Abstract
Introduction
The present case reports highlight the peculiar aspect of Klebsiella pneumoniae liver abscess, an emerging disease in United States and Western countries.
Case presentation
We report two cases of Asiatic patients with Klebsiella-associated liver abscesses evaluated at our institution over a one-year period. Both of them had non-specific clinical symptoms at presentation, a peculiar ultrasonographic appearance and successful treatment with early percutaneous drainage.
Conclusion
Klebsiella related liver abscess is an emerging disease with peculiar clinical features. As compared with other bacterial liver abscesses, Klebsiella pneumonia associated pyogenic liver abscess has distinctive risk factors, unique ultrasonographic and computed tomography features and different prognosis.
Introduction
Pyogenic liver abscess (PLA) is a potentially life-threatening disease that may be caused by bacterial or fungal organisms. The most common bacteria isolated from liver abscess patients are gram-negative rods. Until the end of the last century, Escherichia coli was recognized as the predominant cause of bacterial liver abscesses [1], but more recently Klebsiella pneumoniae was found to be the leading pathogen in Asia and Western countries [2,3].
Here we describe two cases of Klebsiella-associated PLA who were investigated and successfully treated in our department.
Case presentation
Case report 1
A 29 year old Indian man reported a 4-day history of fever, chills and fatigue. He was previously in good health. He immigrated to Italy nine years before. He denied any recent foreign travel.
On general examination temperature was 40°C; pulmonary, cardiac and abdominal examinations revealed no abnormality. Laboratory tests were remarkable for a leukocytosis (14040 cells/mm3), total bilirubin 1.6 mg/dl, alanine transferase 100 U/L, aspartate transferase 69 U/L. Chest X-ray showed an elevated right hemidiaphragm. The patient was empirically treated with intravenous levofloxacin and ceftriaxone but spiking fever persisted.
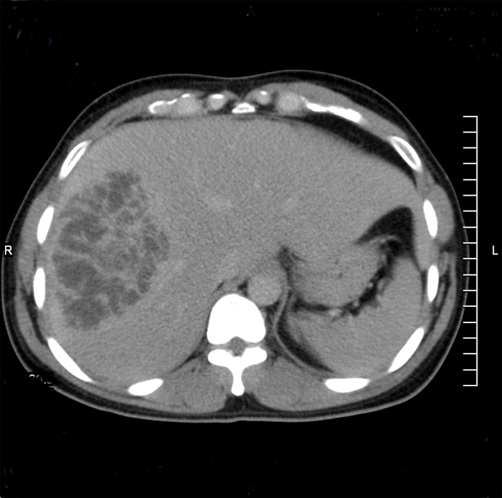
Three days after hospitalization the patient developed right upper quadrant abdominal pain. An abdominal ultrasound (US) revealed a 10 cm diameter lesion in the right lobe of the liver. A Computed Tomography (CT) scan showed a 10 cm hypodense lesion with internal septa (Figure 1). A US-guided percutaneous drainage was placed yielding 150 cc of purulent fluid, but no pathogen was isolated from cultures of aspirated pus. Entamoeba histolytica serology was negative. Two out of three blood cultures grew Klebsiella pneumoniae resistant to levofloxacin. Therefore, the patient was given intravenous gentamicin and metronidazole.
Figure 1.
Computed Tomography scan of a 29 year old man with Klebsiella pneumoniae liver abscess. Abdominal Computed Tomography scan showing a 10 cm diameter Klebsiella related abscess. Notice, as a distinctive feature, the hypodense lesion with internal septa and irregular margins.
This therapy led to a clinical improvement and percutaneous drainage was removed. An abdominal US before discharge revealed significant reduction in abscess size. The patient was discharged and antibiotics were switched to oral ciprofloxacin and metronidazole for a 6-week course. A follow-up US after antibiotic therapy showed resolution of the abscess. Patient turned to his usual state of health.
Case report 2
A 76 year old Chinese man presented with a 5-day history of spiking fever and chills. He was previously in good health; past medical history revealed a cholecystectomy for cholelithiasis ten years before.
General examination showed significant hypotension (85/50 mmHg) and a temperature of 41°C; the remainder of his examination was unremarkable. Laboratory tests revealed elevated C Reactive Protein (31 mg/dl; normal value<1), abnormal serum creatinine (1.8 mg/dl), aspartate transferase (139 U/L), alanine transferase (110 U/L), phosphatase alkaline (823 U/L) and total bilirubin (2.12 mg/dl). The patient was treated with fluids and empiric antibiotic therapy with Piperacillin-Tazobactam was started.
Abdominal US showed a 3 cm diameter lesion in the right lobe of the liver. Abdominal CT scan confirmed the presence of a 3 cm hypodense lesion with irregular margins strongly suspicious for metastatic liver neoplasm. A percutaneous drainage catheter was placed. Diagnostic aspiration of the lesion yielded 50 cc of purulent material that grew Klebsiella pneumoniae. Three blood cultures grew Klebsiella pneumoniae sensitive to all antibiotics. Entamoeba histolytica serology was negative.
