Abstract
Objective
The role of diet quality and nutrient adequacy in the etiology of childhood obesity is poorly understood. The specific aims of these analyses were to 1) assess overall diet quality and nutrient adequacy, and 2) test for association between weight status and diet in children from low socioeconomic status (SES) Hispanic families at high risk for obesity.
Design
A cross-sectional study design was used to assess dietary intake in low-SES non-overweight and overweight Hispanic children enrolled in the VIVA LA FAMILIA Study. Multiple-pass 24-h dietary recalls were recorded on two random, weekday occasions. Diet quality was evaluated according to United States (US) Dietary Guidelines. Nutrient adequacy was assessed using z-scores based on estimated average requirement (EAR) or adequate intake (AI).
Subjects/Setting
The study included 1030 Hispanic children and adolescents, ages 4-19 y, in Houston, Texas who participated between November 2000 and August 2004.
Statistical analysis
STATA was used for generalized estimating equations and random effects regression.
Results
Diet quality did not adhere to US dietary guidelines for fat, cholesterol, saturated fatty acids, fiber, added sugar and sodium. Although energy intake was significantly higher in overweight children, food sources, diet quality, macro- and micronutrient composition were similar between non-overweight and overweight children. Relative to EAR or AI, mean nutrient intakes were adequate (70-98% probability) in the non-overweight and overweight children, except for vitamins D and E, pantothenic acid, calcium and potassium for which z-scores cannot be interpreted given the uncertainty of their AI's.
Conclusion
While the diets of low-SES, non-overweight and overweight Hispanic children were adequate in most essential nutrients, other components of a healthy diet, which promote long-term health, were suboptimal. Knowledge of the diet of high risk Hispanic children will inform nutritional interventions and policy.
Keywords: nutrient adequacy, diet quality, dietary guidelines, childhood obesity, Hispanic population
INTRODUCTION
In the United States (US), the prevalence of overweight is among the highest in Mexican-American children and adolescents according to National Health and Nutrition Examination Surveys (NHANES) (1). In 2005-2006 the prevalence of overweight among children (2-19 y) from all ethnic/racial groups was 15.5%. For Mexican-American males and females (2-19 y) the prevalence was 23.2% and 18.5%, respectively. The increasing prevalence of childhood obesity in the US is attributed to the interaction of genes and the obesigenic environment that encourages sedentary lifestyle and excess food intake (2, 3). In addition, the Hispanic population is burdened with additional risk factors for childhood obesity including parental obesity, low socioeconomic status (SES), recent immigration, acculturation to US diet and lifestyle, limited health insurance coverage and access to medical care (4).
The higher prevalence of obesity in low-SES population groups has been attributed to lower-quality diets (5, 6). The association between low-SES and obesity might be brought about partially by the consumption of low-cost energy-dense foods in place of higher-cost nutrient-dense foods. Indeed, there is evidence (7, 8) that the diet quality of Hispanic children and adolescents does not conform to US Dietary Guidelines (9).
The VIVA LA FAMILIA Study provided the novel opportunity to assess the diet of a large cohort of Hispanic children from low-SES families at high risk for obesity (10). On average, 91% of parents were overweight or obese; parental income and education levels were low. Food insecurity was reported by 49% of households. In the US, the prevalence of obesity in Hispanic children is not inversely related to SES (11-13). However, poorer diet quality has been described in Hispanic children acculturated to the US as compared to the average US pediatric population. In NHANES 1988-94 (7) and the National Longitudinal Study of Adolescent Health (8), acculturation of Hispanic youth, compared to all racial/ethnic youth groups in the US, was associated with higher energy and sodium intakes, and a higher percent of energy from fat and saturated fat, consistent with findings in Mexican-American adults (14).
The VIVA LA FAMILIA Study was designed to identify genetic and environmental factors contributing to childhood obesity in the Hispanic population. A total of 1030 children from 319 Hispanic families, each with at least one overweight child, were thoroughly characterized. As one of the main environmental factors contributing to obesity, dietary intake of the children was assessed and is reported here. It is hypothesized that overweight Hispanic children have higher energy intakes but lower diet quality than non-overweight Hispanic children. The specific aims of these analyses were to 1) assess overall diet quality and nutrient adequacy, and 2) test for the association between weight status and diet in children from low-SES Hispanic families at high risk for obesity.
METHODS
Study design and subjects
A cross-sectional design was used to assess dietary intake in 993 of the 1030 children from 319 Hispanic families enrolled in the VIVA LA FAMILIA Study (10). The dietary recalls of 37 children were known to be unreliable by self-report; intake of the child was not typical due to illness or unusual schedule for that particular day. The study was conducted between November, 2000 and August, 2004 in Houston, Texas. Dietary intakes were obtained at the US Department of Agriculture/Agricultural Research Service Children's Nutrition Research Center on two random, weekday occasions two to four weeks apart to assess nutrient adequacy and diet quality for percent fat, percent saturated fat, cholesterol, fiber, added sugar, and sodium using the US Dietary Guidelines.
To qualify for the VIVA study, each family was required to have at least one child between the ages 4-19 y who was overweight defined as ≥ 95th percentile for body mass index (BMI) for sex and age, according to the growth charts from the US Centers for Disease Control and Prevention (15), and ≥ 85th percentile for fat mass (16, 17). Families were recruited by news interest stories on television and radio, a database maintained at the Children's Nutrition Research Center, and community outreach via health fairs and nutrition information lectures for parent groups. All children and parents gave written informed assent or consent. Families were compensated for participating in the VIVA study. The protocol was approved by the Institutional Review Boards for Human Subject Research for Baylor College of Medicine and Affiliated Hospitals and for Southwest Foundation for Biomedical Research.
Methods
Interviews were conducted with the parents, in Spanish if necessary, to obtain sociodemographic data. The Hazuda Acculturation and Assimilation Scales were completed by the fathers and mothers (scales A1, A2, A3, and S2), and children (scales A1, A2, A3, and S1) (18). Responses were coded into a composite score for each scale which ranged from 1-4, where 1 corresponded to the highest level and 4 the lowest level of accultutration. The United States Department of Agriculture (USDA) 6-item Household Food Security Survey was completed by the mother (19). These data have been presented fully elsewhere (10).
Body weight to the nearest 0.1 kg was measured with a digital balance (Healthometer, Bridegeview, IL) and height to the nearest 1 mm was measured with a stadiometer (Holtain Limited, Crymych, United Kingdom). Body mass index was calculated as weight/height2 (kg/m2). Body composition was determined by dual-energy x-ray absorptiometry using a Hologic Delphi-A whole-body scanner (version 11.2, Hologic, Inc., Waltham, MA).
