Abstract
Objective
To assess the contributions of both microbial larvicides and insecticide-treated nets (ITNs) in terms of reducing malaria incidence in an integrated vector management programme in an area moderately endemic for malaria in the western Kenyan highlands.
Methods
A pre-post, control group design was used. Larval and adult vector populations were surveyed weekly in six separate valley communities. The incidence of Plasmodium infections in children 6 months to 13 years of age was measured during the long and short rainy seasons each year. Baseline data were collected for 17 months, after which Bacillus-based larvicides were applied weekly to aquatic habitats in three of the valleys for another 19 months. At around the same time the larviciding was initiated, ITNs were introduced gradually into all study communities by the National Malaria Control Programme. The effect of larviciding, ITNs and other determinants of malaria risk was assessed by means of generalized estimating equations.
Findings
The risk of acquiring new parasite infections in children was substantially and independently reduced by ITN use (odds ratio, OR: 0.69; 95% confidence interval, CI: 0.48–0.99) and larvicide application (OR: 0.44; 95% CI: 0.23–0.82), after adjusting for confounders.
Conclusion
Vector control with microbial larvicides enhanced the malaria control achieved with ITNs alone. Anti-larval measures are a promising complement to ITN distribution in the economically important highland areas and similar transmission settings in Africa.
Résumé
Objectif
Évaluer les contributions des larvicides microbiens et des moustiquaires imprégnées d’insecticide (MII) à la réduction de l’incidence du paludisme dans le cadre d’un programme de lutte antivectorielle intégrée, appliqué à une zone d’endémie modérée de cette maladie, dans les hauts plateaux du Kenya occidental.
Méthodes
On a fait appel à une étude de type avant-après avec groupe témoin. On a surveillé chaque semaine les populations de larves et de vecteurs adultes menaçant les communautés vivant dans six vallées séparées. On a mesuré chaque année l’incidence des infections à Plasmodium chez les enfants de 6 mois à 13 ans au cours des deux saisons des pluies (longue et courte). On a collecté des donnée de référence pendant 17 mois, après quoi on appliqué chaque semaine des larvicides à base de Bacillus sur les habitats aquatiques de trois des vallées pendant 19 autres mois. En même temps à peu près que débutait la destruction des larves, le Programme kenyan de lutte contre le paludisme a commencé à introduire progressivement des MII dans toutes les communautés étudiées. Les effets de la destruction larvaire, des MII et d’autres déterminants du risque de paludisme ont été évalués à l’aide d’équations d’estimation généralisée.
Résultats
Après ajustement pour les facteurs de confusion, le risque de contracter une nouvelle infestation parasitaire chez l’enfant était substantiellement et indépendamment réduit par l’utilisation de MII (Odds ratio, OR : 0,69, intervalle de confiance à 95 %, IC : 0,48-0,99) et par l’application de larvicide (OR : 0,44 ; IC à 95 % : 0,23-0,82).
Conclusion
La lutte antivectorielle par application de larvicides microbiens a permis de renforcer les résultats obtenus contre le paludisme avec les MII seules. Les mesures de lutte antilarvaire représentent un complément prometteur à la distribution de MII dans les zones importantes sur le plan économique des hauts plateaux et dans d’autres contextes similaires en Afrique où se transmet actuellement le paludisme.
Resumen
Objetivo
Determinar la contribución de los larvicidas microbianos y los mosquiteros tratados con insecticida (MTI) a la reducción de la incidencia de malaria en un programa de lucha antivectorial integrada emprendido en una zona con malaria moderadamente endémica de las tierras altas del oeste de Kenya.
Métodos
Se llevó a cabo un estudio pre-post con un grupo de control en el que se procedió a vigilar las poblaciones de larvas y vectores adultos en las comunidades de seis valles. Anualmente se midió la incidencia de infección por Plasmodium en los niños de 6 meses a 13 años durante cada estación de las lluvias cortas y largas. Se reunieron datos de referencia por espacio de 17 meses, tras lo cual se procedió a aplicar todas las semanas larvicidas basados en Bacillus en hábitats acuáticos en tres de los valles durante otros 19 meses. Aproximadamente al mismo tiempo que se iniciaba la aplicación de larvicidas, el Programa Nacional de Control de la Malaria comenzó también a introducir gradualmente los MTI en todas las comunidades estudiadas. El efecto de los larvicidas, los MTI y otros determinantes del riesgo de malaria se evaluó mediante ecuaciones de estimación generalizadas.
Resultados
El riesgo de los niños de contraer nuevas infecciones por el parásito se vio reducido de forma sustancial e independiente por el uso de MTI (razón de posibilidades, OR: 0,69; intervalo de confianza [IC] del 95%: 0,48–0,99) y por la aplicación de larvicidas (OR: 0,44; IC95%: 0,23–0,82), después de ajustar por los factores de confusión.
Conclusión
La lucha antivectorial con larvicidas microbianos potenció el control de la malaria logrado solo con MTI. Las medidas antilarvarias son un complemento prometedor de la distribución de MTI en las zonas montañosas económicamente importantes y otros entornos de transmisión similares en África.
ملخص
الهدف
تقييم إسهامات المبيدات المكروبية لليرقات، والناموسيات المعالجة بمبيدات الحشرات، من حيث تقليل وقوعات الملاريا، ضمن برنامج التدبير الصحي المتكامل للنواقل، في منطقة تتوطَّنها الملاريا بشكل متوسط، في المرتفعات الغربية بكينيا.
الطريقة
استخدم الباحثون أسلوب المجموعة المضبَّطة السابقة التعيين. وتم مسح تجمعات اليرقات والنواقل البالغة، بصورة أسبوعية، في ستة مجتمعات محلية منفصلة تقطن في الوديان. وقيست وقوعات العدوى بالمتصورات بين الأطفال بين عمر 6 أشهر و13 عاماً، أثناء المواسم الممطرة الطويلة والقصيرة، في كل عام. وجمعت بيانات خط الأساس على مدى 17 شهراً، وبعدها تم وضع مبيدات اليرقات العصوية القاعدة، بصورة أسبوعية، في الموائل المائية، في ثلاثة من الوديان، على مدى 19 شهراً أخرى. وتم في نفس الوقت تقريباً الشروع في إبادة اليرقات. وأدخلت الناموسيات المعالجة بالمبيدات الحشرية تدريجياً إلى جميع المجتمعات المحلية الخاضعة للدراسة، وذلك من قِبَل البرنامج الوطني لمكافحة الملاريا. وتم تقييم عملية إبادة اليرقات، واستخدام الناموسيات المعالجة، وغيرها من محددات مخاطر الملاريا، باستخدام المعدلات التقديرية التعميمية.
الموجودات
أمكن تقليل مخاطر اكتساب عدوى طفيلية جديدة لدى الأطفال بشكل كبير، وبصورة مستقلة باستخدام الناموسيات المعالجة (نسبة الاحتمال 0.69؛ 95%، بفاصل ثقة 0.48 – 0.99)، وباستخدام مبيدات اليرقات (نسبة الاحتمال 0.44؛ 95%، بفاصل ثقة 0.23 – 0.82) بعد عمل التعديل المتعلق بعوامل الإرباك.
