Abstract
Purpose
Since the revised Cancer Act of October 2006, cancer registration was reactivated, based on the Statistics Law.
Materials and Methods
The incidence of cancer during 2002 was calculated on the basis of the information available from the National Cancer Incidence Database. Crude and age-standardized rates were calculated by gender for 18 age groups (0~4, 5~9, 10~14, every five years, 85 years and over).
Results
The overall crude incidence rates (CRs) were 269.2 and 212.8 per 100,000 for males and females, and the overall age-standardized incidence rates (ASRs) were 287.8 and 172.9 per 100,000, respectively. Among males, the five leading primary cancer sites were stomach (CR 62.4, ASR 65.7), lung (CR 45.4, ASR 51.0), liver (CR 43.2, ASR 43.7), colon and rectum (CR 30.7, ASR 32.7), and prostate (CR 8.0, ASR 9.6). Among females, the most common cancer sites were breast (CR 33.1, ASR 26.9), followed by stomach (CR 32.8, ASR 26.0), colon and rectum (CR 23.1, ASR 18.5), thyroid (CR 19.1, ASR 15.7), and uterine cervix (CR 18.2, ASR 14.7). In the 0~14 age group, leukemia was the most common cancer for both genders. For males, stomach cancer was the most common cancer in the 15~64 age-group, but lung cancer was more frequent in men 65 or older. For females, thyroid cancer among the 15~34 age-group, breast cancer among 35~64 age-group and stomach cancer in women 65 years or older were the most common forms of cancer for each age group. The quality indices for the percentage of deaths, by death certificate only, were 4.7% for males and 4.5% for females.
Conclusions
Since the National Cancer Incidence Database was started, the annual percent change of cancer cases increased by 4.8% (4.1% for males, 5.7% for females) during 1999~2002. This value reflects the increase in prostate cancer for males and breast and thyroid cancer in females during 2002. The timely reporting of improved quality of cancer registration is needed for evidence-based decisions regarding cancer control in Korea.
Keywords: Cancer, Incidence, Korea
INTRODUCTION
Originally, cancer registries were primarily concerned with the description of cancer patterns. In the last 20 years, cancer registries provided not only information on the incidence and characteristics of specific cancers but also supplied the source of cancer control planning and evaluation and the care of individual cancer patients with survival (1).
In Korea, since 1980, a nationwide hospital-based cancer registry (Korea Central Cancer Registry: KCCR) has been active in collaborating with training hospitals. The annual report of the KCCR for 2002 was published in December 2003 (2) and showed the trends of cancer occurrence in Korea. In November 2004, the Ministry of Health and Welfare designated the KCCR and eight population-based regional cancer registries (PB-RCR) to facilitate nationwide cancer registration and to obtain regional and national cancer statistics. However, privacy protection laws limited cancer registration between 2004 and 2006. The National Cancer Incidence Database (NCIDB) was constructed with the KCCR original DB and 8 PB-RCR databases, and the site-specific cancer registry databases (such as breast, ovary, uterus, and liver cancer databases), as well as the data from the ad-hoc medical record review surveys and the cancer mortality database from the National Statistical Office (NSO) (3). The national cancer incidence during 1999~2001 was first reported in 2005 (4).
The revised law of the Cancer Act (October 2006) encouraged the collection of information on cancer cases with personal identification, with the introduction of the Statistics law. Hence, the national cancer registration was reactivated to collect newly diagnosed cancer cases by active and passive registration.
In this report, cancer incidence for the year 2002 is reported, using the Korea-NCIDB.
MATERIALS AND METHODS
1) Sources of data
The NCIDB, for the year 2002, was constructed using the same process as the NCIDB for the period 1999~2001 published in 2005 (2,5). In detail, the KCCR identified incident form of cancer cases in Korea through the nationwide hospital-based cancer registration. All malignant neoplasms and in situ cases by international classification of diseases for oncology (ICD-O) were reported by training hospitals. The collection of information was largely passive.