A multiple-pass 24-h dietary recall was recorded on two random, weekday occasions two to four weeks apart in person by one registered dietitian using Nutrition Data Systems for Research (NDSR) (Database version 2005, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN) (20) and food models and household measures/dishware. The multiple-pass 24-h recall method uses 3 distinct passes to garner information about a subject's food intake during the preceding 24 hours. Water consumption and vitamin-mineral supplements were not included in the dietary assessment. The 24-h recalls were obtained without prior notice; children ages 7 y and under were assisted by their mothers. Each subject's recalls were analyzed by NDSR and averaged for further statistical analyses.
Nutrition Data System for Research provides data on the meal and snacks, location and time of meals, and number of servings from 166 food groupings. The 166 NDSR food groups were collapsed into a modification of 40 descriptive food categories described by Hu et al. (21). The 40 food categories were modified to capture foods commonly consumed by children and expanded to include more specific milk, beverage, and dessert/sweets categories. The 166 NDSR food groups were also collapsed into 9 major USDA food groups based on the USDA Food Coding Scheme (22, 9). The broader beverage food group, one of the 9 major USDA food groups, did not contain milk or fruit juice, but was comprised chiefly of drinks containing added sugars. The vegetable food group included legumes, French fries, and tomato/tomato sauce; however, ketchup was assigned to the miscellaneous food group. Mean nutrient intakes, which represent the usual intakes of the children, and number of servings from the food groups were computed from the two 24-h dietary recalls. Percents of total dietary energy derived from 9 major USDA food groups and the descriptive food categories were computed. These measures were used to evaluate diet quality against the standards set by the US Dietary Guidelines (23) and USDA MyPyramid (24).
To assess nutrient adequacy, z-scores were computed using estimated average requirements (EAR) or adequate intakes (AI) (25). Because EAR is expressed on a weight basis, z-scores for protein intake were calculated per kilogram body weight of each subject. This approach estimates the degree of confidence that an individual's usual intake meets his/her requirement, taking into consideration the distributions of requirements and intakes. For nutrients with an EAR, the usual intake most likely exceeds his/her requirement if the z-score is greater than 1 and therefore is deemed adequate (85% probability); similarly, if the z-score is less than −1 the usual intake has a high probability (85%) of inadequacy. The probability of dietary adequacy or inadequacy can only be estimated if the z-score is between −1 and 1. If only an AI is available, the probability that an individual's usual intake is adequate can be estimated if the usual intake equals or exceeds the AI, but if the usual intake is below the AI, no quantitative or qualitative estimate can be made. The within-subject coefficients of variation for nutrient intakes should be less than 60-70% which was the case for this cohort.
To evaluate the impact of under-reporting of dietary intake on the assessment of nutrient adequacy, the Goldberg method as modified by Black (26) was used. In this method, mean reported energy intake (EI) relative to basal metabolic rate (EI:BMR) is evaluated against the expected physical activity level (PAL) of that population. Specific thresholds for EI:BMR are determined for low, medium or high expected PALs. In this application, individual energy intakes were assessed using BMR measured by respiration calorimetry and physical activity monitored by accelerometry which were reported in previous publications (27, 28). The derived 95% confidence limits for EI:BMR were 0.77-1.86, 0.96-2.32, and 1.12-2.71 for low (PAL=1.2), medium (PAL=1.5) and high (PAL=1.75) levels of physical activity defined according to the Dietary Reference Intakes (29).
Statistical Methods
ACCESS software (version 9, Microsoft Corp, Seattle, WA) was used for database management and STATA (version 9.1, STATA Corp., College Station, TX) was used as the statistical software package. Statistics used included means and standard deviations, generalized estimating equations (GEE) and generalized least squares random effects regression.
Demographic characteristics, anthropometrics, eating patterns, food categories, food groups, nutrient intakes, nutrient adequacy, and diet quality were examined using GEE population-averaged panel-data models. To account for correlated data within families, family identification number was used as the cluster variable. Models were adjusted for sex (coded boys=1, girls=2), age and BMI status (coded non-overweight=0, overweight=1). Transformation to normality was performed as appropriate. The GEE model was specified as Gaussian family, identity link function and exchangeable correlation structure. A random effects linear regression model also was fitted to the data to test for relationships with dietary variables. A p-value of 0.05 was used to determine statistical significance.
RESULTS
Demographic data of the VIVA LA FAMILIA cohort are described in Table 1. Most (82%) of the children participating in the VIVA Study were second-generation Americans of Mexican and Central American descent. Most of the parents were from Mexico (71%); the remainder were from Central America (11%), South America (3%), and the United States (15%). Also, 73% of families included both overweight and non-overweight children. Table 2 describes the anthropometrics and eating patterns of the children. Of the overweight children, 47% were above the 99.0th BMI percentile for sex and age with z-scores ranging from 2.3 to 4.5. Most of the parents were either overweight (34%) or obese (57%). The majority of meals (67%) were consumed at home, with eating out at restaurants/cafeterias/fast food establishments occurring only occasionally (6%). The remaining meals were consumed at school (20%), work (1%), friend's home (2%), and other (4%).
Table 1.
Demographic characteristics of the VIVA LA FAMILIA cohort.
| n (n=319 households) |
% | |
|---|---|---|
| Gross Income ($) | ||
| ≤19,999 | 70 | 22 |
| 20,000 – 29,999 | 108 | 34 |
| 30,000 – 39,999 | 80 | 25 |
| ≥40,000 | 61 | 19 |
| Food Security | ||
| Food secure | 163 | 51 |
| Food insecure with no hunger | 105 | 33 |
| Food insecure with hunger | 51 | 16 |
| Education | ||
| ≤ 8th grade | 121 | 38 |
| Some high school/high school graduate |
131 | 41 |
| Some college/college graduate | 67 | 21 |
| Acculturation a | Parents | Children |
| mean ± standard deviation | ||
| Childhood experience with English | 1.2 ± 0.03 | 1.8 ± 0.05 |
| Proficiency with English | 2.5 ± 0.03 | 3.1 ± 0.04 |
| Pattern of English usage | 1.7 ± 0.03 | 3.3 ± 0.10 |
| Interaction with mainstream society | 2.0 ± 0.02 | 2.1 ± 0.04 |
Range of indicator values is 1-4. Level of acculturation decreases as the indicator value increases (18).
Table 2.
