Abstract
Hypertension may lead to irreversible damages in vital organs, such as heart, brain, and kidney, and may cause death in children if treatments are not given despite early diagnosis. This cross-sectional epidemiological study was conducted during 1 January–31 March 2004 to investigate the prevalence of hypertension among high school students. The study cohort included 1,041 students of six high schools, who were selected from among 14,789 students of 26 high schools in Sivas province of Turkey, using the cluster-sampling method. A questionnaire was used for collecting information from students on age, gender, smoking, and whether they or their families have any diseases. Blood pressure, height, and weight of the participitants were determined by the research group. Students whose repeated systolic or diastolic blood pressures were higher than the 95th percentile were considered to be hypertensive patients. Hypertension was prevalent among 4.4% (n=45) of the students. There was a significant correlation between prevalence of hypertension and body mass index. No significant correlation was found between prevalence of hypertension and other variables, such as smoking, age, gender, and family history of diabetes. The results suggest that hypertension is an important public-health problem among high school students. The results also showed that the body mass index was an important parameter in hypertension in such a study group. Researchers should consider overweight a causative risk factor for development of hypertension in early-onset groups.
Key words: Cross-sectional studies, Epidemiology, Hypertension, Prevalence, Risk factors, Turkey
INTRODUCTION
The incidence of hypertension in childhood varies from 1% to 3% (1,2). Hypertension, a chronic disease, can lead to failure in vital organs, such as heart, brain, and kidney, and can cause death. Unlike adults, the incidence of essential (primary) hypertension among children is lower, and 75–80% of all childhood hypertension is induced by renal and renovascular disorders. Congenital and vascular disorders, tumors, and history of renal disease may result in hypertension. Hypertension may lead to death, a sequel, or an irreversible damage in vital organs, such as heart, brain, and kidney, in children who do not undergo therapy despite early diagnosis (2-6).
The rising prevalence of overweight worldwide has led to an increased prevalence of essential hypertension among younger population. The present study was aimed at detecting the prevalence of hypertension and risk factors for hypertension among high school students in Sivas, Turkey.
MATERIALS AND METHODS
This cross-sectional epidemiological study was conducted from 1 January to 31 March 2004. Using a multistage sampling method, six high schools, as clusters, were selected systematically from 26 high schools (with 14,789 students) in Sivas. In total, 1,041 students—from 9th to 11th grades were chosen randomly from those six high schools and examined for hypertension and some other risk factors that could possibly cause hypertension. The study group included 1,020 of targereted 1,041 students. In total, 1,020 students—593 males (58.1%) and 427 females (41.9%)—with the mean age of 15.9±1.0 (range 14–18) years were available for contact in the present study.
A questionnaire was used for obtaining information from students by self-reporting on age, gender, smoking, and whether they or their families have had any diseases, such as urinary tract infection and diabetes. The blood pressure, height, and weight of each student were measured by the research group. Other family members were contacted for diabetes or hypertension if the student had hypertension. Based on the present habit, the smoking status was evaluated for each student.
Measurements of arterial blood pressure were performed in a quiet room after five minutes of resting in a sitting position. Right arms were kept at the same level of heart during the measurement. Cuff bladder was arranged to cover about 75% of the upper arm, and the measurements were performed using a tool calibrated to cover the upper arm fully (7,8). The cuff was inflated until the radial pulse was no longer audible from the antecubital area, and then the cuff was deflated 2–3 mm Hg per second while auscultating the pulse. While decreasing the cuff pressure, the onset of the sound was systolic blood pressure of the student, and the disappearance of the sound was accepted as diastolic blood pressure. The measurements were performed three times repeatedly at an interval of five minutes by the same specialist medical doctors during 9 am–12 noon. First measurements were excluded, and the average of the last two measurements was taken into account. Two weeks later, measurements of blood pressure were repeated for students who were above the 95th percentile according to the blood pressure percentile curves prepared by the USA Task Force Group. Students whose repeated systolic or diastolic blood pressures were higher than the 95th percentile were considered to be hypertensive patients.
Body-weight and height were measured using digital scales (Soehnle, Germany) sensitive to 0.1 kg and 0.5 cm respectively, and a non-stretch tape was fixed to a flat vertical wall. Body mass index (BMI) was calculated dividing the weight by square of height (kg/m2). The BMI values that were considered to be underweight, overweight, and obesity were defined as <5th, ≥85th and ≥95th percentile, respectively, of age- and sex-specific National Center for Health Statistics/Centers for Disease Control and Prevention (NHCS/CDC 2000) (9).
