Abstract
Objective
To investigate racial/ethnic differences in disability onset among older Americans with arthritis. We examined factors amenable to clinical and public health intervention that may explain racial/ethnic differences in incident disability.
Methods
Longitudinal data (1998−2004) from a national representative sample of 5818 non-Hispanic Whites, 1001 African Americans, 228 Hispanics interviewed in Spanish (Hispanic/Spanish), and 210 Hispanics interviewed in English (Hispanic/English), ages 51 or older with arthritis who did not have baseline disability were analyzed. Disability in activities of daily living (ADL) was identified from report of inability, avoidance, or needing assistance to perform one or more ADL tasks.
Results
Over six years, 28.0% African Americans, 28.5% Hispanic/Spanish, 19.1% Hispanic/English, and 16.2% Whites developed disability. The demographic-adjusted disability hazard ratio (AHR) were significantly greater among African Americans (AHR=1.94, 95% CI: 1.51−2.38) and Hispanic/Spanish (AHR=2.03, 95% CI: 1.35−2.71), but not significantly increased for Hispanic/English (AHR=1.41, 95% CI: 0.82−2.00) compared to Whites. Differences in health factors (comorbid conditions, functional limitations, and behaviors) explained over half the excess risk among African Americans and Hispanic/Spanish. Medical access factors (education, income, wealth, and health insurance) were substantial mediators of racial/ethnic differences in all minority groups.
Conclusion
Racial/ethnic differences in the development of disability among older adults with arthritis were largely attenuated by health and medical access factors. Lack of health insurance was particularly problematic. At the clinical level, treatment of comorbid conditions, functional limitations, and promotion of physical activity and weight maintenance should be a priority to prevent the development of disability, especially in minority populations.
Arthritis and other rheumatic conditions (arthritis, hereafter) are common chronic conditions among elderly Americans. They are the leading cause of disability, limiting daily activities for more than 7 million Americans (1). As the U.S. population ages, the impact of arthritis is expected to increase. Data from the National Health Interview Survey (NHIS) showed that the prevalence of arthritis increased from nearly one in every six people in 1990 to one in every five people in 2002 (2, 3). Although evidence showed decreasing disability trends in the general population (4-6), disability was increasing among persons with arthritis. Arthritis-related activity limitations rates almost tripled from 2.8% in 1990 to 7.8% in 2002 based on age-adjusted rates from NHIS data (2, 3).
The racial/ethnic composition of the U.S. population is also changing. Minority (non-White) populations will increase from 30.6% of the U.S. population in 2000 to 49.9% by the year 2050. The fastest increase is among persons of Hispanic origin; this segment is projected to increase from 12.6% of the U.S. population in 2000 to 24.4% by 2050 (7). Among persons with arthritis, African Americans and Hispanic minority groups had substantially higher rates of disability than their White counterparts (3, 8-12).
In order to advance public health efforts to promote equitable health outcomes, it is crucial to identify modifiable factors that contribute to racial/ethnic differences among persons with arthritis. This study addressed this question by examining racial/ethnic differences in the development of disability in activities of daily living (ADL) among older adults with arthritis. Longitudinal data from the 1998−2004 Health and Retirement Study (HRS), a national representative sample of community living adults were used to answer the following research questions:
For older adults with arthritis who were free of disability at baseline (1998), what are the national rates at which racial/ethnic groups develop ADL disability?
How much of the observed racial/ethnic differences in the development of disability can be explained by demographic, health, and medical access factors?
What are the significant risk factors that predict the development of ADL disability among older adults with arthritis?
MATERIALS AND METHODS
Data and study sample
This study used data from HRS, which is sponsored by the National Institute of Aging and conducted by the University of Michigan. The HRS cohort is based on a national representative sample of non-institutionalized older Americans. The ongoing HRS collects biennial in-depth information on medical access, finance, health and sociodemographics.(13).
We used the public release 1998, 2000, 2002, and 2004 HRS data. The baseline arthritis cohort included 9,943 respondents aged 51 or over who self-identified as Hispanic/Latino, African American/black and/or White/Caucasian. To draw inferences about incidence of ADL disability, we restricted our analyses to 7,257 respondents without baseline ADL disability and who were alive at the subsequent 2000 interview. Excluded by design were 1,340 persons with baseline ADL disability, 375 decedents prior to 2000, 480 baseline proxy interviews, 411 non-respondents by 2000 interview. For analytical purposes, another 80 persons with missing data in either HRS 2000 ADL disability status or baseline explanatory variables were excluded.
Arthritis
Baseline arthritis was determined by an affirmative answer to the 1998 HRS question, “Have you ever had or has a doctor ever told you that you have arthritis or rheumatism?” Self-reported arthritis is relevant from a public policy perspective because many persons with arthritis do not see a health care provider for their symptoms (14).
