Abstract
Background
It is assumed, although not proven, that 13CO2-excretion following ingestion of 13C-octanoic acid (13C-OA) does not only depend on gastric emptying (GE) but also on absorption and metabolism of 13C-OA and endogenous CO2-production.
Aims
1. To test the effects of patient characteristics and of diseases that may impair 13C-OA-metabolism on GE parameters. 2. To compare different GE endpoints.
Methods
We investigated effects of age, gender, BMI and diseases with potential impact on 13C-OA-metabolism (including pancreatic, liver and lung disease, diabetes, IBD) on cumulative 4h-13CO2-excretion (4h-CUM) and T½ calculated by nonlinear regression model (NL, determined by shape of breath test curve) and generalized linear regression model (GLR, reflects absolute 13CO2-excretion) in 1279 patients and 19 healthy controls who underwent a standardized 13C-OABT.
Results
Digestive and metabolic disturbances hardly influenced 4h-CUM or T½ calculated by NL or GLR models. In the multivariate linear regression models, 4h-CUM was significantly predicted by diabetes adjusted for age, gender and IBD but influence of these parameters was small (R2=0.028, p<0.0001). T½NL and 4h-CUM were weakly correlated, even after exclusion of tests with unrealistically high estimates for T½NL (n=1095, R2=0.029, p<0.0001). Conversely, 4h-CUM was closely associated with T½GLR (exponential correlation, R2=0.774, p<0.00001, n=1279).
Conclusions
Influences of digestive and metabolic disturbances on 13CO2-excretion following 13C-OA- application are generally low. Thus, our findings resolve an important criticism of methods using absolute 13CO2-excretion for evaluation of 13C-OA-breath tests and suggest that such models (e.g. GLR model) may correctly identify T½ in a mixed patient population.
Keywords: absorption, 13CO2-excretion, gastric emptying test, gastroparesis, motility, scintigraphy
3. Introduction
Measurement of gastric emptying by scintigraphy is generally regarded as the reference method1. Breath tests using 13C-labeled substrates are not associated with radiation exposure and can be performed repeatedly, even in children or pregnant women2-4. Point of service or reference central laboratory measurements are possible5-7.
Delayed gastric emptying of solids usually precedes disturbances in gastric emptying of liquids8. Currently, two substrates are used to measure gastric emptying of solids by breath testing: the medium chain length fatty acid 13C-octanoic acid (13C-octanoic acid breath test, 13C-OABT) or the edible 13C-enriched blue-green alga, Spirulina platensis9-17. The substrates are rapidly absorbed in the duodenum, metabolized in the liver forming 13CO2 which is exhaled rapidly with low interindividual variability9. Thus, 13CO2 exhalation reflects gastric emptying of nutrients9.
Different mathematical models have been developed for analysis of gastric emptying curves derived from breath tests9, 11, 13, 16. Cumulative 13CO2-excretion over time is inversely related but analogous to the scintigraphic gastric emptying curve. Thus, in analogy to scintigraphy, cumulative 13CO2-excretion over a defined period of time may represent a logic and simple estimate of gastric emptying velocity. However, it is assumed that 13CO2-excretion does not only depend on gastric emptying velocity but also on absorption and metabolism of the substrate and endogenous CO2-production rates. For this reason, Ghoos et al. developed the original nonlinear (NL) regression model9. According to this model, T½NL indicates the time at which half of the 13CO2 is excreted, relative to the cumulative excretion when time is infinite. The major advantage of the NL model is believed to be that is independent of the endogenous CO2-production and only assumes a constant CO2 production during the test. Thus it is thought to be more robust than cumulative 13CO2-excretion.
An alternative analysis published by Lee et al. proposed a minimum number (n=3) of breath samples at pre-specified times during the 3 hour postprandial period to mathematically predict the gastric emptying endpoints measured by simultaneous scintigraphy11. Thus, based on the data of 22 diabetic patients and 6 healthy volunteers, a generalized linear regression (GLR) model accurately predicted the expected scintigraphic T lag and T½. The GLR model requires fewer breath samples and, thus would be of high clinical utility. However, none of the above mentioned mathematical approaches for analysis of breath test data has been applied to and compared in a large patient cohort, so far.
The aims of this study were twofold: Firstly, to analyze the effects of various parameters including sex, BMI and age as well as diseases, which may impair absorption or postabsorptive metabolism of 13C-octanoic acid and/or are frequently associated with gastric emptying disturbances on cumulative 13CO2-excretion and on gastric emptying endpoints obtained by the NL and the GLR model in 1279 patients and 19 healthy volunteers who underwent a standardized 13C-OABT at the Israelitic Hospital in Hamburg, Germany. Secondly, we aimed to compare cumulative 13CO2-excretion and gastric emptying half times calculated by both models.
4. Materials and Methods
4.1 Subjects
We performed 1395 13C-OABT for clinical indications in patients with upper abdominal symptoms. Of these, 116 were excluded from analysis because part of the breath test or clinical data was unavailable. In the remaining 1279 patients the presence or absence of pancreatic exocrine insufficiency, liver or lung disease, diabetes mellitus, reflux disease, fundoplication, functional gastrointestinal diseases, inflammatory bowel disease, diverticular disease, small intestinal bacterial overgrowth, carbohydrate intolerance, psychiatric disease and malignant tumors was evaluated according to clinical files. In addition, 19 healthy subjects (8 women) underwent the test for evaluation of normal values. Healthy subjects gave informed written consent (age: 26±2 years, BMI: 23.0±2.7 kg/m2). None of the controls reported history of relevant diseases and/or abdominal surgery except uncomplicated appendectomy (performed in one female). These investigations had been approved by the local ethical committee.
