Abstract
A common form of cancer treatment is radiation therapy. In this investigation individual differences in the psychological reactions of 45 patients undergoing external treatment were examined in the context of the Janis (1958) and linear decline models (e.g., Spielberger, Auerbach, Wadworth, Dunn, & Taulbee, 1973) of medical stressor anxiety. Evaluation included pre- and postradiation assessments of the subjects’ state and trait anxiety, somatic complaints, and treatment side effects. Technologists administering the daily treatments assessed behavioral indicants of affective distress. Data analyses revealed that increases in complaints and side effects were reported by all patients at treatment conclusion. More interesting, significant changes in state anxiety were obtained from pre- to posttreatment: (a) Patients with an initial high level of anxiety reported a significant reduction, although they remained the most anxious subgroup; (b) patients with a moderate level of pretreatment anxiety reported no change; and (c) patients with low levels of anxiety reported significant increases in state anxiety. No change in trait anxiety was found for any group, suggesting that the foregoing changes in state anxiety were not simply attributable to regression. Data trends suggested that patients who were either low or high in state anxiety were also characterized by more anger or hostility than patients moderate in anxiety. The findings are consistent with the Janis model, which posits that in threatening situations the level of fear can potentially determine the adequacy of adaptation.
At least 350,000 cancer patients receive radiation therapy each year. Clinical descriptions (Rotman, Rogow, DeLeon, & Heskel, 1977; Smith & McNamara, 1977; Welch, 1980; Yonke, 1967) have noted cancer patients’ fears of the treatment (e.g., being “burned;” or causing sterility, cancer, sickness, or vomiting) and vast individual differences in their psychological reactions. Peck and Boland (1977) interviewed 50 patients receiving treatment for potentially curable cancer and found mild or moderate anxiety more often than any other emotional response, including depression, irritability, suspicion, or euphoria. In fact, they viewed 60% of the patients as having significant anxiety prior to treatment and 80% of them afterwards. Beyond these few reports, there has been little systematic study of the social or psychological reactions to radiation treatment, and conceptual frameworks have not been offered. Toward these efforts, the present investigation was conducted.
To understand the psychological responses to radiation therapy, research in coping with surgery or difficult diagnostic procedures in noncancer patients may provide a potentially useful conceptual framework. Within this latter context, Janis (1958) provided the first extensive description of psychological stress among surgical patients and emphasized the significance of preoperative fear or anxiety as a factor in postoperative emotional responses and recovery. From his clinical investigation of 22 inpatients and survey research with 149 undergraduates reporting on a wide range of surgery experiences, including both minor (e.g., tooth extraction, nail repair) and major (e.g., appendectomy, hernia repair, tonsilectomy), he proposed that when preoperative anxiety is of moderate intensity and situationally relevant, it stimulates the “mental work of worry” (Marmor, 1958) such that patients are able to anticipate postoperative feelings, conditions, and circumstances so as to prepare themselves.
In contrast, extreme responses, such as overwhelming worry, were thought to have little if any additional value for adjustment or recovery. Hence, highly anxious patients who forecast doom and gloom would experience some reduction in their level of anxiety but remain the most anxious and behaviorally disrupted postsurgery. As well, individuals who minimize the event and assert no fear were thought to be insufficiently motivated to prepare cognitively for the postoperative pain, limitation of movement, and so forth that occurs for all patients and, hence, would subsequently experience anxiety, anger, and irritability following surgery (Janis, 1958).
Moderate anxiety presumably served two functions during the anticipatory period. It served as an emotional signal of the trauma or pain that was imminent, and it prompted defensive actions to minimize negative outcomes and maximize subsequent adjustment (Janis, 1958). We reasoned that both functions could facilitate short-term recovery or long-term adjustment from the more difficult experiences of repeated stressors. That is, if the facilitative function of realistic worry (Marmor, 1958) or anxiety when facing stressful medical experiences (Janis, 1958) is considered in the context of repeated treatments or adjustment to treatment needed for a chronic illness, the maintenance or attainment of a moderate, manageable level of anxiety might be expected and adaptive. For cancer patients undergoing radiotherapy, for instance, both functions are applicable. In addition to the benefits of moderate levels of anticipatory anxiety, the maintenance or attainment of a moderate level of anxiety following therapy could maximize patients’ attention to information important for their recovery, promote acceptance of reassurances regarding the availability and skill of their medical team, and assist them in warding off feelings of helplessness should their condition deteriorate.
Although Janis’ conceptualization is intriguing and corroborated by his findings, subsequent attempts to obtain empirical evidence have not been as supportive. Conceptual replications by other investigators testing more homogeneous samples of medical patients have not confirmed his hypotheses (e.g., Auerbach, 1973; Margalit, Teichman, & Levitt, 1980), or have provided only partially convergent evidence for these relations using measures of recovery or hospital adjustment (e.g., Auerbach, 1973).