Patient's clinical conditions improved; an abdominal US before discharge showed complete resolution of liver abscess. Patient was discharged and treated as an outpatient with levofloxacin and metronidazole for 4 weeks.
Conclusions
First reported from Taiwan as a solitary organism in PLA [4], in recent studies Klebsiella pneumoniae was recognized as the leading pathogen of PLA in Asia and Western countries [2,3]. Furthermore, it was found to be associated with Asian ethnicity, diabetes mellitus and cryptogenic liver abscesses [2,3,5]. Conversely, the presence of biliary disease and coexisting malignancy was recognized as a predictive parameter of Escherichia coli PLA [3].
Patients often complain of vague constitutional symptoms, such as fever and fatigue, while only one-half of cases presents with more specific clinical clues as right upper quadrant pain, jaundice and hepatomegaly [2,6]. Only non-specific clinical symptoms were identified in our cases, even in the first patient who had such a large PLA (10 cm). For this reason the absence of right upper abdominal quadrant findings does not exclude a liver abscess. Moreover a PLA should always be considered in the differential diagnosis of a fever of unknown origin.
Distinctive US and CT features have been reported in Klebsiella pneumoniae PLA [7,8]. A predominantly solid US appearance of the lesion with irregular margins was observed in Klebsiella-associated liver abscesses, possibly due to their failure of liquefaction [7]. As compared with other bacterial abscesses, a smaller quantity of pus obtained at initial aspiration was reported in Klebsiella PLA [7], which can be related to their predominant solid consistency made up of aggregation of multiple locules that do not communicate. These features were observed in our patients, particularly in the second one where a liver neoplasm was considered in the differential diagnosis.
Some studies showed a better prognosis for patients with Klebsiella-associated PLA than for other bacterial liver abscesses [4,9]. However, a higher incidence of metastatic infections at other sites was shown in patients with Klebsiella related PLA [9]. The most common manifestations of metastatic infection are endophthalmitis, meningitis and brain abscess [10]. Major virulence factors of Klebsiella pneumoniae were shown to be associated with a metastatic disease. Capsular K1 serotype is a significant virulence determinant for the development of septic ocular and central nervous system complications from PLA [10]. Furthermore a number of clinical studies pointed to a relationship between the hypermucoviscosity phenotype of Klebsiella pneumoniae and the presence of an invasive disease with metastatic infection [11]. Klebsiella pneumoniae strains possess the hypermucosviscosity phenotype if they are capable of producing a mucoviscous exopolysaccharide web. In the microbiology laboratory, these strains grow in sticky colonies on agar plates and are identified by a string test. Although diabetes mellitus was recognized as a major risk factor for Klebsiella related PLA, the data are conflicting as to whether it is associated with an invasive and metastatic infection [10]. None of our patients had diabetes mellitus, none of them experienced ocular or neurologic complications.
A significant reduction of mortality has occurred for all pyogenic liver abscesses since 1950, possibly related to the advent of percutaneous drainage and broad spectrum antibiotics [12]. In contrast with amoebic abscess, drainage of pyogenic abscess is essential in most cases. This issue is emphasized by Cheng et al. (2003) [13] who observed that early drainage can significantly improve prognosis. Percutaneous drainage is a relatively low-risk and effective method. It has gradually replaced surgical procedures since it was shown to reduce costs and length of hospital stay [14]. Surgical drainage should be considered in patients with multiple and large liver abscesses and when there is no response to percutaneous drainage [15]. In addition to drainage, treatment of Klebsiella liver abscess requires parenteral antibiotics. Since community-acquired Klebsiella strains are resistant to first generation cephalosporin and ampicillin but rarely produce extended-spectrum beta-lactamases (ESBL), a combination of an extended spectrum beta-lactam and an aminoglycoside is the preferred regimen. Although aminoglycosides penetrate the abscess cavity poorly, they can rapidly eradicate organisms in the bloodstream and decrease the risk of metastatic infections.
List of abbreviations
- CT
Computed Tomography
- ESBL
extended-spectrum beta-lactamases
- PLA
Pyogenic liver abscess
- US
Ultrasound
Consent
Written informed consent was obtained from the patients for publication of these case reports and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors' contribution
FC was a major contributor in writing the manuscript; LF was involved in diagnosing and managing the disease; VR performed abdominal Computed Tomography; GR was a major contributor in writing the manuscript; MD was involved in diagnosing and managing the disease; TM performed abdominal ultrasound; RF was a major contributor in writing the manuscript.
This article is available from: http://casesjournal.com/casesjournal/article/view/6879
Contributor Information
Francesco Casella, Email: case.5@libero.it.
