Abstract
Purpose
To compare the efficacy between macular laser grid (MLG) photocoagulation and MLG plus intravitreal triamcinolone acetonide (IVTA; MLG+IVTA) therapy in diabetic macular edema (DME) patients.
Methods
A prospective, randomized, clinical trial was conducted of DME patients. A total of 60 eyes (54 patients) affected by DME were observed for a minimum of 6 months. Thirty eyes of 28 patients who received MLG treatment and 30 eyes of 26 patients who received the combined MLG+IVTA treatment were included in the study. Main outcome measures were BCVA and central macular thickness (CMT) as measured by optical coherence tomography (OCT) at 1, 3, and 6 months after treatment. Additionally, the authors examined retrospectively 20 eyes of 20 patients who were treated with only IVTA and compared with the 2 groups (MLG group and MLG+IVTA group).
Results
Baseline BCVA was 0.53±0.32 and CMT was 513.9±55.1 µm in the MLG group. At 1 and 3 months after treatment, the MLG group showed no significant improvement of BCVA and CMT, although there was significant improvement after 6 months. In the MLG+IVTA group, the baseline BCVA was 0.59±0.29 and CMT was 498.2±19.8 µm. After treatment, significant improvement of BCVA and CMT was observed at all follow-up time periods. When comparing the MLG group with the MLG+IVTA group, the latter had better results after 1 and 3 months, although at 6 months, there was no significant difference of BCVA and CMT between the 2 groups. Additionally, the IVTA group showed more improvement than the MLG group at 1 and 3 months but showed no significant difference at 6 months. In addition, the IVTA group showed no significant difference with the MLG+IVTA group at all follow-up time periods.
Conclusions
For DME patients, the combined MLG+IVTA treatment had a better therapeutic effect than the MLG treatment for improving BCVA and CMT at the early follow-up time periods. IVTA treatment alone could be an additional alternative therapeutic option to combined therapy.
Keywords: Central macular thickness, Diabetic macular edema, Diabetic retinopathy, Intravitreal triamcinolone acetonide injection, Macular laser grid photocoagulation
Diabetic macular edema (DME) is caused by the injury of the internal blood-retinal barrier. The permeability of the retinal capillary, the leakage of body fluid and the plasma component are increased and retained in the macula, and consequently, BCVA is deteriorated.1 According to the Early Treatment Diabetic Retinopathy Study (ETDRS) for the treatment of DME, macular laser grid (MLG) photocoagulation has been reported to be effective, but despite appropriate treatments, the result of a 3-year observation showed a deterioration of BCVA by at least 3 lines in approximately 15% of the patients.2-4 Steroids such as prostaglandin, that have been used to improve DME, suppress the synthesis of cytokines by controlling the inflammatory reaction and thus resulting in the reduction of vascular leakage and decreasing macular edema. Hence, the effect of decreasing central macular thickness (CMT) and improving BCVA can be obtained. Therefore, in the field of ophthalmology, a 4 mg/0.1 cc intravitreal injection of the hydrophobic crystallin cortisone triamcinolone acetonide used in inflammatory diseases has recently been used for diabetic macular treatment as well as various retinal diseases.5-7 In the present study the effectiveness of MLG applied conventionally to DME patients and the combination therapy with MLG plus intravitreal triamcinolone acetonide (IVTA; MLG+IVTA) were compared, and the side effects examined in DME patients who did not show distinct focal leakage in fluorescein angiography.
Materials and Methods
1. Research subjects
The study consisted of 60 eyes of 54 patients who visited the department of ophthalmology at our hospital with the chief complaint of BCVA deterioration diagnosed as DME by fundus examination, fluorescein angiography, and optical coherence tomography (OCT) from January 2006 to December 2006. The patients were divided into 2 groups according to their treatment. The first group consisted of 30 eyes of 28 patients treated with only MLG, and the second group consisted of 30 eyes of 26 patients treated with a combination of MLG+IVTA. The patients excluded from the present study had retinal vascular occlusion (i.e., CRVO, BRVO), vitritis, ARMD, tractional or rhegmatogenous retinal detachment, vitreous hemorrhage, severe macular ischemia, or intraocular treatment during the follow-up observation. Additionally, 20 eyes of 20 patients who were treated only with IVTA were retrospectively examined and compared with the other 2 groups.