Disability
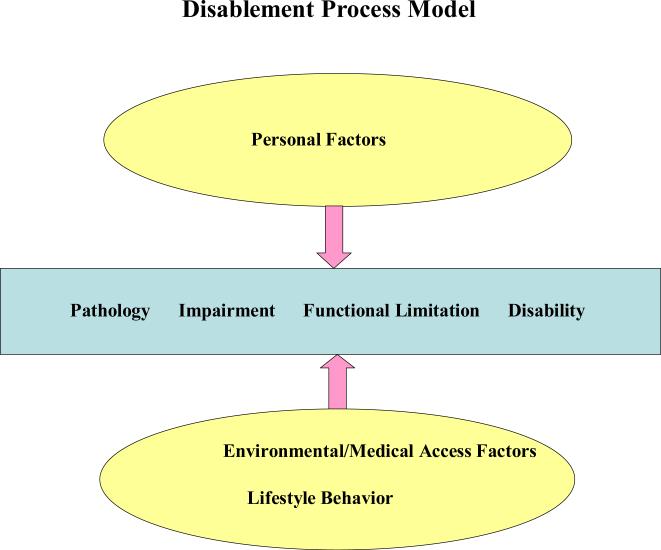
We defined disability as a gap between a person's capabilities and environmental demands, e.g., limitations in ADLs (15). Figure 1 shows Verbrugge and Jette's conceptual model depicting factors that influence the ongoing process of disablement including personal, lifestyle/behavioral (e.g., health behaviors) and physical/social environmental (e.g., medical access) factors.
Figure 1.
Disablement Process Model
The HRS monitors six basic ADL tasks essential for independent living: dressing, walking across a room, transferring in/out of bed, bathing, eating and toileting. Disability in an ADL task expected to last for at least three months was ascertained from self-reported inability, avoidance, or needing assistance from a person or using an assistive device in carrying out such task. This assessment of ADL disability captures chronic dependence in self-care activities that could jeopardize a person's ability to live independently. For the purpose of analysis, the development of ADL disability was identified by the first report of disability in one or more ADL tasks at a subsequent 2000, 2002, or 2004 interview.
Covariates
Baseline (1998) demographic factors consist of race/ethnicity, age, gender, marital status, and living arrangement (live alone or with others). We used HRS race/ethnicity information to classify people into four mutually exclusive groups: English-speaking Hispanic, Spanish-speaking Hispanic, (non-Hispanic) African American, and (non-Hispanic) White. We distinguished English-speaking Hispanic from Spanish-speaking Hispanic adults because prior literature (16) suggested that persons from different linguistic groups might have different views of health and disease or disability. People from other racial/ethnic groups are excluded from analyses due to small subgroups (n=109). Marital status and living situation were assessed at all biennial interviews (1998, 2000, 2002, or 2004).
Health factors assessed at each interview included comorbid chronic conditions, functional limitations, and health behaviors. In addition to arthritis, chronic conditions were ascertained by self-report of physician diagnosis of conditions including cancer, diabetes, heart disease, hypertension, pulmonary disease, or stroke. The presence of depressive symptoms was determined by an abbreviated Center for Epidemiological Studies Depression (CES-D) assessment (17). Persons with high depressive symptoms were identified with a cut point of five or more on the 8 CESD items, which accounted for the upper ten percentile of persons with CESD information. Bad vision was defined as poor or legally blind eyesight.
Functional limitations assessed at each interview included physical and instrumental activities of daily living (IADL) task limitations. Physical limitations were assessed from self-reported inability or avoidance of any of the four tasks of walking several blocks, climbing several stairs without rest, pulling or pushing large objects, and lifting or carrying weights over 10 pounds. IADL limitations were ascertained from reports of receiving help, cannot do, or don't do because of physical, mental, emotional, or memory problems in any of five social tasks including preparing hot meals, grocery shopping, using the telephone, taking medication, or managing money.
Health behaviors assessed at each interview consisted of current smoking, current alcohol consumption, weight status, and regular vigorous physical activity. Current smoking was ascertained from a positive response to “Do you smoke cigarettes now?” Alcohol consumption was based on a positive response to the question, “Do you ever drink any alcoholic beverages such as beer, wine, or liquor?” Weight status was determined from weight gain or loss of 10 pounds or more, obesity, and underweight. Body mass index (BMI, [weight (kg)]/[height (m)]2), calculated from self-reported height and weight, was used to define obesity (BMI ≥30) and underweight (BMI <20). Regular vigorous physical activity was ascertained from the report of participation at least three times a week over the past 12 months in activities such as sports, heavy housework, or a job that involves physical labor.
Medical access factors assessed at each interview consisted of education, wealth, family income, and health insurance. Education, a measure of human capital, was dichotomized as 12 or more versus fewer completed years of education. For analytic purposes, family income (all sources received by the respondent and spouse/partner during the preceding year) and wealth (the sum of housing and non-housing assets) were dichotomized using the lowest baseline HRS population-weighted quartiles (18). If only partial income or wealth information was provided during the interview, dichotomized values were based on imputed estimates developed by the University of Michigan. Health insurance was classified into four mutually exclusive groups: any private insurance coverage, Medicaid enrollment, Medicare or other government insurance programs such as CHAMPUS, CHAMPVA, and the Veteran's Administration without additional Medicaid or private insurance coverage, and no coverage.