4.2 Performance of 13C-OABT
The 13C-OABT was performed as standardized by Delbende et al.10. Following overnight fast, all subjects ingested a test meal consisting of 2 slices of white bread, 10 g butter, 50 g ham, 200 ml orange juice and an omelet made from one egg with egg yolk doped with 91 mg 13C-octanoic acid (Euriso-top, Saarbruecken, Germany, isotopic enrichment of substrate: 99.0 % atom 13C). This test meal contains 380 kcal (1600 kJ, 19% protein, 53% carbohydrate, 31% fat) and is similar to the one used by Lee et al.11. Subjects were encouraged to eat the meal within 10 minutes and were asked to strictly avoid physical activity during study procedures. Breath samples were collected into 1.3 l aluminium bags before ingestion of the meal and at 15-minute intervals for 240 minutes postprandially. 13CO2-excretion in breath was subsequently analyzed using isotope-selective non-dispersive infrared spectroscopy (IRIS, Wagner Analysen Technik GmbH, Bremen, Germany)5-7. 13 C-abundance in breath was expressed as per mil relative difference (δ ‰) from the universal reference standard (carbon from Pee Dee Belemnite limestone). 13C-enrichment was defined as the difference between basal, preprandial 13C-abundance in breath and 13C-abundance at the defined time points postprandially and was given in δ over basal (DOB, ‰). The resulting curve reflected the variation of 13CO2-enrichment in breath over time18.
4.3 Analysis of gastric emptying parameters
4.3.1 Cumulative 13CO2-excretion
Based on the 13C-concentrations in breath measured at 15min intervals over 4 h, cumulative 13CO2-excretion was calculated by addition of mean 13CO2-excretion during each of the sixteen 15 min intervals (transformed to μmol, compare below). In the absence of a simultaneous reference method (scintigraphy), cumulative 13CO2-excretion over 4 hours calculated using the entire 17 breath samples (obtained at baseline and every 15 minutes over 4 hours) represents the most objective parameter based on actual measurements rather than a derived parameter. Moreover, it has been shown recently that cumulative 4 h-13CO2-excretion and scintigraphic T½ give highly concordant results (concordance correlation coefficient: 0.77) in 57 experiments of subjects with normal, accelerated or delayed gastric emptying undergoing simultaneous breath testing and gastric emptying scintigraphy 19.
4.3.2 Nonlinear (NL) regression analysis of Ghoos et al
For analysis of breath test results and for calculation of gastric emptying parameters, NL regression analysis was applied according to Ghoos et al.9, 10. The equation used for calculation of T½NL is given by
where y is the percentage of cumulative 13C-excretion in breath, t is time in hours, and m, k and β are constants with m being the total cumulative 13C-recovery in percent of dose when time is infinite. For calculation of m DOB-values were converted to % of administered dose.
Half time of gastric emptying is given by
Ghoos et al. showed that values calculated for T½NL uncorr overestimate gastric emptying times by about one hour (66 minutes) compared with simultaneously performed scintigraphy. Moreover, the linear regression line which shows the correlation between gastric emptying parameters derived from scintigraphy and breath testing slightly deviates from the y=x line (1.12 versus 1). Thus, we corrected breath test data to give the results expected according to scintigraphy using the following formula:
Since this adjustment of breath test T½ has been criticized before as inappropriate use of regression analysis20, evaluations were also performed using T½NL uncorr. This led to the expected shift of T½ to higher values, but otherwise hardly affected the results and the conclusions to be drawn. Thus, these data are not presented.
4.3.3 Generalized linear regression (GLR) analysis of Lee et al
DOB values were used to calculate the quantity of 13C appearing in breath per unit time according to Lee et al.: 13C (μmol/min) = DOB × 0.0112372 × CO2 production/min, where 0.0112372 is the isotopic abundance of the limestone standard (compare above) and CO2 production is estimated to be 5 mmol/m2/min. Data were analyzed as previously described by Lee et al.11. The following equation was used to calculate T½GLR (calculation performed by Excel-program):
In this formula, the gastric emptying parameter is predicted using 13CO2-production rates in micromoles per minute at the specific time points (i.e. 13C30min, and 13C150min). LP ½ is the linear predictor (i.e. weighted sums of 13CO2 production rates), T½GLR is defined as the reciprocal of this linear predictor.
4.4 Statistics
Statistical analyses including linear and nonlinear regression analysis were performed using JMP® version 6.0.3 from SAS. Analyses were performed on 4 h-cumulative 13C-exhalation, T½NL, the m-value derived from the method of Ghoos et al and T ½GLR. Univariate and multivariate linear regression analyses were used to investigate the influence of clinical parameters on 4 h-cumulative 13C-exhalation, T½NL, the m-value derived from the method of Ghoos et al and T ½GLR. The following parameters were tested as predictors in the univariate and multivariate models: age, gender, BMI and presence or absence of gastroesophageal reflux disease, carbohydrate intolerance, functional gastrointestinal diseases, psychiatric disorders, diverticular disease, diabetes mellitus, post-fundoplication, liver disease, malignant tumor, lung disease, inflammatory bowel disease, small intestinal bacterial overgrowth and pancreatic exocrine insufficiency. For the multivariate analyses, manual stepwise model building was performed.
