Abstract
Introduction
Wireless capsule endoscopy is an important tool for minimally invasive evaluation of the small bowel, allowing improved diagnostic yield with low complication rates relative to traditional modalities. Recently however, reports on small bowel perforation after wireless capsule endoscopy have surfaced. Here we present the first case of acute small bowel perforation in a middle-aged male in the United States.
Case presentation
A 58-year-old male with a presumed quiescent history of Crohn’s Disease presented to the Emergency Department in a septic state 48 hours after a wireless capsule endoscopy procedure complaining of abdominal pain, distension, and frequent emesis. A computed tomography scan of the abdomen was suggestive of small bowel perforation and ischemic enteritis. The patient was adequately resuscitated and taken to the operating room for an ileocecectomy and extensive resection of the small bowel. Pathology of the resected specimen revealed an ileal stricture and associated necrotizing ileitis, and a perforation just proximal to the stricture.
Conclusion
Wireless capsule endoscopy remains the preferred endoscopic imaging method of the small bowel. This case illustrates the importance of appropriate patient selection and evaluation of functional patency of the small bowel prior to wireless capsule endoscopy, especially with the growing role of this procedure in the evaluation of inflammatory bowel disease.
Introduction
Since its conception in 2000, wireless capsule endoscopy (WCE) has become an established tool for minimally invasive evaluation of the small bowel (SB). Today WCE is most commonly utilized for evaluation of obscure GI bleeding unidentified by traditional endoscopic techniques [1]. In recent years however, an advancing body of literature advocating the use of WCE in the diagnosis and management of inflammatory bowel disease (IBD) has emerged. Studies have reported on the utility of WCE for the initial diagnosis and staging of Crohn’s Disease (CD), evaluation of post-operative CD, assessment of treatment efficacy, and investigation of patients with indeterminate colitits [2-4].
While WCE is a generally safe and well tolerated procedure in patients with IBD, it does carry the potential for serious complications. Capsule retention is a well recognized complication occurring at a higher frequency in patients with known or suspected CD [1]. Capsule impaction leading to clinical SB obstruction has also been reported in the literature as a serious complication requiring immediate surgical intervention [5]. Three cases of SB perforation after WCE have recently been reported in the elderly, two involving patients with CD [6-8]. Recipi et al. describe an acute SB perforation in an 82 year old male with suspected CD, while Um et al. report a SB perforation in a 75 year old female with well established active CD 17 days post-procedure. Here we report the first case of acute SB perforation after WCE in the United States in a patient with a presumed quiescent history of CD.
Case presentation
A 58-year-old Caucasian male with a reported 30 year history of CD presented to his gastroenterologist with intermittent diarrhea controlled by bismuth subsalicylate (Kaopectate). He denied any recent flares or pharmacologic management. A colonoscopy was negative for classical findings of CD and the patient next underwent WCE to document possible disease in the SB. On the evening of the procedure the patient reported poorly localized abdominal pain and copious non-bilious/non-bloody emesis. Over the next 48 hours he experienced progressive abdominal distention and presented to the Emergency Department. He denied the chronic use of NSAIDs or a history of prior abdominal operations.
On admission the patient was febrile, tachycardic and tachypneic. He also presented with severe hypotension requiring vasopressors. His physical exam was positive for icteric sclera, a distended abdomen with increased bowel sounds, and marked tenderness in the right lower quadrant. He had a WBC of 13.9 × 109/L (4.5-11.0 × 109/L) and platelet count of 79 × 109/L (150-450 × 109/L). His creatinine was 203.3 umol/L (58-111 umol/L) and total bilirubin was 171 umol/L (3-22 umol/L). A CT scan of the abdomen/pelvis revealed a capsule endoscope located near the terminal ileum along with diffusely thickened bowel wall, fat stranding in the right lower quadrant, hemorrhagic ascities and loculated free air (Figure 1), reported as ischemic enteritis and SB perforation.
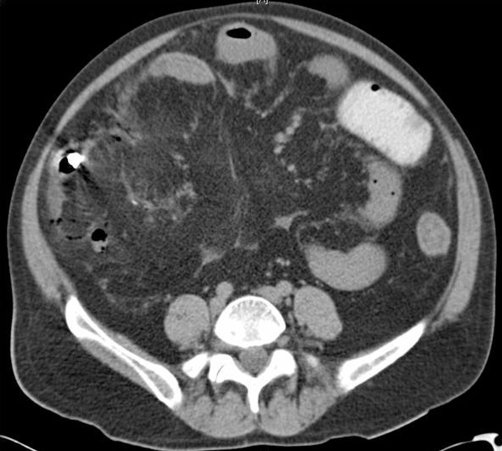
Figure 1.
