Abstract
Introduction
Coronary artery dissections with or without rupture is a rare but well-recognized complication of coronary angiography with a high morbidity and mortality rate.
Case presentation
We present a rare case of right coronary artery dissection distal to a totally occluded vessel. The vessel dissected during the second injection of contrast agent without any direct mechanical manipulation (catheter or guide-wire induced). Hopefully the dissection had no clinical consequences and the patient was discharged after 48 hour intensive monitoring.
Conclusions
We believe that the contrast agent that was forced in the proximal part of the RCA increased through the anastomotic branches the sheer stress on the diseased endothelium of the distal artery causing it to dissect. It is an instructive -not previously described- phenomenon that underscores that atherosclerotic tissue is unpredictable and should be treated with extreme caution.
Introduction
Extensive coronary artery dissections with or without rupture occasionally occur during percutaneous interventions [1-3]. It is more commonly in the right than in the left coronary artery probably due to histological differences in the proximal vessel [4]. Dissection is usually guide-catheter, guide-wire or balloon inflation induced, and it further propagates by contrast injection and/or coronary flow [1-4]. Conservative treatment may be adequate for limited dissections. Extensive dissections with pericardial extravasation require immediate treatment. Although emergency coronary artery by pass grafting (CABG) is effective, it is a time consuming procedure that entails the risk of irreversible myocardial damage. The use of covered stents has obviated the need of high risk emergency surgery [2,4].
Case presentation
We report the case of a 72-year-old Caucasian male, referred to our department for further investigation of recent-onset effort angina. He was a non-smoker, hypertensive and dyslipidemic patient under treatment with ACE inhibitor and statin. No parental history of cardiovascular disease was reported to us.
On admission he was free of symptoms at rest and he had a relatively normal clinical examination. He also had a normal chest X-ray, and laboratory tests yielded no unusual findings besides alter lipoprotein levels (predominantly low HDL).
The patient was subjected to SPECT myocardial perfusion imaging before and after Bruce protocol graded exercise stress test. During the second stage of exercise stress test the patient reported mild chest discomfort and he gradually developed down-sloping ST depression of approximately 1.5 mm at the inferior leads. Exercise was halted at 6:02 due to patient’s fatigue.
SPECT myocardial perfusion imaging revealed an exercise-induced significant inferio-lateral perfusion defect.
The patient was then subjected to coronary angiography (CA), which yielded total occlusion of right coronary artery proximally. The distal part of the artery was well perfused by a wide network of anastomotic branches interconnected to the proximal part of RCA. A lesion in the proximal left anterior descending artery (LAD) was also noted. The lesion compromised the 50% of the arterial lumen diameter. The ejection fraction was normal. The patient was put on aspirin, beta-blocker and calcium channel antagonist and he was discharged 24 hours later. On regular follow-up he was in good condition and did not report any symptoms.
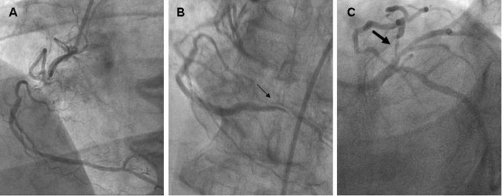
Eight months later and while still on optimal anti-aginal treatment the patient reported relapse of effort angina. He was admitted to our department and he was re-subjected to a CA. The severity of the LAD lesion was subsequently worsened (Figure 1C), while the anatomy of RCA was unchanged (Figure 1A). However on the second attempt to visualize the RCA from the left anterior oblique view, the vessel dissected distally to the total occlusion (Figure 1B and Video 1). Hopefully, the patient remained symptom-free, and hemodynamically stable. Moreover, since the dissection occurred distal to a totally occluded artery, any percutaneous intervention in the dissected lesion was technically impossible. Therefore, the patient was admitted in the intensive care unit and was discharged after 48 hours monitoring. He was referred to the cardiothoracic surgery department for further management of the LAD stenosis which was considered as the symptom-related lesion.
Figure 1.
Coronary angiography yielded total occlusion of right coronary artery proximally. The distal part of the artery was perfused by a wide network of anastomotic branches interconnected to the proximal part of right coronary artery (A). The second attempt to visualize the right coronary artery resulted in dissection of the vessel distal to the total occlusion (B). A lesion in the proximal left anterior descending artery was also noted. The lesion compromised the 90% of the arterial lumen diameter (C).
Discussion
Coronary angiography has become a routine diagnostic procedure in current clinical practice. Complications are uncommon, but still occur during CA and in some instances they can be life-threatening. Catheter-induced dissection of a coronary artery is a rare but well-recognized complication of CA with a high mortality rate if it is left untreated [5,6].