2. Research methods
(1) Laser photocoagulation (grid laser therapy)
Grid laser therapy was performed after the dilation of the subject's eye (Mydrin-P® administered to the inferior conjunctival sac, at 10-minute intervals, 2 times), and the eye was anesthetized with 2% lidocain hydrochloride. Using a contact lens, with a setting of 50-200 µm light intensity and 0.1-0.2 seconds exposure time, the intensity was weaker than panretinal photocoagulation, and performed approximately at 1 laser burn intervals. The laser was irradiated on the area 500-3000 µm from the macular center at the thickened retina showing capillary blood vessel occlusion and considered to be the origin of the leakage in the focal diffusion leakage area as shown by fluorescence fundus angiography. In other words, the area showing initial hyperfluorescence was irradiated.
(2) Intravitreal triamcinolone injection
The subject's eye was anesthetized with 2% lidocain hydrochloride eye drops, and using 0.05% povidone iodine, the palpebra and the eye globe were sterilized. Triamcinolone was well shaken (40 mg/1 ml/vial), withdrawn with a 2 ml syringe and the needle placed facing the top. The triamcinolone was maintained for approximately 30 minutes for complete precipitation. Next, the supernatant was removed and saline in an equal amount to the removed supernatant was added, mixed well by shaking, and 0.1 ml was withdrawn with a 1 cc syringe. After wearing the speculum, using a 30 gauge needle, 4 mg (0.1 ml) triamcinolone was injected to the vitreous cavity through the inferotemporal pars plana, which is distanced from the limbus by 3.5 mm, and antibiotic eye drops administered (Cravit® Santen), followed by compressing the adjacent area for approximately 10 seconds with a sterile cotton swab.
(3) Measurement of corrected BCVA and CMT and data analysis
Baseline and follow-up examination was performed at 1, 3, and 6 months after treatment. Using the Snellen chart of the patient, best corrected BCVA (logMAR) was measured, intraocular pressure was measured using the Goldman application monometer, and using the OCT (STRATUS OCT model 3000, Carl Zees, California), CMT was measured 3 times. For the change of BCVA and CMT from baseline to the last follow-up after treatment, the Wilcox on Signed Rank test was applied, and for the comparison of BCVA as well as CMT of the MLG group with the MLG+IVTA group, the Mann-Whitney U test was applied. Only the IVTA group was retrospectively collected and compared with the above 2 groups using one-way ANOVA. A p-value of <0.05 was considered to be statistically different. The statistics program used was the SPSS program (Ver. 13.0, SPSS Inc., Chicago, IL, USA).
Results
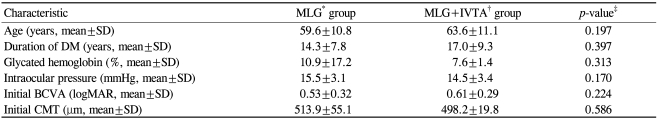
Among 28 patients (30 eyes) of the group treated with the MLG therapy, 12 patients (12 eyes) were male, 16 patients (18 eyes) were female, and the mean age was 59.6 years. The duration of diabetes was an average of 14.3 years. Among 26 patients (30 eyes) of the group treated with the combination of MLG+ IVTA, there were 10 male patients (11 eyes) and 16 female patients (19 eyes), with a mean age of 63.6 years. The duration of diabetes was an average of 17.0 years (Table 1). Between the 2 groups, mean age, the duration of diabetes, intraocular pressure, baseline BCVA, and baseline CMT were not statistically significantly different.
Table 1.