5. Results
5.1 Patient characteristics
Of the 1279 patients with evaluable data, 861 (67.3%) were women. Females were significantly shorter (166±7 vs. 178±8 cm, p<0.0001), had lower weight (65.8±14.9 vs. 77.8±13.7 kg, p<0.0001) and tended to have lower BMI compared to male participants (24.0±5.2 vs. 24.5±3.8 kg/m2, p=0.054) whereas mean age was similar (54.8±17.7 vs. 54.3±16.3 yrs). In 1126 patients, one or more of the following diagnoses were documented: 23.2% gastroesophageal reflux disease, 18.3% carbohydrate intolerance, 15.2% functional gastrointestinal diseases, 14.2% psychiatric disorders, 13.7% diverticular disease, 11.3% diabetes mellitus, 9.9% post-fundoplication, 9.1% liver disease, 9.1% malignant tumor, 6.9% lung disease, 6.3% inflammatory bowel disease, 5.9% small intestinal bacterial overgrowth, 2.7% pancreatic exocrine insufficiency. There were other diagnoses in the remaining 171 patients.
5.2 Estimates of gastric emptying parameters
Mean data for DOB values over time of the 1279 patients with upper abdominal symptoms and of 19 healthy volunteers are shown in figure 1.
Fig. 1.
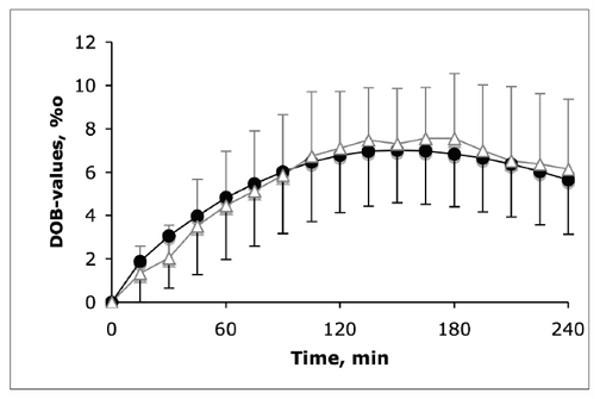
13C-exhalation over time following ingestion of 13C-octanoic acid together with a test meal in 1279 patients with upper abdominal symptoms (closed circles) and 19 healthy controls (open triangles). 13C-exhalation is given in delta over basal (DOB). The figure shows mean values ± standard deviation.
Frequency distributions of cumulative 4h-13CO2-excretion and of gastric emptying T½ calculated according to the NL and the GLR model are shown in figure 2. Thus, while median values and interquartile ranges (Tab. 1) for cumulative 4h-13CO2-excretion, T½NL and T½GLR were generally similar for patients and controls for all endpoints, figure 2 shows that, with the NL and GLR models, T½ data exceed the range of gastric emptying times typically observed with scintigraphy (up to 300 minutes). In fact, with the NL model, the estimated T½ exceeds 1000 minutes in 115 patients. With the GLR model, values >1000 minutes were observed in 3 patients.
Fig. 2.
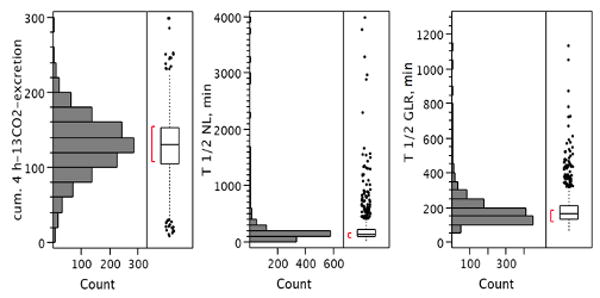
Distribution of cumulative 4h-13CO2-excretion (left panel), T½NL (middle panel) and T½GLR (right panel) obtained in 1279 patients with upper abdominal symptoms. Note that T½ exceeds 1000 minutes in 115 patients with the NL model and in 3 with the GLR model (data of patients with T½NL>4000 min not shown).
Table 1.
Gastric emptying parameters calculated according to different mathematical models in patients with upper abdominal symptoms and healthy volunteers.
| Cumulative 13C-exhalation, μmol | T½NL, min | T½GLR, min | |
|---|---|---|---|
| Patients | 130 (105-153) | 140 (98-220) | 164 (134-207) |
| Controls | 134 (97-170) | 125 (95-159) | 165 (140-222) |
Median values and interquartile ranges (given in parenthesis) for 1279 patients with upper abdominal symptoms and 19 healthy controls.
5.2.1. Impact of parameter “m” on estimates of T½ in NL model
The parameter m is meant to reflect the percentage of 13C-dose administered that is exhaled at time = infinity. Therefore, an m-value markedly exceeding 100% indicates an inappropriate estimation of 13CO2-excretion by the NL model. We observed a highly significant (nonlinear) association (R2=0.867, p<0.00001) for correlation between natural logarithm of T½NL and natural logarithm of m-value showing that tests with estimates for m greater than 100% were associated with unrealistic estimates for T½NL greater than 1000 minutes.
5.3 Correlation between gastric emptying parameters
We examined the relationship between T½GLR or T½NL and cumulative 4h-13CO2-excretion.
