Abstract
Nipple hypertrophy is an occasional deformity in Asians and a rare one in Caucasians. Lately, it has been showing up more often in plastic surgeons’ offices across North America and elsewhere, owing to the influx of Asian immigration worldwide, as well as to the rising interest in esthetic surgery among Asian communities.
A simplified technique for nipple reduction is described herein. It is very easy to execute, delivers accurate results and is extremely safe. It tackles both the excessive ‘projection’ and the less frequent excessive ‘width’ of the nipple. It may be used separately or incorporated as an adjunct to mammary augmentation or mastopexy. Excellent esthetic results are obtained, while both the nipple innervation and its lactiferous ducts are preserved. The patient’s and surgeon’s satisfaction is high.
Keywords: Areola, Breast, Hypertrophy, Nipple, Reduction
Abstract
L’hypertrophie mamelonnaire s’observe à l’occasion chez les femmes asiatiques et rarement chez les femmes de race blanche. On a remarqué dernièrement une augmentation du nombre de consultations en chirurgie plastique, en Amérique du Nord et ailleurs dans le monde, en raison de l’accroissement de l’immigration asiatique sur la planète et de l’intérêt accru que porte la communauté asiatique à l’égard de la chirurgie esthétique.
Les auteurs décrivent, dans le présent article, une technique simplifiée de réduction du mamelon. Celle-ci est très facile à réaliser, donne des résultats précis et est extrêmement sûre. Elle vise autant la « projection » exagérée que la « largeur » excessive du mamelon. Elle peut être pratiquée seule ou en complément de la chirurgie mammaire d’augmentation ou de la mastopexie. La technique donne d’excellents résultats esthétiques tout en préservant l’innervation du mamelon et les conduits lactifères. Les patientes et les chirurgiens se disent très satisfaits des résultats.
Nipple hypertrophy and its reduction have been described in a limited number of articles throughout the medical literature (1–8). Nipple hypertrophy is an uncommon esthetic problem. The epidemiology of this deformity remains largely unknown; it is mostly encountered in the Asian population and, occasionally, in Caucasians. It is sometimes familial, appearing after the onset of adolescence or following pregnancy, and persisting through menopause (1). It may lead to psychological distress because of its association with a negative esthetic image. As well, women may feel embarrassed by their hypertrophic nipples, which are hard to conceal under light clothing because of their prominence.
No formal definition of nipple hypertrophy exists. Some clinicians have suggested that the normal female nipple is roughly 1 cm in diameter, with an almost equal amount of anterior projection (1). In cases of nipple hypertrophy, the size of the nipple may reach 2 cm or even more, and the shape usually becomes spherical.
The aim of the correction is primarily to shorten the nipple length, while secondarily establishing harmony between its diameter size and projection. The patient seeking a correction for nipple hypertrophy is usually also concerned about the functional results of the surgery, in addition to the esthetic outcome.
NIPPLE ESTHETICS
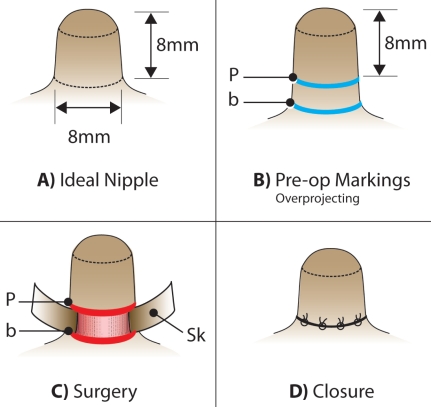
The ideal nipple (Figure 1A) is shaped like a cylinder, with a slightly curved ‘dome-like’ top. The height (projection) of the nipple is by far the most common disturbing factor in nipple hypertrophy. An ideal projection, in our opinion, is approximately 8 mm (with an acceptable margin of 6 mm to 10 mm). The second but less important component of nipple hypertrophy is its diameter, which ideally should be approximately 8 mm (6 mm to 10 mm). Nipple hypertrophy, in our experience, has always presented bilaterally.
Figure 1).