Anthropometrics, percent of total energy from meals, and location of meals for children enrolled in the VIVA LA FAMILIA Study.
| Boys | Girls | |||
|---|---|---|---|---|
| Non-overweight | Overweight | Non-Overweight | Overweight | |
 mean ± standard deviation mean ± standard deviation
|
||||
| Age (y) | 11.1 ± 4.1 | 11.2 ± 3.5 | 10.7 ± 4.5 | 11.0 ± 3.7 |
| Anthropometry | ||||
| Weight (kg)a | 43.5 ± 19.7 | 70.5 ± 29.4 | 38.8 ± 17.4 | 64.1 ± 25.0 |
| BMIb z-scorea | 0.7 ± 0.8 | 2.4 ± 0.4 | 0.6 ± 0.8 | 2.2 ± 0.3 |
| % fat massc | 22.8 ± 5.9 | 38.1 ± 5.8 | 29.6 ± 6.3 | 41.1 ± 4.9 |
|
Meal Distribution (% of total energy) |
||||
| Breakfast | 18.5 ± 10.5 | 18.1 ± 11.3 | 19.0 ± 12.3 | 17.6 ± 12.8 |
| Lunch | 29.4 ± 13.5 | 29.2 ± 13.5 | 29.2± 14.9 | 30.8 ± 13.9 |
| Snack/Other | 21.1 ± 13.5 | 19.5 ± 15.0 | 21.0 ± 14.4 | 20.0 ± 14.1 |
| Dinner/Supper | 31.0 ± 15.1 | 33.2 ± 15.3 | 30.8 ± 13.7 | 31.6 ± 15.3 |
|
Meal Location (% of total energy) |
||||
| Home | 66.2 ± 25.0 | 68.0 ± 22.9 | 67.3 ± 25.6 | 67.9 ± 23.8 |
| Work d | 1.4 ± 6.4 | 0.7 ± 5.0 | 0.4 ± 3.1 | 0.2 ± 2.1 |
| School | 19.8 ± 20.9 | 18.8 ± 20.1 | 20.3 ± 21.8 | 20.1 ± 20.9 |
| Restaurant/Cafeteria | 7.0 ± 15.1 | 6.3 ± 13.8 | 6.1 ± 14.4 | 6.2 ± 13.7 |
| Friend's Home | 2.1 ± 7.5 | 1.9 ± 8.7 | 2.2 ± 7.9 | 2.3 ± 9.6 |
| Other d,e | 3.5 ± 10.8 | 4.3 ± 11.9 | 3.7 ± 10.5 | 3.3 ± 10.4 |
Adjusted for family membership and age, significant difference by sex and BMI status (P=0.001-0.003)
BMI=body mass index
Adjusted for family membership and age, significant interaction by sex × BMI status (P=0.001)
Adjusted for family membership and age, significant difference by sex (P=0.001-0.02)
Other category includes: Daycare, Deli/Store/Take-out/Store, Community Meal Program, Party/Sporting Event
The relationships between sociodemographic factors and diet quality and nutrient adequacy were analyzed, controlling for age, sex and BMI status of the child. Household Food Security score and parental education were not related to diet quality and nutrient adequacy. Family income, paternal, maternal and child acculturation (A1, A2 and A3) were positively associated with sodium intake (P<0.05). Within the limited SES range of these families, sociodemographic factors were not associated with the nutrient z-scores.
Under-reporting was found in 9.7% of the children overall. Although elimination of the under-reporters from the diet assessment resulted in a statistically insignificant increase of 3% in total energy intake, there were no statistically significant differences in z-scores for any of the nutrients, except for phosphorus (increased from 1.26 to 1.42) and protein (increased from 4.22 to 4.62). Therefore, all children were included in the dietary assessment and analysis.
Diet Quality
Percent of total energy from each of the 15 food categories most commonly consumed by the VIVA LA FAMILIA children is presented in Table 3. Together these 15 categories provide 68% of the total energy intake (21). Although absolute energy intakes differed by BMI status, the percent of energy from most food categories (e.g. grains, soda, beef, desserts, poultry, pizza, fruit, processed meats, other milk and burgers) was similar between the non-overweight and overweight children. The percent of total energy intake from cold cereal and whole milk, however, was lower in the overweight compared with the non-overweight children (P<0.04). The percent of energy from snack chips was higher and the percent from juice lower in the overweight than the non-overweight girls (P<0.01).
Table 3.
Percent of total energy intake from the fifeteen food categories most commonly consumed by children in the VIVA LA FAMILIA cohort.
| Food Category | Boys | Girls | ||
|---|---|---|---|---|
| Non-overweight | Overweight | Non-Overweight | Overweight | |
| n | 220 | 274 | 265 | 234 |
 mean ± standard deviation mean ± standard deviation 
|
||||
| Grains | 10.8 ± 8.9 | 11.7 ± 7.7 | 11.0 ± 8.2 | 10.8 ± 7.7 |
| Soda | 6.7 ± 6.5 | 6.8 ± 6.6 | 5.5 ± 6.8 | 6.4 ± 6.8 |
| Beefa | 5.8 ± 7.9 | 5.5 ± 8.0 | 4.5 ± 6.3 | 5.1 ± 7.4 |
| Dessertsa | 5.6 ± 7.2 | 3.9 ± 6.3 | 5.3 ± 7.7 | 5.5 ± 7.7 |
| Poultry | 5.3 ± 8.5 | 6.1 ± 7.6 | 5.6 ± 8.2 | 5.3 ± 7.2 |
| Cold cerealb | 5.1 ± 5.9 | 3.9 ± 4.8 | 4.5 ± 5.4 | 3.2 ± 4.6 |
| Pizza | 4.9 ± 8.5 | 4.3 ± 8.5 | 4.2 ± 8.8 | 3.4 ± 6.9 |
| Whole milkb | 4.3 ± 6.2 | 3.2 ± 5.2 | 4.3 ± 7.0 | 3.0 ± 5.7 |
| Snack chipsc | 4.1 ± 6.6 | 3.3 ± 5.6 | 4.1 ± 6.0 | 5.7 ± 7.7 |
| Fruit drinks | 3.6 ± 5.5 | 3.4 ± 5.0 | 3.4 ± 5.0 | 4.2 ± 6.2 |
| Fruit juicec | 2.8 ± 4.3 | 3.2 ± 5.0 | 4.1 ± 5.5 | 2.6 ± 4.1 |
| Fruit | 2.7 ± 3.8 | 2.6 ± 3.3 | 3.1 ± 4.2 | 2.9 ± 3.7 |
| Processed meats | 2.7 ± 4.7 | 3.8 ± 6.0 | 3.3 ± 5.1 | 3.1 ± 5.5 |
| Other milk | 2.7 ± 4.3 | 3.2 ± 4.9 | 2.7 ± 4.1 | 2.9 ± 4.5 |
| Burgers | 2.5 ± 6.2 | 3.2 ± 8.2 | 1.8 ± 5.1 | 2.5 ± 6.5 |
Adjusted for family membership and age, significant difference by sex (P=0.002-0.034)
Adjusted for family membership and age, significant difference by BMId status (P=0.001-0.04)
Adjusted for family membership and age, significant interaction by sex × BMI status (P=0.004)
BMI=body mass index
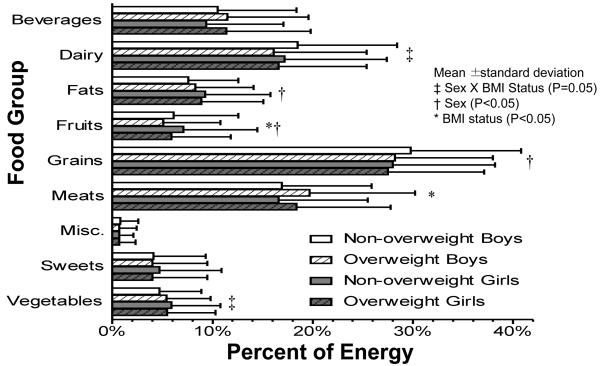
Diet quality also was evaluated based on the recommended servings from the USDA food groups (Table 4). The number of servings of vegetables, meats, fats and beverages were higher in the overweight than the non-overweight children (P<0.05). The overweight girls ate less servings of fruit than the non-overweight girls (P=0.04). The percent of energy from the 9 USDA food groups did not differ by BMI status, except for the percent of energy derived from fruit (lower in overweight) and meat (higher in overweight) and dairy (lower in overweight boys) (P<0.05) (Figure 1).