الاستنتاج
عززت مكافحة النواقل باستخدام المبيدات المكروبية لليرقات من نتائج المكافحة التي تحققت باستخدام الناموسيات المعالجة وحدها. وتعد التدابير المضادة لليرقات تدابير واعدة، تكمِّل عملية توزيع الناموسيات المعالجة في مناطق المرتفعات ذات الأهمية الاقتصادية، وأماكن الانتشار المشابهة في أفريقيا.
Introduction
A marked increase in malaria has recently been noted in the African highlands, largely due to the rise of drug-resistant strains of Plasmodium falciparum parasites.1–4 The ecological features of the western highlands of Kenya support stable parasite transmission, and increasing population pressure has led to the clearance of natural swamps, massive deforestation and crop cultivation in the valley bottoms.5,6 Because of these agricultural changes, many water bodies are now exposed to the sun and provide ideal conditions for vector proliferation and increased malaria transmission.7 Malaria control in these highlands is based on insecticide-treated nets (ITNs), indoor-residual spraying (IRS) with insecticides and prompt and effective treatment of clinical malaria.8 Many believe integrated vector management (IVM), targeting both larval and adult mosquitoes, is the future for malaria control.9–11 While ITNs are currently the priority strategy, there is growing interest in attacking the aquatic stages of malaria vectors with microbial larvicides, in conjunction with environmental management.5,6,12–21 Presently, microbial larvicides are being used in an operational context only in Dar es Salaam, in the United Republic of Tanzania.22,23 However, in the future larvicide application will be expanded to many of the 15 countries included in the President’s Malaria Initiative and this interest is likely to spread to other African countries. While IVM is often advocated,10,11 there is little evidence from the recent scientific literature on the effectiveness of this approach.
We have demonstrated that microbial larvicides reduced malaria vector mosquito larvae and adult females by > 90% in a rural town in western Kenya.19 However, the effectiveness of this approach for reducing the incidence of malaria among vulnerable children remains unproven. ITNs are a firm favourite in the armamentarium against malaria and their protective efficacy is well known,24,25 with reductions of 40–70% in human mosquito biting rates.23,26 In this study we used a “pre-test/post-test control group” design to investigate the contributions of both mosquito larval control with microbials and ITNs to reducing the burden of malaria in the Kakamega and Vihiga highlands of western Kenya, an area moderately endemic for the disease.27
Methods
Study area
Six highland valley communities (at an altitude of 1453–1632 m) were recruited in two densely populated districts in Kenya28 (Table 1). These hilly areas were characterized by steep-sided valleys with flat bottoms and plateaus, where most homes were built. Small streams ran along the valley bottoms and papyrus swamps were common. Valleys were approximately 2–4 km² in area and at least 1 km apart. Baseline entomological and clinical data were collected for 17 months (February 2004 to June 2005), after which microbial larvicide was applied to all aquatic habitats in three of the six study sites at weekly intervals for a further 19 months (July 2005 to January 2007). At the same time, larviciding was initiated by project staff in half the sites (Table 1) and ITNs were gradually introduced in all study communities by the National Malaria Control Programme through government health facilities and nongovernmental organizations (NGOs).
Table 1. Study site characteristics before a malaria mosquito larval control intervention (February 2004 to June 2005) in intervention and non-intervention groups, Kenya.
| Valleya | District | Mean altitude, in m | Longitude | Latitude | Average no. of aquatic habitats (95% CI) | Average % of habitats with late instar Anopheles (95% CI) | Average no. of Anopheles adults per house (95% CI) | Average P. falciparum prevalence, in % (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Non-LCI group | ||||||||
| Kimingini | Kakamega | 1453 | 34.7606 | 0.171193 | 123.3 | 13.1 | 0.8 | 39.6 |
| (107.4–139.3) | (10.6–15.6) | (0.41–1.29) | (35.5–43.7) | |||||
| Emutete | Vihiga | 1522 | 34.6358 | 0.025958 | 232.7 | 12.1 | 4.21 | 44.3 |
| (191.7–273.8) | (7.6–16.5) | (3.11–5.60) | (40.0–48.6) | |||||
| Wakikuyu | Vihiga | 1576 | 34.7699 | 0.108041 | 44.4 | 23 | 0.62 | 39.6 |
| (39.8–49.1) | (14.5–31.6) | (0.37–0.92) | (35.6–43.6) | |||||
| Averages of pooled data (non-LCI) | 133.5 | 17.3 | 1.48 | 48.0 | ||||
| (107.8–159.4) | (14.4–20.3) | (1.06–1.99) | (45.6–50.4) | |||||
| LCI-group | ||||||||
| Musilongo | Vihiga | 1492 | 34.6035 | 0.020763 | 149.4 | 21 | 3.92 | 63.9 |
| (127.5–171.2) | (12.8–29.3) | (2.42–6.07) | (59.8–68.0) | |||||
| Kezege | Vihiga | 1545 | 34.6506 | 0.026348 | 251.2 | 17.4 | 1.61 | 55.2 |
| (221.3–281.0) | (13.8–21.0) | (1.10–2.25) | (51.0–59.4) | |||||
| Wamondo | Vihiga | 1632 | 34.7011 | 0.026763 | 81.9 | 13.6 | 0.38 | 26.1 |
| (74.2–89.6) | (11.8–15.5) | (0.24–0.53) | (22.4–29.8) | |||||
| Averages of pooled data (LCI) | 160.8 | 16.1 | 1.61 | 48.3 | ||||
| (137.9–183.8) | (12.7–19.4) | (1.14–2.18) | (45.9–50.7) | |||||
CI, confidence interval; LCI, larval control intervention; P. falciparum, Plasmodium falciparum. a Study valleys were divided into two groups so that the averages of their pooled data were similar. Of the two groups, one was chosen for LCI and the other served as a control (non-LCI). Musilongo, Kezege and Wamondo received weekly larvicide applications from July 2005 to January 2007.
After baseline monitoring, three valleys were selected for Group 1, the larval control intervention (LCI), and another three for Group 2, the non-LCI group. Since the study valleys varied considerably in their entomological and epidemiological characteristics, the sites were grouped so that at baseline both groups were similar in the total number of aquatic habitats, the proportion of available habitats colonized by Anopheles larvae, the density and seasonality of adult mosquito household infestation, and malaria prevalence (Table 1). Group 2 was chosen as the control because one of the sites in the group bordered a malaria study site of the Kenya Medical Research Institute and we were afraid that treatment in our site would interfere with malaria transmission in the neighbouring site.
Eligibility criteria
Children between 6 months and 10 years of age were enrolled in the study because their complete or partial lack of protective immunity against malaria put them at the greatest risk. A census of resident children in this age group was carried out in all six study valleys in March 2004 (between 120 and 163 children were in each site, total n = 843). A cohort of 120 children was randomly selected from each study site (720 children out of 843) according to a computer-generated randomization list. Informed consent for enrolment was obtained from all selected participants or their guardians.