A baseline comparison between the study groups
*MLG=Macular laser grid photocoagulation; †MLG+IVTA=Macular laser grid photocoagulation+intravitreal triamcinolone injection group; ‡p-value measuredby Mann-Whitney U test.
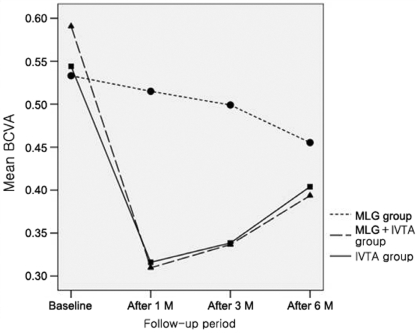
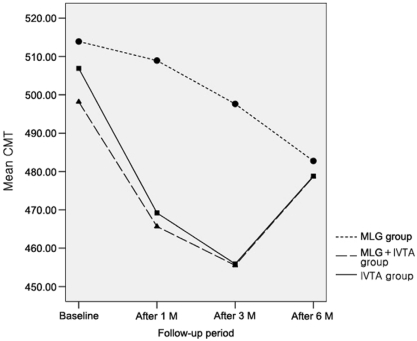
The effectiveness of the group treated with the MLG therapy was evaluated by the change of BCVA as well as CMT at baseline and 1, 3, and 6 months after treatment. Baseline BCVA was an average of 0.53±0.32, and BCVA at 1 and 3 months was 0.51 ±0.29 and 0.50±0.26, respectively. A statistically significant improvement of BCVA was not detected (p-value=0.255, 0.139). However, 6 months after treatment, the BCVA was improved to 0.46±0.19, and was statistically significant (p-value=0.01). Baseline CMT was an average of 513.9±55.1 µm. At 1 and 3 months after treatment, CMT was 508.9±32.9 µm and 497.6±18.6 µm, respectively, and a statistically significant change was not detected (p-value=0.253, 0.172). However, at 6 months after treatment, CMT was decreased to 482.8±14.5 µm, and was statistically significant (p-value=0.002). The mean BCVA of the group treated with the combination of MLG+IVTA was 0.59±0.29, and the average CMT was 498.2±19.8 µm. The mean BCVA at 1, 3, and 6 months was 0.31±0.21, 0.34±0.17, and 0.40 ±0.26 and was significantly improved (p-value<0.001, p-value<0.001, p-value<0.001), respectively. The mean CMT at 1, 3, and 6 months after treatment was 465.7±12.1 µm, 455.5±12.3 µm, and 478.7±9.0 µm, and all were significantly decreased (p-value<0.001, p-value 0.001, p-value<0.001), respectively (Fig 1, 2).
Fig. 1.
Graph illustrating BCVA(logMAR) in eyes affected with DME. In the MLG+IVTA and IVTA groups, compared with baseline, values were significantly lower at all time points (Wilcoxon signed ranks test). Compared with the MLG group, values for MLG+IVTA and IVTA groups were significantly lower at 1 and 3 months but had no difference 6 months after treatment. No difference was observed between the MLG+IVTA and IVTA groups (one-way ANOVA test).
Fig. 2.
Graph illustrating central macular thickness (CMT) in eyes-affected with DME. In the MLG+IVTA and IVTA groups, compared with baseline, values were significantly lower at all time points (Wilcoxon signed ranks test). Compared with the MLG, values for the MLG+IVTA and IVTA groups were significantly lower at 1 and 3 months but had no difference 6 months after treatment. No deference was observed between the MLG+IVTA and IVTA groups (oneway ANOVA test).