5.3.1 Correlation between 4h-13CO2-excretion and T½GLR of Lee et al
As shown in figure 3 A, an excellent linear correlation was observed between cumulative 4h-13CO2-excretion and LP½ (R2= 0.774, p<0.0001) for the whole patient population. LP½ is the linear predictor which is calculated as the weighted sums of 13CO2 production rates and which represents the reciprocal of T½GLR. Accordingly, an identically tight, yet exponential correlation was observed between cumulative 4 h-13C-exhalation and T½GLR (3B). However, for the vast majority of breath test data (all tests with cumulative 13CO2-excretion between 40 and 200 μmol, n=1209, equivalent to 94.5% of all tests) a highly significant linear correlation could be established (R2=0.711, p<0.00001). Only the extremes with very low (n=27) or high (n=43) cumulative 13CO2-excretion markedly deviated from this approximately linear part of the curve.
Fig. 3.
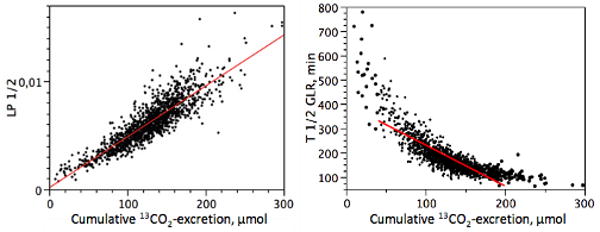
An excellent linear correlation was observed between LP½ and cumulative 4 h-13C-exhalation (R2=0.774, p<0.00001) (A). LP½ is the linear predictor which is calculated as weighted sums of 13CO2 production rates (derived from 3 breath samples, only) and is defined as the reciprocal of T½GLR. Accordingly, an identically tight, yet exponential correlation was observed between cumulative 4 h-13C-exhalation and T½GLR (B). For the vast majority of breath test data (all tests with cumulative 13CO2-excretion between 40 and 200 μmol, n=1209, equivalent to 94.5% of all tests) a highly significant linear correlation could also be established (solid line, R2=0.711, p<0.00001). Only the extremes with very low (n=27) or high (n=43) cumulative 13CO2-excretion markedly deviate from this approximately linear part of the curve.
5.3.2 Correlation between cumulative 4h-13CO2-excretion and T ½ NL of Ghoos et al
When calculated for the whole patient population (n=1279), T½NL did not correlate well with 4h-13CO2-excretion (R2=0.012) and, when limited to tests with m-values below 100%, the correlation was still very weak (R2=0.029, p<0.0001).
5.3.3 Correlation between T½GLR and T½NL
Taking all data into account, we observed no meaningful correlation between T½GLR and T½NL. We conducted further analysis on the 85.6% (n=1095) of all tests that had m-values <100% in the NL model. We applied a stepwise approach (using 5% steps for the m-values) to identify the subgroup in which the T½NL results were optimally correlated with T½GLR results. The highest correlation coefficient was observed for tests with m-values between 40% and 70% (R2=0.571, p<0.0001). However, this included only 31.7% of tests (n=406). For tests with m-values between 25% and 80%, the correlation was significant (R2=0.378, p<0.0001), and 69.1% of the tests could be compared using the 2 models (n=884).
5.4 Impact of gender on gastric emptying parameters
Compared with men, women had significantly increased DOB-values (fig. 4) and cumulative 13CO2-excretion (131±40 vs. men 124±39 μmol, p=0.0015). Accordingly, T½GLR was significantly lower in women (183±92 vs. men 196±106 min, p=0.02). By contrast, T½NL was similar in both groups (142±79 vs. men 143±84 min, NS, for 1095 patients with m-values <100%).
Fig. 4.
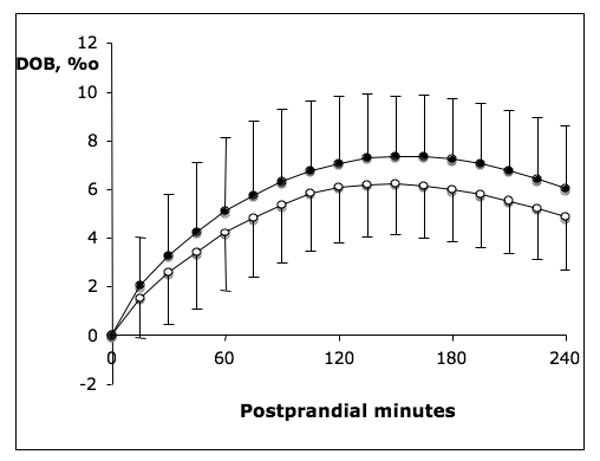
Differential 13C-exhalation (expressed as DOB) in men (n=418, open circles) and women (n=861, closed circles). Throughout the postprandial observation period women always had significantly higher DOB-values compared with men (p<0.0001).
5.5 Effect of patient characteristics and specific diseases on gastric emptying parameters
5.5.1 Univariate linear regression analysis
Results of univariate linear regression analysis for the association between clinical and gastric emptying parameters are shown in table 2. The most consistent, albeit small, effects on gastric emptying parameters were shown for gender (see above), age (T½GLR decreased and cumulative 13CO2-excretion increased with age), diabetes mellitus (associated with prolonged gastric emptying and decreased cumulative 13CO2-excretion) and bacterial overgrowth based on breath test (associated with accelerated gastric emptying). Pancreatic exocrine insufficiency and liver disease affected T½NL only if all tests including those with m-values greater than 100% were taken into account. The other gastric emptying parameters were not associated with presence of pancreatic exocrine insufficiency or liver disease. There was no significant association between any gastric emptying results and lung disease. Patients with IBD tended to have decreased cumulative 13CO2-excretion associated with prolonged T½GLR. By contrast, patients with malignant disease had increased cumulative 13CO2-excretion and tended to have decreased T½GLR.