Data obtained were analyzed using the SPSS software (version 10.0.5) (SPSS Inc., Chicago, IL, USA). Chi-square, Pearson correlation, and Student's t-test were used in evaluating data. Additionally, multiple linear regression analyses were performed. BMI, age, gender, smoking, presence of diabetes mellitus or urinary tract infection, and presence of diabetes mellitus or hypertension among the members of the family were included in the models as independent variables. Results were expressed as mean±standard deviation.
RESULTS
Data of 1,020 students were used; 58.1% (n=593) of them were male, and 41.9% (n=427) were female. Their average age was 15.9±1.0 years. Table 1 shows the distribution of age-groups by gender.
Table 1.
Distribution of age group by gender
| Age (years) | Male (n=593, 58.1%) | Female (n=427, 41.9%) | Total (n=1020, 100.0%) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| 14 | 28 | 46.7 | 32 | 53.3 | 60 | 5.9 |
| 15 | 173 | 56.2 | 135 | 43.8 | 308 | 30.2 |
| 16 | 194 | 55.6 | 155 | 44.4 | 349 | 34.2 |
| 17 | 156 | 64.5 | 86 | 35.5 | 242 | 23.7 |
| 18 | 42 | 68.9 | 19 | 31.1 | 61 | 6.0 |
4.4% (n=45) of the students had blood pressures above the 95th percentile. Hypertension was prevalent among 5.4% of male and 3.0% of female students. Distribution of systolic and diastolic blood pressures by age and gender is given in Table 2. Both systolic and diastolic blood pressures were significantly (p<0.05) higher among the male students. Systolic blood pressures were higher among 18-year old male students, whereas diastolic blood pressures were significantly (p<0.05) higher than the values of female students in the 16–17 years old group.
Table 2.
Distribution of systolic and diastolic blood pressures by age and gender
| Age (years) | Systolic blood pressure (mean±SD) | Diastolic blood pressure (mean±SD) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| 14 | 109.6±9.4 | 111.9±9.0 | 70.5±9.4 | 73.6±7.5 |
| 15 | 111.2±10.3 | 109.3±9.1 | 71.3±8.6 | 70.1±8.4 |
| 16 | 112.4±10.6 | 110.0±9.0 | 72.7±8.4 | 70.7±7.6* |
| 17 | 112.5±11.8 | 109.0±9.5 | 72.5±8.9 | 70.1±6.8* |
| 18 | 111.7±10.7 | 108.7±6.8* | 72.1±7.7 | 72.1±7.3 |
| Total | 111.9±10.7 | 109.7±9.0* | 72.1±8.6 | 70.7±7.7* |
*Student t-test, p<0.05
The male students had the mean height of 171.5±7.7 cm, the mean weight of 59.4±9.9 kg, and BMI of 20.1±2.6, whereas the female students had the mean height of 160.6±5.7 cm, the mean weight of 53.4±8.4 kg, and BMI of 20.7±2.9. All the three mean values were observed to be significantly (p<0.05) different with respect to gender.
Table 3 demonstrates the correlation of systolic and diastolic blood pressures with age, height, weight, and BMI. Although systolic and diastolic blood pressures did not significantly (p>0.05) correlate with age, statistically significant (p<0.05) positive correlation was observed with height, weight, and BMI.
Table 3.
Relationship of systolic and diastolic blood pressures with age, height, weight, and body mass index in Pearson correlation analysis
| Variable | Systolic blood pressure | Diastolic blood pressure | ||
|---|---|---|---|---|
| R | p value | R | p value | |
| Age (years) | 0.02 | 0.44 | 0.03 | 0.31 |
| Height (m) | 0.24 | 0.00 | 0.14 | 0.00 |
| Weight (kg) | 0.30 | 0.00 | 0.26 | 0.00 |
| BMI (kg/m2) | 0.26 | 0.00 | 0.23 | 0.00 |
Hypertension was detected in 5.9% of one or both parents, but could not be detected in 3.8% of parents of the hypertensive students. This difference was not statistically significant.