Spielberger and colleagues (Spielberger, Auerbach, Wadsworth, Dunn, & Taulbee, 1973), for instance, have demonstrated a linear relation between pre- and postoperative anxiety. Inconsistencies between the latter research and Janis’ may have been due in part to differences in methodologies. Spielberger et al. evaluated the emotional reactions of patients with the State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970). This measure was used to contrast anxiety generated as a result of the surgery experience (i.e., situational or state anxiety), and anxiety as a relatively stable individual difference that would reflect anxiety proneness and be impervious to situational stress (i.e., person or trait anxiety), whereas the Janis methodology had been to ask surgery-relevant questions (e.g., “During the hour immediately before the operation or treatment was started, how intense was the most severe fear or anxiety that you experienced?” (Janis, 1958, p. 278).
Spielberger et al. (1970) administered the STAI to 26 male general surgery’ patients 18–24 hrs before surgery and 3 to 9 days postsurgery. On the basis of the presurgery anxiety scores, subjects were divided into high and low anxiety groups. For the state-anxiety measure, analyses revealed significant main effects for time, but the time by anxiety level interaction predicted by Janis (1958) was not significant. Indeed, state anxiety declined for all patients, with less state anxiety during recovery reported by those with low rather than high preoperative anxiety. Trait anxiety, in contrast, was unaffected across measurement periods, as predicted by Spielberger. Linear reductions with situational or state measures and stability of trait-anxiety measures have been reported by other investigators (Auerbach, 1973; Margalit et al., 1980; Martinez-Urrutia, 1975; Wolfer & Davis, 1970; Endler, Hunt, & Rosenstein, 1962). Thus, past research has been largely supportive of a linear relationship between pre- and postoperative anxiety.
The linear decline model that has emerged from this research, therefore, provides an alternative conceptualization within which to view psychological reactions to radiation therapy. Which is preferable is an empirical question. There are several reasons, however, why a linear decline in anxiety responses might not be evidenced among cancer patients and the Janis framework may be more appropriate. First, data indicate that hospitalized cancer patients as a group report greater anxiety than individuals hospitalized for nonmalignant conditions (Lucente & Fleck, 1972). After surgery, greater and more lasting emotional distress, general feelings of experiencing a crisis, and feelings of helplessness, in particular, are reported by cancer in comparison to general surgery patients (Gottesman & Lewis, 1982). Such data indicate that more extreme anxiety reports would possibly be obtained from patients both pre- and postradiotherapy, and treatment-related anxiety may dissipate slowly.
Second, extreme psychological responses have been documented in a subset of patients undergoing other forms of cancer treatment, and it may be expected that comparable disruption may be experienced by cancer patients undergoing radiotherapy. Some chemotherapy patients exhibit anxiety that becomes so extreme across trials that they eventually refuse particular drugs, regardless of their therapeutic effectiveness, or discontinue regimens completely (Redd & Andrykowski, 1982). Experimental treatments such as hyperthermia are also associated with considerable pain and distress (Reeves, Redd, Minagawa, & Storm, 1983).
Third, a factor unique to the conclusion of a radiation therapy course may affect posttreatment anxiety. Because radiation effects on many tumors or microscopic disease are not determined until months after treatment has ended, many patients are left with uncertainty about the adequacy of radiation in curing their disease. Such uncertainty may become more salient on the final treatment day. A possible indication of this uncertainty was reported by Mitchell and Glicksman (1977) who interviewed 50 patients. Thirty (60%) patients felt “improved” because of their therapy, 16 (32%) saw “no change,” and 4 (8%) felt they had become “worse.” Such a circumstance of uncertainty could significantly influence posttreatment anxiety in at least two important respects. First, it could interfere with the dissipation of anxiety expected with the linear decline model when a medical treatment has ended. Second, such a circumstance of uncertainty could mark the beginning of a new period for which the maintenance or attainment of moderate anxiety during recovery would be an adaptive coping response.
To examine the psychological responses to radiation therapy and to test the applicability of the two conceptualizations, measures of situational and dispositional anxiety were administered immediately pre- and posttreatment to cancer patients undergoing a full course of external radiation therapy. The factors in our analysis were patients’ pretreatment anxiety (low, moderate, or high), anxiety scale (state or trait), and time (pretreatment or posttreatment). It was predicted that if the linear decline model was most appropriate, a significant Anxiety Scale × Time interaction would be found; specifically, significant reductions in state anxiety would be found from pre- to posttreatment for all levels of pretreatment anxiety but trait anxiety scores would remain stable.
In contrast, it was predicted that if the Janis model was most appropriate for analyzing individual differences in response to radiotherapy, then a significant three-way interaction between pretreatment anxiety, anxiety scale, and time would be found, with convergence in anxiety levels occurring across time on the state anxiety scale, but no change in anxiety levels occurring across time on the trait anxiety scale.