The list of KCCR-registered cases and a list of cancer cases of the billing claims made by the National Health Insurance Corporation (NHIC) for each region were sent to the regional cancer registries to identify unregistered cancer cases. The data collection methods of regional cancer registries were both passive and active.
From 2002 to 2006, we conducted an ad hoc nation-wide medical record review survey of patients who were newly diagnosed during 1999~2003, and were not registered through both registration systems (hospital-based cancer registration and regional population-based cancer registration).
In 2002, the KCCR constructed the Korea National Cancer Incidence DataBases (KNCIDB) by merging the KCCR mother DB, all 8 PB-RCR databases, and the site-specific cancer registry databases (breast, ovary, cervix, liver cancer etc) as well as the data from the ad-hoc medical record review surveys and the cancer mortality database from the National Statistical Office (NSO). The KNCIDB was further refined by confirming multiple primary cancers according to the rules provided by the International Agency for Research on Cancer (IARC); only one tumor per organ or pair of organs per person per lifetime is reportable. Duplicates were removed with the help of experts from a variety of fields such as clinicians, pathologists and medical record administrators.
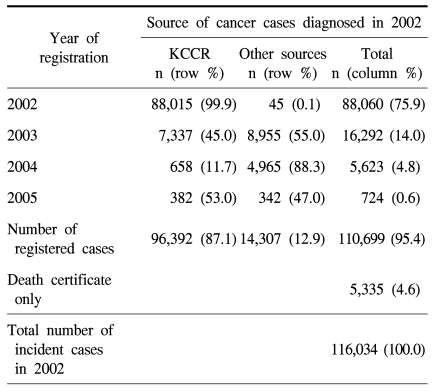
All newly diagnosed cancer cases in 2002 according to ICD-O-3 were included in this study. They were 116,034 cases analyzed during 2002. Among them, 110,699 (95.4%) cases were included, from 593 hospitals-including 164 KCCR-affiliated hospitals. In 2002, there were 40,029 hospitals and clinics including 284 general hospitals, and 691 hospitals in Korea (6). Approximately 87.1% (96,392 cases out of 110,699 cases) were registered through the KCCR program and 12.9% of the cases were collected through the PB-RCR, site-specific cancer registry, and other ad-hoc medical record review surveys. There were 5,335 cancer deaths not identified by the medical records and included as death certificate reports only, in the final data set of the incidence database for the year of 2002. Table 1 shows the number of incident cases by year of registration and the final data set for the calculation of incidence in the year 2002.
Table 1.
Number of cancer cases first diagnosed in the year 2002
2) Data control and quality indices
We calculated several quality indices. For the mortality: incidence ratio (M : I), an indicator of data completeness, the mortality data on cancer by gender, age group and cancer site, for the same period as the mortality from the NSO, were compared to the incidence data from the registry, which is presented as a percent. The microscopic verification percentage (MV%), an indicator of the validity of the diagnostic information, is the percentage of cases for which the diagnosis was based on morphological verification by a tissue specimen. The Death Certificate Only percentage (DCO%), is the percentage of cases registered on the basis of death certificates only, and was one of the indices for the validity of the diagnosis. Primary site unknown percentage (PSU%) and age unknown percentage (Age UNK%) are the percentage of cases registered with unknown primary cancer sites or unknown age.
3) Statistical analysis
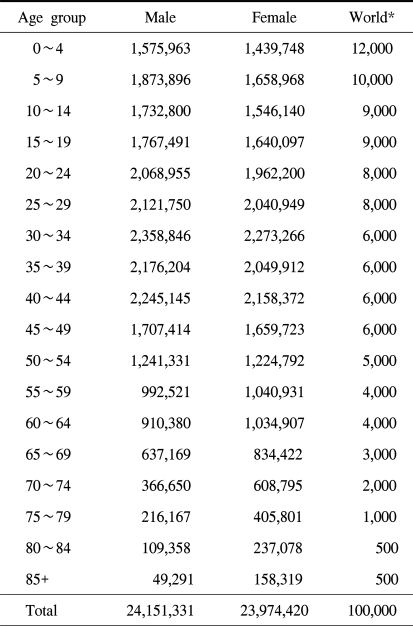
The crude incidence rates (CRs) per 100,000 by gender were calculated for 18 age groups (0~4, 5~9, 10~14, every five year, 85 years and over) and standardized to the World Standard Population of the World Health Organization (WHO). The population used as the denominator to calculate the cancer incidence was a mid-year population (the population as of July 1st). In this report, we modified the registered population that was released annually from NSO, to obtain the mid-year population value (7).