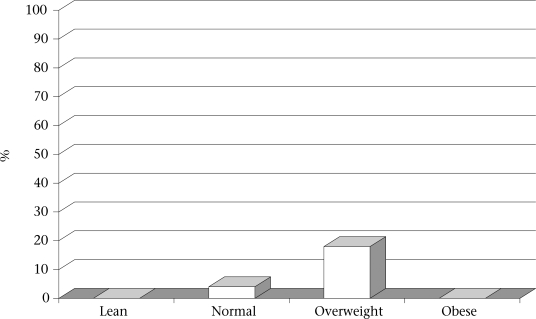
The involvement of some factors/variables in the prevalence of hypertension is shown in Table 4. The prevalence of hypertension was significantly higher among overweight students (18.4 %; p<0.05) than among non-obese students (4%). The figure shows the distribution of the prevalence of hypertension according to BMI. There was no significant difference between hypertension and age, gender, smoking, presence of diabetes mellitus, or hypertension among the members of the family. Multivariate regression analysis showed that only BMI was independently associated with hypertension (Table 5).
Table 4.
Percentage of hypertension due to some variables in the present study
| Variable | No. | % | Test* |
|---|---|---|---|
| Age (years) | |||
| 14 | 60 | 3.3 | NS* |
| 15 | 308 | 4.2 | |
| 16 | 349 | 4.9 | |
| 17 | 242 | 5.0 | |
| 18 | 61 | 1.6 | |
| Gender | |||
| Male | 593 | 5.4 | NS* |
| Female | 427 | 3.0 | |
| Smoking | |||
| Yes | 112 | 6.3 | NS* |
| No | 908 | 4.2 | |
| Diabetes melitus | |||
| Yes | 6 | - | NS* |
| No | 969 | 4.4 | |
| Family history of diabetes melitus | |||
| Yes | 160 | 3.8 | NS* |
| No | 860 | 4.5 | |
| Family history of (hypertension) | |||
| Yes | 304 | 5.9 | NS* |
| No | 716 | 3.8 | |
| Urinary tract infection | |||
| Yes | 110 | 7.3 | NS* |
| No | 910 | 4.1 | |
| Body mass index | |||
| Lean | 20 | - | 0.00 |
| Normal | 962 | 4.0 | |
| Overweight | 36 | 18.4 | |
| Obese | 2 | - | |
| Total | 1,020 | 4.4 | |
*Chi-Square; NS=Not significant
Table 5.
Relationship between hypertension and sociodemographic factors in multiple linear regression analysis
| Independent variable | β | p value | 95% confidence interval | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age (years) | 0.08 | 0.60 | −3.52 | 6.00 |
| Gender | −0.23 | 0.16 | −16.42 | 2.90 |
| Smoking | 0.22 | 0.19 | −4.00 | 19.85 |
| Family history of diabetes melitus | 0.33 | 0.06 | −0.86 | 26.75 |
| Family history of hypertension | 0.18 | 0.25 | −3.63 | 13.6 |
| Urinary tract infection | 0.14 | 0.36 | −9.06 | 24.2 |
| Body mass index | 0.50 | 0.00 | 0.62 | 3.43 |
Gender: Male=1, Female=2; Smoking, family history of diabetes melitus or hypertension and urinary tract infection: Yes=1, No=2
Fig.
Prevalence of hypertension according to body mass index among study subjects
DISCUSSION
In Turkish population, the prevalence of hypertension was 5.8% in the age-group of 13–20 years (10), 7.2% in the age-group of 13–18 years (11), 4.8% among females and 3.8% among males of 7–18 years age-group (12). The prevalence of hypertension was 6.9% in the age-group of 6–18 years in Brazil (13), 6.0% in the age-group of 14–19 years in the United States (14,15), 5.1% in the age-group of 8–16 years in Papua New Guinea (16), 2.9% in the age-group of 4–18 years in Germany (17), and 3.4% in the age-group of 4–18 years in Argentina (18). In our study, the prevalence of hypertension was 4.4%. The prevalence of hypertension reported in this study is consistent with the prevalence reported in the literature. The reason for the difference between the prevalence of hypertension in this study and those in the previous studies might be the usage of different age-groups.
In the present study, blood pressure correlated positively with height, weight, and BMI significantly (p=0.00). Furthermore, the BMI was also significantly (p=0.00) associated with hypertension after multivariate regression analysis. This result is consistent with the results of previous studies (19-22). As reported in some studies, race and ethnicity also have an impact on blood pressure. Blood pressure values are particularly higher for black and south East Asian races (23,24).