Statistical analysis
The HRS is a national probability sample. All analyses used person-weights, stratum, and sampling codes for the 1998 HRS data developed at the University Michigan to provide valid inferences of the U.S. population. Analyses were restricted to 1998 HRS self-respondents. Non-respondents (including proxy interviews) compared to respondents tended to disproportionately be African American or Hispanic adults. We adjusted for potential bias due to missing interview information and/or non-response by handling respondents with completed data as another stage of sampling to obtain adjusted sampling weights, using standard sampling methodology (19). Statistical testing was conducted at a nominal five percent alpha significance level.
Bivariate analyses were employed to examine whether there are differences in the baseline demographic, health and medical access factors between minority groups and Whites using chi-square tests. We calculated unadjusted six-year cumulative risks of incident disability by race and ethnicity. All analyses adjust for the complex sampling design (20) using SUDAAN software version 9.0.
Survival analysis for discrete data was used to analyze racial/ethnic differences in the development of ADL disability. The development of ADL disability was measured in discrete rather than continuous time because ADL disability is monitored only at 2-year intervals (1998−2000, 2000−2002, and 2002−2004). A discrete hazard rate modeled the probability of developing disability by the next 2-year interview given a disability-free status and risk profile at the current interview. To investigate whether demographic, health, and medical access factors explain the racial/ethnic differences in development of disability, we employed a series of hierarchical survival models to estimate race/ethnicity related discrete hazard rate of disability by first controlling for demographic factors, and then sequentially adding to the model health and medical access factors. To be included in the analyses, a person's disability status must be known at the start and the end of a 2-year period. All completed interview pairs (1998/2000, 2000/2002, and 2002/2004) from a person prior to death contributed to the analyses. This method specifically accounts for repeated measures on the same individual and uses time-varying covariates. We used the SAS GENMOD procedure with a complementary log-log link to estimate the discrete hazard model. To account for the complex sampling design, variance was estimated using balanced repeated replication (BRR), a form of bootstrapping (19, 21). Hazard ratios and associated 95% confidence intervals (CI) estimated from the discrete hazard model were reported.
RESULTS
Our sample of 7,257 respondents represented 24.6 million older Americans with self-reported arthritis free of baseline disability, comprising 85.5% Whites, 9.3% African Americans, 2.4% Hispanics/Spanish, and 2.9% Hispanics/English. This population was predominantly female (61.5%) with an average baseline age of 66.7. By 2004, six years post baseline interview, 908 (12.5%) persons from the 7,257 study cohort had deceased. The mortality rate was the highest among African Americans (13.8%), followed by Whites (12.4%), Hispanic/English (11.4%), and Hispanic/Spanish (9.7%). The non-response rates among the survivors were 4.2% and 5.7% for the 2002, and 2004 interviews.
Information on the baseline characteristics, stratified by the four racial/ethnic groups, were presented in Table 1. Compared to Whites, African Americans were more likely to be unmarried and live alone, while Hispanic/Spanish were more likely to live with someone else. Hispanic/English were disproportionately younger than the other three subgroups and tended to be unmarried. Complex patterns of racial/ethnic differences in health factors emerged from Table 1. For comorbid chronic conditions, all three minority groups, especially Hispanic/Spanish and African Americans, compared to Whites, were generally less likely to report life threatening conditions (cancer, heart disease, and stroke) as well as pulmonary disease, but more likely to report other chronic conditions (diabetes, high depressive symptoms, hypertension, and poor vision). For functional limitations, physical limitation was 50% greater among African Americans and 75% greater among Hispanic/Spanish, and IADL limitation was 100% greater among African Americans and Hispanic/Spanish than their White counterparts. The prevalence of functional limitations among Hispanic/English was similar to Whites. Health behaviors, which include current smoking, alcohol-abstinence, less participation in regular vigorous physical activities, and weight problems such as obesity and weight loss were more often reported by African Americans. Hispanic/Spanish compared to Whites were more likely to be alcohol-abstinent. Hispanic/English acted more like Whites in terms of health behavior.
Table 1.