The cumulative risk is the proportion of initially susceptible individuals in a population who become incident cases during a specified time, in the absence of other competing causes of death. The cumulative risk could be derived from the cumulative rate, which is the summation of each age-specific rate over each year of age, from birth to a defined upper age limit. In this report, we used 74 as the upper age limit.
RESULTS
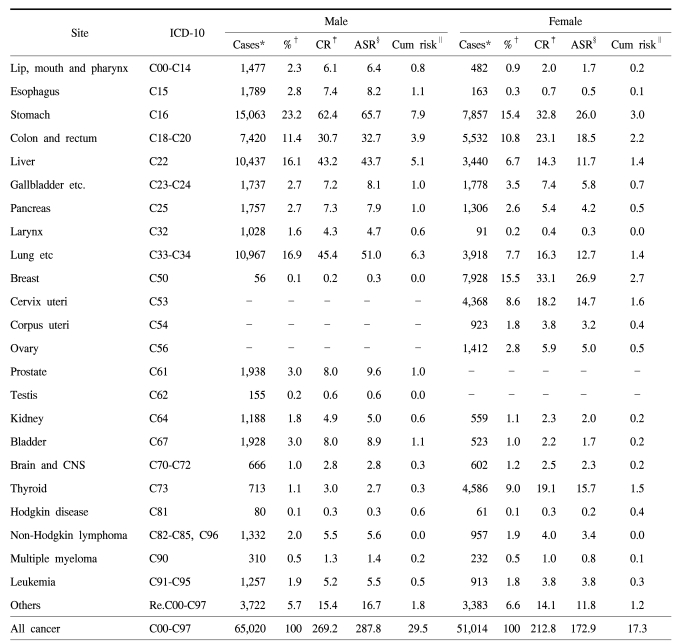
The overall CRs were 269.2 and 212.8 per 100,000 for males and females and the overall ASRs were 287.8 and 172.9 per 100,000, respectively. The overall cumulative risk for developing cancer before the age of 74 was 29.5% for males and 17.3% for females (Table 2). For males, the five leading primary cancer sites were stomach (CR 62.4, ASR 65.7), lung (CR 45.4, ASR 51.0), liver (CR 43.2, ASR 43.7), colon and rectum (CR 30.7, ASR 32.7), and prostate (CR 8.0, ASR 9.6). In females, the most common cancer sites were breast (CR 33.1, ASR 26.9), followed by stomach (CR 32.8, ASR 26.0), colon and rectum (CR 23.1, ASR 18.5), thyroid (CR 19.1, ASR 15.7), and the uterine cervix (CR 18.2, ASR 14.7).
Table 2.
Number of cancer cases for crude and age standardized incidence rates by gender in Korea during 2002
*the Total number of cases by site, †proportional frequency to the total of all cancer, ‡crude rate per 100,000 population, §the World age-standardized rate per 100,000 population, ∥cumulative risk up to age 74. Note: the sum of each %, CR, ASR, Cum risk may differ from the total of each value due to rounding-off error.