According to Turkish literature, investigating the association among age-groups, gender, and mean blood pressure values, Kıyak et al. reported the higher mean systolic and diastolic blood pressure values for girls aged 6–11 years when compared with their male peers (20). Tümerdem et al. stated that the mean systolic and diastolic blood pressure values for boys aged 7–12 years were higher than those of girls (21). Özkan et al. reported the higher mean diastolic blood pressure for girls aged 7–12 years (22) and the higher mean systolic blood pressure for boys aged 7–8 years and for girls aged 9–12 years. The study by Cşokun et al. demonstrated the similar mean systolic blood pressure values for both genders between the ages of 7 and 10 years (25). However, the mean systolic blood pressure was higher for boys aged 11–15 years, and the mean diastolic blood pressure values were higher for girls in both the age-groups. In a study by Koç et al., the mean systolic blood pressure values for boys at the ages of 6 and 15 years were observed to be higher, while girls had higher values in other age-groups (26). On the other hand, there were no significant gender-related differences in terms of the mean diastolic blood pressure values. According to data obtained in the present study, while the mean values for systolic blood pressure were higher for boys aged 18 years, the mean diastolic blood pressure values were significantly higher for boys aged 16–17 years. Boys in general had significantly higher mean values for both systolic and diastolic blood pressures when all the subjects enrolled were considered. On the other hand, when the blood pressure values were compared with respect to age-groups for both genders, no significant differences were observed. The discrepancies between studies may be attributed to socioeconomic and environmental factors.
If any one of the parents is hypertensive, the probability of being hypertensive for their children may be 28%. If both the parents are hypertensive, the probability of being hypertensive for their children may be 41.0% (27). Our results showed no significant difference between parents with and without hypertension.
It is known that infections in the urinary system, particularly reflu-dependent nephropathy and parenchyma damage, may lead to hypertension (28,29). In this study, the prevalence of hypertension was 7.3% among students who had urinary infection in the past and 4.1% among the non-infected group. There was no significant difference between these groups. It might be that the discrepancy might be based on memory factor.
Hypertension was demonstrated as an important public-health problem among high school students in Sivas. Our results showed that BMI was an important parameter in hypertension in such a study group. Frequent measurement of blood pressure of such cases, especially students with overweight, could be an effective preventive method for the early detection of hypertension and its complications. Effective therapy and continuous health education concerning healthy lifestyle are also essential in this age-group.
REFERENCES
- 1.Sinaiko AR. Hypertension in children. N Engl Med. 1996;335:1968–71. doi: 10.1056/NEJM199612263352607. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein D. In: Nelson Textbook of pediatrics. Philadelphia: Saunders; 2000. Systemic hypertension; pp. 1450–5. [Google Scholar]
- 3.Greydanus DE, Rowlett JD. Hypertension in adolescence. Adolesc Health Update. 1993;6:1. [Google Scholar]
- 4.Harshfield GA, Alpert BS, Pulliman DA, Somes GW, Wilson DK. Ambulatory blood pressure recordings in children and adolescents. Pediatrics. 1994;94((2 Pt 1)):180–4. [PubMed] [Google Scholar]
- 5.Gillman MW, Ellison RC. Childhood prevention of essential hypertension. Pediatr Clin North Am. 1993;40:179–94. doi: 10.1016/s0031-3955(16)38489-9. [DOI] [PubMed] [Google Scholar]
- 6.Bartosh SM, Aronson AJ. Childhood hypertension. Pediatr Clin North Am. 1999;46:235. doi: 10.1016/s0031-3955(05)70115-2. [DOI] [PubMed] [Google Scholar]
- 7.Update on the 1987 Task Force report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 8.Houtman PN, Dillon MJ. Routine measurement of blood pressure in schoolchildren. Arch Dis Child. 1991;66:567–8. doi: 10.1136/adc.66.5.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Body mass index-for-age percentiles, 2000. (http://www.cdc.gov /growthcharts).