A Ideal nipple esthetics: The ideal nipple is shaped like a cylinder, with a ‘dome-like’ curved top. The ideal projection of a nipple, measured from the top of its dome to its base, is approximately 8 mm (6 mm to 10 mm). In addition, the ideal perimeter of the nipple is approximately 8 mm (6 mm to 10 mm) in diameter. B Preoperative marking of the overprojecting nipple: The height of the new nipple is measured as 8 mm from the top of its dome, and a circumferential line ‘p’ is drawn to delineate the perimeter of the new base. Another circumferential line is drawn around the present nipple base ‘b’. C Two circumferential incisions are made along lines ‘p’ and ‘b’. The excess skin between these two lines is dissected as a very thin skin flap ‘Sk’ and excised, leaving the lower section of the nipple exposed (pink area). The lactiferous ducts are left intact. D Closure: The exposed nipple between incisions ‘p’ and ‘b’ (Figure 1C) is invaginated into the areola. The two incisions ‘p’ and ‘b’ are approximated with interrupted or continuous sutures
SURGICAL TECHNIQUE
Reducing the nipple projection
Preoperative planning:
The marking of the hypertrophic nipple is performed in three steps. Firstly, the new projection of the nipple is delineated. This is done by measuring 8 mm from the top of its dome, and drawing a circumferential perimeter (Figure 1B: p) representing its new base. Secondly, a line (Figure 1B: b) is drawn around the present base. Finally, a vertical line (superior to inferior) and a horizontal line (from right to left) are drawn across the areola and the nipple to orient the surgeon during the final closure.
Infiltration:
The infiltration of the base and trunk of each nipple is done using 2 mL to 3 mL of 1% xylocaine with 1/100,000 adrenaline, delivered through a 30G needle.
Surgical reduction of excessive projection:
A circular incision is made at the bottom of the new nipple (circle p, Figure 1C). Another circular incision is made at the base of the present nipple (circle b, Figure 1C). The extra skin between these two incisions is meticulously dissected as a very thin cutaneous flap and then excised (Figure 1C: Sk), using an Adson-Brown forceps and a No 15 blade. Fine electrocautery is used for hemostasis.
Interrupted inverted 4-0 or 5-0 vicryl sutures are used to approximate the four corners (superior, inferior, medial, lateral) of the new nipple to its base (Figure 1D), using the drawn vertical and horizontal lines as references. This suturing leads to invagination of the naked section of the nipple (between incisions ‘p’ and ‘b’). The rest of the closure is done by using a continuous or interrupted inverted 4-0 or 5-0 vicryl structures.
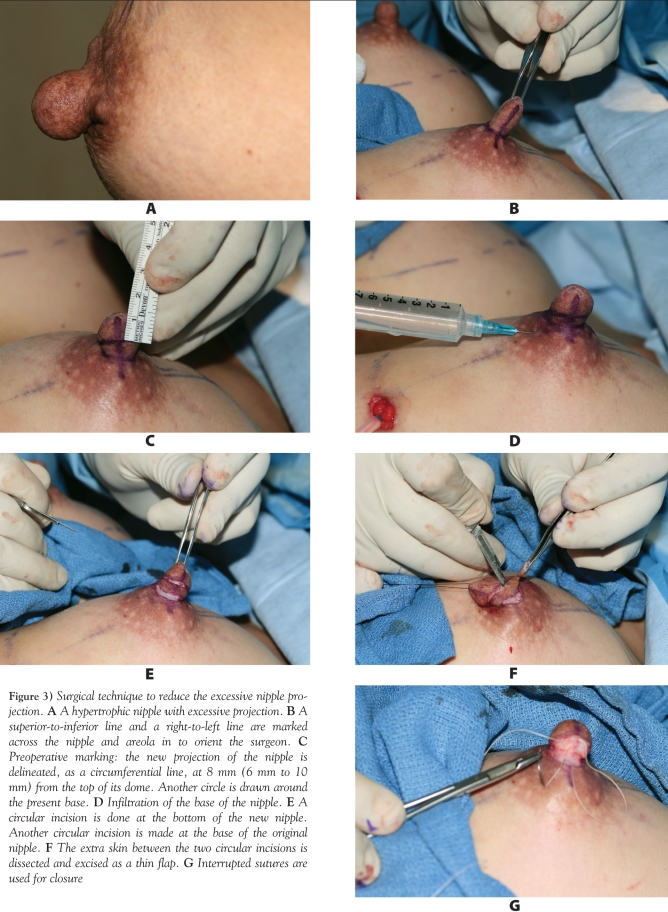
Figure 3 shows the step-by-step technique for the surgical reduction of the excessive nipple projection.