Table 2.
Influence of clinical parameters on gastric emptying: Results of univariate linear regression analysis.
| T ½ NL | T ½ GLR | Cum. 4h-13CO2-excretion | ||
|---|---|---|---|---|
| All data | m<100% | All data | All data | |
| Sex | Ø | Ø | R2=0.004↓(a)* | R2=0.008↑ (c) ** |
| Age | Ø | Ø | R2=0.008↓(b)** | R2=0.005↑ (d) ** |
| BMI | Ø | Ø | Ø | Ø |
| PEI | R2=0.032↑*** | Ø | Ø | Ø |
| Liver disease | R2=0.003↑§ | Ø | Ø | Ø |
| Lung disease | Ø | Ø | Ø | Ø |
| Diabetes mellitus | Ø | R2=0.006↑* | R2=0.010↑*** | R2=0.008↓** |
| GERD | R2=0.003↑§ | Ø | Ø | Ø |
| Fundoplication | Ø | R2=0.005↓* | Ø | Ø |
| IBD | Ø | Ø | R2=0.004↑* | R2=0.006↓** |
| FGID | Ø | Ø | Ø | Ø |
| Constipation | Ø | Ø | Ø | R2=0.003↑§ |
| Diverticular disease | Ø | R2=0.009↑** | Ø | Ø |
| Carbohydrate intolerance | Ø | Ø | Ø | Ø |
| SIBO | Ø | R2=0.003↓§ | R2=0.003↓* | Ø |
| Psychiatric disease | Ø | Ø | Ø | Ø |
| Malignant disease | Ø | Ø | R2=0.006↓** | R2=0.002↑§ |
For the NL model, associations between patient characteristics and T½ have been tested for all patients (n=1279) and additionally for the subgroup of patients with m-values below 100% (n=1095).
BMI: body mass index; PEI: pancreatic exocrine insufficiency; GERD: gastroesophageal reflux disease; IBD: inflammatory bowel disease; SIBO: small intestinal bacterial overgrowth, FGID: functional gastrointestinal disease.
p<0.10;
p<0.05;
p<0.01;
p<0.001
decreased if present
increased if present
(a) decreased values in women
(b) decreased values in older subjects
(c) increased values in women
(d) increased values in older subjects
5.5.2 Multivariate linear regression analysis
In the multivariate linear regression models, the consistent association of gastric emptying results was with diabetes mellitus. Cumulative 4h-13CO2-excretion was significantly predicted by diabetes adjusted for age, gender and presence of inflammatory bowel disease (R2=0.028, p<0.0001). T½GLR was significantly predicted by diabetes adjusted for age and gender, bacterial overgrowth and malignant disease (R2=0.032, p<0.0001). T½NL for tests with m<100% was significantly predicted by diabetes adjusted for diverticular disease, fundoplication and bacterial overgrowth (R2=0.022, p<0.0001). However, although significant multivariate linear regression models could be developed for all gastric emptying parameters, the overall variance attributable to these predictors was low (R2≤0.037).
6. Discussion
In this study, we analysed 13C-OABT obtained in nearly 1300 subjects. Our main aim was to evaluate the influence of patient characteristics on cumulative 13CO2-excretion and on gastric emptying parameters obtained by the NL and GLR models. In consideration of these results we aimed to compare T½NL, T½GLR and cumulative 13CO2-excretion.
6.1 Influence of patient characteristics on cumulative 13CO2-excretion
In essence, our data demonstrate that diseases which might affect absorption and/or postabsorptive metabolism of 13C-octanoic acid such as pancreatic exocrine insufficiency, liver and lung disease have no detectable effect on cumulative 13CO2-excretion, T½GLR or T½NL (the latter applies if tests with realistic m-values are taken into account).
Our data confirm the observation by Maes et al. that 13CO2-excretion following administration of 13C-octanoic acid was similar in patients with or without pancreatic disease21 including those (10/14) with steatorrhea as a sign of severe pancreatic exocrine insufficiency22, 23. Moreover, metabolism of octanoic acid is maintained not only in patients with steatohepatitis but also in patients with liver cirrhosis24, 25. Disturbances of 13CO2-exhalation in patients with lung diseases are only expected in patients with very severe disease and reduced CO2-diffusion capacity. Literature data on potential impairment of 13C-breath tests in such cases are not available.
According to our data, patients with IBD have decreased cumulative 13CO2-excretion. This may be attributed to delayed gastric emptying as has been reported in patients with Crohn's disease26-29. However, reduced absorption of 13C-octanoic acid might also occur in a subset of patients with proximal small intestinal involvement.
By contrast, bacterial overgrowth and malignant disease are correlated with decreased T½GLR. Hypothetical mechanisms apart from acceleration of gastric emptying include metabolization of 13C-octanoic acid by the bacterial flora and a catabolic state with increased CO2-production, respectively. Conversely, patients with rapid gastric emptying and an associated acceleration of small intestinal transit may also have false positive findings in the H2-breath test that is used for diagnosis of bacterial overgrowth.
Another factor that may hamper reliability of parameters based on absolute 13CO2-excretion such as cumulative 13CO2-excretion and T½GLR is varying physical activity during performance of breath tests30. Even moderate activity such as walking roughly doubles energy expenditure compared with sedentary subjects and has corresponding effects on endogenous CO2 production31, 32. However, this confounding factor can be mitigated by asking all patients to strictly avoid physical activity, as we did in our study.