It was also predicted that any other affective disturbance, anger or hostility in particular, would be manifest during the early rather than mid or final treatment stages. This period is analogous to the first or early morning awakening after a surgical procedure. In addition, because the actual procedure of receiving a radiation treatment varies little from day to day, we reasoned that such a routine would facilitate the dissipation of affective distress unique to being in the treatment room. According to the Janis conceptualization, greater distress on the first day of treatment should occur for those with initial low or high anxiety levels than for those with moderate anxiety. According to the linear decline model, on the other hand, there should be a direct relation between pretreatment anxiety level and affective distress.
Finally, measures of symptomatology were obtained to document the debilitating effect of the radiation treatment, per se. We hypothesized that it was possible that symptomatology outcomes could covary with pretreatment anxiety level, although it was unlikely due to the magnitude of radiation effects and the inconsistency with which such interactions had been observed with lesser medical interventions (e.g., Cohen & Lazarus, 1973; Johnson, Leventhal, & Dabbs, 1971; Martinez-Urrutia, 1975).
Method
Subjects
Participants included 27 male and 18 female cancer patients receiving a definitive full course of external radiation therapy (RT) through a large university hospital. All patients were ambulatory and ranged in age from 16 to 79 (male M = 55 yrs., female M = 47 yrs.). Sites for treatment for the male sample included head and neck (n = 12), lung (n = 5), bone (n = 3), and prostate or colorectal (n = 7). Survival estimates (SEER, 1976) of 5-year survival for the male sample ranged from 0 to 80% with a mean of 41%. Sites for treatment for the female sample included: head and neck (n = 2), lung (n = 1), gynecologic (n = 12), breast (n = 1), kidney (n = 1), and colon (n = l). Estimated 5-year survival for the female sample ranged from 1 to 86% with a mean of 63%.
Measures
State-Trait Anxiety Inventory (STAI)
This inventory (Spielberger et al., 1970) is a self-report scale for measuring two distinct anxiety concepts in normal adults. The A-Trait scale consists of 20 statements that ask subjects to describe how they generally feel, an attempt to tap relatively stable individual differences in anxiety proneness. The A-State scale also consists of 20 statements, but the instructions require subjects to indicate how they feel at a particular moment in time. For each item subjects indicate on a 4-point scale whether or not each statement is, almost never/not at all to almost always/very much so, descriptive of their feelings. Scores for each scale may range from 20 to 80.
Because the state measure is regarded similar to mood measures that have expectedly lower test-retest reliabilities, comparison of internal consistency reliabilities for the state and trait measures is more appropriate. Coefficient alpha reliabilities for the state measure range from .86 to .92 and those for the trait measure are equally high (Spielberger et al., 1970).
Profile of Mood States (POMS)
An abbreviated version of the 65-item POMS measure (McNair, Lorr, & Droppleman, 1971) was chosen to assess the patients’ affective behavior immediately preceding and following radiation treatments. Two items from each of the six POMS factors—Tension–Anxiety, Depression–Dejection, Anger–Hostility, Vigor–Activity, Fatigue–lnertia, and Confusion–Bewilderment—were selected on the basis of their high factor loadings and judged rateability by the technologists. The specific items included were tense, confused, hopeless, fatigued, angry, full of pep, unable to concentrate, nervous, exhausted, unhappy, alert, and grouchy. For each item, raters indicated on a 5-point scale whether or not the adjective was not at all (l) to extremely (5) descriptive of the patient’s behavior that day. Ratings were completed on treatment day I, 5, 10, 15, and so forth, and the last treatment day, by the patient’s radiation therapy technologist who administered treatment during his or her entire course but who was unaware of the patient’s STAI scores.
Symptomatology reports
Before and after radiation therapy, patients indicated on a 10-point scale, not at all (1), moderate (5), severe (10), the presence and severity of fatigue, appetite loss, pain, and each of four short-term radiation therapy side effects relevant for their treatment site (e.g., diarrhea for gynecology patients, shortness of breath for lung patients). The list of complications for each site had previously been generated with the assistance of radiation therapy technologists and physicians. Agreement among these personnel was 85% across complication categories.
Procedure
Following the patient’s consultation for treatment, patients were approached by an investigator or assistant for possible study participation. Verbal and written explanations of the study were provided to patients. At that time the majority of patients consented with a few preferring to extend consideration into the next day. Of the 47 patients contacted, only two (<5%) chose not to participate.