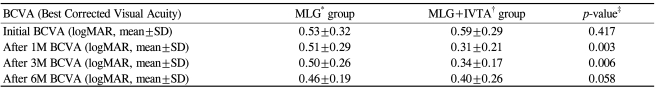
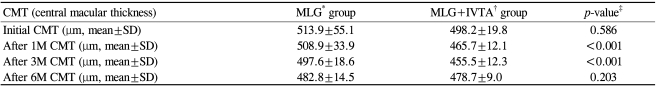
The effectiveness was compared by the level of change of BCVA and CMT of the 2 groups (MLG and MLG+IVTA). At 1 and 3 months after treatment, the mean BCVA of the MLG+IVTA group had significantly better results than the MLG group (p-value=0.003, 0.006). However, at 6 months after treatment, a statistically significant difference between the 2 groups was not detected (p-value=0.058) (Table 2).
Table 2.
Changes in BCVA (logMAR) obtained with different treatments in eyes affected with DME
*MLG=Macular laser grid photocoagulation; †MLG+IVTA=Macular laser grid photocoagulation+intravitreal triamcinolone injection group; ‡p-value measured by Mann-Whitney U test.
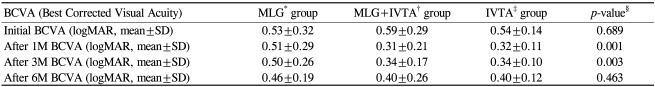
At 1 and 3 months after treatment, the mean CMT of the MLG+IVTA group showed a more statistically significant decrease than the MLG group (p-value<0.001, p-value<0.001, respectively), and at 6 months, a statistically significant difference between the 2 groups was not detected (p-value=0.203) (Table 3).
Table 3.
Changes in CMT obtained with different treatments in eyes affected with DME
*MLG=Macular laser grid photocoagulation; †MLG+IVTA=Macular laser grid photocoagulation+intravitreal triamcinolone injection group; ‡p-value measured by Mann-Whitney U test.
In both groups, no complication that seriously affects BCVA, such as retinal detachment, intravitreal hemorrhage, endopthalmitis, or epiretinal membrane, developed in any patient after treatment. Two weeks after treatment, only 15 eyes out of 60 eyes (25%) experienced a temporarily elevated intraocular pressure, which was normalized after the use of eye drops for glaucoma. During the 6-month follow-up period, no patient from either group had cataract surgery.
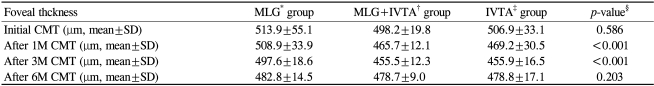
Additionally, the patients who received the IVTA treatment were retrospectively examined and compared with the other 2 groups (MLG group and MLG+IVTA group). Between the MLG and IVTA groups, the IVTA group had better visual acuity and CMT results at 1 and 3 months but no significant difference at 6 months after treatment. Additionally, between the MLG+IVTA and IVTA groups, there was no significant visual acuity and CMT difference at 1, 3 and 6 months after treatment (Table 4, 5).
Table 4.
Changes in BCVA (logMAR) obtained with different treatments in eyes affected with DME
*MLG=Macular laser grid photocoagulation; †MLG+IVTA=Macular laser grid photocoagulation+intravitreal triamcinolone injection; ‡IVTA=Intravitreal triamcinolone injection; §p-value measured by one-way ANOVA (tukey) test.
Table 5.
Changes in CMT obtained with different treatments in eyes affected with DME
*MLG=Macular laser grid photocoagulation; †MLG+IVTA=Macular laser grid photocoagulation+intravitreal triamcinolone injection; ‡IVTA=Intravitreal triamcinolone injection; §p-value measured by one-way ANOVA (tukey) test.