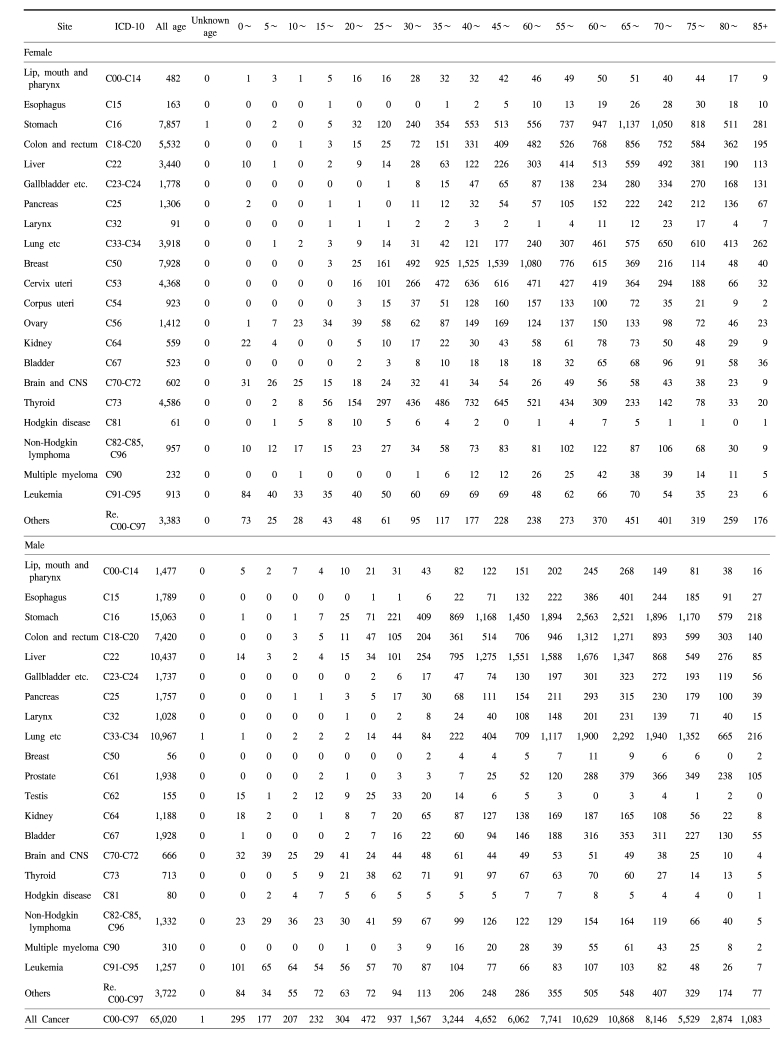
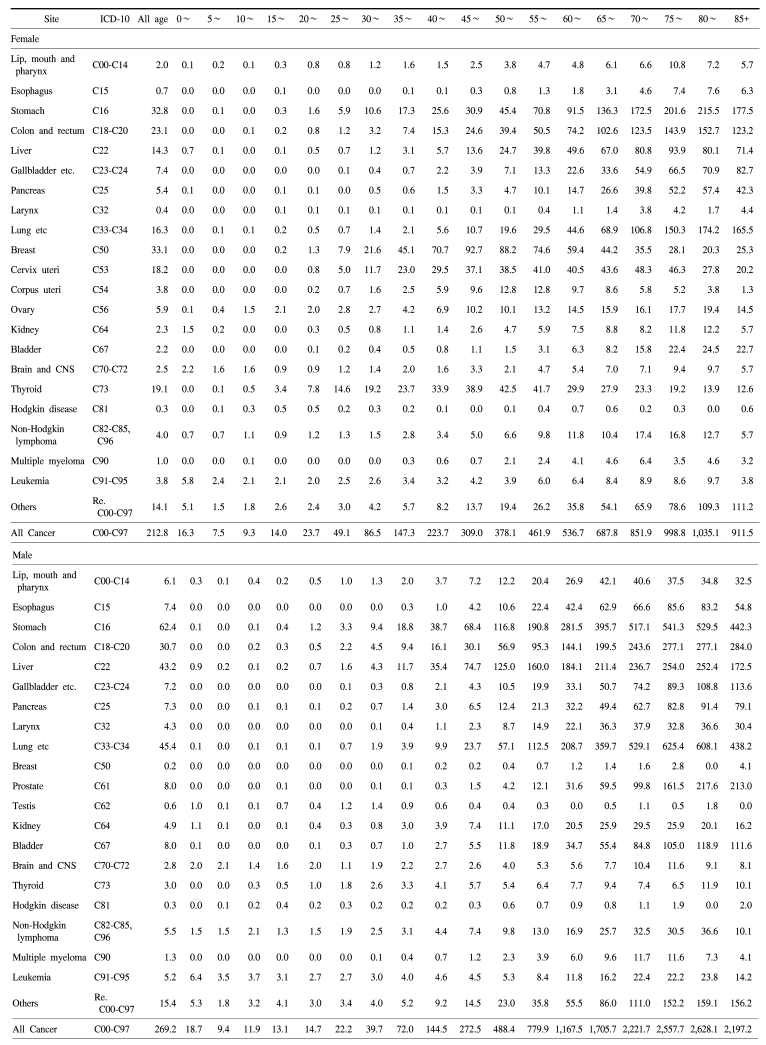
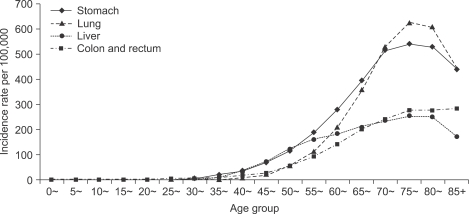
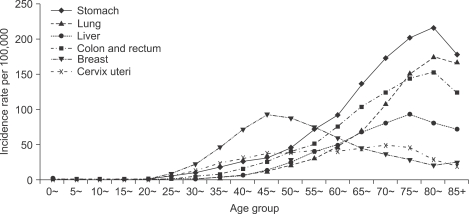
In the 0~14 age group, leukemia was the most common cancer in both genders. For males, stomach cancer was the most common cancer in the 15~64 age group, but lung cancer was more frequent in the over 65 age group. For females, thyroid cancer for the 15~34 age group, breast cancer for the 35~64 age group and stomach cancer among the over 65 group were the most common forms of cancer for each age group (Table 3, 4). Fig. 1 shows an age-specific incidence graph for the four major cancers in males. Fig. 2 shows an age-specific incidence graph for the six major cancers in females. The data shows that cancer incidence gradually increased with age, but there was some decline after 80.
Table 3.