Small bowel perforation caused by capsule endoscope. Contrast-enhanced CT scan of the abdomen taken on admission showing loculated free air, fat stranding and a capsule endoscope near the terminal ileum (white arrow).
After adequate resuscitation the patient was taken to the operating room where an ileocecectomy was performed, including removal of 160 cm of SB. The capsule endoscope found just proximal to the stricture. Given the patient’s hemodynamic instability the abdomen was initially closed with a 2 mm GORE-TEX (WL Gore & Associates Inc., Flagstaff, AZ) patch and loose suture. He required 12 subsequent operations for various complications and was discharged after 1 month with an ileostomy and colostomy. Pathology of the resected specimen showed an ileal stricture 15 cm proximal to the ileocecal valve, with associated necrotizing ileitis. A perforation was noted just proximal to the stricture where the capsule endoscope was found.
Discussion
WCE is a safe and well tolerated procedure with few complications. Over 400,000 capsules have been deployed worldwide since 2000 with rare complications and no reported deaths [9]. To date, the most common complication is retention of the capsule, ranging from 0% to 13% of all cases, with larger single institution studies reporting a rate of up to 2.5% [1,9]. Patients at high risk for capsule retention include those with radiation enteritis, known CD, SB tumors, NSAID enteritis, SB diaphragm disease, prior SB obstruction, and those with prior SB resection and primary anastamosis [1]. Although a time limit has not been set for intervention after documented capsule retention, surgical and enteroscopic retrieval have proven beneficial for removal of the capsule endoscope and correction of the underlying pathology in symptomatic patients [10]. In asymptomatic patients surgical retrieval may be indicated if the identified pathology can be treated operatively.
Despite concerns over capsule retention and possible obstruction, the widespread use of WCE for evaluation of CD is justified by improvements in diagnostic yield relative to traditional modalities, with low procedure risk. Overall diagnostic yield has commonly been reported between 15% and 44%, and a recent case series has shown a diagnostic yield of 86% leading to a change in management in 64% of cases [11,12].
In the present case, capsule impaction secondary to a stricture in the terminal ileum was likely the inciting mechanism leading to acute SB obstruction and subsequent perforation. The use of more rigorous pre-procedure evaluation in patients with suspected or known CD should therefore be pursued. Specifically, additional imaging in the form of barium follow-through, and CT/MR enterography may help characterize SB disease, although the presence or absence of a stricture does not necessarily preclude the possibility of SB obstruction. In this regard, the patency capsule has shown promise for the evaluation of patients with known strictures or other SB disease leading to obstruction [13]. Spada et al. showed a 100% video capsule passage rate in 10 patients with known strictures, screened from an original pool of 34 patients by the Agile Patency Capsule (Given Imaging, Yoqneam, Israel) [14]. Although the patency capsule itself has also been shown to result in symptomatic SB obstruction in a few cases [15], appropriate utilization and interpretation with this system is valuable in evaluating the functional patency of WCE candidates.
The advent of WCE has revolutionized imaging of the SB, improving diagnostic yield at relatively low complication rates. Our report, in combination with the Repici and Um reports, suggests that more serious complications than previously anticipated exist for this technique and may not be limited to the elderly. Furthermore, SB perforation should be recognized as a possible complication in patients with well established, suspected, or even a presumed quiescent history of CD. Capsule endoscopists must exercise extended caution in patient selection, especially as utilization of WCE increases in the management of IBD.
Abbreviations
- CD
Crohn’s disease
- CT
computed tomography
- IBD
inflammatory bowel disease
- MR
magnetic resonance
- NSAIDs
non-steroidal anti-inflammatory drugs
- SB
small bowel
- WCE
wireless capsule endoscopy
Consent
Formal written consent from the patient was not obtained. The authors maintain that all reasonable attempts to gain consent have been made. The patient is anonymous and there is no reason to think that the patient or their family would object to publication.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DAP involved in initial writing and editing of the manuscript. JAP and GCA involved writing and editing of the manuscript. CFC involved in editing of the manuscript, providing clinical care.
This article is available from: http://casesjournal.com/casesjournal/article/view/7607
Contributor Information
Dhavan A Parikh, Email: dhavan15@gmail.com.
Janak A Parikh, Email: jparikh@mednet.ucla.edu.
Gregory C Albers, Email: galbers@uci.edu.
Charles F Chandler, Email: cchandler@mednet.ucla.edu.