Table 4.
Number of servings from nine major USDA food groups consumed by non-overweight and overweight Hispanic children in the VIVA LA FAMILIA cohort.
| Food Group | Recommended Rangea |
Boys | Girls | ||
|---|---|---|---|---|---|
| Non- overweight |
Overweight | Non- Overweight |
Overweight | ||
| n | 220 | 274 | 265 | 234 | |
 mean ± standard deviation mean ± standard deviation 
|
|||||
| Fruitsb | 2-5 | 1.8 ± 2.0 | 1.8 ± 1.9 | 2.0 ± 2.0 | 1.5 ± 1.6 |
| Vegetablesc | 2-8 | 1.9 ± 1.8 | 1.9 ± 1.5 | 1.6 ± 1.3 | 1.8 ± 1.3 |
| Grainsd | 3-10 | 7.2 ± 3.3 | 6.9 ± 2.8 | 5.4 ± 2.2 | 5.8 ± 2.7 |
| Meatse | 2-7 | 4.8 ± 3.0 | 5.8 ± 3.5 | 3.8 ± 2.2 | 4.5 ± 2.8 |
| Dairyd | 2-3 | 2.4 ± 1.5 | 2.4 ± 1.5 | 2.0 ± 1.2 | 2.0 ± 1.3 |
| Fatsc | 2.6 ± 2.5 | 2.9 ± 2.6 | 2.6 ± 2.3 | 2.6 ± 2.2 | |
| Sweets | 1.0 ± 2.0 | 0.8 ± 1.5 | 0.9 ± 2.0 | 0.8 ± 1.2 | |
| Beveragese | 2.7 ± 2.1 | 2.9 ± 2.3 | 2.0 ± 1.8 | 2.7 ± 1.9 | |
| Miscellaneousd | 1.2 ± 1.7 | 1.0 ± 1.3 | 0.8 ± 1.2 | 0.8 ± 1.1 | |
Recommendations are based on MyPyramid (24)
Adjusted for family membership and age, significant interaction by sex × BMIf status (P=0.003)
Adjusted for family membership and age, significant difference by BMI status (P=0.001-0.05)
Adjusted for family membership and age, significant difference by sex (P=0.001)
Adjusted for family membership and age, significant difference by sex, BMI status (P=0.001-0.003)
BMI=body mass index
Figure 1.
Percent of total energy intake from nine major United States Department of Agriculture food groups for children in the VIVA LA FAMILIA cohort.
Macronutrient intakes are summarized in Table 5. Adjusted for age, energy intake was higher in the overweight compared with the non-overweight children (P=0.02) and in boys compared with girls (P<0.001). Absolute amounts of carbohydrate (girls only), protein and fat consumed by the overweight children exceeded that of the non-overweight children (P<0.05). However, the distribution of macronutrients differed only slightly between BMI groups: percent of energy derived from carbohydrate was lower (P=0.006) and the percent from protein higher (P=0.01) in the overweight children; the percent of energy from fat did not differ between BMI groups. Relative to the Acceptable Macronutrient Distribution Range (AMDR) for fat intake (25), 43% of subjects exceeded the upper limit of 35% and 7% fell below the lower limit of 25%. Protein intakes exceeded the upper limit of 30% in 8% of subjects. Carbohydrate intake fell within the AMDR for most children; 5% exceeded and 12% fell below the AMDR for carbohydrate. Total fiber intake of these children was higher in boys than girls, but did not differ by BMI status. In general, the intake of specific fatty acids was higher among the overweight children (P<0.05). Cholesterol intake was significantly higher in the overweight children (P=0.02). Approximately 31% of the children consumed more than 300 mg/d cholesterol and 80% consumed greater than 10% saturated fatty acids. Total simple sugars and added sugar provided approximately 30% and 20%, respectively, of total energy intake. Total simple sugar and added sugar consumption were higher in overweight compared with non-overweight girls (P<0.01). Total simple sugar and added sugar as percentages of total energy intake did not differ between the overweight and non-overweight children. The recommended maximal intake level of 25% for added sugars was exceeded in the diets of 24.8% of the children.
Table 5.
Energy, carbohydrate, protein and fat intakes of non-overweight and overweight Hispanic children enrolled in the VIVA LA FAMILIA Study.