Discussion
DME has been shown to be caused by the increase of the permeability of retinal capillary blood vessels due to the injury of the internal blood-retina barrier caused by diabetes, resulting in the leakage of body fluid and plasma components.1 In addition, the increase of the secretion of cytokines such as prostaglandin within the retina, activation of VEGF and other growth factors, abnormality of the retinal pigment epithelium, and traction of the vitreous body, are thought to be involved in the development of DME. The purpose of DME treatment is to prevent the deterioration of visual acuity by recovering the thickened retina, and occasionally absorb hard exudates. Therefore, even if the visual acuity of the patient is good, as a prophylactic purpose, immediate treatment is recommended for the invasion to the macular center. As to the treatment methods for DME reported by the ETDRS, in the 5-year follow-up observation period of the group treated with local laser photocoagulation therapy, approximately 17% of patients showed improvement of visual acuity. Conversely, in the untreated group, only 11% of the patients showed improvement of visual acuity.3 Concerning focal laser photocoagulation therapy, the laser is irradiated to the thickened retina, targeting the lesion understood to be treatable as assessed by fundus angiography. Distinct hyperfluorescence or leakage points can be primarily detected by fluorescence angiogram, and if determined to be the cause of macular edema, such treatment is effective. However, in the diffused type of DME without distinct leakage points on the fluorescence angiograph, little improvement is observed.
MLG therapy performed for DME induces burn in the retinal pigment epithelial layer and thus temporarily destroys the lateral blood-retina barrier. The adjacent healthy retinal pigment epithelial cells proliferate and replace destroyed cells and thus allow recovery as a strong barrier within a few weeks. Inaddition, MLG therapy destroys a few optical cells, reduces the oxygen demand of the retinal lining, and thus reduces edema. The shortcoming of this type of MLG therapy is if the edema invaded the macular center, deterioration of visual acuity by laser therapy may occur, and due to the burn caused by laser, an inflammatory reaction is stimulated, and thus the permeability of the retinal capillary blood vessels may be somewhat increased.
Triamcinolone acetonide is a crystal type steroid that has been widely used in the field of ophthalmology, and has been reported by several studies that intravitreous injection is effective on the reduction of the macular thickness in DME and the improvement of visual acuity.5-11 Injection of triamcinolone is effective on the reduction of a proliferative retinal lesion by stabilizing the blood-retina barrier temporarily, which has been shown to suppress vascular endothelial growth factors that induce the increase of vascular permeability and prostaglandins that induce inflammatory reactions, thus decreasing vascular permeability, and reducing macular edema by the stabilization of the blood-retina barrier, and therefore improving visual acuity.12,13 Diverse dosages of triamcinolone for intravitreal injection from 1 mg up to 25 mg have been attempted. Nonetheless, when comparing treatment outcomes, the minimum dosage could minimize side effects, thus, the 4 mg presently utilized most often in clinics as well as used in the present study may be appropriate.5,6,14 However, triamcinolone injected to the vitreous body disappears approximately 3-6 months after the absorption of the drug, and the recurrence of macular edema afterward has been reported in several studies.15,16 In the combination therapy of grid laser therapy and triamcinolone injection, the reaction mechanism of each therapy to macular edema is different, hence, not only greater effects on the reduction of macular edema can be anticipated but also the stimulation of inflammatory reaction induced by grid laser could be prevented by the anti-inflammatory reaction of steroids, as investigated in several studies. Choi et al.17 have reported that in patients with simultaneous proliferative diabetic retinopathy and macular edema, by the administration of the combination therapy of pan retinal photocoagulation and intravitreal injection of triamcinolone, macular edema was reduced and the deterioration of macular edema caused by photocoagulation was prevented. In addition, Jeong et al.18 have reported that only in DME cases with a definite leakage point shown on fluorescence fundus angiography, the increased level of visual acuity by local laser therapy was higher and the maintenance was more effective. However, in DME cases without definite leakage points, laser therapy and steroid therapy showed comparable effects on the improvement of visual acuity, and for these cases, the combination of the 2 therapies was thought to possibly be more effective.