Interventions
Insecticide-treated nets
From 2005 onwards, ITNs were intensively promoted and supplied by government health facilities and NGOs. In addition, in July and August 2006, joint measles–malaria campaigns combining the distribution of ITNs with measles vaccinations were conducted.29,30 The nets were treated mainly with long-lasting insecticides (PermaNet®, Vestergaard Frandsen, Lausanne, Switzerland; Olyset®, Sumitomo Chemical, Tokyo, Japan). ITN use was recorded in sentinel households where adult mosquitoes were collected and during cross-sectional clinical surveys.
Larviciding
Water-dispersible and granule formulations of the commercial strains of Bacillus sphaericus or B. thuringiensis var. israelensis (Valent BioSciences Corporation, United States of America) were applied to three of the six valleys beginning in July 2005. B. sphaericus was used for the first 6 months of the intervention but for lack of a residual effect, it was replaced with B. thuringiensis var. israelensisi, which is cheaper and forestalls the development of resistance due to its more complex mode of action.31 Larvicide was applied to all water bodies at weekly intervals.
Objectives and measures
To assess the contributions of both microbial larvicides and ITNs in decreasing malaria transmission and infection in an integrated vector management programme we used the incidence of new Plasmodium infections in children as the primary outcome, and anopheline larval and adult abundance as secondary outcomes.
Larval vector abundance
Larval surveys were carried out weekly in all valleys. The presence or absence of anopheline and culicine larvae was recorded in all aquatic habitats. Purposive dipping was used to sample larvae (10 dips per site).19 Larvae were categorised as early stage (first and second instars) and late stage (third and fourth instars). In 10 randomly selected sentinel sites per valley, weekly larval densities (average number of larvae per dip per habitat) were recorded and the proportion of late instar larvae was calculated as an indicator of larval survival and emergence.
Adult vector abundance
Indoor-resting mosquitoes were collected monthly using pyrethrum spray collections from 10 sentinel houses in each valley32 that were randomly selected from households within 500 m of the valley bottom, where most breeding occurs. These households were likely to have the greatest numbers of vectors.33 The type of household, the number of occupants during the night before, and the mosquito control methods used were recorded routinely. Anopheles gambiae sensu lato (s.l.) were identified to the species level using polymerase chain reaction, and the presence of sporozoites was determined by enzyme-linked immunosorbent assay (ELISA) of pooled samples of 10 mosquitoes per test.34,35
Malaria parasitaemia
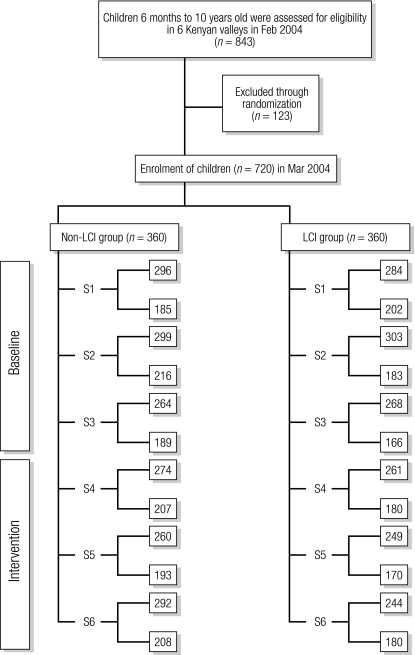
The incidence of new parasite infections was measured during the long rains (April–June) and short rains (November–January) each year, when transmission was likely to be highest. On each occasion two surveys were carried out 2 months apart. Thus, parasite infection status was assessed during six consecutive rainy seasons (S1-S3 at baseline, S4-S6 during the intervention; Fig. 1) from April 2004 to January 2007. A short history of each child’s health and of mosquito control at their home (use of ITN, coil or insecticide spray) was recorded at each survey. Rapid malaria tests (OptiMal®, DiaMed, Cressier, Switzerland) were used to determine whether the children had malaria parasites or not. Thick and thin blood smears were obtained for microscopic parasite identification and determination of parasite density. Children with parasites, as indicated by the rapid test, were treated with the first line drug recommended by the Government of Kenya. Sulfadoxine-pyrimethamine (Fansidar®, F Hoffmann-La Roche Ltd., Basel, Switzerland) was administered in the first season (S1: April–June 2004), and artemether–lumefantrin combination therapy (Coartem®, Novartis, Basel, Switzerland), thereafter (S2-S6: November 2004 to January 2007).
Fig. 1.
Profile of pre–post intervention trial for assessing the effects of larviciding, ITNs and other factors affecting malaria risk, Kenya, 2004–2007
ITN, insecticide-treated net; LCI, larval control intervention; S1–S6, six consecutive rainy season surveys each consisting of two visits.
Sample size
This study was designed to determine the level of transmission and intensity of infection in the study area. No prior information about the level of infection in children was available, but we assumed it varied from 40% to 60%. To detect a 33% reduction in infection associated with an intervention, we required a sample size of 107–214 children in each group, at a 5% level of significance and 80% power.
Blinding
Entomological data collection was not blinded to the assignment of mosquito larval control interventions in the study areas. Residents were aware of ongoing interventions. The reading of blood films and ELISA tests was blinded.
Protection of human subject
Institutional and ethical clearance was granted by the ethical review committee of the Kenya Medical Research Institute and by Durham University, in the United Kingdom. Interviews and malaria parasite screening were only started after the purpose of the study had been clearly explained to the participants and parents or guardians of children and an informed consent form had been read and signed. A research and import permit for the use of microbial larvicides was granted by the Kenyan Pest Control Products Board.
Statistical analysis
Children with no parasites at the first cross-sectional survey of the season who had become infected 2 months later were used to calculate the incidence rate of new parasite infections over the 2-month follow-up period.
General estimating equations were used to evaluate the determinants of all outcome measures. If the outcome measure was binary, a binomial distribution with a logit link function was fitted. For count data a logarithmic link function and a normal distribution were used. A first-order autoregressive relationship was chosen for all repeated measurements. Active larviciding and ITN use were treated as categorical independent variables in the model evaluating the impact of these control measures on adult mosquito density and human parasitaemia. The valleys were treated as the unit of geographic location and included as confounders in the model.
General estimating equations were also used to calculate differences in mean Anopheles larval and adult densities, Anopheles human biting rate (average number of bloodfed female mosquitoes per person per sampling date) and entomological inoculation rate (EIR; mean number of infectious bites per person per year)36 between intervention and non-intervention areas. Analyses of the incidence of newly-acquired parasite infections (new cases per child month at risk) were performed, and rate ratios were calculated; 95% confidence intervals (CIs) were determined.37 All analyses were carried out using SPSS 15 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Participants and baseline demographics
Fig. 1 shows the number of children screened at the start of each rainy season survey and followed up 2 months later. In all cases absence from a survey was because the child was travelling. The sex ratio was approximately 1:1 in all surveys. The average age of children in LCI and non-LCI groups was similar.