Thus, we have shown in a large patient cohort that cumulative 4h-13CO2-excretion is only marginally influenced by patient characteristics and diseases with theoretical impact on absorption and/or postabsorptive metabolism of 13C-octanoic acid. Since these findings resolve an important criticism of methods using absolute 13CO2-excretion for evaluation of breath test data, they indirectly support the hypothesis that such models may provide accurate estimates of gastric emptying parameters. In accordance with this assumption, a recent report has shown that cumulative 4 h-13CO2-excretion and scintigraphic T½ gave highly concordant results (concordance correlation coefficient: 0.77) in 57 experiments in healthy subjects undergoing simultaneous breath testing and gastric emptying scintigraphy19. The concordance correlation coefficient was even higher when comparing scintigraphic T½ with T ½ obtained by the GLR regression model. Our current findings further imply that reliable results may not only be obtained in healthy subjects but also in a mixed patient population.
6.2 Comparison of cumulative 4h-13CO2-excretion and non-linear regression model
Distributions of breath test data analyzed according to these two models varied markedly. The NL model led to extreme estimations of gastric emptying with T½ exceeding 1000 minutes in almost 10% of patients.
T½NL indicates the time at which half of the 13CO2 is excreted relative to the cumulative excretion when time is infinite. The parameter m of the NL model is defined as the relative amount of 13C which is cumulatively exhaled when time is infinite (expressed in % of dose)9. The parameter m is derived from the regression curve and, by the model, it determines estimation of T½NL.
As a result of this assumption in the NL model, the breath test curve can only be approximated adequately if the peak of the curve and a steady decline are achieved within the observation period while breath samples are collected, and therefore m is indeed constant. On the other hand, if 13C-exhalation continues to rise through the 4 h observation period and steady state in the cumulative 13CO2-excretion is not achieved, both the m-value and T½NL will be overestimated. The m-value should theoretically not exceed 100% of the given dose, but it was found to be much higher in more than 10% of patients in our series.
Compared with the original study performed by Ghoos et al.9, we used a higher caloric test meal. The choice of the calorie content of a gastric emptying test meal is the subject of disagreement and controversy. Some suggest that total caloric loads should be in excess of 300 kcal33 on the grounds that the meal should provide some assessment of the capacity of the stomach to respond to a “stress”; others have used lower calorie content34 with low fat to ensure that patients who experience nausea or vomiting are able to complete the meal during the test. However, consensus statements also concede that “meal composition may need to be altered depending on the patient's specific symptoms”35.
The type of test meal used in our study was previously validated by Delbende et al. who applied the formulae developed by Ghoos et al. and showed a highly significant correlation between breath test results and scintigraphic values in 88 subjects10. However, it is important to notice that with the higher caloric test meal, the 13C-excretion curve may be shifted to the right so that the maximum of the curve and steady decline are not achieved within the 4 h observation period. This may lead to overestimation of the m-value. With lower caloric meals or prolongation of the observation period beyond 4 hours, overestimation of the m-value might be mitigated but these measures may reduce clinical utility of the test.
6.3 Generalized linear regression model
As shown in figure 3 T½GLR, is tightly associated with cumulative 4h-13CO2-excretion. When considering the entire patient data set, the curve is best represented by an exponential function. However, for the vast majority of data (94.5% of all tests) a linear correlation can be established that approximates the curve adequately. These findings are remarkable because the GLR model is based on only 3 breath samples collected over less than 3 hours. Thus, our observations indirectly support the conclusion of the study by Lee et al.11 that the simplified breath test can be expected to correctly identify T½ which in their study was compared to simultaneous scintigraphy. Application of the GLR model may markedly facilitate the use of 13C-octanoic breath tests in clinical practice. The test meal used in our study and the one used by Lee et al. for establishment of the GLR model were similar but not identical. There were differences with respect to fluid volume (200 instead of 440 ml) and nutrient composition (380 kcal, 19% protein, 53% carbohydrate and 31% fat versus 420 kcal, 18% protein, 45% carbohydrate and 37% fat). These are potential confounding factors because it is not clear whether the weighting factors established by Lee et al. can be applied to our test meal.
6.4 Summary
We have shown in a large group of heterogenous patients that diseases which might affect absorption and/or postabsorptive metabolism of 13C-octanoic acid have no detectable effect on cumulative 13CO2-excretion and that the effect of age and gender is small. These findings resolve an important criticism of methods using absolute 13CO2-excretion for evaluation of breath test data. Thus, they indirectly support the hypothesis that such models may serve as a reliable marker of gastric emptying velocity not only in healthy volunteers but also in a mixed patient population.
T½GLR correlated astonishingly well with cumulative 4h-13CO2-excretion, although based on only 3 instead of 17 breath samples. These results support the findings of previous studies that the simplified breath test can be expected to correctly identify T½ and that application of the GLR model may markedly facilitate the use of 13C-octanoic breath tests in clinical practice. However, since our test meal slightly deviated from the one used for establishment and evaluation of the GLR model, weighting factors used for calculation of T½GLR would need to be adapted or at least further validated with simultaneous scintigraphic studies.
T½NL resulted in large overestimation of gastric emptying time in more than 10% of patients. This was explained by lack of steady state 13C-exhalation at the end of the observation period and may partly depend on the size of the test meal used. At present, we would recommend a necessary, additional precaution, that is to estimate the parameter m, and to report with extreme caution any T½NL estimated when m approximates or exceeds 100%.
Acknowledgments
Dr M Camilleri's work on this project was supported by K24 NIH grant, DK 02638.