| Boys | Girls | ||||
|---|---|---|---|---|---|
| Nutrient | Dietary Reference Intakes |
Non- overweight |
Overweight | Non- overweight |
Overweight |
| n | 220 | 274 | 265 | 234 | |
 mean ± standard deviation mean ± standard deviation 
|
|||||
| Energy (kcal/d)a | 2190 ± 769 | 2180 ± 655 | 1752 ± 507 | 1912 ± 636 | |
| Carbohydrate (g/d)b | 130† | 294 ± 108 | 282 ± 87 | 233 ± 71 | 252 ± 89 |
| Protein (g/d)a | 19-52† | 75 ± 25 | 79 ± 27 | 60 ± 20 | 66 ± 23 |
| Fat (g/d)a | 82 ± 35 | 85 ± 33 | 67 ± 25 | 74 ± 31 | |
| Saturated fatty acids (SFA) (g/d)c |
30 ± 13 | 30 ± 12 | 24 ± 10 | 26 ± 12 | |
| Carbohydrate (% energy)d |
45-65%† | 54.1 ± 6.7 | 52.1 ± 7.7 | 53.7 ± 6.9 | 53.0 ± 7.5 |
| Protein (% energy)a | 10-30%† | 13.9 ± 2.9 | 14.6 ± 2.9 | 13.8 ± 3.2 | 14.0 ± 3.5 |
| Fat (% energy) | 25-35%† | 33.3 ± 5.5 | 34.4 ± 6.4 | 33.8 ± 5.9 | 34.1 ± 6.1 |
| SFA (% energy) | 10%≡ | 12.4 ± 2.9 | 12.4 ± 2.8 | 12.3 ± 2.7 | 12.2 ± 2.7 |
| Trans fatty acids (g/d)c | 5.5 ± 3.5 | 5.4 ± 3.0 | 4.4 ± 2.6 | 4.7 ± 3.3 | |
| Cholesterol (mg/d)a | 270 ± 170 | 301 ± 188 | 224 ± 123 | 246 ± 155 | |
| Total fiber (g/d)c | 25-38† | 16 ± 8 | 15 ± 7 | 13 ± 6 | 13 ± 6 |
| Simple sugars (g/d)b | 161 ± 68 | 154 ± 57 | 127 ± 51 | 139 ± 60 | |
| Simple sugars (% energy) |
29.6 ± 7.0 | 29.5 ± 7.2 | 29.0 ± 7.7 | 29.3 ± 8.1 | |
| Added sugars (g/d)b | 114 ± 63 | 111 ± 72 | 83 ± 49 | 101 ± 61 | |
| Added sugar (% energy) |
25%≡ | 20.8 ± 8.0 | 20.4 ±11.8 | 19.0 ± 9.0 | 21.0 ± 9.3 |
Range of Recommended Dietary Allowances for 4-18y (29)
Maximal intake level (29)
Adjusted for family membership and age, significant difference by sex, BMIe status (P=0.001-0.04)
Adjusted for family membership and age, significant interaction by sex × BMI status (P=0.001-0.04)
Adjusted for family membership and age, significant difference by sex (P=0.001-0.04)
Adjusted for family membership and age, significant for BMI status (P=0.001-0.03)
BMI=body mass index
Nutrient Adequacy
The z-scores for the assessment of the nutrient adequacy of the diets based on EAR or AI are presented in Table 6. With the exceptions of vitamin A, vitamin D, vitamin E, pantothenic acid, magnesium, calcium, potassium and fiber, the nutrient z-scores exceeded 1.0, indicating that usual intakes were most likely adequate in the overweight and non-overweight children. In the case of vitamin A and magnesium, there is a 70% probability that the usual intake was adequate. For vitamin E, there is a 50% probability that the usual intake was inadequate. For vitamin D, pantothenic acid, calcium and potassium, the negative z-scores cannot be interpreted given the uncertainty of the AIs. Fiber intake exceeded the AI in only 7% of children.
Table 6.
Z-scores for assessment of the nutrient adequacy of the diets of non-overweight and overweight Hispanic children participating in the VIVA LA FAMILIA Study.
| Boys | Girls | |||
|---|---|---|---|---|
| Nutrient | Non- overweight |
Overweight | Non- Overweight |
Overweight |
| n | 220 | 274 | 265 | 234 |
 mean ± standard deviation mean ± standard deviation 
|
||||
| Proteina | 6.23 ± 4.5 | 2.74 ± 3.28 | 5.46 ± 4.85 | 2.26 ± 3.05 |
| Vitamin A | 0.76 ± 2.39 | 0.59 ± 2.79 | 0.47 ± 2.03 | 0.44 ± 3.11 |
| Vitamin D | 0.42 ± 1.89 | 0.32 ± 1.80 | −0.23 ± 1.54 | −0.23 ± 1.59 |
| Vitamin Eb | 0.01 ± 1.25 | −0.12 ± 1.18 | −0.46 ± 1.31 | −0.25 ± 1.36 |
| Vitamin C | 1.59 ± 1.89 | 1.30 ± 1.47 | 1.65 ± 1.96 | 1.56 ± 1.91 |
| Thiaminc | 2.24 ± 1.68 | 2.11 ± 1.45 | 1.93 ± 1.32 | 2.02 ± 1.54 |
| Riboflavin | 2.26 ± 1.56 | 2.1 ± 1.43 | 2.19 ± 1.55 | 2.22 ± 1.72 |
| Niacin | 1.79 ± 1.32 | 1.76 ± 1.28 | 1.61 ± 1.25 | 1.72 ± 1.37 |
| Pantothenic acida | 0.31 ± 1.64 | 0.40 ± 1.54 | −0.31 ± 1.60 | −0.21 ± 1.60 |
| Vitamin B6 | 1.72 ± 1.36 | 1.61 ± 1.21 | 1.67 ± 1.44 | 1.66 ± 1.57 |
| Folatec | 1.75 ± 1.81 | 1.4 ± 1.50 | 1.37 ± 1.97 | 1.18 ± 1.83 |
| Vitamin B12c | 2.01 ± 2.09 | 2.00 ± 3.43 | 1.58 ± 1.82 | 1.96 ± 4.15 |
| Calciumc | −0.21 ± 1.65 | −0.52 ± 1.4 | −1.08 ± 1.70 | −1.16 ± 1.63 |
| Phosphorusc | 1.52 ± 1.65 | 1.29 ± 1.66 | 1.05 ± 1.72 | 1.07 ± 1.84 |
| Magnesiumc | 0.76 ± 1.58 | 0. 7 ± 1.47 | 0.43 ± 1.72 | 0.45 ± 1.73 |
| Iron | 1.76 ± 1.20 | 1.62 ± 1.09 | 1.62 ± 1.34 | 1.64 ± 1.28 |
| Zinc | 1.15 ± 1.04 | 1.08 ± 1.14 | 1.01 ± 1.26 | 1.05 ± 1.36 |
| Copperc | 1.66 ± 1.22 | 1.57 ± 1.15 | 1.32 ± 1.15 | 1.42 ± 1.38 |
| Seleniuma | 3.14 ± 1.77 | 3.45 ± 1.82 | 2.26 ± 1.26 | 2.70 ± 1.84 |
| Sodiuma | 1.85 ± 1.08 | 1.97 ± 1.28 | 1.52 ± 1.11 | 1.85 ± 1.38 |
| Potassiumc | −2.58 ± 1.25 | −2.54 ± 1.08 | −3.86 ± 1.4 | −3.76 ± 1.50 |
| Fiber | −2.94 ± 1.54 | −3.12 ± 1.34 | −2.65 ± 1.29 | −2.61 ± 1.31 |
Adjusted for family membership and age, significant difference by sex and BMI status (P=0.001-0.03)
Adjusted for family membership and age, significant interaction by sex × BMId status (P=0.001-0.03)
Adjusted for family membership and age, significant difference by sex (P=0.001-0.03)
BMI=body mass index
Associations between nutrient z-scores and percent of energy from the 9 major USDA food groups were examined by regression analysis. Significant independent predictors of nutrient z-scores are presented in Table 7. Percent of energy from beverages was negatively correlated with all nutrient z-scores except vitamin C and sodium. Percent of energy from dairy was positively correlated with z-scores for protein, vitamin A, vitamin D, riboflavin, pantothenic acid, vitamin B12, calcium, phosphorus, magnesium, and zinc. A positive correlation between percent of energy intake from grains and z-scores from vitamin E, thiamin, riboflavin, niacin, folate, and iron was observed, but the correlation was negative for protein, pantothenic acid, and potassium.