One day prior to beginning treatment, a brief structured interview was conducted and subjects completed the STAI and symptomatology reports. Radiation treatment is administered to each patient by the same treatment technologist on a daily basis Monday through Friday. The treatment experience varies little from day to day. Patients typically arrive in the department 5 to 10 min before their regularly scheduled time and then go to a lounge where other patients are also waiting. When their name is called, he or she walks to the nearby treatment room where a technologist is waiting. Here the patient removes the necessary clothing to expose the body area to be treated, and the technologist aligns the machine and positions any lead blocks to prevent radiation absorption to vital organs (e.g., kidneys). The patient then lies on the treatment table in the necessary position, the table is slid under the machine, and the machine is adjusted a final time to align the radiation beam and treatment field. When set, the technologist leaves the room, closing a heavy lead door. Patients are monitored on closed-circuit television screens located at the technologist’s control panel should the patient move from position or request assistance. Voice contact between the technologist and patient is possible with an intercom. Actual treatment time varies from 2 to 10 min, depending on the radiation dosage and number of body positions or angles required. When finished, the technologist enters the room, helps the patient down from the table, and begins set up for the next patient. This entire period of technologist and patient contact is 10 to 20 min. Treatment for all study participants lasted 5 to 8 weeks, reaching a total tumor dose for each patient of 4–6,000 rads. Posttreatment assessment included a brief interview with the patient assessing symptomatology and retesting with the STAI immediately following the patient’s last treatment.
Results
To investigate the effect of individual differences in transient pretreatment anxiety, scores on the pretreatment state anxiety scale for the 45 subjects were hierarchically ordered and the sample was subdivided into three groups: low, moderate, and high pretreatment anxiety. One-way analyses of variance (anovas) were conducted on relevant variables, which could confound the comparison among anxiety groups. Analyses revealed no significant differences among these groups as a function of demographic variables: sex, age, education, religiosity, or amount contributed to total family income; and illness/disease variables: inpatient/outpatient status, site, or estimated 5-year survival (all ps > .10).
A 3 × 2 × 2 (Patient’s Pretreatment Anxiety: Low, Moderate, or High State Anxiety × Anxiety Scale: State or Trait × Time: Pretreatment or Posttreatment) anova was then performed for the anxiety data. For significant main effects and interactions, Duncan multiple range tests for pairwise comparisons were calculated with p < .05. The main effect for patient’s pretreatment anxiety was significant, F(2, 42) = 33.85, p < .001, indicating that patients assigned to the high anxiety group based on a high pretreatment state anxiety score were also characterized by the highest overall level of anxiety (i.e., across time and state–trait scales), M = 47; patients assigned to the moderate group were characterized by a middling overall level of anxiety, M = 37; and patients assigned to the low group were characterized by the lowest overall level of anxiety, M = 31 (all ps < .05). There was also a significant main effect for the Anxiety Scale factor, F(I, 42)= 8.36, p < .001, which indicated higher scores for the subjects on the State scale (M = 39) than on the Trait scale (M = 37). These latter findings simply attest to the stressfulness of the disease and radiation therapy for the patients. The main effect for the Time factor was not significant, suggesting as we suspected that the overall level of anxiety was not lowered by the simple completion of radiation therapy.
To test the applicability of the linear decline and Janis conceptualizations, the analyses of interactions among factors are crucial. According to the linear decline model, a signficant overall Anxiety Scale × Time interaction is expected, with significant reductions in anxiety only with the State scale and not the trait scale. In fact, however, there was no hint of such a significant interaction, F < 1. Indeed, the only significant two-way interaction was the Patients’ Pretreatment Anxiety × Time effect, F(2, 42) = 8.65, p < .001.