Figure 3).
Surgical technique to reduce the excessive nipple projection. A A hypertrophic nipple with excessive projection. B A superior-to-inferior line and a right-to-left line are marked across the nipple and areola in to orient the surgeon. C Preoperative marking: the new projection of the nipple is delineated, as a circumferential line, at 8 mm (6 mm to 10 mm) from the top of its dome. Another circle is drawn around the present base. D Infiltration of the base of the nipple. E A circular incision is done at the bottom of the new nipple. Another circular incision is made at the base of the original nipple. F The extra skin between the two circular incisions is dissected and excised as a thin flap. G Interrupted sutures are used for closure
Reducing the nipple diameter
Preoperative marking:
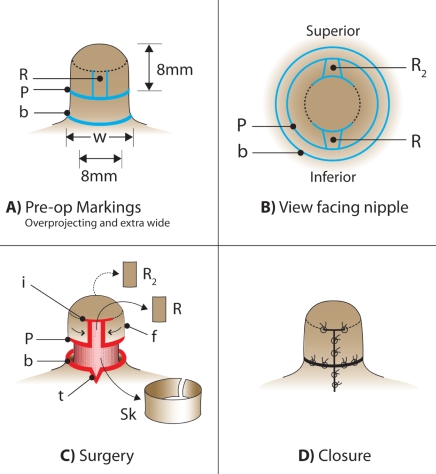
In approximately 10% of cases of hypertrophic nipples, in addition to the excessive projection, the diameter may also be too large (larger than 1 cm), and needs to be reduced. In such a case, the same marking described for the overprojecting nipple (Figure 1B) is completed. Then, the width of the present base is measured (Figure 2A: w). The excess width (exceeding 8 mm to 10 mm) is divided in two ([w–8 mm]/2), resulting in the width of each of two rectangles, placed at opposing sides of the nipple. These two small rectangles of skin, each measuring 2 mm to 5 mm in width, are marked on both the inferior and superior surfaces of the new nipple (Figure 2A: R; and Figure 2B: R and R2). Two transverse incisions, on both sides of the top of each rectangle, measuring approximately 2 mm to 3 mm, are marked just below the dome (Figure 2C: i). These two incisions will eventually allow the creation of two advancing flaps that will close each rectangular defect and narrow the new nipple in the process.
Figure 2).
A Preoperative marking of an overprojecting nipple with excessive width: The new height ‘p’ of the nipple is marked as in Figure 1B. The width of the present base ‘w’ is measured. The excess width exceeding 8 mm (w–8 mm) is divided between two rectangles (R and R2, as shown in Figure 2B). The first rectangle ‘R’ is drawn between the dome and line ‘p’, on the inferior surface of the nipple. Therefore, its width is equal to half the excess width of the base. In other words, the width of R or R2 is equivalent to w–8 divided by 2. (R = R2 = [w–8 mm]/2). B The second rectangle ‘R2’, identical to ‘R’, is drawn on the superior surface of the nipple. C Incisions are done along lines ‘p’ and ‘b’, as well as around the two rectangles, ‘R’ and ‘R2’. Two additional small transverse incisions (i) are made on each side of the top of each rectangle (in other words, along the lower limit of the dome) to allow for the creation of two advancement flaps ‘f’. A small triangle ‘t’ is marked at the inferior and superior midline of the basal incision ‘b’. The base of the triangle, being part of circle ‘b’, measures 2 mm to 5 mm. The two triangles of skin are excised to reduce the diameter of the old base perimeter ‘b’ so that it better fits the new inner base. D Final closure of all incisions. The small triangular defects at the base are closed after minimal bilateral dissection
Surgical reduction of excessive width:
For the nipple diameter to be reduced, the two skin rectangles (Figure 2C: R and R2) are excised as two very thin skin pieces by superficial dissection.
Two incisions (Figure 2C: i) are made on both sides of the superior limit of each bare rectangle. A minimal subcutaneous dissection of about 2 mm to 3 mm bilaterally is performed to raise two advancing skin flaps that are approximated with inverted 4-0 or 5-0 vicryl sutures (Figure 2C: f; Figure 2D).