ITN use
Gradually increasing ITN use in the study communities was observed during the mosquito collections in sentinel houses and during the cross-sectional malaria surveys. ITN use in sentinel households increased from 4·8% (95% CI: 3.0–6.6; range in non-LCI valleys 1–9% and in LCI valleys 2–6%) at baseline to 40.8% (95% CI: 36.7–45.0; range in non-LCI valleys 24–51% and in LCI valleys 25–51%) during the intervention year. The probability that ITNs were used was the same in the non-LCI and LCI group (odds ratio, OR: 1.06, 95% CI: 0.56–1.99) in both years but increased in both groups during the intervention (OR: 13.58, 95% CI: 7.30–25.28).
During cross-sectional surveys we observed higher ITN use by children ≤ 5 years of age, and there was a gradual increase in ITN use from survey to survey; the odds of a child sleeping under an ITN were 14 times greater at the last survey than in the first. ITN use was higher in LCI sites (Table 2).
Table 2. Factors affecting ITN use in various LCI and non-LCI survey sites, Kenya, 2004–2007.
| Factor | All children seen at surveysa |
Follow-up surveysb |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | OR | 95% CI | No. | % | OR | 95% CI | ||
| Non-LCI site | 3266 | 51.3 | 1 | 770 | 48.2 | 1 | |||
| LCI site | 3099 | 48.7 | 1.703 | 1.421–2.040 | 717 | 51.8 | 1.712 | 1311–2.236 | |
| Survey | |||||||||
| S1 | 1054 | 16.6 | 1 | 152 | 10.2 | 1 | |||
| S2 | 1152 | 18.1 | 1.496 | 1.141–1.961 | 203 | 13.7 | 1.789 | 1.009–3.170 | |
| S3 | 1062 | 16.7 | 3.577 | 2.726–4.694 | 197 | 13.2 | 3.975 | 2.290–6.901 | |
| S4 | 1048 | 16.5 | 5.436 | 4.137–7.144 | 272 | 18.3 | 5.533 | 3.187–9.606 | |
| S5 | 1014 | 15.9 | 6.885 | 5.210–9.098 | 292 | 19.6 | 9.795 | 5.625–17.057 | |
| S6 | 1035 | 16.3 | 13.616 | 10.302–17.996 | 371 | 24.9 | 11.207 | 6.491–19.350 | |
| Age, in years | |||||||||
| > 5 | 3714 | 58.4 | 1 | 995 | 66.9 | 1 | |||
| ≤ 5 | 2651 | 41.6 | 1.989 | 1.654–2.391 | 492 | 33.1 | 2.252 | 1.670–3.036 | |
CI, confidence interval; ITN, insecticide-treated net; LCI; larval control intervention; OR, odds ratio. a n = 6365; cases with ITN use = 1592 (25.5%); the analysis is based on the entire data set, including the children who attended only one survey per season. b n = 1487; cases with ITN use = 494 (33.2%); this subgroup analysis is based on study children who attended both the first and follow-up visit of a season survey and who were negative for parasites at the first visit. Only the follow-up data are included in the analysis.
Mosquito abundance
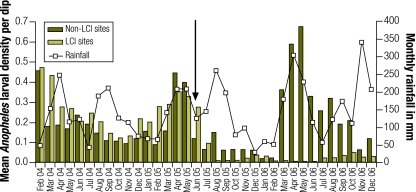
Anopheline larval abundance was highly seasonal, with peaks during the long rainy seasons (March–June). While larval densities remained at similar levels in non-LCI sites throughout the study, larviciding was associated with a 91.1% reduction in the mean number of late instar anopheline larvae (Table 3 and Fig. 2).
Table 3. Vector abundance, human biting rate and entomological inoculation rate at baseline and during intervention in non-LCI and LCI sites, Kenya, 2004–2007.
| Baseline |
Intervention |
Per cent reductiona | ||||
|---|---|---|---|---|---|---|
| Non-LCI sites | LCI sites | Non-LCI sites | LCI sites | |||
| Anopheles late instar larval abundance | ||||||
| Mean number of mosquito larvae per dip | 0.19 | 0.26 | 0.21 | 0.02* | 91.1 | |
| 95% CI | 0.14–0.26 | 0.18–0.36 | 0.15–0.28 | 0.01–0.05 | 87.1–94.8 | |
| Anophelesb adult abundance | ||||||
| Mean number of adult mosquitos per house | 3.69 | 3.49 | 0.6 | 0.08* | 85.9 | |
| 95% CI | 2.25–6.06 | 2.49–4.88 | 0.45–0.79 | 0.06–0.13 | 79.6–88.0 | |
| Average human biting rate | ||||||
| Mean number of bloodfed Anopheles females per person per sampling date | 0.45 | 0.39 | 0.06 | 0.014* | 73.1 | |
| 95% CI | 0.28–0.73 | 0.27–0.56 | 0.04–0.09 | 0.006–0.028 | 59.4–84.4 | |
| Annual entomological inoculation rate | ||||||
| Mean number of infectious bites per person per year | 11.98 | 10.3 | 1.68 | 0.39* | 73.1 | |
| 95% CI | 7.39–19.4 | 7.2–14.95 | 1.16–2.42 | 0.19–0.79 | 59.4–84.4 | |
*Difference between LCI and non-LCI sites in same time period significant at P < 0.001. CI, confidence interval; LCI, larval control intervention. a Percent reduction = 100 − (non-LCI at baseline / LCI at baseline × LCI during intervention / non-LCI during intervention) × 100. b Anopheles gambiae and Anopheles funestus combined.
Fig. 2.
Monthly mean density of late instar Anopheles larvae in sentinel sites in non-LCI and LCI sites in relation to rainfall, Kenya, 2004–2007a
LCI, larval control intervention.
a The arrow indicates the start of larviciding in LCI sites.
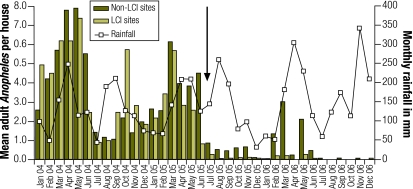
A total of 4274 Anopheles adults were collected during indoor-resting catches. Of these, 3107 (72.7%) were A. gambiae s.l., 1161 (27.2%) A. funestus s.l. and 6 (0.1%) A. rufipes. Further analysis of 160 A. gambiae s.l. showed that 97% were A. gambiae sensu stricto (s.s.) and 3% A. arabiensis. Testing for sporozoite infection was conducted on 1280 A. gambiae and 401 A. funestus females. The average sporozoite infection rate was similar before and during the intervention: 7.1% for A. gambiae and 8.1% for A. funestus. The seasonality of Anopheles adults followed that of the larval populations. Most adults were caught during the long rains (Fig. 3 and Table 4). Although mean Anopheles indoor adult densities were similar during the baseline period in non-LCI and LCI sites, during the second half of the study the adult density dropped by 84% in the non-LCI sites and by 98% in the LCI sites (Table 3 and Fig. 3). After the baseline year, adult density was significantly smaller in the LCI sites than in the non-LCI sites during the larval control intervention (P < 0.001). Larviciding was associated with an additional 85.9% reduction in adult mosquitoes resting indoors. Similar reductions were seen with the average human biting rate and EIR in non-LCI and LCI sites. The annual EIR of A. gambiae and A. funestus combined was 10–12 infectious bites per person in both groups at baseline (Table 3). With the increase in ITNs during the intervention year (Table 2), annual EIR dropped to 1.68 infectious bites per person in the non-LCI sites. Where larviciding was also carried out, annual EIR dropped to 0.39 infectious bites, and this accounted for an additional 73% reduction in EIR.
