Abstract
The management of Meckel diverticulum found unexpectedly during an abdominal operation remains controversial. Most published reports have included only patients undergoing diverticulectomy or bowel resection through laparotomy. We report a case of a carcinoid tumor in a Meckel’s diverticulum which was incidentally detected and removed during laparoscopic inguinal hernia repair. Although there is no compelling evidence in the literature to recommend prophylactic diverticulectomy, laparoscopic stapled resection represents a viable and safe approach in healthy individuals undergoing elective surgery for other purposes.
Keywords: Laparoscopy, Incidental findings, Meckel’s diverticulum, Carcinoid tumor
INTRODUCTION
Meckel’s diverticulum (MD) is one of the most common congenital abnormalities of the gastrointestinal tract, as it occurs in approximately 2% of the population. This true diverticulum results from an incomplete obliteration of the vitelline duct during the fifth week of gestation and arises from the antimesenteric border of the distal ileum, within 100 cm of the ileocecal valve in the adult. In the majority of cases, the MD is asymptomatic and the diagnosis is made during elective surgery for other intra-abdominal disorders. In some circumstances, the MD can be associated with heterogeneous clinical manifestations ranging from recurrent abdominal pain to life-threatening problems, such as gastrointestinal bleeding or acute bowel obstruction. The diverticulum may contain areas of ectopic mucosa, more commonly of gastric type, or malignant tumors such as carcinoids[1].
The decision to perform diverticulectomy for MD incidentally detected during an abdominal operation is still controversial. Over the past two decades, laparoscopy has been extensively used in the diagnosis and treatment of various abdominal disorders. The opportunity provided by the laparoscopic approach to perform a complete abdominal exploration may increase the number of incidental findings, and this may again pose a dilemma to the surgeon who is more and more committed to the principles of evidence-based medicine for a better and more cost-effective patient care.
CASE REPORT
A 66 year-old man was seen in the outpatient clinic because of the chronic complaint of pain on exertion and a bulge localized at his left groin. His medical history was unremarkable, except for a mild hypertension. The body mass index was 30. Physical examination showed a bilateral inguinal hernia. An abdominal ultrasonography was negative. Elective laparoscopic repair of the bilateral hernia was scheduled after the patient gave his informed consent.
Preoperative antibiotic prophylaxis (Cefazolin, 2 g i.v.) was administered. Under general anesthesia, pneumoperitoneum was established using a Veress needle. Three bladeless trocars were inserted along the transverse umbilical line, and a 30° angled scope was introduced through the umbilical port. Laparoscopic exploration immediately revealed a 4 cm long MD arising from the distal ileum, about 70 cm proximal to the ileocecal valve (Figure 1). Priority was given to the inguinal hernia repair. Starting from the left groin, a curvilinear incision was made in the peritoneum beginning laterally and extending to the medial umbilical ligament. A peritoneal flap was created medially by blunt dissection to expose the Cooper’s ligament. A preformed polypropylene mesh was placed within the pre-peritoneal pocket and secured with staples and fibrin glue. The peritoneal layer was closed with a running suture (PDS, Ethicon). The same procedure was repeated in the right groin. Upon completion of the hernia repair, the MD was hold with an atraumatic grasper through the left port and an endoscopic linear stapler (EndoGIA II, 60 mm, Covidien) was tangentially applied across the base of the diverticulum and fired. The specimen was put into a plastic bag and removed through one of the ports. The patient had an uncomplicated recovery and was discharged home on postoperative day 2. Pathologic examination of the surgical specimen showed a normal ileal mucosa lining and a nodule, 1.5 cm in diameter, with a pattern indicative for a carcinoid tumor located in the proximity of the tip of the diverticulum (Figure 2).
Figure 1.
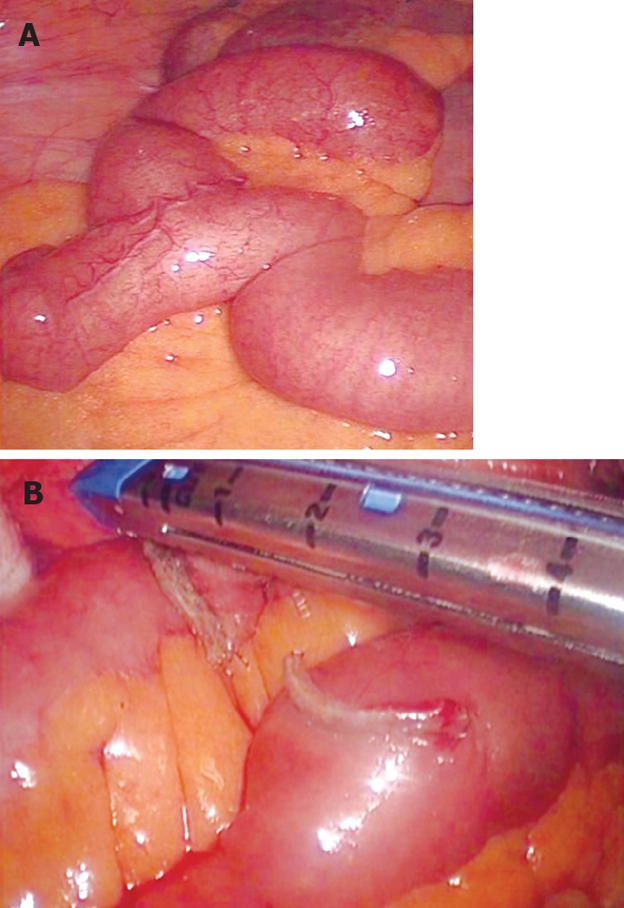
Meckel diverticulum found unexpectedly during laparoscopic inguinal hernia repair (A) and resection of the diverticulum with an endoscopic linear stapler (B).