In the present study, both groups (MLG group and MLG+IVTA group) showed significant improvement of corrected visual acuity and the reduction of macular thickness on OCT 6 months after treatment. There was a difference in results between the 2 groups at 1 month and 3 months after treatment showing the MLG+IVTA group had better results in macular thickness as well as corrected visual acuity than the MLG group, and thus a rapid recovery rate. However, during the follow-up observation at 6 months after treatment, a statistically significant difference in corrected visual acuity as well as macular thickness was not shown between the 2 groups. As mentioned above, this result may bedue to the concentration of triamcinolone decreasing with time and thus decreasing its effect. Therefore, for a continuous effect, repeated intravitreal injection of triamcinolone is required, although in such cases, the risk of developing complications is high. The IVTA group had better results of visual acuity and CMT than the MLG group at 1 month and 3 months even though the IVTA group had no significant differences 6 months after treatment. In addition, only the IVTA group showed no significant differences with the MLG+IVTA group.
Complications known to be associated with the intravitreal injection of triamcinolone include the elevation of intraocular pressure, cataract, endophthalmitis, retinal detachment, vitreous hemorrhage, retinal venous occlusion, and choroidal hemorrhage with the elevation of intraocular pressure reported as the most common complication.19-21 Jonas et al.5 have reported that in 52% of patients treated with a 25 mg intraocular injection, intraocular pressure was elevated by more than 21 mmHg. Wingate et al.19 have reported that after a 4 mg intraocular injection, within 3 months the intraocular pressure was elevated by more than 5 mmHg in 30% of the patients. Nevertheless, all patients responded well to glaucoma eye drops, and normalized 6 months after treatment with no additional treatments required.
The present study showed similar results to the above-mentioned studies where during the follow-up period, the elevation of intraocular pressure higher than 21 mmHg was detected (15 out of 60 eyes; 25%), and all patients were controlled by glaucoma eye drop medication. However, in cases treated with repeated intravitreal injections, in addition to reversible complications such as the elevation of intraocular pressure, the risk of developing complications that may cause permanent adverse effects on the prognosis of the visual acuity in the future such as endophthalmitis and in severe cases blindness, is high. Although not detected in the subject groups of the present study, in the department of ophthalmology at our hospital, 2 eyes developed endophthalmitis after intravitreal injection of triamcinolone, and even after treatments, the prognosis of visual acuity was not favorable. Recently, studies attempting subtenon injection of triamcinolone in order to avoid the most severe side effects, endophthalmitis was performed and the outcomes reported, indicating future studies are necessary.22
Limitations of the present study include the small number of patients in the study subject groups and not considering the effect on the progression of cataracts in response to intravitreal injection of steroids as assessed by the division of subjects to the phakic eyes and the aphakic eyes prior to surgery which may influence the results. In addition, because only the IVTA group was comprised of retrospective data, comparison with prospective data (MLG group and MLG+IVTA group) could present a bias.
In conclusion, the present study suggests that the MLG+IVTA therapy had a better effect than the MLG-only treatment in the early follow-up time periods but had no difference in the late follow-up time periods. Additionally, the IVTA-only therapy can be used for an alternative to the combined IVTA+MLG therapy, because the IVTA-only treatment had no significant difference for all follow-up time periods studied.