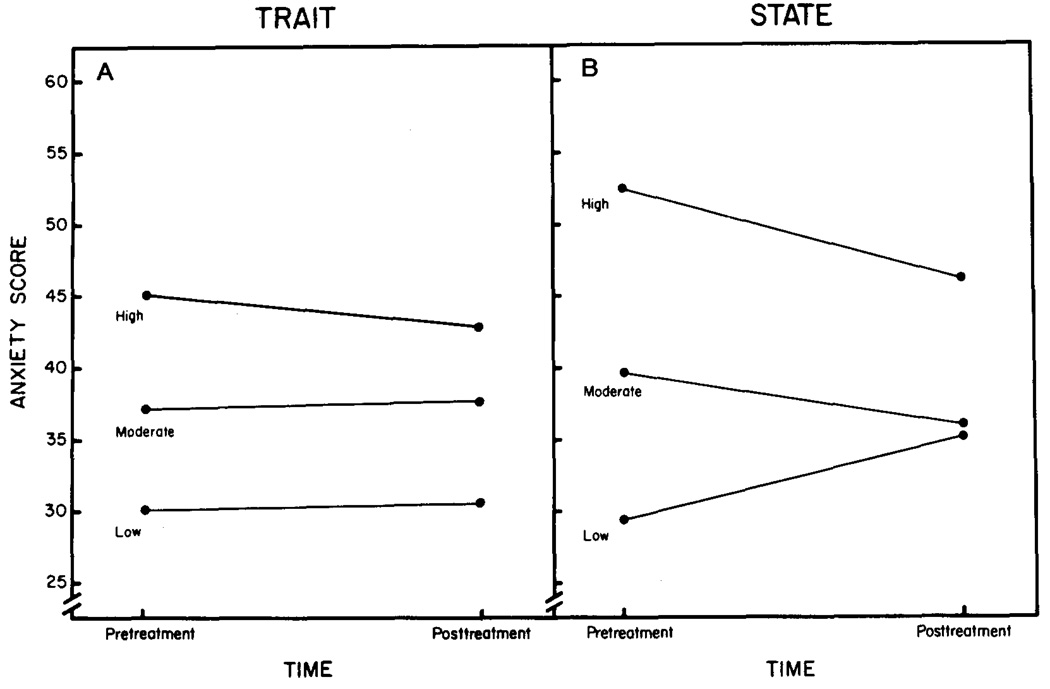
According to the Janis conceptualization, a significant Patient’s Pretreatment Anxiety × Anxiety Scale × Time interaction is to be expected, and such an interaction was found, F(2, 42) = 6.73, p < .001, which is illustrated in Figure 1. Multiple comparisons revealed significant increases in state anxiety for low pretreatment anxiety subjects, no change in state anxiety for moderate pretreatment anxiety subjects, and a significant decrease in state anxiety for high pretreatment anxiety subjects (see Figure lb). There are also significant differences in posttreatment state anxiety between the high pretreatment anxiety group and both the low and moderate pretreatment anxiety groups. This pattern contrasts sharply with findings for the trait anxiety scale, which indicated significant differences between the low, moderate, and high pretreatment anxiety groups but no change in trait scores across time (see Figure la).
Figure 1.
Data pattern for significant three-way interaction. Figure la indicates stability of trait-anxiety scores across time for low, moderate, and high pretreatment anxiety groups. Figure lb indicates significant interactions in state-anxiety scores across time for low, moderate, and high pretreatment anxiety groups.
Because the state anxiety levels converge following radiation therapy, the question could be raised that this portion of the data reflects regression to the mean. The significant three-way interaction, however, argues against this possibility, particularly because the reliabilities of the State–Trait scales are high and comparable. That is, if the convergence depicted in Figure lb was a statistical artifact (i.e., regression), then a comparable pattern of convergence would be expected for the data depicted in Figure l a. This, of course, was not the case.1
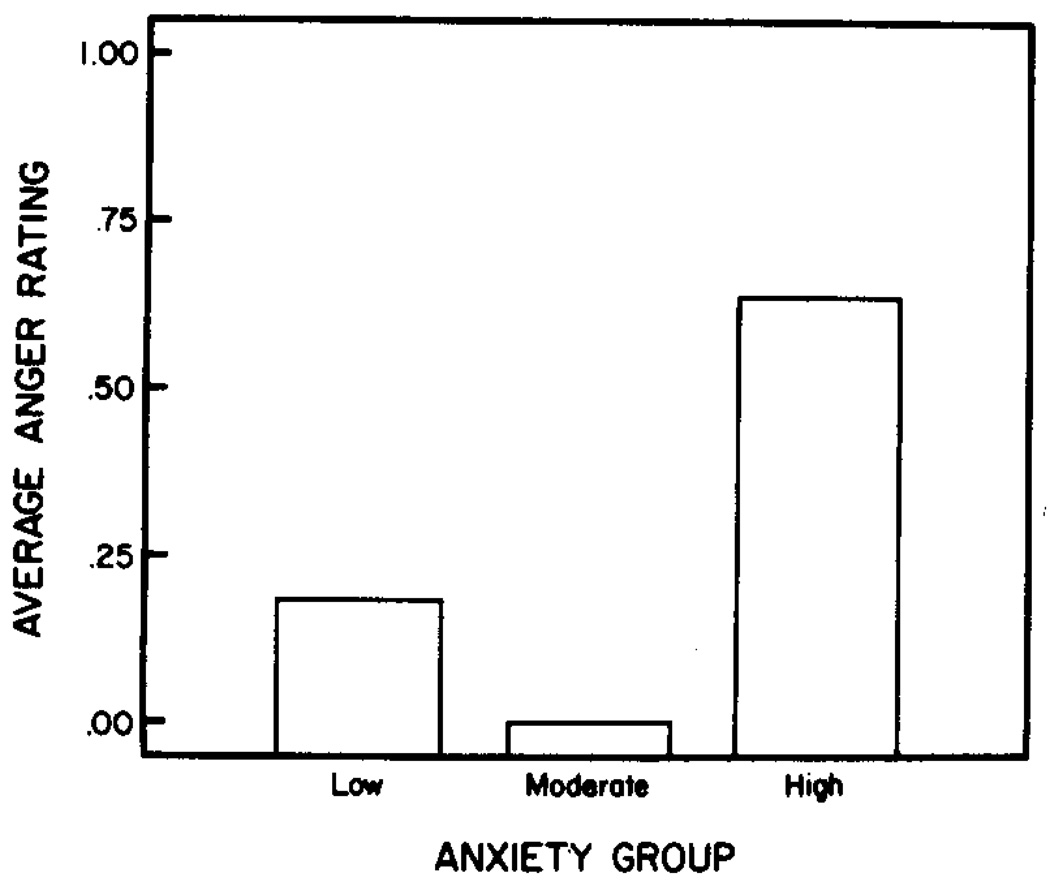
One-way anovas were conducted for the POMS data. Comparisons among patient pretreatment anxiety groups for the various treatment days were made to test the specific hypothesis that the means would reflect greater distress in the early phases of treatment among low or high pretreatment anxiety groups relative to patients with moderate anxiety (according to Janis) or that the means would be ordered according to the pretreatment anxiety level (according to the linear decline model). Analyses were first conducted for the total POMS score for the 10 items. These revealed no significant differences between groups for the various treatment days. Analyses were next conducted for the sum of the two Anger-Hostility items of the measure. Analyses revealed marginal differences among groups on treatment day 1, F(2, 42) = 2.58, p < .08, and no differences between groups thereafter. These means, approximating the Janis predictions, are displayed in Figure 2.
Figure 2.
Ratings of radiotherapy technologists of angry mood on the first day of treatment among patients reporting low, moderate, or high pretreatment anxiety.
Additional 3 × 2 anovas with the factors of patient’s pretreatment anxiety (high, moderate, or low) and time (pretreatment or posttreatment) were calculated for the patient symptomatology reports. Significant main effects for time, for all variables were found indicating that patients reported significant increases in fatigue, appetite loss, pain, and radiation therapy side effects by the end of their treatment course. Values for these measures are presented in Table 1. Main effect of anxiety level or the interaction of factors was not found.