Frequency of Baseline (1998) Characteristics among 7257 Participants with Arthritis at Risk of Incident ADL Disability in the Health and Retirement Study
| Baseline (1998) Characteristics | African American N=1001 |
Hispanic/Spanish N=228 |
Hispanic/English N=210 |
White N=5818 |
|---|---|---|---|---|
| |
Population % |
Population % |
Population % |
Population % |
| Demographics | ||||
| Female | 66.35* | 67.16* | 62.80 | 60.74 |
| Age 51−60 | 34.24†** | 31.92†** | 46.23† | 31.18 |
| 61−70 | 35.60 | 38.48 | 32.64 | 32.14 |
| 71−80 | 20.60 | 23.21 | 15.50 | 26.91 |
| 81up | 9.56 | 6.39 | 5.63 | 9.76 |
| Unmarried | 60.96** | 38.83 | 46.51* | 34.93 |
| Live Alone | 32.63** | 15.09** | 25.00 | 25.48 |
| Health Factors | ||||
| Chronic Conditions: None | 20.68** | 24.33* | 25.52* | 31.64 |
| Cancer | 8.98* | 5.44* | 9.01 | 11.48 |
| Diabetes | 20.98** | 26.64* | 19.52* | 11.49 |
| Heart Disease | 19.60 | 9.64** | 17.11 | 20.67 |
| High Depressive Symptoms | 17.39** | 34.10** | 17.06* | 9.06 |
| Hypertension | 63.94** | 56.03* | 43.10 | 44.53 |
| Pulmonary Disease | 6.18** | 6.37 | 2.78** | 9.09 |
| Stroke | 6.08 | 0.54** | 3.59 | 4.26 |
| Vision (Poor /legally blind) | 10.01** | 8.35* | 6.65 | 4.58 |
| Functional Limitation: | ||||
| Physical function | 33.92** | 39.59* | 26.20 | 22.43 |
| IADL disability | 14.40** | 15.51 | 9.23 | 6.81 |
| Health Behaviors: | ||||
| Current Smoker | 19.90* | 13.97 | 17.70 | 16.08 |
| Current Alcohol Use | 16.39** | 15.34** | 30.62 | 32.20 |
| Lack of Regular Vigorous Physical Activity | 64.98** | 72.03* | 58.57 | 55.33 |
| Weight: Obese | 36.13** | 26.24 | 27.04 | 24.97 |
| Underweight | 2.58** | 6.10 | 3.13 | 4.67 |
| Gain > 10 lbs | 19.77 | 17.83 | 16.66 | 15.31 |
| Loss < 10 lbs | 20.03* | 15.66 | 16.43 | 15.53 |
| Medical Access Factors | ||||
| Low Education (<= 11 years) | 53.53** | 85.60** | 50.17** | 24.36 |
| Low Income | 54.63** | 71.90** | 41.38** | 22.59 |
| Low Net Wealth | 58.53** | 71.32** | 50.76** | 20.59 |
| Health Insurance | ||||
| Private | 40.60†** | 19.71†** | 43.35†* | 58.14 |
| Medicaid | 18.68 | 35.19 | 14.17 | 3.94 |
| Medicare/CHAMPS/CHAMPVA/VA | 31.84 | 24.48 | 28.52 | 34.35 |
| None | 8.88 | 20.63 | 13.96 | 3.57 |
Statistical test of minority group compared to White reference group from Chi-square test
indicates Chi-square result over multiple risk factor categories
unadjusted p-value < .05 (*) and < .01 (**).
Table 1 also shows substantial racial/ethnic differences in baseline medical access factors. All minority groups compared to Whites had fewer medical access resources in terms of low education, low income, and low wealth. Minorities were more likely to be uninsured or have Medicaid enrollment, while about 60% of Whites reported private insurance coverage. The most economically disadvantaged group was the Hispanic/Spanish. More than 85% of Hispanic/Spanish had less than a high school education and only 19.7% of this minority group had private insurance coverage.
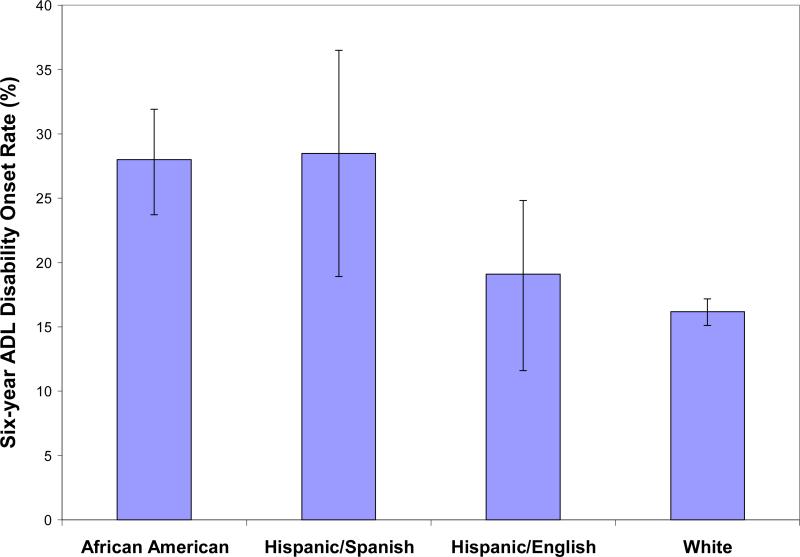
After six years, 17.7% of this arthritis cohort developed ADL disability. The six-year cumulative ADL disability incidence rates were significantly higher among African Americans (28.0%) and Hispanic/Spanish (28.5%) compared to Whites (16.2%), while Hispanic/English (19.1%) reported a similar disability rate as Whites (Figure 2).
Figure 2.
Six-year Cumulative Rates of Onset Disability among Older Americans with Arthritis from Health and Retirement Study Participants Aged 51+
Table 2 shows for the three minority groups relative to Whites the adjusted hazard ratios (HR) for developing ADL disability over the six-year period controlling for demographic differences. The demographic adjusted disability hazard rates were significantly greater among African Americans (adjusted HR=1.94, 95% CI = 1.51, 2.38) and Hispanic/Spanish (adjusted HR =2.03, 95% CI= 1.35, 2.71), and moderately but not significantly elevated for Hispanic/English (adjusted HR =1.41, 95% CI = 0.82, 2.00) compared to Whites with arthritis.