To narrow the circular defect in the areola (Figure 2C: b), a small triangle (Figure 2C: t), with its base measuring 2 mm to 5 mm in width, is marked and excised at the inferior and superior midline of the basal incision ‘b’. Closure of these triangular defects is facilitated by minimal bilateral dissection.
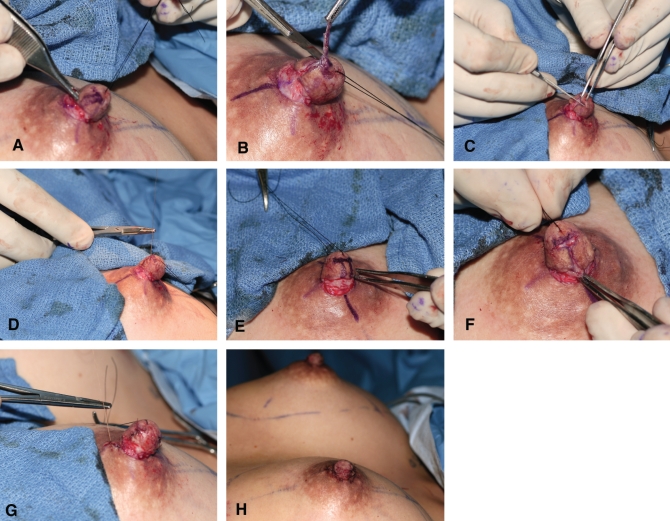
Figure 4 shows the step-by-step technique for the uncommon surgical reduction of the excessive nipple diameter.
Figure 4).
Surgical technique to reduce the excessive nipple diameter. Surgical technique to reduce the excessive nipple diameter – caption continued from previous page. A The surgical correction of the excessive nipple projection has just been completed. To reduce the excessive diameter, a rectangle (measuring in width one-half of the total excess diameter) is drawn on the inferior surface of the new nipple. B The rectangle of skin is excised from the inferior surface of the nipple. C Two bilateral transverse incisions, on both sides of the top of the rectangle, are made. D Two advancement flaps are dissected and the defect is closed. E The same technique is used to mark a rectangle on the superior surface of the nipple. F Closure of the rectangle defect on the superior surface of the nipple. G Excision and closure of a small triangle of skin from the inferior and superior basal incision, to narrow the circular defect around the base to fit the new slimmer nipple. H Final bilateral result
Dressing
A simple band-aid is placed over the nipple and areola to press down and stabilize the new nipple. A light gauze dressing is added on top of the band-aid to absorb any potential blood oozing.
Postoperative visits
The patient is seen the next morning, regardless of whether the nipple reduction is accompanied by a mammaplasty or a mastopexy. The dressing is changed and a new one is applied. The patient is then seen a week later, then in six months, then yearly.
RESULTS
A total of 30 operated nipples in 15 healthy female patients, aged 27 to 47 years (average 36 years) were included in the present series. The follow-up ranged from six months to 62 months (five years and two months), with an average of 29 months (two years and five months).
All scars healed nicely. There were no complications. The nipple sensation was preserved in all cases, as per the patients’ assessment. However, preservation of lactation function could not be tested in this series because it was not tried by any patient during the follow-up period. Theoretically, the ability to breast feed should be unharmed because this technique does not injure or alter the lactiferous ducts.
Overall, all patients (100%) had a breast augmentation performed at the same time as the nipple reduction procedure. All patients were Asian, except for one Caucasian.
Figures 5 to 7 show results of the nipple reduction technique.