The work of Dr J Keller, Dr V Andresen and Dr P Layer on this project was supported by the Anna-Lorz-Foundation, Esther-Christiansen-Foundation and the Gustav & Catharina-Schürfeld-Foundation.
List of abbreviations
- 4h-CUM
cumulative 4h-13CO2-excretion
- 13C-OABT
13C-octanoic acid breath test
- GE
gastric emptying
- GLR
generalized linear regression
- LP
linear predictor
- NL
nonlinear regression
- T½
gastric emptying half time
Footnotes
disclosures: None of the authors has any competing interests.
References
- 1.Parkman HP, Hasler WL, Fisher RS. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology. 2004;127:1592–1622. doi: 10.1053/j.gastro.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 2.Schoeller DA, Schneider JF, Solomons NW, Watkins JB, Klein PD. Clinical diagnosis with the stable isotope 13C in CO2 breath tests: methodology and fundamental considerations. J Lab Clin Med. 1977;90:412–421. [PubMed] [Google Scholar]
- 3.Maes BD, Ghoos YF, Geypens BJ, Hiele MI, Rutgeerts PJ. Relation between gastric emptying rate and energy intake in children compared with adults. Gut. 1995;36:183–188. doi: 10.1136/gut.36.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramirez A, Wong WW, Shulman RJ. Factors regulating gastric emptying in preterm infants. J Pediatr. 2006;149:475–479. doi: 10.1016/j.jpeds.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 5.Leodolter A, von Arnim U, Gerards C, Glasbrenner B, Malfertheiner P. Is the accuracy of isotope-selective non-dispersive infrared spectrometry (NDIRS) sufficient for determination of gastric emptying using the 13C-octanoic acid breath test (13C-OABT): Comparison with isotope-ratio mass spectrometry (IRMS) Gastroenterology. 2000;118:A850. [Google Scholar]
- 6.Savarino V, Mela GS, Zentilin P, Bisso G, Pivari M, Mansi C, Mele MR, Bilardi C, Vigneri S, Celle G. Comparison of isotope ratio mass spectrometry and nondispersive isotope-selective infrared spectroscopy for 13C-urea breath test. Am J Gastroenterol. 1999;94:1203–1208. doi: 10.1111/j.1572-0241.1999.01067.x. [DOI] [PubMed] [Google Scholar]
- 7.Mion F, Ecochard R, Guitton J, Ponchon T. (13)CO(2) breath tests: comparison of isotope ratio mass spectrometry and non-dispersive infrared spectrometry results. Gastroenterol Clin Biol. 2001;25:375–379. [PubMed] [Google Scholar]
- 8.Camilleri M. Clinical practice. Diabetic gastroparesis N Engl J Med. 2007;356:820–829. doi: 10.1056/NEJMcp062614. [DOI] [PubMed] [Google Scholar]
- 9.Ghoos YF, Maes BD, Geypens BJ, Mys G, Hiele MI, Rutgeerts PJ, Vantrappen G. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1993;104:1640–1647. doi: 10.1016/0016-5085(93)90640-x. [DOI] [PubMed] [Google Scholar]
- 10.Delbende B, Perri F, Couturier O, Leodolter A, Mauger P, Bridgi B, Bizais Y, des Varannes SB, Andriulli A, Galmiche JP. 13C-octanoic acid breath test for gastric emptying measurement. Eur J Gastroenterol Hepatol. 2000;12:85–91. doi: 10.1097/00042737-200012010-00016. [DOI] [PubMed] [Google Scholar]
- 11.Lee JS, Camilleri M, Zinsmeister AR, Burton DD, Choi MG, Nair KS, Verlinden M. Toward office-based measurement of gastric emptying in symptomatic diabetics using [13C]octanoic acid breath test. Am J Gastroenterol. 2000;95:2751–2761. doi: 10.1111/j.1572-0241.2000.03183.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee JS, Camilleri M, Zinsmeister AR, Burton DD, Kost LJ, Klein PD. A valid, accurate, office based non-radioactive test for gastric emptying of solids. Gut. 2000;46:768–773. doi: 10.1136/gut.46.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanaka M, Yamamoto T, Ishii T, Kuyama Y. The Wagner-Nelson method can generate an accurate gastric emptying flow curve from CO2 data obtained by a 13C-labeled substrate breath test. Digestion. 2004;69:71–78. doi: 10.1159/000077391. [DOI] [PubMed] [Google Scholar]
- 14.Bromer MQ, Kantor SB, Wagner DA, Knight LC, Maurer AH, Parkman HP. Simultaneous measurement of gastric emptying with a simple muffin meal using [13C]octanoate breath test and scintigraphy in normal subjects and patients with dyspeptic symptoms. Dig Dis Sci. 2002;47:1657–1663. doi: 10.1023/a:1015856211261. [DOI] [PubMed] [Google Scholar]
- 15.Viramontes BE, Kim DY, Camilleri M, Lee JS, Stephens D, Burton DD, Thomforde GM, Klein PD, Zinsmeister AR. Validation of a stable isotope gastric emptying test for normal, accelerated or delayed gastric emptying. Neurogastroenterol Motil. 2001;13:567–574. doi: 10.1046/j.1365-2982.2001.00288.x. [DOI] [PubMed] [Google Scholar]
- 16.Choi MG, Camilleri M, Burton DD, Zinsmeister AR, Forstrom LA, Nair KS. [13C]octanoic acid breath test for gastric emptying of solids: accuracy, reproducibility, and comparison with scintigraphy. Gastroenterology. 1997;112:1155–1162. doi: 10.1016/s0016-5085(97)70126-4. [DOI] [PubMed] [Google Scholar]