Table 1.
Mean and Standard Deviation Scores for Measures of Symptomatology Preand Postradiotherapy
| Pretreatment | Posttreatment | |||
|---|---|---|---|---|
| Measure | M | SD | M | SD |
| Fatigue** | 2.49 | 2.43 | 4.72 | 2.93 |
| Appetite loss** | 1.07 | 2.40 | 4.33 | 3.67 |
| Pain* | 1.60 | 2.53 | 2.84 | 3.38 |
| Radiation therapy side effects** | 6.13 | 6.37 | 20.19 | 10.09 |
p < .01.
p < .001.
Discussion
This investigation was designed to determine individual differences in psychological responses to external radiation therapy administered as a curative effort. Data analyses revealed that patients with an initial high level of pretreatment anxiety reported a significant reduction in their state anxiety, although at posttreatment they remained the most anxious subgroup. Patients with a moderate level of pretreatment anxiety reported little change in their state-anxiety responses. Patients with low levels of anxiety prior to radiation therapy reported significant increases in state anxiety at posttreatment such that they equaled the state-anxiety level maintained by the group with moderate pretreatment anxiety. This pattern replicates the anxiety-response data provided by Janis (1958). When fear responses were assessed in this latter research, approximately 47%, 50%, and 73% of the low, moderate, and high anxious subjects, respectively, reported some degree of postoperative fear. With Janis’ data as with that from the present investigation, significant differences were noted between the high and moderate groups and the high and low groups, with comparable levels of fear expressed between the low and moderate groups at posttreatment.
In contrast to the state-anxiety data, trait-anxiety scores showed no significant change across time for any anxiety subgroup. The stability of the trait measure replicates the data of other investigators who have used the STAI or other traitlike anxiety measures (e.g., S–R Inventory of Anxiousness, MMPI subscales) in studying stressful medical experiences. Perhaps more important, however, the pattern of results for the state and trait data as indicated by the significant three-way interaction, weakens the plausibility of artifactual explanations for the state-anxiety findings.
In addition to the anxiety data, Janis (1958) also suggested that a moderate level of anxiety would have a facilitative effect for other post-operative responses or recovery measures. In the present research the technologist ratings provided preliminary data on behavioral manifestations of affective disturbance among radiation patients when actually receiving their treatments. When total mood disturbance was evaluated, no difference between groups was found across the treatment days. However, when anger or hostility ratings were analyzed separately, trends indicated that the low and high anxious subjects displayed or were regarded as manifesting such behavior in contrast to no disruption among the moderately anxious group. Whereas postoperative anger and aggressiveness were hypothesized to be the greatest problem for individuals with low preoperative anxiety, the Janis (1958) data indicated distress for high anxious patients as well. In either case, the means for the anger/hostility data were not ordered according to a low, moderate, high ranking as would be expected with the linear decline model. Although these findings are convergent with the Janis (1958) data, they should be regarded as preliminary and in need of replication due to the effect size and modest rating procedure.