Table 2.
Hazard Ratios (HR) of Developing ADL Disability (HRS 1998−2004) *
|
Adjustment Factors† |
African American N=1001 Adjusted HR (95% CI) |
Hispanic/Spanish N=228 Adjusted HR (95% CI) |
Hispanic/English N=210 Adjusted HR (95% CI) |
White N=5818 (Reference) |
|---|---|---|---|---|
| Demographic Factors | 1.94 (1.51, 2.38) | 2.03 (1.35, 2.71) | 1.41 (0.82, 2.00) | 1.00 |
| Demographics+Chronic Diseases | 1.68 (1.27, 2.08) | 1.72 (1.10, 2.33) | 1.38 (0.77, 1.98) | 1.00 |
| Demographics+Functional Limitations | 1.68 (1.31, 2.05) | 1.67 (1.20, 2.14) | 1.39 (0.92, 1.86) | 1.00 |
| Demographics+Health Behaviors | 1.63 (1.29, 1.97) | 1.69 (1.12, 2.27) | 1.41 (0.82, 2.00) | 1.00 |
| Demographic+ ALL Health Factors | 1.42 (1.10, 1.74) | 1.41 (1.00, 1.82) | 1.42 (0.91, 1.93) | 1.00 |
| Demographic+Health+Medical Access Factors | 1.31 (1.01, 1.61) | 1.20 (0.82, 1.58) | 1.32 (0.88, 1.76) | 1.00 |
Adjustment factors include: Demographic Factors (race/ethnicity, age, gender, marital status, living arrangement), Health Factors (Chronic Diseases: cancer, diabetes, heart disease, high depressive symptoms, hypertension, pulmonary disease, stroke, vision problem; Functional Limitations: physical limitations, IADL limitations; Health Behaviors: smoke, alcohol use, exercise, weight problems), and Medical Access Factors (education, income, wealth, health insurance).
Bolded value indicates associated Race/Ethnicity incident disability hazard rate compared to White reference group is significant at a 0.05 alpha level of testing.
Separately adjusting for health factor differences related to chronic conditions, functional limitations, or health behaviors, each explained 28−35% of the excess hazard for African Americans and Hispanic/Spanish, but had little influence on Hispanic/English disability differences. Taken together, health factors reduced the excess hazard among African Americans 55% (to 1.42), among Hispanic/Spanish 60% (to 1.41), but the adjusted hazard ratio of Hispanic/English was almost unchanged. It was notable that after adjusting for demographic and health factors, the excess risk was similar across all three minority groups (1.41−1.42) compared to Whites.
Finally, Table 2 analyses that additionally control for medical access factors further reduced the excess risk among African Americans by an additional 12% (to 1.31), among Hispanic/Spanish an additional 20% (to 1.20), and among Hispanic English an additional 24% (to 1.32) even after accounting for differences due to health and demographic factors. Recognizing that the impact of medical access factors may overlap with that of health factors, sensitivity analyses that control for medical access factors and demographics (without the influence of health factors) were conducted. Medical access factors alone explained 60% of excess risk for African Americans, 95% for Hispanic/Spanish and 73% for Hispanic/English. This finding reflects the influence of substantial economic disparities among minorities compared to Whites indicated by Table 1. However, economic disparities and types of insurance held also are likely to partially reflect the health of individuals.
We have also conducted sensitivity analyses to include an additional 1569 people who developed arthritis after baseline interview. The results were essentially identical to those presented in Table 2.
Table 3 presents the results from the full discrete hazard model, showing the relative impact of demographics, health and medical access factors on the development of ADL disability. Besides race/ethnicity, age was the only significant predictor of ADL disability among demographic factors. The risk of disability increased dramatically for people with older age (age 71−80: adjusted hazard ratio [AHR] =1.38; age 81 or over: AHR=3.27). Among the health factors, the strongest risk factor was IADL disability (AHR=2.74), followed by lack of regular vigorous physical activities (AHR=1.87), and weight loss (AHR=1.84). Other health factors that significantly increased the risk of ADL disability include stroke (AHR=1.68), obesity (AHR=1.52), weight gain (AHR=1.50), diabetes (AHR=1.47), pulmonary disease (AHR=1.33), limitation in physical function (AHR=1.32), high depressive symptoms (AHR=1.29), current smoker (AHR=1.26), and hypertension (AHR=1.17). Alcohol consumption was associated with lower likelihood for developing ADL disability (AHR=0.64). Medical access factors were not significant predictors of developing disability after controlling for other risk factors except for holding public health insurance. Both Medicaid enrollment (AHR=1.65) and Medicare or other public health insurance (AHR=1.41) were associated with greater risk of ADL disability relative to holding private insurance coverage, after adjusting for demographic and health factors. At least part of this large, positive effect of the Medicaid variable may reflect the fact that low income people in poor health are more likely to be put on Medicaid in order to cover otherwise uninsured medical expenses. We also noted that if we removed the insurance variables, the low income variable would become statistically significant (AHR =1.22, CI=1.02, 1.43).