Number of cancer cases by gender, age and primary site in Korea during 2002
Table 4.
Age-specific incidence rates per 100,000 population by gender and primary site in Korea during 2002
Fig. 1.
Age specific incidence rates of the four major cancers in males.
Fig. 2.
Age specific incidence rates of the six major cancers in females.
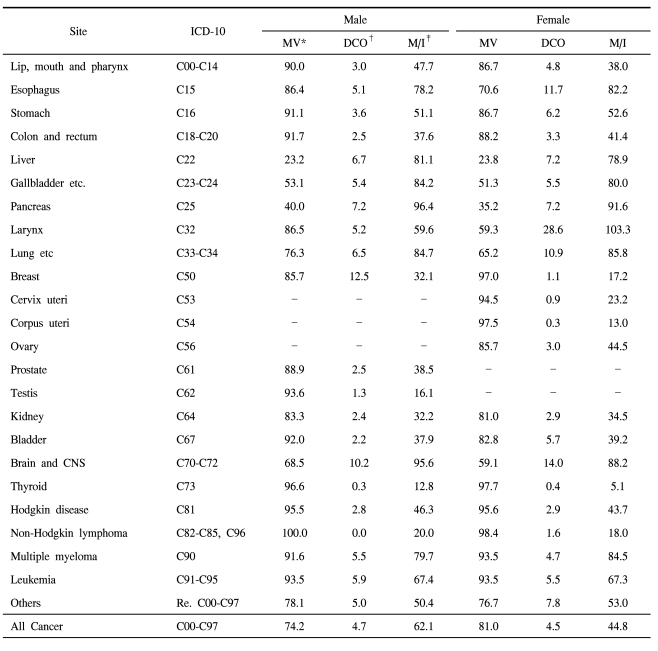
To assess the quality of the data in terms of completeness and validity, we examined several indices of quality (Table 5). The M : I ratios were 62.1% and 44.8% for males and females. We also evaluated the validity of the KNCIDB data using indices such as the percentages for the MV, DCO, PSU, and Age UNK. The MV% for the diagnosis was 74.2% for males and 81.0% for females. The DCO% was 4.7% for males and 4.5% for females. The PSU% was 1.9% for males and 1.9% for females. The Age UNK was one case for males and two cases for females.