Finally, the measures of symptomatology indicated radiation therapy exacerbated patients’ feelings of distress and illness with comparable disruption for all patients. As previously suggested, the absence of covariation between such data and patients’ pretreatment anxiety level may indicate that the side effects of radiation therapy overpower, at least initially, the psychological contributions to the patients’ symptomatology. Larger sample sizes or measures of tissue or organ sensitivity may be necessary to detect the small but important differences in symptomatology that are thought to be mediated by individuals’ emotional reactions.
If the Janis conceptualization is an appropriate context for viewing the psychological reactions to radiotherapy, the expression of moderate fear or distress may have substantial benefits for cancer patients. It may begin a pretreatment “work of worry” period which may include attending to information important for undergoing treatment in the least stressful manner, accepting reassurances from others, and warding off feelings of helplessness. All such responses would presumably facilitate adjustment to the treatment process. A question remains, however: Why at the end of treatment a moderate level of anxiety would be maintained (or approached) if it actually facilitated adjustment during treatment? For relatively healthy individuals undergoing corrective medical treatment, maintaining moderate anxiety at treatment’s end would presumably serve no useful purpose as long as recovery was expected to be uncomplicated and resumption of life style assured. In the context of a difficult treatment or a life-threatening illness, the maintenance (or attainment) of moderate anxiety posttreatment may indicate a level of anxiety appropriate for the context of cancer and anxiety that can facilitate adaptation, rather than simply reflecting distress and psychosocial disruption.
In a related context, it has been suggested that psychological factors may have an impact on the course of cancer. In particular, it has been suggested that coping styles that involve suppression, denial of affect, or have depressive qualities lead to the onset of or higher than expected risk of death from cancer (e.g., Schmale & Iker, 1971; Shekelle et al., 1981). In contrast, responses of anxiety and coping styles that facilitate external, conscious expression of negative emotions and psychological distress have been suggested as characteristic of those cancer patients who survive longer (Derogatis, Abelof, & Melisaratos, 1979).
This group at risk seems to include two subtypes, some patients who evidence denial and others of whom appear hopeless and helpless about their cancer. These extreme responses appear parallel to and convergent with Janis’ (1958) discussion of the responses and complications for low and high anxious patients undergoing surgery. Between the extreme responses to either cancer or medical stressors there presumably lies a moderate, adaptive, and perhaps survival-enhancing response. In essence, the work of worrying may then be a never-ending task when confronted by the changing circumstances of a life-threatening disease.
Acknowledgments
The research was supported by a University of Iowa Old Gold Fellowship and a National Institute of Health Biomedical Research Grant NIH-S07-RR07035-16 awarded to the first author.
The authors would like to thank a number of individuals who provided assistance in this research. Greatest appreciation is extended to the participating patients.
In addition, the following persons assisted with the research: Ulf Kadsson, Ramesh Kakria, Howard Latourette, Farida Rajput, Gary Schultz, Ferial Tewfik, Charles Bischof; Vicki Betts, Diane Brenneman, Patricia DeJong, Judith Washa; Jennifer Kadsson, Virginia Lee; Becky Huber and Terry Kirk. John Cacioppo and Suzanne Kell provided helpful comments on the article.
Footnotes
Yet another question could be raised that regression is operating in these findings with our use of the state anxiety scores as both a grouping variable (i.e., patient’s pretreatment anxiety) and a dependent variable. To address this concern, we repeated the same analysis, instead, however, using the pretreatment trait scores as a grouping variable. As expected, we found the significant outcomes for the Patient’s Pretreatment Anxiety factor F(2, 42) = 70.99, p < .001, and Anxiety Scale, F(l, 42) = 8.36, p < .001. However, the Time factor and all interactions, including Anxiety Scale × Time, did not approach significance (F < l). Thus, these findings cannot be discounted on the basis of regression to the mean.