Table 3.
Adjusted Hazard Ratio (HR) for Developing ADL Disability (HRS 1998−2004)*
| |
Adjusted HR |
95% CI |
|---|---|---|
| Second interval (2000−2002) | 0.82 | 0.70, 0.94 |
| Third interval (2002−2004) | 0.84 | 0.68, 0.99 |
| Demographic | ||
| African American | 1.31 | 1.01, 1.61 |
| Hispanic/Spanish | 1.20 | 0.82, 1.58 |
| Hispanic/English | 1.32 | 0.88, 1.76 |
| Female | 1.06 | 0.90, 1.22 |
| Age 61−70 | 0.80 | 0.61, 0.99 |
| Age 71−80 | 1.38 | 1.07, 1.70 |
| Age 81 or older | 3.27 | 2.49, 4.06 |
| Unmarried | 0.85 | 0.63, 1.08 |
| Live alone | 1.04 | 0.86, 1.22 |
| Health Factors | ||
| Chronic Condition | ||
| Cancer | 1.03 | 0.86, 1.19 |
| Diabetes | 1.47 | 1.20, 1.75 |
| Heart Disease | 1.06 | 0.87, 1.24 |
| High Depressive Symptoms | 1.29 | 1.02, 1.57 |
| Hypertension | 1.17 | 1.00, 1.35 |
| Pulmonary Disease | 1.33 | 1.08, 1.58 |
| Stroke | 1.68 | 1.28, 2.07 |
| Vision (Poor /legally blind) | 1.11 | 0.89, 1.34 |
| Functional Limitation: | ||
| Physical function | 1.32 | 1.15, 1.49 |
| IADL disability | 2.74 | 2.30, 3.17 |
| Health Behaviors | ||
| Current Smoker | 1.26 | 1.00, 1.53 |
| Current Alcohol Use | 0.64 | 0.50, 0.78 |
| Lack vigorous physical activities | 1.87 | 1.50, 2.24 |
| Weight: Obese | 1.52 | 1.30, 1.74 |
| Underweight | 1.33 | 0.95, 1.71 |
| Gain > 10 lbs | 1.50 | 1.25, 1.75 |
| Loss >10 lbs | 1.84 | 1.58, 2.10 |
| Medical Access Factors | ||
| Low Education (<=11 years) | 0.92 | 0.78, 1.06 |
| Low income | 1.12 | 0.91, 1.33 |
| Low net wealth | 1.06 | 0.89, 1.24 |
| Health Insurance | ||
| Medicaid | 1.65 | 1.18, 2.11 |
| 1.41 | 1.11, 1.71 | |
| Medicare/CHAMPS/CHAMPVA/VA | ||
| None | 0.82 | 0.50, 1.14 |
Bolded value indicates associated adjusted hazard is significantly different from unity at 0.05 alpha-level.
DISCUSSION
This study provided evidence of racial/ethnic differences in the development of ADL disability among older Americans with arthritis who had no ADL disability at baseline. Overall, one out of six persons of this arthritis cohort reported disability in at least one ADL task over the six-year follow-up period. However, there were substantial and complex differences across race and ethnicity. The incident rates of ADL disability among African Americans (28.0%) and Hispanic/Spanish (28.5%) were more than 1.7 times that of Whites (16.2%). But Hispanic/English reported a rate (19.1%) similar to Whites.
Racial and ethnic differences in the prevalence of disability for persons with arthritis have long been a concern.(8-11, 22) However, national data on racial/ethnic differences in the development of disability among persons with arthritis are sparse. One study based on national data from Shih and colleagues(12) showed higher rates in the development of disability among African Americans and Hispanics compared to Whites based on the 1998−2000 Health and Retirement Study and noted that factors contributing to disability differ across racial ethnic groups.
The present study added to the arthritis literature by exploring the contribution of health and medical access factors to racial/ethnic differences in the development of disability. In addition, we considered acculturation, which can influence health status(23, 24). The present study used language of preferred interview as a proxy for acculturation. Participants who choose to respond in their native language (rather than the language of the host country) usually have lower levels of acculturation. Language barriers may limit opportunities for integration with the host culture and reduce social acceptance resulting from being identified as Hispanic. While many cultural features are not captured by this attribute, it differentiates two distinct populations that may have different experiences which influence disability. For example, disadvantages stemming from limited educational and occupational choices, and social stress related to poverty may contribute to the greater disability burden experienced by the Hispanic/Spanish group compared to Hispanic/English.