References
- Eliakim R. Video capsule endoscopy of the small bowel [review] Curr Opin Gastroenterol. 2008;24:159–163. doi: 10.1097/MOG.0b013e3282f3d946. [DOI] [PubMed] [Google Scholar]
- Herrerias JM, Caunedo A, Rodriguez-Tellez M, Pellicer F, Herrerias JM., Jr Capsule endoscopy in patients with suspected Crohn’s disease and negative endoscopy. Endoscopy. 2003;35:564–568. doi: 10.1055/s-2003-40241. [DOI] [PubMed] [Google Scholar]
- Pons Beltrán V, Nos P, Bastida G, Beltrán B, Argüello L, Aguas M, Rubín A, Pertejo V, Sala T. Evaluation of postsurgical recurrence in Crohn’s disease: a new indication for capsule endoscopy? Gastrointest Endosc. 2007;66(3):533–540. doi: 10.1016/j.gie.2006.12.059. [DOI] [PubMed] [Google Scholar]
- Maunoury V, Savoye G, Bourreille A, Bouhnik Y, Jarry M, Sacher-Huvelin S, Ben Soussan E, Lerebours E, Galmiche JP, Colombel JF. Value of wireless capsule endoscopy in patients with indeterminate colitis (inflammatory bowel disease type unclassified) Inflamm Bowel Dis. 2007;13(2):152–155. doi: 10.1002/ibd.20060. [DOI] [PubMed] [Google Scholar]
- Lin OS, Brandabur JJ, Schembre DB, Soon MS, Kozarek RA. Acute symptomatic small bowel obstruction due to capsule impaction. Gastrointest Endosc. 2007;65(4):725–728. doi: 10.1016/j.gie.2006.11.033. [DOI] [PubMed] [Google Scholar]
- Carro PG, Yuste JP, Diez SF, Roldan FP, Garcia-Escribano OR. Intestinal Perforation Due to Retained Wireless Capsule Endoscope. Endoscopy. 2005;37:684. doi: 10.1055/s-2005-861424. [DOI] [PubMed] [Google Scholar]
- Um S, Poblete H, Zavotsky J. Small bowel perforation caused by an impacted endocapsule. Endoscopy. 2008;40:E122–E123. doi: 10.1055/s-2007-995694. [DOI] [PubMed] [Google Scholar]
- Repici A, Barbon V, De Angelis C, Luigiano C, De Caro G, Hervoso C, Danese S, Preatoni P, Pagano N, Comunale S, Pennazio M, Rizzetto M. Acute small-bowel perforation secondary to capsule endoscopy. Gastrointest Endosc. 2008;67(1):180–183. doi: 10.1016/j.gie.2007.05.044. [DOI] [PubMed] [Google Scholar]
- Cheon JH, Kim YS, Lee IS, Chang DK, Ryu JK, Lee KJ, Moon JS, Park CH, Kim JO, Shim KN, Choi CH, Cheung DY, Jang BI, Seo GS, Chun HJ, Choi MG. Can we predict spontaneous capsule passage after retention? A nationwide study to evaluate the incidence and clinical outcomes of capsule retention. Endoscopy. 2007;39:1046–1052. doi: 10.1055/s-2007-966978. [DOI] [PubMed] [Google Scholar]
- Cave D, Legnani P, de Franchis R, Lewis BS. ICCE consensus for capsule retention. Endoscopy. 2005;37:1065–1067. doi: 10.1055/s-2005-870264. [DOI] [PubMed] [Google Scholar]
- Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn’s Disease. Am J Gastroenterol. 2006;101:954–964. doi: 10.1111/j.1572-0241.2006.00506.x. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Zúñiga V, de Vega VM, Domènech E, Cabré E, Mañosa M, Boix J. Impact of Capsule Endoscopy Findings in the Management of Crohn’s Disease. Dig Dis Sci. doi: 10.1007/s10620-009-0758-8. in press. [DOI] [PubMed] [Google Scholar]
- Banerjee R, Bhargav P, Reddy P, Gupta R, Lakhtakia S, Tandan M, Rao VG, Reddy ND. Safety and efficacy of the M2A patency capsule for diagnosis of critical intestinal patency: Results of a prospective clinical trial. J Gastroenterol Hepatol. 2004;22:2060–2063. doi: 10.1111/j.1440-1746.2007.05039.x. [DOI] [PubMed] [Google Scholar]
- Spada C, Spera G, Riccioni M, Biancone L, Petruzziello L, Tringali A, Familiari P, Marchese M, Onder G, Mutignani M, Perri V, Petruzziello C, Pallone F, Costamagna G. A novel diagnostic tool for detecting functional patency of the small bowel: the Given patency capsule. Endoscopy. 2005;37:793–800. doi: 10.1055/s-2005-870246. [DOI] [PubMed] [Google Scholar]
- Delvaux M, Ben Soussan E, Laurent V, Lerebours E, Gay G. Clinical evaluation of the use of the M2A patency capsule system before a capsule endoscopy procedure, in patients with known or suspected intestinal stenosis. Endoscopy. 2005;37(9):801–807. doi: 10.1055/s-2005-870241. [DOI] [PubMed] [Google Scholar]