Table 7.
Nutrient Z-scores and percent of energy from the nine major United States Department of Agriculture food groups in non-overweight and overweight Hispanic children from the VIVA LA FAMILIA cohort.
| Dependent variable: Nutrient Z-scores |
Significant independent variablesa: Percent of energy from food groups (regression coefficients) |
R2 | ||||
|---|---|---|---|---|---|---|
| Protein | −13.4 Bev | 7.32 Dairy | −7.18 Fat | −5.95 Grain | 0.143 | |
| Vitamin A | −3.24 Bev | 5.35 Dairy | 0.060 | |||
| Vitamin D | −3.49 Bev | 6.20 Dairy | 0.186 | |||
| Vitamin E | −1.51 Bev | 6.19 Fat | 2.41 Grain | 0.116 | ||
| Vitamin C | 14.1 Fruit | 4.23 Veg | 0.263 | |||
| Thiamin | −4.58 Bev | 1.63 Grain | −2.59 Meat | −2.83 Sweet | 0.120 | |
| Riboflavin | −3.38 Bev | 5.55 Dairy | 1.70 Grain | 0.198 | ||
| Niacin | −2.71 Bev | 0.92 Grain | −2.32 Sweet | 0.042 | ||
| Pantothenic acid | −6.01 Bev | 2.35 Dairy | −2.53 Grain | −2.80 Sweet | 0.154 | |
| Vitamin B6 | −3.74 Bev | 3.14 Fruit | −2.98 Sweet | 2.46 Veg | 0.104 | |
| Folate | −5.85 Bev | 2.54 Grain | −3.07 Meat | −2.17 Sweet | 10.31 Veg | 0.215 |
| Vitamin B12 | −2.95 Bev | 4.84 Dairy | 4.54 Meat | 0.052 | ||
| Calcium | −1.85 Bev | 9.62 Dairy | 0.364 | |||
| Phosphorus | −3.04 Bev | 6.57 Dairy | 0.182 | |||
| Magnesium | −4.02 Bev | 4.86 Dairy | 2.99 Fruit | 6.78 Veg | 0.204 | |
| Iron | −3.04 Bev | 2.48 Grain | 1.02 Veg | 0.105 | ||
| Zinc | −2.01 Bev | 2.96 Dairy | 2.24 Meat | 0.103 | ||
| Copper | −1.45 Bev | 2.72 Fruit | 7.71 Veg | 0.100 | ||
| Selenium | −3.54 Bev | 3.04 Fat | −4.72 Fruit | 3.82 Meat | 0.093 | |
| Sodium | 1.82 Fat | −3.25 Fruit | 0.053 | |||
| Potassium | −3.49 Bev | 2.69 Fruit | −2.33 Grain | −2.47 Sweet | 6.05 Veg | 0.152 |
| Fiber | −3.24 Bev | −2.72 Meat | 14.4 Veg | 0.303 | ||
(P=0.03 − 0.001)
Abbreviations: Bev=beverage, Veg=vegetable
DISCUSSION
Diets in low-SES Hispanic children were adequate in most nutrients, but frequently exceeded guidelines for percent total fat, percent saturated fat, cholesterol, added sugar, and sodium intakes. Low intakes of fruits, vegetables, and fiber diminished the quality of the diet. With few exceptions (noted in the results section), non-overweight and overweight children from these Hispanic families consumed diets that were qualitatively, but not quantitatively, similar. This finding may result from the availability of similar foods within a shared household.
In the present VIVA study, diet quality of both the non-overweight and overweight children did not adhere to the US Dietary Guidelines which recommend the consumption of a variety of nutrient-dense foods and beverages within and among the basic food groups while choosing foods that limit the intake of saturated and trans fats, cholesterol, added sugars and salt (9). The principal food sources providing 68% of dietary energy included soda, desserts, pizza, snack chips, fruit drinks, fruit juice, processed meats and burgers which are high in fat, sugar, and/or sodium. The high reliance on grains, cold cereal, fruit juice, and fruit drinks suggests that the nutrient adequacy of the diets of these children was augmented by food fortification. Interestingly, the percent of energy from cold cereal and whole milk consumed by overweight children was less than that consumed by non-overweight children. Overweight children tended to consume greater amounts of low-fat milks, so that only the percent of energy varied, consistent with similar numbers of milk servings between groups. The association between dairy intake and weight status is not clear in the literature (30). Conflicting results in the literature may be attributed to differences in study design and subject profiles, use of all dairy food products versus milk, and use of milks varying in fat content. Further exploration of the association between dairy product consumption and weight status is needed to better interpret the results from the current study.
The mean number of servings of fruits and vegetables was lower than recommended in the US Dietary Guidelines for all children. A dietary pattern consisting of low intakes of fruits and vegetables, together with high intakes of high-fat, high-sugar foods, is consistent with that found in previous studies in Mexican-American children (31, 32). However, the relatively higher vegetable intake among overweight children, compared with their non-overweight siblings, maybe due to eating greater amounts of raw and cooked vegetables or combination foods prepared with vegetables.
The relatively low proportion of restaurant/cafeteria/fast foods consumed by the VIVA cohort, as reported in the Results section, is in contrast to findings from the Continuing Survey of Food Intakes by Individuals (CSFII) 1994-1996 in which 30.3% of all children and 23.3% of Hispanic children reported consuming fast food on a typical day (33). Limited income or cultural practices may have limited the number of meals outside of the home for the VIVA families.
In other aspects, the food consumption patterns of the VIVA children were not qualitatively dissimilar from other American children. The macronutrient composition of the diets of these Hispanic children resembles that of the general US population of children. Data collected from NHANES 2003-2004 (34) were not different for Mexican-Americans versus all ethnic/racial groups (6-19 y): 53%, 14%, and 33% of energy from carbohydrate, protein, and fat, respectively. These percentages are similar to those attained in this study, although total energy intake in VIVA was lower by 200 kcals. Qualitative results similar to those in the current study were found in yet another study. The macronutrient distribution, 4-18 y old, was 14% of energy from protein, 54% from carbohydrate, and 32% from fat in the Continuing Survey of Food Intakes by Individuals (CSFII) 1994-1996, 1998 (29). The mean cholesterol intake was 232 g and the mean fiber intake was 13.7 g. Percent of energy from added sugar was not comparable between the VIVA children and those in the CSFII sample, however, where intakes were 20.3% and 15.5%, respectively (35). The reason for this is not clear. Differences between VIVA and NHANES or CSFII data sets could result from regional influences unique to southeast Texas, socio-economic parameters, or acculturation into Hispanic traits and social patterns. Alternatively, an increase of added sugar intake in the overall population in more recent years could account for the difference. Milk consumption decreases with age, coincident with the rise in soda intake (36, 37).