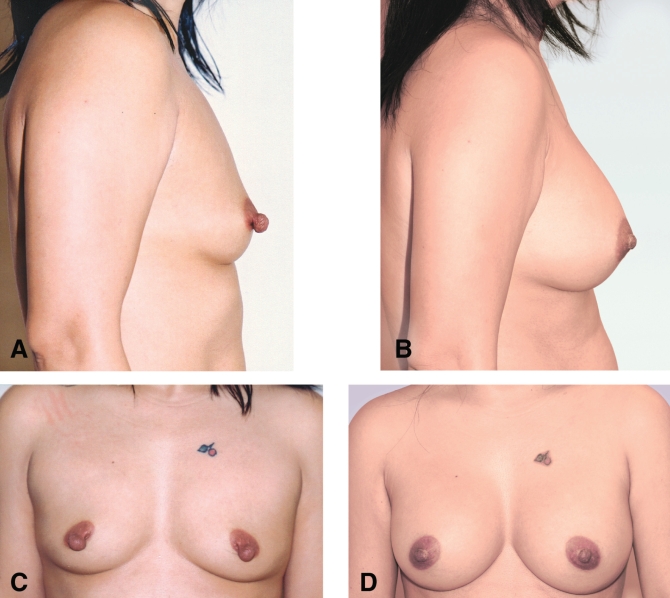
Figure 5).
Example of nipple reduction case: A and C Preoperative photographs of a 45-year-old Asian woman with severe nipple hypertrophy, including both excessive nipple projection and large nipple diameter. B and D Postoperative results 13 months after surgery. Breast augmentation was also performed
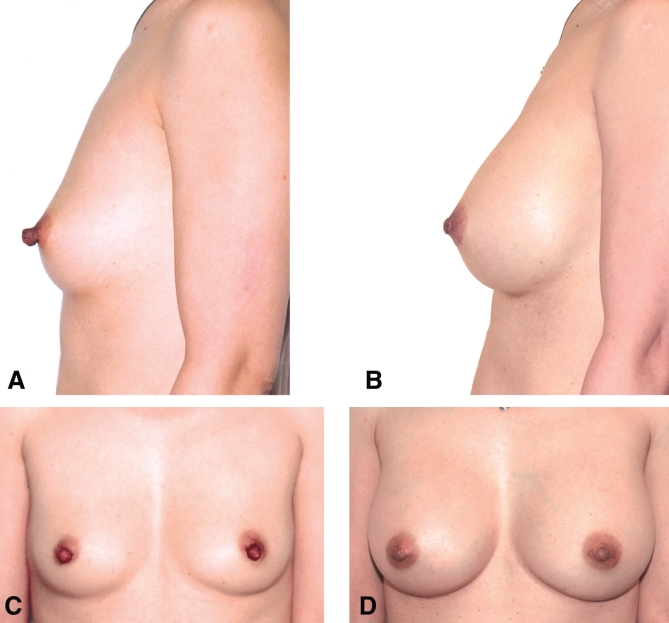
Figure 7).
Example of nipple reduction case: A and C Preoperative photographs of a 33-year-old Asian woman, suffering from excessive nipple projection. B and D Postoperative photographs six months after surgery. Breast augmentation was also performed
DISCUSSION
Ideally, nipple reduction has to take into account the sensation and the function of the nipple, not just its esthetics. The procedure should thrive to preserve the nipple’s nerve supply, as well as its network of lactiferous ducts. Both Vecchione’s nipple amputation (3) and Marshall’s core excision (4) intersect the lactiferous ducts, thus disrupting lactation and possibly affecting nipple sensation as well. Both Sperli’s (6) and Ferreira’s (7) methods correct the height and the diameter of the nipple, but the residual skin flaps may be compromised, resulting in a prolonged oedema and an increased risk. Bostwick (8) described two techniques for correcting the hypertrophic nipple, depending on whether lactation needs to be preserved. In the case of a patient who has successfully completed lactation, Bostwick suggested performing a simple resection of the top of the nipple, leaving the wound exposed to reepithelialize. On the other hand, if the patient wanted to preserve the ability to lactate, he opted for a circumferential ‘sleeve’ skin resection, followed by ‘telescoping back’ the exposed part of the nipple into the breast. This later technique is similar to the one presented in the present article. However, in the Bostwick technique, the analysis of the nipple esthetic was absent, the suggested new nipple projection of 2 mm to 3 mm seemed incredibly short, and the details of the technique were completely omitted. As well, the correction of the occasionally associated condition of excessive nipple diameter was not addressed.
Our nipple reduction approach has advantages. It is a very simple technique to plan and execute when compared with other classical techniques, such as Regnault’s (5), or even more recent techniques such as Lai’s (1,2). It may be used to address both nipple overprojection and excessive diameter. It is a physiological technique that preserves the nipple sensation and, in theory, does not interfere with its lactation function. It is a highly safe procedure with, so far, no recorded complications. It causes minimal edema and has a very short recovery period. It can be safely combined with areolar reduction, breast augmentation or mastopexy. Finally, it delivers a controlled and excellent esthetic result with a main (basal) scar that is hardly noticeable because it is located at the nipple-areola junction.