Table 5.
Indices of data quality for the cancer incidence database in 2002 by gender Unit: %
*microscopically verified, †death certificate only, ‡mortality/incidence ratio.
DISCUSSION
Since the revision of the Cancer Act in October 2006, the annual cancer incidence rates have been available, based on the Statistics law. As shown in Table 1, three years are needed to report the annual rates with more complete data. The annual percent change of cancer cases increased by 4.8% (4.1% for males, 5.7% for females) during 1999~2002 (data not shown). We observed a pattern of cancer incidence for the most common cancer sites similar to the incidence from 1999~2001 published in 2005. Two-thirds of the cancer burden in males was from stomach, lung, liver, and colorectal cancers and two-thirds of the female cancer burden from stomach, breast, colorectal, cervix, lung, and liver cancers. However, in 2002, there was a significant increase of prostate cancer and of breast and thyroid cancers. Moreover, breast cancer was the most common cancer in women during 2002, and was the second most common cancer after stomach cancer in 2002.
Compared to the cancer incidence estimates (all cancers except skin) reported in the Globocan 2002 (8), the overall ASR (excluding skin) was 285.1 per 100,000 males; similar to the estimates for Korean men (285.7 per 100,000) and the estimates for Northern European men (283.1 per 100,000). However, the estimates were higher than the world average (209.6 per 100,000) males. In contrast, Korean females had an overall ASR higher than the world average (170.8 vs. 161.5 per 100,000 females) but lower than the Northern European average (252.3). In addition, it was slightly higher than that of Japan (167.4) and higher than the estimates for Korean women (155.3 per 100,000 females). The reported data in this paper is from the national population-based cancer registry and included in the publication "Cancer Incidence in Five continents, Volume IX" (9), therefore we should be cautious in comparing or in interpreting between the magnitude of cancer incidences among different countries and estimates, in terms of the completeness of cancer registration and quality indices.
For both genders, the ASRs of stomach, colon and rectum, liver, lung, and thyroid cancers were higher than the world average ASR.
For most cancers, the incidence increases with age. This trend begins to increase after the age of 30. However, there is some decline after the age of 80. This trend has been observed in the oldest age groups of other cancer registries. It is partly due to less efficient case ascertainment, some of which is a consequence of competing causes of mortality in the elderly, as well as a decrease in the proportion of the population predisposed to cancer (10).
It is essential to assess the quality of the data for completeness and validity. We evaluated the completeness and the validity of the data from the KNCIDB using indices such as the DCO%, the M : I ratio, the MV%, the PSU% and the Age UNK%. All values for these indices of our data were within the inclusion criteria of the Cancer Incidence in Five Continents, Volume IX, which was published on the IARC website in November 2007 (9). The standards for the DCO% from the North American Association of Central Cancer Registries (11) was less than 5% for the silver standard; that of the Canadian Cancer Registry (12) was less than 5% for the acceptable standard. For a DCO% higher than 15%, probable underreporting was considered as the cause of this value (13). Conversely, a very low DCO% (under 1%) might indicate that not all death certificates, with a diagnosis of cancer, were ascertained. According to these rules, the DCO% in this report (4.7% for males and 4.5% for females) was acceptable. The PSU% from the KNCIDB (1.9% for males and 1.9% for females) was acceptable by the standards of the Canadian Cancer Registry (0~8%) and relatively low compared to those of most other countries (9, 12). For the Age UNK%, which rarely exceeds 1% in developed countries, there were a few cases with unknown age in our data (males: 1 case, females: 2 cases).