To guide a public health response to promote equitable health outcomes, we investigated the relative influence of health and medical access factors on racial/ethnic differences in the development of disability. Disability developed most frequently among African Americans and Hispanic/Spanish, whose risk was almost doubled compared to Whites after controlling for demographic differences. Differences in health factors related to chronic comorbid conditions, functional limitations, and health behaviors explained over half that excess risk for developing disability among African Americans and Hispanic/Spanish. In contrast, Hispanic/English had an insignificant, but slightly elevated risk for developing disability than Whites; little of that excess was attenuated by differences in health factors. The limited influence of health factors on elevated Hispanic/English disability rates as compared to Whites reflected the strongly similar profiles on functional limitations and health behaviors, and few differences in chronic conditions for Hispanic/English versus Whites (Table 1). Hispanic/Spanish had poorer health profiles than Hispanic/English. Once individual health factors were controlled for in the analyses, the higher disability incidence for Spanish-speaking versus English-speaking Hispanics was eliminated.
Medical access factors were substantial mediators of racial/ethnic differences in the development of disability. African American, Hispanic/Spanish, and Hispanic/English minorities compared to Whites had disproportionately fewer economic resources in terms of education, income, and wealth. Minorities were also more likely to be uninsured or rely on Medicaid coverage. Hispanic/Spanish adults were the most economically disadvantaged in every category. Even after controlling for health factors, medical access factors explained an additional 12% excess risk among African Americans and 20% among Hispanic/Spanish. Similarly, medical access factors had an attenuating effect on the Hispanic/ English disability risk compared to Whites.
There is a large body of literature that showed that lower income is directly related to poorer health outcomes.(25, 26) However, it was not just poverty but the social gradient i.e. place in society that affected health outcomes. (26) It was found that non-English-speaking immigrants experience tremendous discrimination not only in schools and the work-place but also in health-care settings and in society in general (27-30). Lack of private insurance may indicate poorer quality of health care received. Individuals in lower tier health plans commonly have fewer choices with regard to health services which can compromise their quality of care. For example, fewer joint replacements are done for racial/ethnic minorities than for Whites (31), although whether or not this is due to medical access or discrimination or other factors is unclear. The measured economic disparities in this study may additionally reflect unmeasured differences in social gradient, which explained the large excess risk of disability related to medical access factors for minorities in general and Hispanic/Spanish adults in particular.
Several limitations common to secondary databases may affect our findings. First, data were self-reported. However, self-reported information was standard in epidemiologic research and its reliability had been documented (32, 33). Second, no information on disease severity was available. However, we used limitations in physical functioning and IADL tasks, likely consequences of disease, as surrogates for disease severity measures. Including functional limitations also adjusted for where individuals started on the disability spectrum. Third, although this study demonstrated that racial/ethnic differences in disability were largely due to health and medical access factors, these findings could be confounded by unmeasured environmental factors contributing to disability. Such factors may include occupation, job demands, poorer living conditions, and segregation. Additionally, Hispanic/Spanish and Hispanic/English language differences may reflect distinct paradigms concerning health and illness. (34, 35) Finally, dividing Hispanics into two groups based on interview language was a gross distinction of cultural differences. It is also likely that there are important cultural differences aggregated into African American and White subgroups. Therefore analyses adjusted for common correlates of race/ethnicity (e.g., education, income, wealth).
In summary, these national data from the Health and Retirement Study indicated that among older adults with arthritis, excess racial/ethnic rates for developing ADL disabilities were largely explained by differences in health and medical access factors. Differences in economic resources between groups were great. Lack of health insurance was especially problematic given limited income and wealth available to minority populations to enable medical access. Differences in health factors were especially great for African Americans and Spanish speaking Hispanics and exacerbated excess disability for those groups when compared to Whites. At the clinical level, not only should treatment of comorbid conditions be considered, but also disease prevention, prevention and treatment of functional limitations, and promotion of healthy behaviors should be a priority for all patients with arthritis to prevent the development of disability. Future research should be directed at how to more effectively deliver such programs especially to minority populations. Policy recommendations that provide incentives to address these factors should be considered.
Acknowledgments
This study is supported in part by funding from NIH/National Institute for Arthritis and Musculoskeletal Diseases P60-AR48098, and NIH/ National Center for Medical Rehabilitation Research R01-HD45412.