Fig. 3.
Monthly mean density of adult Anopheles mosquitoes in sentinel houses in non-LCI and LCI sites in relation to rainfall, Kenya, 2004–2007a
LCI, larval control intervention.
a The arrow indicates the start of larviciding in LCI sites.
Table 4. Factors affecting Anopheles adult resting densities in households, Kenya, 2004–2007.
| Factor | No.a | %a | OR | 95% CI |
|---|---|---|---|---|
| Study area | ||||
| Musilongo | 360 | 16.8 | 1.000 | |
| Emutete | 348 | 16.2 | 1.311 | 0.807–2.131 |
| Kezege | 359 | 16.7 | 0.651 | 0.319–1.330 |
| Wamondo | 360 | 16.8 | 0.110 | 0.066–0.184 |
| Wakikuyu | 358 | 16.7 | 0.179 | 0.127–0.251 |
| Kimingini | 360 | 16.8 | 0.421 | 0.253–0.702 |
| Study period | ||||
| Baseline | 1075 | 50.1 | 1.000 | |
| Intervention | 1070 | 49.9 | 0.140 | 0.065–0.304 |
| Survey season | ||||
| Dry | 1069 | 49.8 | 1.000 | |
| Short rains | 536 | 25.0 | 0.985 | 0.736–1.319 |
| Long rains | 540 | 25.2 | 1.746 | 1.322–2.305 |
| People sleeping in house before sampling | ||||
| 1–2 | 686 | 32.0 | 1.000 | |
| 3–4 | 856 | 39.9 | 1.181 | 0.930–1.500 |
| > 4 | 603 | 28.1 | 1.525 | 1.052–2.212 |
| ITN use in the household | ||||
| No | 1656 | 77.2 | 1.000 | |
| Yes | 489 | 22.8 | 0.844 | 0.637–1.119 |
| Larviciding in area | ||||
| No | 1605 | 74.8 | 1.000 | |
| Yes | 540 | 25.2 | 0.353 | 0.149–0.838 |
CI, confidence interval; ITN, insecticide-treated net; OR, odds ratio. a The number and proportion of indoor-resting collections per factor analysed.
Regression analyses adjusted for study site, baseline period, season of sampling, number of people that slept in the house before sampling and ITN use revealed that larviciding was associated with a 65% reduction in indoor-resting vectors (95% CI: 149–83.0%; Table 4).
Plasmodium infections
Plasmodium parasites were found in 2057 of 6365 blood slides, and 94.4% of the infections were caused by P. falciparum. Parasite prevalence was similar in both groups at baseline (OR: 1.01; 95% CI: 0.69–1.46), even though ITN use was higher in LCI sites (Table 2). The prevalence of new infections was 32.0% (95% CI: 26.5–37.5%) for the three baseline surveys. During the intervention period, the prevalence of new infections (OR: 0.59; 95% CI: 0.37–0.92) was significantly lower in the LCI-group (7.0%; 95% CI: 4.6–10.7%) than in the non-LCI group (12.8%; 95% CI: 9.7–15.9%). Nevertheless, it is inappropriate to compare prevalence between the baseline and intervention periods because at baseline two surveys were conducted in the long rainy season (April to June), the main transmission season, compared with only one during the intervention period.
During the baseline period the incidence of new infections declined during the long rains (Table 5). This occurred in both treatment groups and coincided with a four-fold increase in ITN use (OR: 3.98; 95% CI: 2.29–6.90; Table 2). The incidence rate immediately before the intervention was similar in both groups (Table 5).
Table 5. Incidence of Plasmodium infections by study area (non-LCI and LCI sites), stratified by cross-sectional surveys at baseline and during intervention period, 2004–2007a.
| Survey period | Non-LCI sites |
LCI sites |
RR | 95% CI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rb | Incidencec | 95% CI | Rb | Incidencec | 95% CI | |||||
| Baseline | ||||||||||
| Apr–Jun 2004 | 40/140 | 285.7 | 272.1–300.1 | 30/164 | 182.9 | 171.4–195.3 | 1.56 | 1.31–1.86 | ||
| Nov 2004–Jan 2005 | 22/232 | 94.8 | 86.7–103.7 | 24/174 | 1379 | 127.1–149.7 | 0.69 | 0.53–0.89 | ||
| Apr–Jun 2005 | 27/184 | 146.7 | 136.5–157.8 | 34/210 | 161.9 | 152.8–171.5 | 0.91 | 0.73–1.12 | ||
| Intervention | ||||||||||
| Nov 2005–Jan 2006 | 18/278 | 64.7 | 61.7–68.0 | 8/266 | 30.1 | 28.2–32.1 | 2.15 | 1.40–3.31 | ||
| Apr–Jun 2006 | 30/312 | 96.2 | 88.0–105.1 | 9/272 | 331 | 30.5–35.9 | 2.91 | 1.96–4.30 | ||
| Nov 2006–Jan 2007 | 8/394 | 20.3 | 18.9–21.8 | 14/348 | 40.2 | 38.0–42.6 | 0.50 | 0.30–0.86 | ||
CI, confidence interval; LCI, larval control intervention; R, rate; RR, rate ratio. a The analysis is based on study children aged 9 months to 13 years, that attended both the first and follow-up visit of a survey and were negative for parasites at the first visit. Data from children who attended only one visit of any survey or were already positive for parasites at the first visit are not included here. b Children positive for parasites at follow-up divided by children negative for parasites at the first survey. c Per 1000 child months at risk.
During the short rains, half a year after larviciding started in the LCI sites, new Plasmodium infections declined in both treatment groups. Compared to baseline, there were 32% fewer new infections in the non-LCI group (a drop from 94.8 to 64.7 new infections per 1000 child months at risk) compared with 78% fewer in the LCI group (a drop from 137.9 to 30.1 new infections per 1000 child months at risk; Table 5). During the long rains, new infections in the LCI-group were almost as frequent as in the previous season’s survey. In marked contrast, incidence in the non-LCI group was 50% higher than during the short rains. During the main malaria transmission season, the incidence rate of new parasite infections was 2.9 times (95% CI: 2.0–4.3) higher in children from areas without larviciding. However, during the short rainy season, larviciding had no effect on incidence.