- 10.Çalı Ş, Bircan İ, Ertuğ H. Antalya il merkezindeki liselerde arteryel hipertansiyon araştırması. Akdeniz Üniv Tıp Fak Derg. 1985;2:351–6. [Google Scholar]
- 11.İrgil E, Erkenci Y, Aytekin N, Aytekin H. Prevalence of hypertension among schoolchildren aged 13–18 years in Gemlik, Turkey. Eur J Public Health. 1998;8:176–8. [Google Scholar]
- 12.Uçar B, Kılıç Z, Çolak O, Öner S, Kalyoncu C. Coronary risk factors in Turkish schoolchildren: randomized cross-sectional study. Pediatr Int. 2000;42:259–67. doi: 10.1046/j.1442-200x.2000.01221.x. [DOI] [PubMed] [Google Scholar]
- 13.Simonatto DM, Dias MD, Machado RL, Abensur H, Cruz J. Arterial Hypertension in students of the Great Sao Paulo area. Rev Assoc Med Bras. 1991;37:109–14. [PubMed] [Google Scholar]
- 14.Sinaiko AR, Gomez-Marin O, Prineas RJ. Prevalence of significant hypertension in junior high school-aged children: the children and adolescent blood pressure program. J Pediatr. 1989;114:664–9. doi: 10.1016/s0022-3476(89)80718-8. [DOI] [PubMed] [Google Scholar]
- 15.O’Quin M, Sharma BB, Miller KA, Tomsovic JP. Adolescent blood pressure survey: Tulsa, Oklahoma, 1987 to 1989. S Med J. 1992;85:487–90. doi: 10.1097/00007611-199205000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Ampofo EK. Blood pressure distribution in children at Port Moresby, Papua New Guinea. PNG Med J. 1989;32:101–8. [PubMed] [Google Scholar]
- 17.Klimm HD, Reuter-Kuhn I. Pravalenz der hypertonie im kindesalter: eine untersuchung in 21 hauserztlichen praxen [Prevalence of hypertension in childhood: a study of 21 family physician practices] Fortschr Med. 1994;112:49–52. [PubMed] [Google Scholar]
- 18.Lodolo AD, Novoa P, Sakuyama E, Lodolo MM, Palma JA, Martinez JR. Arterial hypertension in childhood and adolescence. Rev Fac Cien Med Univ Nac Cordoba. 1989;47:19–22. [PubMed] [Google Scholar]
- 19.Lauer RM, Burns TL, Clarke WR. Assessing children's blood pressure—considerations of age and body size: the Muscatine study. Pediatrics. 1985;75:1081–90. [PubMed] [Google Scholar]
- 20.Kıyak M, Dişçi R, Ertem G. İlkokul çocuklarında kan basıncı araştırması. İstanbul Tıp Fakültesi Mecmuası. 1985;48:386–393. [Google Scholar]
- 21.Tümerdem Y, Ayhan B, Özçelik H, Tümerdem B, Alnıgeniş E. İlkokul çocuklarında arteryel kan basıncı değerlendirilmesi. Çocuk Sağlığı ve Hastalıkları Derg. 1993;36:353–61. [Google Scholar]
- 22.Özkan B, Akdağ R, Karakelleoğlu C, Alp H, Ceviz N, Energin M. Arterial blood pressure values in a school-age population in Erzurum: relation with age, sex weight, height and ponderosity index. Turk J Med Sci. 1994;22:171–7. [Google Scholar]
- 23.Munger RG, Gomez-Marin O, Prineas RJ, Sinaiko AR. Elevated blood pressure among Southeast Asian refugee children in Minesota. Am J Epidemiol. 1991;133:1257–65. doi: 10.1093/oxfordjournals.aje.a115837. [DOI] [PubMed] [Google Scholar]
- 24.Primatesta P, Brookes M, Poulter NR. Improved hypertension management and control: results from the health survey for England 1998. Hypertension. 2001;38:827–32. [PubMed] [Google Scholar]
- 25.Coşkun Y, Bayraktaroğlu Z. Coronary risk factors in Turkish school children—report of a pilot study. Acta Paediatr. 1997;86:187–91. doi: 10.1111/j.1651-2227.1997.tb08866.x. [DOI] [PubMed] [Google Scholar]
- 26.Koç A, Kösecik M, Ataş A, Erel Ö, Tatlı M. Şanlıurfa'da 6–16 yaş grubu çocuklarda hipertansiyon sıklığı ve etiyolojisi araştırması. Çocuk Sağlığı ve Hastalıkları Derg. 1999;42:513–21. [Google Scholar]
- 27.Saatçi Ü. Çocukluk çağında hipertansiyon. Katkı Pediatri Dergisi. 1992;13:93–113. [Google Scholar]
- 28.Pruitt AW. In: Behrman RE, Kliegman RM, Arvin AM, editors. Nelson Textbook of pediatrics. 15th ed. Philadelphia: Saunders; 1996. Systemic hypertension; pp. 1368–74. [Google Scholar]
- 29.Hellerstein S. Urinary tract infections. Pediatr Clin North Am. 1995;42:1433–57. doi: 10.1016/s0031-3955(16)40092-1. [DOI] [PubMed] [Google Scholar]