REFERENCE
- 1.Centers for Disease Control and Prevention Prevalence of disabilities and associated health conditions among adults--United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(7):120–5. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Arthritis prevalence and activity limitations--United States, 1990. MMWR Morb Mortal Wkly Rep. 1994;43(24):433–8. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis--United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54(5):119–23. [PubMed] [Google Scholar]
- 4.Manton KG, Gu X. Changes in the prevalence of chronic disability in the United States black and nonblack population above age 65 from 1982 to 1999. Proc Natl Acad Sci U S A. 2001;98(11):6354–9. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cutler DM. Declining disability among the elderly. Health Aff (Millwood) 2001;20(6):11–27. doi: 10.1377/hlthaff.20.6.11. [DOI] [PubMed] [Google Scholar]
- 6.Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982−2002. Am J Public Health. 2005;95(11):2065–70. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Census Bureau U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin. Available at http://www.census.gov/ipc/www/usinterimproj/
- 8.Kington RS, Smith JP. Socioeconomic status and racial and ethnic differences in functional status associated with chronic diseases. Am J Public Health. 1997;87(5):805–10. doi: 10.2105/ajph.87.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verbrugge LM, Lepkowski JM, Konkol LL. Levels of disability among U.S. adults with arthritis. J Gerontol. 1991;46(2):S71–83. doi: 10.1093/geronj/46.2.s71. [DOI] [PubMed] [Google Scholar]
- 10.Dunlop DD, Manheim LM, Song J, Chang RW. Arthritis prevalence and activity limitations in older adults. Arthritis Rheum. 2001;44(1):212–21. doi: 10.1002/1529-0131(200101)44:1<212::AID-ANR28>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 11.Abraido-Lanza AF, White K, Armbrister AN, Link BG. Health status, activity limitations, and disability in work and housework among Latinos and non-Latinos with arthritis: an analysis of national data. Arthritis Rheum. 2006;55(3):442–50. doi: 10.1002/art.21981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shih VC, Song J, Chang RW, Dunlop DD. Racial differences in activities of daily living limitation onset in older adults with arthritis: a national cohort study. Arch Phys Med Rehabil. 2005;86(8):1521–6. doi: 10.1016/j.apmr.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 13.Heeringa S. Technical description of the Asset and Health Dynamics Among the Oldest Old (AHEAD) Study Sample Design. Population Studies Center; Ann Arbor, MI: 1995. Report No.: HRS Documentation Report DR-003. [Google Scholar]
- 14.Centers for Disease Control and Prevention Adults who have never seen a health-care provider for chronic joint symptoms --- United States, 2001. MMWR Morb Mortal Wkly Rep. 2003;52:416–9. [PubMed] [Google Scholar]
- 15.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 16.Shewder AR, Much CN, Mahapatra M, Park L. Morality and Health. Routledge; New York: 1997. The “Big Three” of Morality (Autonomy, Community, Divinity) and the “Big Three” Explanations of Suffering. p. ix.p. 416. Morality and health. [Google Scholar]
- 17.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Journal of Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 18.Smith JP. Wealth inequality among older Americans. J Gerontol B Psychol Sci Soc Sci. 1997;52:74–81. doi: 10.1093/geronb/52b.special_issue.74. Spec No. [DOI] [PubMed] [Google Scholar]
- 19.Korn EL, Graubard BI. Analysis of Health Surveys. John Wiley and Sons, Inc; New York: 1999. [Google Scholar]
- 20.Research Triangle Institute . SUDAAN Language Manual, Release 9.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- 21.Korn EL, Graubard BI. Epidemiologic studies utilizing surveys: accounting for the sampling design. Am J Public Health. 1991;81(9):1166–73. doi: 10.2105/ajph.81.9.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verbrugge LM, Gates DM, Ike RW. Risk factors for disability among U.S. adults with arthritis. J Clin Epidemiol. 1991;44(2):167–82. doi: 10.1016/0895-4356(91)90264-a. [DOI] [PubMed] [Google Scholar]
- 23.Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979−2003. Int J Epidemiol. 2006;35(4):903–19. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- 24.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- 25.Kawachi Io, Kennedy BP, Wilkinson RG. The society and population health reader. Volume 1 : income inequality and health. New Press ; W.W. Norton [distributor]; New York: 1999. [Google Scholar]
- 26.Marmot MG. Understanding social inequalities in health. Perspect Biol Med. 2003;46(3 Suppl):S9–23. [PubMed] [Google Scholar]
- 27.Meier KJ, Stewart J. The politics of Hispanic education : un paso pa'lante y dos pa'tras. State University of New York Press; Albany: 1991. [Google Scholar]
- 28.Lowell BL, Teachman J, Jing Z. Unintended consequences of immigration reform: discrimination and Hispanic employment. Demography. 1995;32(4):617–28. [PubMed] [Google Scholar]
- 29.Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health. 2003;93(2):277–84. doi: 10.2105/ajph.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Turner MA, United States. Dept. of Housing and Urban Development. Office of Policy Development and Research . Discrimination in metropolitan housing markets national results from phase I HDS 2000. U.S. Dept. of Housing and Urban Development, Office of Policy Development and Research; Washington, D.C.: 2002. [Google Scholar]
- 31.Dunlop DD, Song J, Manheim LM, Chang RW. Racial disparities in joint replacement use among older adults. Med Care. 2003;41(2):288–98. doi: 10.1097/01.MLR.0000044908.25275.E1. [DOI] [PubMed] [Google Scholar]
- 32.Otiniano ME, Du XL, Ottenbacher K, Markides KS. The effect of diabetes combined with stroke on disability, self-rated health, and mortality in older Mexican Americans: results from the Hispanic EPESE. Arch Phys Med Rehabil. 2003;84(5):725–30. doi: 10.1016/s0003-9993(02)04941-9. [DOI] [PubMed] [Google Scholar]
- 33.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. Jama. 2001;286(10):1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 34.Shweder RA, LeVine RA, Social Science Research Council (U.S.) Culture theory : essays on mind, self, and emotion. Cambridge University Press; Cambridge [Cambridgeshire] ; New York: 1984. Committee on Social and Affective Development During Childhood. [Google Scholar]
- 35.Brandt AM, Rozin P. Morality and health. Routledge; New York: 1997. [Google Scholar]