Figure 2.
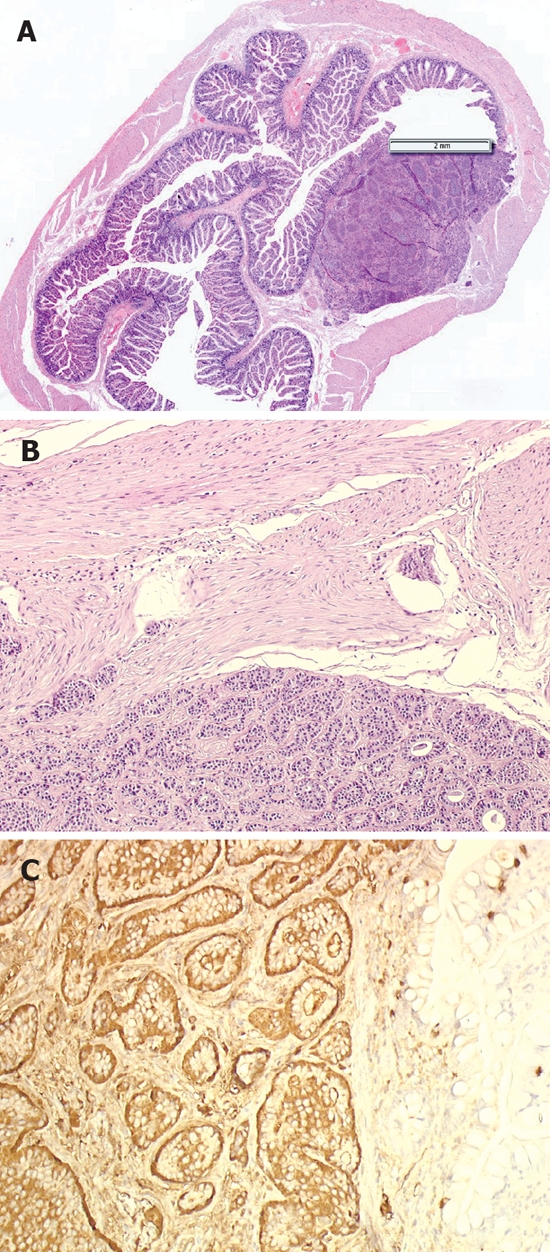
Meckel diverticulum with a nodule 1.5 cm in size (HE, × 1.5) (A), superficial infiltration of the diverticulum wall (HE, × 10) (B), and immuno-histochemical stain with chromogranin A showing a strongly positive reaction and normal intestinal mucosa with control stain of endocrine single cells on the right (× 10) (C).
DISCUSSION
It has long been stated that the risk of developing complications following the incidental removal of MD can offset the potential benefits of this procedure[2]. Opponents to incidental diverticulectomy often cite Soltero and Bill[3] who, in 1976, estimated that the life-time risk of complications from an untreated MD was 4.2%, and that this risk decreased to zero with age. These authors recommended refraining from incidental diverticulectomy because there is only a small chance of MD-related complications in later life. In contrast, almost twenty years later, the results of a large population-based study in Olmsted County, Minnesota, provided data in support of prophylactic diverticulectomy[4]). This study reported a 6.4% cumulative rate of developing complications of MD that required surgery over a life-time, especially in male patients up to 80 years of age. Diverticulectomy for complicated MD carried an operative mortality and morbidity of 2% and 12%, and a cumulative risk of long-term complications of 7%. The corresponding rate for incidental diverticulectomy is 1%, 2% and 2%, respectively. Interestingly, in this latter subgroup of patients, the mortality was related to the primary operation or the patient fitness but not to the diverticulectomy itself[4]. A subsequent report from the Mayo Clinic recommended MD resection only in male patients younger than 50 years of age, or when the diverticulum length is greater than 2 cm, or when abnormal features are detected within the diverticulum[1]. Of interest, a carcinoid tumor was found in 2.2% of the symptomatic patients and in 2.1% of the asymptomatic ones in this series[1]. More recently, however, a systematic review of the English literature has shown that there is no compelling evidence to support prophylactic resection[5]. In fact, resection of incidentally detected MD has a significantly higher early complication rate than leaving the diverticulum in situ (5.3% vs 1.3%, P < 0.0001)[4].