References
- 1.Ryan Stephen J. Nonproliferative diabetic retinopathy. In: Chew Emily Y., Ferris Fredrick L., III, editors. Retina. 4th ed. v. 2. New York: Mosby, Elsevier Inc.; 2006. chap. 67. [Google Scholar]
- 2.Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 1. Arch Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 3.Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology. 1987;94:761–774. doi: 10.1016/s0161-6420(87)33527-4. [DOI] [PubMed] [Google Scholar]
- 4.Early Treatment Diabetic Retinopathy Study Research Group. Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Arch Ophthalmol. 1995;113:1144–1155. [PubMed] [Google Scholar]
- 5.Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920–927. doi: 10.1016/s0161-6420(02)00975-2. [DOI] [PubMed] [Google Scholar]
- 6.Jonas JB, Kreissig I, Sofker A, Degenring RF. Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol. 2003;121:57–61. [PubMed] [Google Scholar]
- 7.Massin P, Audren F, Haouchine B, et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology. 2004;111:218–224. doi: 10.1016/j.ophtha.2003.05.037. discussion 224-5. [DOI] [PubMed] [Google Scholar]
- 8.Jonas JB, Akkoyun I, Kreissig I, Degenring RF. Diffuse diabetic macular oedema treated by intravitreal triamcinolone acetonide: a comparative, non-randomised study. Br J Ophthalmol. 2005;89:321–326. doi: 10.1136/bjo.2004.046391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozkiris A, Evereklioglu C, Erkilic K, et al. Intravitreal triamcinolone acetonide injection as primary treatment for diabetic macular edema. Eur J Ophthalmol. 2004;14:543–549. [PubMed] [Google Scholar]
- 10.Sutter FK, Simpson JM, Gillies MC. Intravitreal triamcinolone for diabetic macular edema that persists after laser treatment: three-month efficacy and safety results of a prospective, randomized, double-masked, placebo-controlled clinical trial. Ophthalmology. 2004;111:2044–2049. doi: 10.1016/j.ophtha.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 11.Micelli Ferrari T, Sborgia L, Furino C, et al. Intravitreal triamcinolone acetonide: valuation of retinal thickness changes measured by optical coherence tomography in diffuse diabetic macular edema. Eur J Ophthalmol. 2004;14:321–324. [PubMed] [Google Scholar]
- 12.Floman N, Zor U. Mechanism of steroid action in ocular inflammation: inhibition of prostaglandin production. Invest Ophthalmol Vis Sci. 1977;16:69–73. [PubMed] [Google Scholar]
- 13.Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992;110:1155–1159. doi: 10.1001/archopht.1992.01080200135041. [DOI] [PubMed] [Google Scholar]
- 14.Antcliff RJ, Spalton DJ, Stanford MR, et al. Intravitreal triamcinolone for uveitic cystoid macular edema: An optical coherence tomography study. Ophthalmology. 2001;108:765–772. doi: 10.1016/s0161-6420(00)00658-8. [DOI] [PubMed] [Google Scholar]
- 15.Schindler RH, Chandler D, Thresher R, Machmer R. The clearance of intravitreal triamcinolone acetonide. Am J Ophthalmol. 1982;93:415–417. doi: 10.1016/0002-9394(82)90130-1. [DOI] [PubMed] [Google Scholar]
- 16.Beer PM, Bakri SJ, Singh RJ, et al. Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology. 2003;110:681–686. doi: 10.1016/S0161-6420(02)01969-3. [DOI] [PubMed] [Google Scholar]
- 17.Choi KS, Chung JK, Lim SH. Laser photocoagulation combined with intravitreal triamcinolone acetonide injection in proliferative diabetic retinopathy with macular edema. Korean J Ophthalmol. 2007;21:11–17. doi: 10.3341/kjo.2007.21.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong YC, Bae SH, Kim JW. Comparison of effects of IVTA and photocoagulation, depending on types of diabetic macular edema. J Korean Ophthalmol Soc. 2007;48:655–664. [Google Scholar]
- 19.Wingate RJ, Beaumont PE. Intravitreal triamcinolone and elevated intraocular pressure. Aust N Z J Ophthalmol. 1999;27:431–432. doi: 10.1046/j.1440-1606.1999.00238.x. [DOI] [PubMed] [Google Scholar]
- 20.Moshfeghi DM, Kaiser PK, Scott IU, et al. Acute endophthalmitis following intravitreal triamcinolone acetonide injection. Am J Ophthalmol. 2003;136:791–796. doi: 10.1016/s0002-9394(03)00483-5. [DOI] [PubMed] [Google Scholar]
- 21.Nelson ML, Tennant MT, Sivalingam A, et al. Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina. 2003;23:686–691. doi: 10.1097/00006982-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Thomas ER, Wang J, Ege E, et al. Intravitreal triamcinolone acetonide concentration after subtenon injection. Am J Ophthalmol. 2006;142:860–861. doi: 10.1016/j.ajo.2006.05.023. [DOI] [PubMed] [Google Scholar]