The exact mechanism of iatrogenic coronary artery dissection (ICAD) is not clear. It has been related to vigorous hand-injection of contrast medium, subintimal passage of the guide-wire, or inappropriate handling of the guide-wire catheter [4]. In all instances mechanical straining and shearing forces during CA result in increased wall stress. The atherosclerotic-dysfunctional relatively rigid arterial wall is prone to rapture and can easily dissect if not treated with care [1-5].
Nevertheless, in our case no direct manipulation of the distal part of the vessel could have been performed since it was proximally occluded and no guide-wire was inserted distally to the occlusion. It is however plausible that the contrast agent that was forced in the proximal part of the RCA increased through the anastomotic branches the sheer stress on the diseased endothelium of the distal artery causing it to dissect. Hopefully, the clinical stability of the patient made unnecessary any intervention in the dissected vessel. However the outcome might not have been favorable if the dissection had been complicated with rapture. It would be technically challenging if not impossible the placement of a covered stent at the dissected vessel while surgical treatment of the dissection-a more technically feasible alternative- would have been time consuming.
In conclusion, we report a case of iatrogenic coronary artery dissection distal to a totally occluded RCA. Such a complication has never been reported before and it was rather instructive. It puts forward that injection of contrast medium should be performed with extreme caution especially in patients with severe coronary artery disease. It also reminds that direct mechanical manipulation is not the only way to cause coronary artery dissection.
Abbreviations
- ACE
angiotensin-converting enzyme
- CA
coronary angiography
- CABG
coronary artery bypass graft
- HDL
high density lipoprotein
- ICAD
iatrogenic coronary artery dissection
- LAD
left anterior descending
- RCA
right coronary artery
- SPECT
single photon emission computed tomography
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the journal’s Editor-in-Chief.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SA wrote the manuscript and edited the images. DA performed and interpreted the coronary angiography. KL and ST suggested the presentation of this case and reviewed the manuscript. All authors read and approved the manuscript.
This article is available from: http://casesjournal.com/casesjournal/article/view/6797
Contributor Information
Demetrios Antoniades, Email: cardiologiki@nimts.gr.
Stavros Apostolakis, Email: stavrosapos@hotmail.com.
Spiros Tzoras, Email: sptzoras@hotmail.com.
Kyriakos Lazaridis, Email: cardiologiki@nimts.gr.
Supplementary file
The video (MP4 – 4.2MB) can be accessed here: http://casesjournal.com/casesjournal/article/downloadSuppFile/6797/19302
References
- Connors JP, Thanavaro S, Shaw RC, Sandza JG, Ludbrook PA, Krone RJ. Urgent myocardial revascularization for dissection of the left main coronary artery: a complication of coronary angiography. J Thorac Cardiovasc Surg. 1982;84:349–352. [PubMed] [Google Scholar]
- Mulvihill NT, Boccalatte M, Fajadet J, Marco J. Catheter-induced left main dissection: a treatment dilemma. Catheter Cardiovasc Interv. 2003;59:214–216. doi: 10.1002/ccd.10481. [DOI] [PubMed] [Google Scholar]
- Awadalla H, Salloum JG, Smalling RW, Sdringola S. Catheter-induced dissection of the left main coronary artery with and without extension to the aortic root: a report of two cases and a review of the literature. J Interv Cardiol. 2004;17:253–257. doi: 10.1111/j.1540-8183.2004.00381.x. [DOI] [PubMed] [Google Scholar]
- El-Jack SS, Pornratanarangsi S, Webster MW. Images in cardiology. Covering your mistakes: PTFE covered stents in iatrogenic coronary artery dissection. Heart. 2006;92:68. doi: 10.1136/hrt.2005.071985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Robles JA, Garcia E, Rico M, Esteban E, Perez de Prado A, Delcan JL. Emergency coronary stenting for acute occlusive dissection of the left main coronary artery. Cathet Cardiovasc Diagn. 1993;30:227–229. doi: 10.1002/ccd.1810300310. [DOI] [PubMed] [Google Scholar]
- Kennedy JW, Baxley WA, Bunnel IL, Gensini GG, Messer JV, Mudd JG, Noto TJ, Paulin S, Pichard AD, Sheldon WC, Cohen M. Mortality related to cardiac catheterization and angiography. Cathet Cardiovasc Diagn. 1982;8:323–340. doi: 10.1002/ccd.1810080402. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video (MP4 – 4.2MB) can be accessed here: http://casesjournal.com/casesjournal/article/downloadSuppFile/6797/19302