General estimating equation analyses showed, after adjustment for confounders, that the risk of finding a child with malaria parasites was almost 40% less in children who slept under an ITN (OR: 0.61, 95% CI: 0.51–0.72) and in those that lived in an area where microbial larvicides were applied (OR: 0.63, 95% CI: 0.49–0.80) A more conservative analysis was carried out with only those children who were uninfected at the first survey and present at the following survey, 2 months later, to reduce the possibility of relapses or incomplete treatment. In this case, ITN use was associated with a 31% reduction in the risk of new malaria infections (OR: 0.69, 95% CI: 0.48–0.99), while residence in an area with additional larviciding reduced the risk of new infections by 56% (OR: 0.44; 95% CI: 0.23–0.82; Table 6).
Table 6. Factors affecting Plasmodium parasitaemia in children, Kenya, 2004–2007.
| Factor | Prevalence of parasitaemia in any surveya |
Incidence of new parasite infections at follow-upb |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | OR | 95% CI | No. | % | OR | 95% CI | ||
| Study area | |||||||||
| Musilongo | 1101 | 17.3 | 1.000 | 237 | 15.9 | 1.000 | |||
| Emutete | 1168 | 18.4 | 0.771 | 0.577–1.031 | 226 | 15.2 | 0.595 | 0.322–1.100 | |
| Kezege | 1050 | 16.5 | 0.683 | 0.523–0.891 | 210 | 14.1 | 0.895 | 0.537–1.492 | |
| Wamondo | 948 | 14.9 | 0.197 | 0.147–0.264 | 270 | 18.2 | 0.144 | 0.077–0.269 | |
| Wakikuyu | 1007 | 15.8 | 0.444 | 0.335–0.589 | 245 | 16.5 | 0.467 | 0.261–0.837 | |
| Kimingini | 1091 | 17.1 | 0.366 | 0.279–0.480 | 299 | 20.1 | 0.408 | 0.232–0.717 | |
| Study period | |||||||||
| Baseline | 3268 | 51.3 | 1.000 | 552 | 62.9 | 1.000 | |||
| Intervention | 3097 | 48.7 | 0.291 | 0.248–0.343 | 935 | 37.1 | 0.344 | 0.234–0.506 | |
| Survey season | |||||||||
| Short rains | 3235 | 50.8 | 1.000 | 846 | 56.9 | 1.000 | |||
| Long rains | 3130 | 49.2 | 1.349 | 1.210–1.504 | 641 | 43.1 | 2.203 | 1.651–2.939 | |
| Age of child, in years | |||||||||
| > 5 | 2651 | 41.6 | 1.000 | 995 | 66.9 | 1.000 | |||
| ≤ 5 | 3714 | 58.4 | 1.125 | 0.966–1.310 | 492 | 33.1 | 1.011 | 0.728–1.404 | |
| ITN use on previous night | |||||||||
| No | 4773 | 75.0 | 1.000 | 993 | 66.8 | 1.000 | |||
| Yes | 1592 | 25.0 | 0.610 | 0.514–0.723 | 494 | 33.2 | 0.691 | 0.481–0.995 | |
| Larviciding in area | |||||||||
| No | 4890 | 76.8 | 1.000 | 1044 | 70.2 | 1.000 | |||
| Yes | 1475 | 23.2 | 0.627 | 0.491–0.800 | 443 | 29.8 | 0.437 | 0.233–0.822 | |
ITN, insecticide-treated net; OR, odds ratio. a n = 6365; cases with parasitaemia = 2055 (32.2%); the analysis is based on the entire data set, including the children who attended only one visit of any season survey or who were already positive for parasites at the first visit. b n = 1490; cases with parasitaemia = 267 (17.8%); this subgroup analysis was used to calculate new parasite infections over the follow-up period and is based on study children who attended both the first and follow-up visit of a season survey and who were negative for parasites at the first visit.
Discussion
This study was designed to investigate whether mosquito larval control in highland areas with moderate and focal malaria transmission could reduce Plasmodium infections in children. We have provided the first evidence of the effect of a double vector control intervention targeting both larval and adult mosquitoes. Vector control with microbial larvicides and ITNs combined resulted in a two-fold reduction in new malaria infections compared with ITNs alone. Thus, the addition of anti-larval measures to ITN programmes can provide substantial additional protection against malaria parasites.
The reduction in transmission associated with larviciding may have been greater than our data suggest since sampling from pyrethrum spray collections in homes with ITNs would have underestimated the true biting rate. This is because in homes with ITNs many vectors would have left the room during the night before the spray collections the following day. One weakness of our study was the non-random allocation of larviciding to the study sites. Nonetheless, sites were grouped to ensure that the rate of malaria transmission and infection with malaria parasites was similar in each group at baseline. The reading of blood films was blinded, but project staff collecting the entomological data could not be blinded to the larvicides applied. However, pyrethrum spray collections are not prone to operator bias, so this should not be a major source of error. The treatment of children with artemisinin-based combination therapies may have contributed to the decline in malaria seen across the study communities, since artemether has gametocidal properties. Nevertheless, it is unlikely that the gametocyte reservoir was substantially reduced because no adults were treated by the project team and artemisinin-based combination therapies were only available in local health centres by mid 2006.
We are at a critical time in the history of malaria control in Africa. For the first time in a generation, reports of malaria declining have become common.29,38,39 In Kenya, ITN coverage increased from 7% in 2004 to 67% by the end of 2006, and cross-sectional surveys showed that ITN use was associated with a reduction in mortality of 44%.29 As Roll Back Malaria gathers momentum, it is essential to maintain these hard-won gains. The “current best practice” of malaria control has several long-term weaknesses: (i) over-reliance on drugs and insecticides targeting adult mosquitoes and the likelihood that the development of resistance will threaten the future efficacy of malaria control40; (ii) behavioural changes in humans, with people less inclined to sleep under ITNs when vector populations decline; (iii) behavioural changes in mosquito adults in response to increased personal protection measures (e.g. earlier biting, outdoor biting)23; and (iv) over-reliance on a single vector control tool that will be less effective than integrated vector management at reducing vector populations.
Larval source management and the use of microbial larvicides offer additional protection against malaria. Microbials are highly effective at killing mosquito larvae, highly specific in action and safe to use. Importantly, the risk that resistance will develop is very low and can be easily managed and reversed.19,22,31,41 Larval source management may also delay the emergence of resistance to the pyrethroid insecticides used on ITNs. The cost of larviciding is similar to that of ITN and IRS programmes and may drop if environmental modifications can reduce breeding sites42 and if larviciding can be targeted in space, time or both. In our study, vector densities peaked during the main transmission seasons, even though bednet coverage was high. Targeting larval control briefly at the end of the dry season and beginning of the long rainy season may be equally efficient at controlling malaria, and more cost-effective, than continual application throughout the year.
The integration of larval source management into ongoing programmes is likely to be most effective where transmission is moderate or low and where mosquito breeding sites are contained and well defined.12,19 These include highland areas, desert-fringe areas, urban settings and areas prone to epidemics. The current success of ITN programmes will result in far more areas with low and focal malaria transmission and offers a great opportunity for integrated vector management programmes, including larval source management, to maintain hard-won gains and aim for even further reductions.