Even though the completeness of incidence data was not calculated for this report, the medical record review for the unregistered cancer cases of the billing claims from NHIC since 1999 enhanced the completeness of cancer registration in Korea and improved the quality. The assessment of completeness of NCIDB is underway, with more than 5 years of incidence database.
Considering the magnitude of the incident cancer cases in this report and cancer mortality in 2002 (7), cancer is currently the most important public health problem in Korea. These numbers will continue to increase with the aging Korean population, even if age-specific rates remain constant. Further efforts to improve the quality of the data for cancer registration should be made by all registry staff, clinicians, pathologists, and policy makers to collect more accurate and timely information that can be used for evaluation and planning of cancer control activities in Korea.
CONCLUSIONS
Since the National Cancer Incidence Database was started, the annual percent change of cancer cases increased by 4.8% (4.1% for males, 5.7% for females) during 1999~2002. This value reflects the increase in prostate cancer for males and breast and thyroid cancer in females during 2002.
Further efforts to improve the quality of the data for cancer registration should be made by all registry staff, clinicians, pathologists, and policy makers to collect more accurate and timely information that can be used for evaluation and planning of cancer control activities in Korea.
Appendix 1.
The mean number of the mid-year population during the year 2002 in Korea and the world standard population
*World standard population: it is a theoretical proportion of world populations to use for standardization.
ACKNOWLEDGEMENT
The authors are deeply grateful to KCCR-affiliated Hospitals, non KCCR-affiliated Hospitals and staff members of the Busan, Daegu, Incheon, Gwangju, Daejeon, Ulsan, and Jeju-do Cancer Registries.
Footnotes
This work was supported by a grant 0710040-1 from the National Cancer Center and the 2007 National Health Promotion Program grant 0760100-1 from the Ministry of Health & Welfare, Republic of Korea.
References
- 1.Parkin DM. The evolution of the population-based cancer registry. Nat Rev Cancer. 2006;6:603–612. doi: 10.1038/nrc1948. [DOI] [PubMed] [Google Scholar]
- 2.Shin HR, Jung KW, Won WJ, Park JG. 139 KCCR-affiliated hospitals. 2002 Annual Report of the Korea Central Cancer Registry: based on registered data from 139 hospitals. Cancer Res Treat. 2004;36:103–114. doi: 10.4143/crt.2004.36.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Statistical Office in Korea. Annual report on the cause of death statistics (based on vital registration) Daejeon: National Statistical Office in Korea; 2007. [Google Scholar]
- 4.Shin HR, Won YJ, Jung KW, Kong HK, Yim SY, Lee J, et al. Nationwide cancer incidence in Korea, 1999-2001; first result using the National Cancer Incidence Database. Cancer Res Treat. 2005;37:325–331. doi: 10.4143/crt.2005.37.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Statistical Office. Annual report on the cause of death statistics (based on vital registration) 2003. [Google Scholar]
- 6.Ministry of Health and Welfare. Yearbook of health & welfare statistics. Korea: 2007. [Google Scholar]
- 7. Korean Statistical Information Service. 2007. [cited 2007/12/11]. Available from: http://www.kosis.kr/
- 8.Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2002 Cancer Incidence, Mortality and Prevalence Worldwide. 2.0 ed. Lyon: 2004. [Google Scholar]
- 9.Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, editors. Cancer incidence in five continents. Vol. IX. Lyon: IARC; 2007. IARC Scientific Publications No. 160. [Google Scholar]
- 10.Parkin DM. Comparability and quality control in cancer registration. International Agency for Research on Cancer; 1994. [Google Scholar]
- 11.Seiffert J North American Association of Central Cancer R, Registry Operations C. Standards for Completeness, Quality, Analysis, and Management of Data. North American Association of Central Cancer Registries; 2000. [Google Scholar]
- 12.Cormier M. User guide to data quality reports for provincial/Territorial Cancer Registries. 2005. [Google Scholar]
- 13.Jensen OM, Parkin DM, Maclennan R, Muir CS, Skeet RG, editors. Cancer Registration Principles and Methods. Lyon: IARC Scientific Publication; 1991. [Google Scholar]