In the VIVA study, the percent of energy intake from sodas (6.3%) and fruit drinks (3.7%) did not differ between the non-overweight and overweight children. According to the Nationwide Food Consumption Survey 1977/1978, CSFII 1994/1996, and the Supplemental Children's Survey 1998, the mean intake of soda in children, 6-17 y, increased from 5 to 12 fl oz per day in 1977/78 to 1994/98; energy derived from soda doubled from 2.9 to 5.9% of total energy intake (38).
Correlations between percent of energy from food groups and nutrient z-scores were consistent with expected food composition values, with few exceptions. Iron z-scores were not significantly correlated with meat, but were positively correlated with percent of energy from grains, which likely reflects fortification of cereals consumed. Further evidence of dietary fortification was the positive correlation between percent of energy from grains and z-scores for vitamin E, thiamin, riboflavin, niacin, and folate and also between percent of energy from dairy and z-scores of vitamin A and vitamin D. The lack of an association between percent of energy from meat and protein z-score was unexpected; however, protein z-score was calculated per kilogram body weight which may explain why the anticipated result was not observed. Most notably, in these Hispanic children, intake of energy in the form of beverages was negatively associated with z-scores for a majority of nutrients; only z-scores for vitamin C and sodium were not associated. Nutrient dilution results when energy-dense and nutrient-poor foods, frequently sugar-laden beverages, are consumed to the extent that the nutritive quality of the diet is reduced. The beverages food group did not contain milk or fruit juice, but was comprised chiefly of drinks containing added sugars. The negative association between energy from beverages and nutrient z-scores corroborates findings in other studies where increasing intake of sweetened beverages was associated with nutrient dilution (35, 39, 40). However, the positive correlations between percent of energy from dairy and many nutrient z-scores substantiates the contribution of dairy products to nutrient adequacy.
The nutrient intakes of these Hispanic children were adequate, for the most part. Exceptions included vitamin E which was low relative to the EAR and vitamin D, pantothenic acid, calcium and potassium which were lower than the AI. Fiber intake also was considerably below the AI. These are nutrients or dietary components that are commonly reported low in US diets (41). Definitive assessment of the nutrient adequacy or inadequacy of vitamin D, pantothenic acid, calcium and potassium is not possible given the uncertainty of the AI. For the determination of the EAR for vitamin E and the AI for fiber, there were no substantive pediatric data to determine requirements and therefore the extrapolation of adult data to children may be inappropriate.
This study has some limitations. First, the results of this study are only generalizable to low-SES Hispanic children living in an urban community. Secondly, since these data were cross-sectional, cause and effect relationships cannot be determined. Longitudinal studies would be needed to test the effect of diet on the development of obesity.
CONCLUSION
The diets of these low-SES Hispanic children were adequate in most essential nutrients, but suboptimal for the promotion of long-term health. Diet quality did not satisfy US dietary guidelines for fat, cholesterol, saturated fatty acids, fiber, added sugar and sodium. Although energy intake was higher in overweight children, food sources, diet quality and macro- and micronutrient composition were similar between non-overweight and overweight siblings. Relative to EAR or AI, mean nutrient intakes indicated adequate (70-98% probability) usual intakes in the non-overweight and overweight children, except for vitamins D and E, pantothenic acid, calcium and potassium for which z-scores cannot be interpreted given the uncertainty of their AI's. Future studies might investigate diet quality and nutrient adequacy of other ethnic groups at risk for overweight. Knowledge of the dietary intake of children from low-SES Hispanic families at high risk for obesity will provide a basis on which to build nutritional interventions and policy that are appropriately tailored to population sub-groups.
Supplementary Material
ACKNOWLEDGMENTS
The authors wish to thank the families who participated in this study, and to acknowledge the contributions of Mercedes Alejandro and Marilyn Navarrete for study coordination, and Sopar Seributra for nursing and Nitesh Mehta, Tina Ziba, Maurice Puyau, Firoz Vohra, Roman Shypailo, JoAnn Pratt, and Maryse Laurent for technical assistance. Theresa A. Wilson is responsible for the dietary analysis and Anne L. Adolph for the statistical analysis. Nancy F. Butte is responsible for the study design, execution and analysis of the study.
This work is a publication of the U.S. Department of Agriculture (USDA)/Agricultural Research Service (ARS) Children's Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children's Hospital, Houston, Texas. This project was funded with federal funds from the NIH R01 DK59264 and from USDA/ARS under Cooperative Agreement 58-6250-51000-037. The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest with the research described in this manuscript.
Contributor Information
Theresa A. Wilson, USDA/ARS Children's Nutrition Research Center, Department of Pediatrics Baylor College of Medicine, 1100 Bates Street; Houston, Texas 77030 713-798-7111 tel; 713-798-7187 FAX; tkoteras@bcm.edu.
Anne L. Adolph, USDA/ARS Children's Nutrition Research Center, Department of Pediatrics Baylor College of Medicine, 1100 Bates Street; Houston, Texas 77030 713-798-6750 tel; 713-798-7187 FAX; aadoph@bcm.edu.
Nancy F. Butte, USDA/ARS Children's Nutrition Research Center, Department of Pediatrics Baylor College of Medicine, 1100 Bates Street; Houston, Texas 77030 713-798-7179 tel; 713-798-7187 FAX; nbutte@bcm.edu.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Comuzzie AG, Allison DB. The search for human obesity genes. Science. 1998;280:1374–1377. doi: 10.1126/science.280.5368.1374. [DOI] [PubMed] [Google Scholar]
- 3.Allison DB, Matz PE, Pietrobelli A, Zannolli R, Faith MS. Genetic and environmental influences on obesity. In: Bendich A, Deckelbaum RJ, editors. Primary and Secondary Preventive Nutrition. Humana Press Inc.; Totowa: 2001. p. 147. [Google Scholar]
- 4.Kumanyika SK. Obesity treatment in minorities. In: Wadden T, Stunkard A, editors. Handbook of Obesity Treatment. Gullford Press; New York: 2002. pp. 416–446. [Google Scholar]
- 5.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82(1):265S–273S. doi: 10.1093/ajcn/82.1.265S. [DOI] [PubMed] [Google Scholar]
- 6.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 7.Mazar RE, Marguis GS, Jensen HH. Diet and food insufficiency among Hispanic youths: acculturation and socioeconomic factors in the third National Health and Nutrition Examination Survey. Am J Clin Nutr. 2003;78:1120–1127. doi: 10.1093/ajcn/78.6.1120. [DOI] [PubMed] [Google Scholar]
- 8.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 9.U.S.Department of Health and Human Services The Report of the Dietary Guidelines for Americans, 2005. Healthier US Website. http://www.health.gov/DietaryGuidelines/dga2005/report/. Accessed July 31, 2007.