Contributor Information
Barbara L. Andersen, University of Iowa
Hamed H. Tewfik, Department of Radiology, University of Iowa
References
- Auerbach SM. Trait-state anxiety and adjustment to surgery. Journal of Consulting and Clinical Psychology. 1973;40:264–271. doi: 10.1037/h0034538. [DOI] [PubMed] [Google Scholar]
- Axtell LM, Asire AJ, Meyers MH, editors. Cancer surveillance, epidemiology, and end results (SEER) program. Bethesda, MD: National Cancer Institute; Cancer patient survival: Report number 5. 1976
- Cohen F, Lazarus R. Active coping processes, coping dispositions, and recovery from surgery. Psychosomatic Medicine. 1973;35:375–389. doi: 10.1097/00006842-197309000-00002. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Abeloff MD, Melisaratos N. Psychological coping mechanisms and survival time in metastatic breast cancer. Journal of the American Medical Association. 1979;242:1504–1508. [PubMed] [Google Scholar]
- Endler NS, Hunt JMcV, Rosenstein AJ. An S–R inventory of anxiousness. Psychological Monographs. 1962;76(17):1–33. [Google Scholar]
- Gottesman D, Lewis MS. Differences in crisis reactions among cancer and surgery patients. Journal of Consulting and Clinical Psychology. 1982;50:381–388. doi: 10.1037//0022-006x.50.3.381. [DOI] [PubMed] [Google Scholar]
- Janis IL. Psychological stress: Psychoanalytic and behavioral studies of surgical patients. New York: Wiley; 1958. [Google Scholar]
- Johnson J, Leventhal H, Dabbs J. Contributions of emotional and instrumental response processes in adaptation to surgery. Journal of Personality and Social Psychology. 1971;20:55–64. doi: 10.1037/h0031730. [DOI] [PubMed] [Google Scholar]
- Lucente EE, Fleck S. A study of hospitalization anxiety in 408 medical and surgical patients. Psychosomatic Medicine. 1972;34:304–312. doi: 10.1097/00006842-197207000-00004. [DOI] [PubMed] [Google Scholar]
- Margalit C, Teichman Y, Levitt R. Emotional reaction to physical threat: Reexamination with female subjects. Journal of Consulting and Clinical Psychology. 1980;48:403–404. doi: 10.1037//0022-006x.48.3.403. [DOI] [PubMed] [Google Scholar]
- Marmor J. The psychodynamics of realistic worry. Psychoanalysis and Social Science. 1958;5:155–163. [Google Scholar]
- Martinez-Urrutia A. Anxiety and pain in surgical patients. Journal of Consulting and Clinical Psychology. 1975;43:437–442. doi: 10.1037/h0076898. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LE. Profile of mood states. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- Mitchell GW, Glicksman AS. Cancer patients: Knowledge and attitudes. Cancer. 1977;50:61–66. doi: 10.1002/1097-0142(197707)40:1<61::aid-cncr2820400112>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Peck A, Boland J. Emotional reactions to radiation treatment. Cancer. 1977;40:180–184. doi: 10.1002/1097-0142(197707)40:1<180::aid-cncr2820400129>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Redd WH, Andrykowski M. Behavioral intervention in cancer treatment: Controlling aversive reactions to chemotherapy. Journal of Consulting and Clinical Psychology. 1982;50:1018–1029. doi: 10.1037//0022-006x.50.6.1018. [DOI] [PubMed] [Google Scholar]
- Reeves JL, Redd WH, Minagawa RY, Storm CK. Hypnosis in the control of pain during hyperthermia treatment of cancer. In: Bonica JJ, Lindbland U, Iggo A, editors. Advances in pain research. Vol. 5. New York: Raven Press; 1983. pp. 857–861. [Google Scholar]
- Rotman M, Rogow L, DeLeon G, Heskel N. Supportive therapy in radiation oncology. Cancer. 1977;39:744–750. doi: 10.1002/1097-0142(197702)39:2+<744::aid-cncr2820390709>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Schmale AH, Iker H. Hopelessness as a predictor of cervical cancer. Social Science and Medicine. 1971;5:95–100. doi: 10.1016/0037-7856(71)90090-4. [DOI] [PubMed] [Google Scholar]
- Shekelle RB, Raynor WJ, Osfeld AM, Garron DC, Bieliauskas LA, Liu SC, Maliza C, Paul O. Psychological depression and 17-year risk of death from cancer. Psychosomatic Medicine. 1981;43:117–125. doi: 10.1097/00006842-198104000-00003. [DOI] [PubMed] [Google Scholar]
- Smith LL, McNamara JJ. Social work services for radiation therapy patients and their families. Hospital and Community Psychiatry. 1977;28:752–754. doi: 10.1176/ps.28.10.752. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Auerbach SM, Wadsworth AE, Dunn TM, Taulbee ES. Emotional reactions to surgery. Journal of Consulting and Clinical Psychology. 1973;40:33–38. doi: 10.1037/h0033982. [DOI] [PubMed] [Google Scholar]
- Spieiberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Welch DA. Assessment of nausea and vomiting in cancer patients undergoing external beam radiotherapy. Cancer Nursing. 1980:365–371. [PubMed] [Google Scholar]
- Wolfer JA, Davis CE. Assessment of surgery patients' preoperative emotional condition and postoperative welfare. Nursing Research. 1970;19:402–414. [PubMed] [Google Scholar]
- Yonke G. Emotional response to radiotherapy. Hospital Topics. 1967;45:107–108. [PubMed] [Google Scholar]