Luigi Finazzi, Email: lfinazzi@yahoo.com.
Valentina Repetti, Email: vale84@libero.it.
Giampaolo Rubin, Email: rubin64@libero.it.
Maria DiMarco, Email: mariadimarco@libero.it.
Tiziana Mauro, Email: tizianamauro@libero.it.
Raffaello Furlan, Email: raffaello.furlan@unimi.it.
References
- Alvarez Perez JA, Gonzalez JJ, Baldonedo RF, Sanz L, Carreno G, Junco A, Rodriguez JI, Martinez MD, Jorge JI. Clinical course, treatment, and multivariate analysis of risk factors for pyogenic liver abscess. Am J Surg. 2001;181:177–186. doi: 10.1016/S0002-9610(00)00564-X. [DOI] [PubMed] [Google Scholar]
- Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39:1654–1659. doi: 10.1086/425616. [DOI] [PubMed] [Google Scholar]
- Chen SC, Wu WY, Yeh CH, Lai KC, Cheng KS, Jeng LB, Wang PH, Lin DB, Chen CC, Lee MC, Bell WR. Comparison of Escherichia coli and Klebsiella pneumoniae liver abscesses. Am J Med Sci. 2007;334:97–105. doi: 10.1097/MAJ.0b013e31812f59c7. [DOI] [PubMed] [Google Scholar]
- Wang JH, Liu YC, Lee SS, Yen MY, Chen YS, Wann SR, Lin HH. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin Infect Dis. 1998;26:1434–1438. doi: 10.1086/516369. [DOI] [PubMed] [Google Scholar]
- Choi HY, Cheon GJ, Kim YD, Han KH, Kim KS, Nah BK. Comparison of clinical characteristics between cryptogenic and biliary pyogenic liver abscess. Korean J Gastroenterol. 2007;49:238–244. [PubMed] [Google Scholar]
- Chan KS, Yu WL, Tsai CL, Cheng KC, Hou CC, Lee MC, Tan CK. Pyogenic liver abscess caused by Klebsiella pneumoniae: analysis of the clinical characteristics and outcomes of 84 patients. Chin Med J (Engl) 2007;120:136–139. [PubMed] [Google Scholar]
- Hui JY, Yang MK, Cho DH, Li A, Loke TK, Chan JC, Woo PC. Pyogenic liver abscesses caused by Klebsiella pneumoniae: US appearance and aspiration findings. Radiology. 2007;242:769–776. doi: 10.1148/radiol.2423051344. [DOI] [PubMed] [Google Scholar]
- Kim SB, Je BK, Lee KY, Lee SH, Chung HH, Cha SH. Computed tomographic differences of pyogenic liver abscesses caused by Klebsiella pneumoniae and non-Klebsiella pneumoniae. J Comput Assist Tomogr. 2007;31:59–65. doi: 10.1097/01.rct.0000224629.48068.69. [DOI] [PubMed] [Google Scholar]
- Yang CC, Yen CH, Ho MW, Wang JH. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004;37:176–184. [PubMed] [Google Scholar]
- Fang CT, Lai SY, Yi WC, Hsueh PR, Liu KL, Chang SC. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007;45:284–293. doi: 10.1086/519262. [DOI] [PubMed] [Google Scholar]
- Lee HC, Chuang YC, Yu WL, Lee NY, Chang CM, Ko NY, Wang LR, Ko WC. Clinical implications of hypermucoviscosity phenotype in Klebsiella pneumoniae isolates: association with invasive syndrome in patients with community-acquired bacteraemia. J Intern Med. 2006;259:606–614. doi: 10.1111/j.1365-2796.2006.01641.x. [DOI] [PubMed] [Google Scholar]
- Lederman ER, Crum NF. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol. 2005;100:322–331. doi: 10.1111/j.1572-0241.2005.40310.x. [DOI] [PubMed] [Google Scholar]
- Cheng HP, Siu LK, Chang FY. Extended-spectrum cephalosporin compared to cefazolin for treatment of Klebsiella pneumoniae-caused liver abscess. Antimicrob Agents Chemother. 2003;47:2088–2092. doi: 10.1128/AAC.47.7.2088-2092.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng DL, Liu YC, Yen MY, Liu CY, Shi FW, Wang LS. Pyogenic liver abscess: clinical manifestations and value of percutaneous catheter drainage treatment. J Formos Med Assoc. 1990;89:571–576. [PubMed] [Google Scholar]
- Tan YM, Chung AY, Chow PK, Cheow PC, Wong WK, Ooi LL, Soo KC. An appraisal of surgical and percutaneous drainage for pyogenic liver abscesses larger than 5 cm. Ann Surg. 2005;241:485–490. doi: 10.1097/01.sla.0000154265.14006.47. [DOI] [PMC free article] [PubMed] [Google Scholar]