It should be noted that most of the data upon which recommendations have been based so far originate from retrospective studies in patients who underwent incidental diverticulectomy or bowel resection through laparotomy[5]. The advent of laparoscopy may have changed this scenario. Laparoscopy allows a complete abdominal exploration in patients undergoing minimally invasive procedures and has the potential to reveal additional pathological findings. Moreover, laparoscopy has been used to diagnose and treat patients with MD complicated by small bowel obstruction or bleeding caused by occult heterotopic gastric mucosa[6,7].
To our knowledge, this is the first reported case of carcinoid in MD which was incidentally found and removed during laparoscopy for inguinal hernia repair. Carcinoids are slow growing tumors with a malignant potential arising from the diffuse neuroendocrine system. The gastrointestinal tract is the largest neuroendocrine organ in the body and the site of origin for 90% of all carcinoids. The most common location of carcinoid is the appendix, where tumors are usually small and benign, followed by the ileum, where they are often multiple and characterized by a more aggressive biological behavior. More than 100 cases of carcinoids in MD have been reported in the literature, 72% of the tumors were located at the tip of the diverticulum, and distant metastases were present in 24% of the patients at the time of diagnosis[8]. Immunohistochemical studies have shown that Meckel’s carcinoids are closer to the ileal rather than to the appendiceal carcinoids[9]. Histopathological analysis in our patient demonstrated a R0 resection and the presence of limited superficial invasion of the diverticulum wall, confirming that diverticulectomy is adequate. Although there is no compelling evidence in the current literature to support prophylactic diverticulectomy for patients with MD, we believe that simple laparoscopic tangential resection with an endostapler is a viable and safe procedure during elective operations for healthy patients.
Footnotes
Peer reviewer: Kazuhiro Hanazaki, MD, Professor and Chairman, Department of Surgery, Kochi Medical School, Kochi University, Kohasu, Okohcho, Nankoku, Kochi 783-8505, Japan
S- Editor Zhong XY L- Editor Wang XL E- Editor Ma WH
References
- 1.Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002) Ann Surg. 2005;241:529–533. doi: 10.1097/01.sla.0000154270.14308.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leijonmarck CE, Bonman-Sandelin K, Frisell J, Raf L. Meckel's diverticulum in the adult. Br J Surg. 1986;73:146–149. doi: 10.1002/bjs.1800730225. [DOI] [PubMed] [Google Scholar]
- 3.Soltero MJ, Bill AH. The natural history of Meckel's Diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel's Diverticulum found in King County, Washington, over a fifteen year period. Am J Surg. 1976;132:168–173. doi: 10.1016/0002-9610(76)90043-x. [DOI] [PubMed] [Google Scholar]
- 4.Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, Melton LJ 3rd. Surgical management of Meckel’s diverticulum. An epidemiologic, population-based study. Ann Surg. 1994;220:564–568; discussion 568-569. doi: 10.1097/00000658-199410000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zani A, Eaton S, Rees CM, Pierro A. Incidentally detected Meckel diverticulum: to resect or not to resect? Ann Surg. 2008;247:276–281. doi: 10.1097/SLA.0b013e31815aaaf8. [DOI] [PubMed] [Google Scholar]
- 6.Sanders LE. Laparoscopic treatment of Meckel’s diverticulum. Obstruction and bleeding managed with minimal morbidity. Surg Endosc. 1995;9:724–727. doi: 10.1007/BF00187950. [DOI] [PubMed] [Google Scholar]
- 7.Rivas H, Cacchione RN, Allen JW. Laparoscopic management of Meckel’s diverticulum in adults. Surg Endosc. 2003;17:620–622. doi: 10.1007/s00464-002-8613-4. [DOI] [PubMed] [Google Scholar]
- 8.Nies C, Zielke A, Hasse C, Ruschoff J, Rothmund M. Carcinoid tumors of Meckel's diverticula. Report of two cases and review of the literature. Dis Colon Rectum. 1992;35:589–596. doi: 10.1007/BF02050541. [DOI] [PubMed] [Google Scholar]
- 9.Moyana TN. Carcinoid tumors arising from Meckel’s diverticulum. A clinical, morphologic, and immunohisto-chemical study. Am J Clin Pathol. 1989;91:52–56. doi: 10.1093/ajcp/91.1.52. [DOI] [PubMed] [Google Scholar]