In summary, this simple and safe technique leads to gratifying results and a high patient and surgeon satisfaction rate.
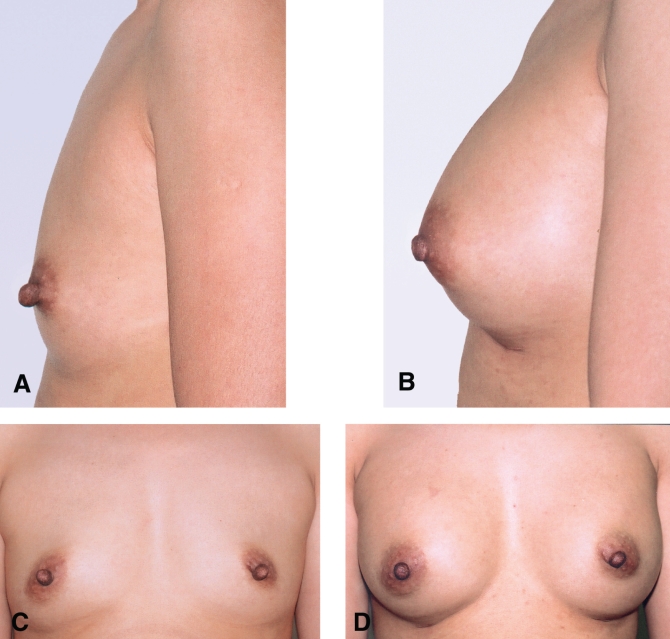
Figure 6).
Example of nipple reduction case: A and C Preoperative photographs of a 41-year-old Asian woman, suffering from excessive nipple projection. B and D Postoperative photographs 2.5 years after surgery. Breast augmentation was also performed
Acknowledgments
The authors express their thanks to Ildiko Horvath, medical artist, Montreal General Hospital (Montreal, Quebec), for her assistance in preparing the artwork; to Maria Iancu, administrative assistant, for the typing of the manuscript; to Minerva Khalife for her photographic contribution; to Barbara Armbruster MA for the editing, to Michael Fanous for the literature search, and to Stephanie Luetticken MBA for organizing the manuscript.
REFERENCES
- 1.Lai YL, Wu WC. Nipple reduction with a modified circumcision technique. Br J Plast Surg. 49:307. doi: 10.1016/s0007-1226(96)90160-5. [DOI] [PubMed] [Google Scholar]
- 2.Lai YL, Weng CJ, Samuel Noordhoft M. Areolar reduction with inner doughnut incision. Plast Reconstr Surg. 1998 May;:1695–9. doi: 10.1097/00006534-199805000-00044. [DOI] [PubMed] [Google Scholar]
- 3.Vecchione TR. The reduction of the hypertrophic nipple. Aesthetic Plast Surg. 1979;3:343–5. doi: 10.1007/BF01577873. [DOI] [PubMed] [Google Scholar]
- 4.Marshall KA, Wolfort FG, Cochran TC. Surgical correction of nipple hypertrophy in male gynecomastia: case report. Plast Reconstr Surg. 1977;60:277–9. doi: 10.1097/00006534-197708000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Regnault P. Nipple hypertrophy. A physiologic reduction by circumcision. Clin. Plast. Surg. 1975;2:391–6. [PubMed] [Google Scholar]
- 6.Sperli AE. Cosmetic reduction of the nipple with functional preservation. Br J Plast Surg. 1974;27:42–3. doi: 10.1016/0007-1226(74)90061-7. [DOI] [PubMed] [Google Scholar]
- 7.Ferrereira LM, Neto MS, Okamoto RH, Andrews J de M. Surgical correction of nipple hypertrophy. Plast Reconstr Surg. 1995;95:753–4. doi: 10.1097/00006534-199504000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Bostwick John., IIIPlastic and Reconstructive Breast Surgery Vol. 1Quality Medical Publishing, St-Louis: Missouri; 2000629–31. [Google Scholar]