- 10.Butte NF, Cai G, Cole SA, Comuzzie AG. VIVA LA FAMILIA Study: genetic and environmental contributions to childhood obesity and its comorbidities in the Hispanic population. Am J Clin Nutr. 2006;84(3):646–654. doi: 10.1093/ajcn/84.3.646. [DOI] [PubMed] [Google Scholar]
- 11.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology and demographics. Pediatrics. 1998;101(3):497–504. [PubMed] [Google Scholar]
- 12.Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in U. S. adolescents. Obes Res. 2003;11(1):121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 14.Dixon LB, Sundquist J, Winkleby M. Differnces in energy, nutrient, and food intakes in a US sample of Mexican-American women and men: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2000;152:548–557. doi: 10.1093/aje/152.6.548. [DOI] [PubMed] [Google Scholar]
- 15.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC Growth Charts: United States. Adv Data. 2000;317:1–27. [PubMed] [Google Scholar]
- 16.Ellis KJ. Body composition of a young, multiethnic, male population. Am J Clin Nutr. 1997;66:1323–1331. doi: 10.1093/ajcn/66.6.1323. [DOI] [PubMed] [Google Scholar]
- 17.Ellis KJ, Abrams SA, Wong WW. Body composition of a young, multiethnic female population. Am J Clin Nutr. 1997;65:724–731. doi: 10.1093/ajcn/65.3.724. [DOI] [PubMed] [Google Scholar]
- 18.Hazuda HP, Stern MP, Haffner SM. Acculturation and assimilation among Mexican Americans: scales and population-based data. Soc Sci Quart. 1988;69:687–705. [Google Scholar]
- 19.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security. USDA, Food and Nutrition Service; Alexandria: 2000. (Report No. 6). [Google Scholar]
- 20.Johnson RK, Driscoll P, Goran MI. Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. J Am Diet Assoc. 1996;96(11):1140–1144. doi: 10.1016/S0002-8223(96)00293-3. [DOI] [PubMed] [Google Scholar]
- 21.Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–249. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Agriculture, Agricultural Research Service USDA Nutrient Database for Standard Reference, Release 20. Nutrient Data Laboratory Home Page. http://www.ars.usda.gov/ba/bhnrc/ndl. Accessed July 31, 2007.
- 23.U.S. Department of Agriculture Dietary Guidelines for Americans, Executive Summary. 2005 [Google Scholar]
- 24.U.S. Department of Agriculture MyPyramid. MyPyramid Website. http://mypyramid.gov/. Accessed July 31, 2007.
- 25.Food and Nutrition Board . DRI Dietary Reference Intakes: applications in dietary assessment. National Academy Press; Washington, D.C.: 2000. [PubMed] [Google Scholar]
- 26.Black AE. The sensitivity and specificity of the Goldberg cut-off for EI:BMR for identifying diet reports of poor validity. Eur J Clin Nutr. 2000;54:395–404. doi: 10.1038/sj.ejcn.1600971. [DOI] [PubMed] [Google Scholar]
- 27.Butte NF, Puyau MR, Vohra FA, Adolph AL, Mehta NR, Zakeri I. Body size, body composition, and metabolic profile explain higher energy expenditure in overweight children. J Nutr. 2007;137(12):2660–2667. doi: 10.1093/jn/137.12.2660. [DOI] [PubMed] [Google Scholar]
- 28.Butte NF, Puyau MR, Adolph AL, Vohra FA, Zakeri I. Physical activity in nonoverweight and overweight Hispanic children and adolescents. Med Sci Sports Exerc. 2007;39(8):1257–1266. doi: 10.1249/mss.0b013e3180621fb6. [DOI] [PubMed] [Google Scholar]
- 29.Institute of Medicine . Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. 5 ed. National Academy of Science; Washington DC: 2002. [DOI] [PubMed] [Google Scholar]
- 30.Barba G, Russo P. Dairy foods, dietary calcium and obesity: a short review of the evidence. Nutr Metab Cardiovasc Dis. 2006;16(6):445–451. doi: 10.1016/j.numecd.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Trevino RP, Marshall RM, Jr., Hale DE, Rodriguez R, Baker G, Gomez J. Diabetes risk factors in low-income Mexican-American children. Diabetes Care. 1999;22(2):202–207. doi: 10.2337/diacare.22.2.202. [DOI] [PubMed] [Google Scholar]
- 32.Murphy SP, Castillo RO, Martorell R, Mendoza FS. An evaluation of food group intakes by Mexican-American children. J Am Diet Assoc. 1990;90:388–393. [PubMed] [Google Scholar]
- 33.Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113:112–118. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 34.US Department of Agriculture, Agricultural Research Service Nutrient Intakes from Food: Mean Amounts Consumed per Individual, by Race/Ethnicity and Age, One Day, 2003-2004. http://www.ars.usda.gov/ba/bhnrc/fsrg. Accessed May 28, 2008.
- 35.Bowman SA. Diets of individuals based on energy intakes from added sugars. Fam Econ Nutr Rev. 1999;12(2):31–38. [Google Scholar]
- 36.Lytle LA, Seifert S, Greenstein J, McGovern P. How do children's eating patterns and food choices change over time? Results from a cohort study. Am J Health Promot. 2000;14(4):222–228. doi: 10.4278/0890-1171-14.4.222. [DOI] [PubMed] [Google Scholar]
- 37.Striegel-Moore RH, Thompson D, Affenito SG, Franko DL, Obarzanek E, Barton BA, Schreiber GB, Daniels SR, Schmidt M, Crawford PB. Correlates of beverage intake in adolescent girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2006;148(2):183–187. doi: 10.1016/j.jpeds.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 38.French SA, Lin BH, Gutherie JF. National trends in soft drink consumption among children and adolescents age 6 to 17 years: Prevalence, amounts, and sources, 1977/1978 to 1994/1998. J Am Diet Assoc. 2003;103:1326–1331. doi: 10.1016/s0002-8223(03)01076-9. [DOI] [PubMed] [Google Scholar]
- 39.Forshee RA, Storey ML. The role of added sugars in the diet quality of children and adolescents. J Am Coll Nutr. 2001 Feb;20(1):32–43. doi: 10.1080/07315724.2001.10719012. [DOI] [PubMed] [Google Scholar]
- 40.Alexy U, Sichert-Hellert W, Kersting M. Associations between intake of added sugars and intakes of nutrients and food groups in the diets of German children and adolescents. Br J Nutr. 2003;90(2):441–447. doi: 10.1079/bjn2003904. [DOI] [PubMed] [Google Scholar]
- 41.Pennington J, Kandian J, Nicklaus T, Pitman S, Stitzel K. Practice paper of the American Dietetic Association: nutrient density: meeting nutrient goals within calorie needs. J Am Diet Assoc. 2007;107(5):860–869. doi: 10.1016/j.jada.2007.03.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.