Vector control in Africa should target all stages of the mosquito life cycle, yet for the past 50 years it has focused almost exclusively on adult mosquito control. ITNs have not only saved thousands of lives; they have also restored confidence in vector control in Africa. However, adult-based methods are limited in what they can achieve43,44 because adult mosquitoes feed outside houses and before sleeping hours.23,43 Larval source management targeting both indoor and outdoor biting vector populations should therefore contribute to greater reductions in transmission than ITNs alone. Truly integrated and well-managed malaria control efforts have led to major successes in the past, including the eradication of A. gambiae from Brazil45 and Egypt,46 the eradication of malaria in the United States, Europe and the Middle East47,48 and the control of malaria in Zambia.20 Yet these successes have largely been forgotten or dismissed. Our study is among the first to reassess the impact of larval source management on malaria transmission and infection incidence in contemporary Africa. Our findings suggest that integrated vector management can be a highly effective tool for reducing malaria in the future in many parts of sub-Saharan Africa. ■
Acknowledgements
We thank the communities and especially the children of Kimingini, Musilingo, Emutete, Kezege, Wakikuyu and Wamondo for their support and willingness to participate in this research. We are also grateful to the field and laboratory team for its tireless support, and we thank Brian Greenwood for his critical review of the manuscript and Valent BioSciences Corp., USA, for the donation of larvicides. This study has been published with the permission of the director of the Kenya Medical Research Institute.
Footnotes
Funding: The project was funded by the Environmental Health Project of the United States Agency of International Development. The funding sources had no role in the design, conduct, data collection analyses or interpretation of this study. All authors had access to all the data.
Competing interests: The programme evaluated in this manuscript was partially supported by Valent BioSciences Corporation, a commercial manufacturer of microbial larvicides.
References
- 1.Shanks GD, Hay SI, Omumbo JA, Snow RW. Malaria in Kenya’s western highlands. Emerg Infect Dis. 2005;11:1425–32. doi: 10.3201/eid1109.041131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guyatt HL, Ochola SA, Snow RW. Too poor to pay: charging for insecticide-treated bednets in highland Kenya. Trop Med Int Health. 2002;7:846–50. doi: 10.1046/j.1365-3156.2002.00929.x. [DOI] [PubMed] [Google Scholar]
- 3.Hay SI, Were EC, Renshaw M, Noor AM, Ochola SA, Olusanmi I, et al. Forecasting, warning, and detection of malaria epidemics: a case study. Lancet. 2003;361:1705–6. doi: 10.1016/S0140-6736(03)13366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bødker R, Kisinza W, Malima R, Msangeni HA, Lindsay SW. Resurgence of malaria in the Usambara mountains, Tanzania is due to an epidemic of drug-resistant parasites. Glob Change Hum Health. 2000;1:134–43. doi: 10.1023/A:1010077105257. [DOI] [Google Scholar]
- 5.Mushinzimana E, Munga S, Minakawa N, Li L, Feng CC, Bian L, et al. Landscape determinants and remote sensing of anopheline mosquito larval habitats in the western Kenya highlands. Malar J. 2006;5:13. doi: 10.1186/1475-2875-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Munga S, Minakawa N, Zhou G, Mushinzimana E, Barrack OO, Githeko AK, et al. Association between land cover and habitat productivity of malaria vectors in Western Kenyan highlands. Am J Trop Med Hyg. 2006;74:69–75. [PubMed] [Google Scholar]
- 7.Briet OJ, Dossou-Yovo J, Akodo E, van de Giesen N, Teuscher TM. The relationship between Anopheles gambiae density and rice cultivation in the savannah zone and forest zone of Cote d’Ivoire. Trop Med Int Health. 2003;8:439–48. doi: 10.1046/j.1365-3156.2003.01054.x. [DOI] [PubMed] [Google Scholar]
- 8.Roll Back Malaria Partnership. Roll Back Malaria: global strategic plan 2005‑2015 Geneva: RBM; 2005. [Google Scholar]
- 9.Guidelines for integrated vector management Harare: WHO Regional Office for Africa; 2003.
- 10.Townson H, Nathan MB, Zaim M, Guillet P, Manga L, Bos R, et al. Exploiting the potential of vector control for disease prevention. Bull World Health Organ. 2005;83:942–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Report of the WHO consultation on integrated vector management (IVM) Geneva: World Health Organization; 2007. [Google Scholar]
- 12.Fillinger U, Sonye G, Killeen GF, Knols BG, Becker N. The practical importance of permanent and semipermanent habitats for controlling aquatic stages of Anopheles gambiae sensu lato mosquitoes: operational observations from a rural town in western Kenya. Trop Med Int Health. 2004;9:1274–89. doi: 10.1111/j.1365-3156.2004.01335.x. [DOI] [PubMed] [Google Scholar]
- 13.Gu W, Utzinger J, Novak RJ. Habitat-based larval interventions: a new perspective for malaria control. Am J Trop Med Hyg. 2008;78:2–6. [PubMed] [Google Scholar]
- 14.Killeen GF, Fillinger U, Kiche I, Gouagna LC, Knols BG. Eradication of Anopheles gambiae from Brazil: lessons for malaria control in Africa? Lancet Infect Dis. 2002;2:618–27. doi: 10.1016/S1473-3099(02)00397-3. [DOI] [PubMed] [Google Scholar]
- 15.Killeen GF, Fillinger U, Knols BG. Advantages of larval control for African malaria vectors: low mobility and behavioural responsiveness of immature mosquito stages allow high effective coverage. Malar J. 2002;1:8. doi: 10.1186/1475-2875-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Killeen GF, Tanner M, Mukabana WR, Kalongolela MS, Kannady K, Lindsay SW, et al. Habitat targeting for controlling aquatic stages of malaria vectors in Africa. Am J Trop Med Hyg. 2006;74:517–8. [PubMed] [Google Scholar]
- 17.Shililu J, Ghebremeskel T, Seulu F, Mengistu S, Fekadu H, Zerom M, et al. Larval habitat diversity and ecology of anopheline larvae in Eritrea. J Med Entomol. 2003;40:921–9. doi: 10.1603/0022-2585-40.6.921. [DOI] [PubMed] [Google Scholar]
- 18.Utzinger J, Tanner M, Kammen DM, Killeen GF, Singer BH. Integrated programme is key to malaria control. Nature. 2002;419:431. doi: 10.1038/419431a. [DOI] [PubMed] [Google Scholar]
- 19.Fillinger U, Lindsay SW. Suppression of exposure to malaria vectors by an order of magnitude using microbial larvicides in rural Kenya. Trop Med Int Health. 2006;11:1629–42. doi: 10.1111/j.1365-3156.2006.01733.x. [DOI] [PubMed] [Google Scholar]
- 20.Utzinger J, Tozan Y, Singer BH. Efficacy and cost-effectiveness of environmental management for malaria control. Trop Med Int Health. 2001;6:677–87. doi: 10.1046/j.1365-3156.2001.00769.x. [DOI] [PubMed] [Google Scholar]