- 17.Sanaka M, Nakada K, Nosaka C, Kuyama Y. The Wagner-Nelson method makes the [13C]-breath test comparable to radioscintigraphy in measuring gastric emptying of a solid/liquid mixed meal in humans. Clin Exp Pharmacol Physiol. 2007;34:641–4. doi: 10.1111/j.1440-1681.2007.04624.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim DY, Camilleri M, Schuster MM, Crowell MD, Koch KL. Schuster Atlas of gastrointestinal motility in health and disease. Vol. 2. Hamilton, Londo: BC Decker Inc; 2002. Stable isotope breath test and gastric emptying; pp. 203–218. [Google Scholar]
- 19.Odunsi ST, Camilleri M, Szarka LA, Zinsmeister AR. Optimizing analysis of stable isotope breath tests to estimate gastric emptying of solids. Neurogastroenterol Motil. 2009 doi: 10.1111/j.1365-2982.2009.01283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanaka M, Yamamoto T, Kuyama Y. The “Corrected” Half Emptying Time Is a Valueless Parameter in the 13C-Octanoic Acid Breath Test: Misuse of the Regression Analysis. J Clin Gastroenterol. 2003;36:284–285. doi: 10.1097/00004836-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Maes BD, Ghoos YF, Geypens BJ, Hiele MI, Rutgeerts PJ. Relation between gastric emptying rate and rate of intraluminal lipolysis. Gut. 1996;38:23–27. doi: 10.1136/gut.38.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiMagno EP, Go VL, Summerskill WH. Relations between pancreatic enzyme ouputs and malabsorption in severe pancreatic insufficiency. N Engl J Med. 1973;288:813–815. doi: 10.1056/NEJM197304192881603. [DOI] [PubMed] [Google Scholar]
- 23.Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut. 2005;54 6:vi1–28. doi: 10.1136/gut.2005.065946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van de CM, Luypaerts A, Geypens B, Fevery J, Ghoos Y, Nevens F. Oxidative breakdown of octanoic acid is maintained in patients with cirrhosis despite advanced disease. Neurogastroenterol Motil. 2003;15:113–120. doi: 10.1046/j.1365-2982.2003.00397.x. [DOI] [PubMed] [Google Scholar]
- 25.Schneider AR, Kraut C, Lindenthal B, Braden B, Caspary WF, Stein J. Total body metabolism of 13C-octanoic acid is preserved in patients with non-alcoholic steatohepatitis, but differs between women and men. Eur J Gastroenterol Hepatol. 2005;17:1181–1184. doi: 10.1097/00042737-200511000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Annese V, Bassotti G, Napolitano G, Frusciante V, Bruno M, Conoscitore P, Germani U, Morelli A, Andriulli A. Gastric emptying of solids in patients with nonobstructive Crohn's disease is sometimes delayed. J Clin Gastroenterol. 1995;21:279–282. doi: 10.1097/00004836-199512000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Grill BB, Lange R, Markowitz R, Hillemeier AC, McCallum RW, Gryboski JD. Delayed gastric emptying in children with Crohn's disease. J Clin Gastroenterol. 1985;7:216–226. doi: 10.1097/00004836-198506000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Keller J, Szai S, Begliner C, Holst JJ, Fibbe C, Layer P. Disturbed gastric emptying in CrohnÔs disease: mediated by gastrointestinal hormones? Gastroenterology. 2003;124:A–676. [Google Scholar]
- 29.Keller J, Begliner C, Holst JJ, Szai S, Fibbe C, Muench M, Layer P. Gastric emptying of solids in ulcerative colitis and release of regulatory hormones. Regul Pept. 2004;12:25. [Google Scholar]
- 30.Keller J, Fliegner-Baia M, Layer P. Physical activity alters normal values of the “European standard” 13C-octanoic acid breath test. Gut. 2002;51:A136. [Google Scholar]
- 31.Westerterp KR, Plasqui G. Physical activity and human energy expenditure. Curr Opin Clin Nutr Metab Care. 2004;7:607–613. doi: 10.1097/00075197-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Keim NL, Blanton CA, Kretsch MJ. America's obesity epidemic: measuring physical activity to promote an active lifestyle. J Am Diet Assoc. 2004;104:1398–1409. doi: 10.1016/j.jada.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 33.Peracchi M, Gebbia C, Ogliari C, Fraquelli M, Vigano R, Baldassarri A, Bianchi PA, Conte D. Influence of caloric intake on gastric emptying of solids assessed by 13C-octanoic acid breath test. Scand J Gastroenterol. 2000;35:814–818. doi: 10.1080/003655200750023174. [DOI] [PubMed] [Google Scholar]
- 34.Tougas G, Eaker EY, Abell TL, Abrahamsson H, Boivin M, Chen J, Hocking MP, Quigley EM, Koch KL, Tokayer AZ, Stanghellini V, Chen Y, Huizinga JD, Ryden J, Bourgouis I, McCallum RW. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462. doi: 10.1111/j.1572-0241.2000.02076.x. [DOI] [PubMed] [Google Scholar]
- 35.Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP, Shreve P, Szarka LA, Snape WJ, Jr, Ziessman HA. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. J Nucl Med Technol. 2008;36:44–54. doi: 10.2967/jnmt.107.048116. [DOI] [PubMed] [Google Scholar]


