S, Wetherell JL, Golshan S. A spiritually based group intervention for combat veterans with posttraumatic stress disorder: Feasibility study. Journal of Holistic Nursing. 2008;26(2):109–116. doi: 10.1177/0898010107311276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. Journal of Consulting and Clinical Psychology. 1998;66:979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]
- Broderick PC. Mindfulness and coping with dysphoric mood: Contrasts with rumination and distraction. Cognitive Therapy and Research. 2005;29:501–510. [Google Scholar]
- Carrico AW, Antoni MH, Duran RE, Ironson G, Penedo F, Fletcher MA, Klimas N, Schneiderman N. Reductions in depressed mood and denial coping during cognitive behavioral stress management with HIV-positive gay men treated with HAART. Annals of Behavioral Medicine. 2006a;3(2):155–164. doi: 10.1207/s15324796abm3102_7. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Antoni MH, Weaver KE, Lechner SC, Schneiderman N. Cognitive-behavioural stress management with HIV-positive homosexual men: Mechanisms of sustained reductions in depressive symptoms. Chronic Illness. 2005;1:207–215. doi: 10.1177/17423953050010030401. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Gifford EV, Moos RH. Spirituality/religiosity promotes acceptance-based responding and twelve-step involvement. Drug and Alcohol Dependence. 2007 doi: 10.1016/j.drugalcdep.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Ironson G, Antoni MH, Lechner SC, Duran RE, Kumar M, Schneiderman A path model of the effects of spirituality on depressive symptoms and 24-hour urinary-free cortisol in HIV-positive persons. Journal of Psychosomatic Research. 2006b;61(1):51–58. doi: 10.1016/j.jpsychores.2006.04.005. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine. 2003;65:1038–1046. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- Cruess DG, Antoni MH, Kumar M, Schneiderman N. Reductions in salivary cortisol are associated with mood improvement during relaxation training among HIV-seropositive men. Journal of Behavioral Medicine. 2000;23(2):107–121. doi: 10.1023/a:1005419917023. [DOI] [PubMed] [Google Scholar]
- Easwaran E. The mantram handbook. 4. Tomales, CA: Nilgiri Press; 2001. [Google Scholar]
- Enders CK. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosomatic Medicine. 2006;68:427–436. doi: 10.1097/01.psy.0000221275.75056.d8. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Age differences in stress and coping processes. Psychology and Aging. 1987;7:171–184. doi: 10.1037//0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Ways of Coping Questionnaire. Palo Alto, CA: Consulting Psychologists Press; 1988. [Google Scholar]
- Gifford EV, Ritsher JB, McKellar JD, Moos RH. Acceptance and relationship context: A model of substance use disorder treatment outcome. Addiction. 2006;101:1167–1177. doi: 10.1111/j.1360-0443.2006.01506.x. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Ironson G, Friedman A, Klimas N, Antoni M, Fletcher MA, LaPerriere A, Simoneau J, Schneiderman N. Distress, denial, and low adherence to behavioral interventions predict faster disease progression in gay men infected with human immunodeficiency virus. International Journal of Behavioral Medicine. 1994;1(1):90–105. doi: 10.1207/s15327558ijbm0101_6. [DOI] [PubMed] [Google Scholar]
- Jacobs GD. Clinical applications of the relaxation response and mind-body interventions. Journal of Alternative and Complementary Medicine. 2001a;7(Suppl 1):S93–S101. doi: 10.1089/107555301753393850. [DOI] [PubMed] [Google Scholar]
- Jacobs GD. The physiology of mind-body interactions: The stress response and the relaxation response. The Journal of Alternative and Complementary Medicine. 2001b;7(Suppl 1):S83–S92. doi: 10.1089/107555301753393841. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- Lane JD, Seskevich JE, Pieper CF. Brief meditation training can improve perceived stress and negative mood. Alternative Therapies. 2007;31(1):38–44. [PubMed] [Google Scholar]
- Lechner SC, Antoni MH, Lydston D, LaPerriere AIshii M, Devieux J, et al. Cognitive-behavioral interventions improve quality of life in women with AIDS. Journal of Psychosomatic Research. 2003;54:253–261. doi: 10.1016/s0022-3999(02)00480-4. [DOI] [PubMed] [Google Scholar]
- Leserman J. HIV disease progression: Depression, stress, and possible mechanisms. Biological Psychiatry. 2003;54:295–306. doi: 10.1016/s0006-3223(03)00323-8. [DOI] [PubMed] [Google Scholar]
- London P, Spielberger C. Job stress, hassles, and medical risk. American Health, March. 1983:58–63. [Google Scholar]
- Litt MD, Cooney NL, Morse P. Reactivity to alcohol-related stimuli in the laboratory and in the field: Predictors of craving in treated alcoholics. Addiction. 2000;95:889–900. doi: 10.1046/j.1360-0443.2000.9568896.x. [DOI] [PubMed] [Google Scholar]
- Lutgendorf SK, Antoni MH, Ironson G, Klimas N. Cognitive behavioral stress management intervention decreases dysphoria and herpes simplex virus-type 2 titers in symptomatic HIV-seropositive gay men. Journal of Consulting and Clinical Psychology. 1997;65:23–31. doi: 10.1037//0022-006x.65.1.31. [DOI] [PubMed] [Google Scholar]
- Lutgendorf SK, Antoni MH, Ironson G, Starr K, Costello N, Zuckerman M, Klimas N, Fletcher MA, Schneiderman N. Changes in cognitive coping skills and social support during cognitive behavioral stress management intervention and distress outcomes in symptomatic human immunodeficiency virus-seropositive gay men. Psychosomatic Medicine. 1998;60:204–214. doi: 10.1097/00006842-199803000-00017. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- MacLean CR, Walton KG, Wenneberg SR, Levitsky DK, Mandarino JP, Waziri R, et al. Effects of the transcendental meditation program on adaptive mechanisms: Changes in hormone levels and response to stress after 4 months of practice. Psychoneuroendocrinology. 1997;22(4):277–295. doi: 10.1016/s0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- Oman D, Driskill JD. Holy name repetition as a spiritual exercise and therapeutic technique. Journal of Psychological Christianit. 2003;22:5–19. [Google Scholar]
- Oman D, Hedberg J, Thoresen CE. Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:714–719. doi: 10.1037/0022-006X.74.4.714. [DOI] [PubMed] [Google Scholar]
- Rusting CL, Nolen-Hoeksema S. Regulating responses to anger: Effects of rumination and distraction on angry mood. Journal of Personality and Social Psychology. 1998;74:790–803. doi: 10.1037//0022-3514.74.3.790. [DOI] [PubMed] [Google Scholar]
- Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine. 2000;62:613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Jacobs G, Russel S, Crane R. Assessment of anger: The state-trait anger scale. In: Butcher JN, Spielberger CD, editors. Advances in Personality Assessment. Vol. 2. Hillsdale, N. J: Lawrence Erlbaum Associates, Inc; 1983. pp. 159–187. [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was then, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]