- 21.Yohannes M, Haile M, Ghebreyesus TA, Witten KH, Getachew A, Byass P, et al. Can source reduction of mosquito larval habitat reduce malaria transmission in Tigray, Ethiopia? Trop Med Int Health. 2005;10:1274–85. doi: 10.1111/j.1365-3156.2005.01512.x. [DOI] [PubMed] [Google Scholar]
- 22.Fillinger U, Kannady K, William G, Vanek MJ, Dongus S, Nyika D, et al. A tool box for operational mosquito larval control: preliminary results and early lessons from the Urban Malaria Control Program in Dar es Salaam, Tanzania. Malar J. 2008;7:20. doi: 10.1186/1475-2875-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geissbühler Y, Chaki P, Emidi B, Govella NJ, Shirima R, Mayagaya V, et al. Interdependence of domestic malaria prevention measures and mosquito-human interactions in urban Dar es Salaam, Tanzania. Malar J. 2007;6:126. doi: 10.1186/1475-2875-6-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawley WA, Phillips-Howard PA, ter Kuile FO, Terlouw DJ, Vulule JM, Ombok M, et al. Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western Kenya. Am J Trop Med Hyg. 2003;68:121–7. [PubMed] [Google Scholar]
- 25.Lengeler C, Grabowsky M, McGuire D, deSavigny D. Quick wins versus sustainability: options for the upscaling of insecticide-treated nets. Am J Trop Med Hyg. 2007;77:222–6. [PubMed] [Google Scholar]
- 26.Killeen GF, Smith TH, Ferguson HM, Mshinda H, Abdulla S, Lengeler C, et al. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. 2007;4:e229. doi: 10.1371/journal.pmed.0040229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ndenga B, Githeko A, Omukunda E, Munyekenye G, Atieli H, Wamai P, et al. Population dynamics of malaria vectors in western Kenya highlands. J Med Entomol. 2006;43:200–6. doi: 10.1603/0022-2585(2006)043[0200:PDOMVI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Brown DR, Stephens EC, Ouma JO, Murithi FM, Barret C. Livelihood strategies in the rural Kenyan highlands. AfJARE. 2006;1:21–36. [Google Scholar]
- 29.Fegan GW, Noor AM, Akhwale WS, Cousens S, Snow RW. Effect of expanded insecticide-treated bednet coverage on child survival in rural Kenya: a longitudinal study. Lancet. 2007;370:1035–9. doi: 10.1016/S0140-6736(07)61477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noor AM, Amin AA, Akhwale WS, Snow RW. Increasing coverage and decreasing inequity in insecticide-treated bed net use among rural Kenyan children. PLoS Med. 2007;4:e255. doi: 10.1371/journal.pmed.0040255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mulla MS, Thavara U, Tawatsin A, Chomposri J, Su T. Emergence of resistance and resistance management in field populations of tropical Culex quinquefasciatus to the microbial control agent Bacillus sphaericus. J Am Mosq Control Assoc. 2003;19:39–46. [PubMed] [Google Scholar]
- 32.Entomological field techniques for malaria control Geneva: World Health Organization; 1992. [Google Scholar]
- 33.Zhou G, Minakawa N, Githeko A, Yan G. Spatial distribution patterns of malaria vectors and sample size determination in spatially heterogeneous environments: a case study in the west Kenyan highland. J Med Entomol. 2004;41:1001–9. doi: 10.1603/0022-2585-41.6.1001. [DOI] [PubMed] [Google Scholar]
- 34.Scott JA, Brogdon WG, Collins FH. Identification of single specimens of the Anopheles gambiae complex by the polymerase chain reaction. Am J Trop Med Hyg. 1993;49:520–9. doi: 10.4269/ajtmh.1993.49.520. [DOI] [PubMed] [Google Scholar]
- 35.Beier JC, Perkins PV, Wirtz RA, Whitmire RE, Mugambi M, Hockmeyer WT. Field evaluation of an enzyme-linked immunosorbent assay (ELISA) for Plasmodium falciparum sporozoite detection in anopheline mosquitoes from Kenya. Am J Trop Med Hyg. 1987;36:459–68. doi: 10.4269/ajtmh.1987.36.459. [DOI] [PubMed] [Google Scholar]
- 36.Drakeley C, Schellenberg D, Kihonda J, Sousa CA, Arez AP, Lopes D, et al. An estimation of the entomological inoculation rate for Ifakara: a semi-urban area in a region of intense malaria transmission in Tanzania. Trop Med Int Health. 2003;8:767–74. doi: 10.1046/j.1365-3156.2003.01100.x. [DOI] [PubMed] [Google Scholar]
- 37.Kirkwood BR, Sterne J. Medical statistics 2nd ed. Malden: Blackwell; 2003. [Google Scholar]
- 38.Roberts L. Battling over bed nets. Science. 2007;318:556–9. doi: 10.1126/science.318.5850.556. [DOI] [PubMed] [Google Scholar]
- 39.The World Bank. World Bank group report on malaria in Africa Washington, DC: WB; 2007. Available from: www.worldbank.org/afr/malaria [accessed on 29 June 2008].
- 40.N’Guessan R, Corbel V, Akogbeto M, Rowland M. Reduced efficacy of insecticide-treated nets and indoor residual spraying for malaria control in pyrethroid resistance area, Benin. Emerg Infect Dis. 2007;13:199–206. doi: 10.3201/eid1302.060631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO International programme on chemical safety (IPCS): Microbial pest control agent Bacillus thuringiensis. Environ Health Criteria. 1999;217:1–105. [Google Scholar]
- 42.Worral E. Cost analyses for large scale use of larval source management in malaria control Washington, DC: Prepared for RTI International by Liverpool Associates in Tropical Health under contract to the Bureau for Global Health, US Agency for International Development; 2007. [Google Scholar]
- 43.Killeen GF, Kihonda J, Lyimo E, Oketch FR, Kotas ME, Mathenge E, et al. Quantifying behavioural interactions between humans and mosquitoes: evaluating the protective efficacy of insecticidal nets against malaria transmission in rural Tanzania. BMC Infect Dis. 2006;6:161. doi: 10.1186/1471-2334-6-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Killeen GF, Smith TA. Exploring the contributions of bed nets, cattle, insecticides and excitorepellency to malaria control: a deterministic model of mosquito host-seeking behaviour and mortality. Trans R Soc Trop Med Hyg. 2007;10:867–80. doi: 10.1016/j.trstmh.2007.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Soper FL, Wilson DB. Anopheles gambiae in Brazil New York, NY: The Rockefeller Foundation; 1943. [Google Scholar]
- 46.Shousha AT. The eradication of Anopheles gambiae from Upper Egypt 1942-1945. Bull World Health Organ. 1948;1:309–33. [PMC free article] [PubMed] [Google Scholar]
- 47.Hays CW. The United States Army and malaria control in World War II. Parassitologia. 2000;42:47–52. [PubMed] [Google Scholar]
- 48.Kitron U, Spielman A. Suppression of transmission of malaria through source reduction: antianopheline measures applied in Israel, the United States, and Italy. Rev Infect Dis. 1989;11:391–406. doi: 10.1093/clinids/11.3.391. [DOI] [PubMed] [Google Scholar]