Abstract
Do richer friends and neighbors improve your health through positive material effects, or do they make you feel worse through the negative effect of social comparison and relative deprivation? Using the newly available National Social Life, Health, and Aging Project (NSHAP) data set that reports individuals’ income positions within their self-defined social networks, this paper examines whether there is an association between relative position and health in the US. Because this study uses measures of individuals’ positions within their self-defined social groups rather than researcher-imputed measures of relative position, I am able to more precisely examine linkages between individual relative position and health. I find a relationship between relative position and health status, and find indirect support for the biological mechanism underlying the relative deprivation model: lower relative position tends to be associated with those health conditions thought to be linked to physiological stress. I also find, however, that only extremes of relative position matter: very low relative position is associated with worse self-rated physical health and mobility, increased overall disease burden, and increased reporting of cardiovascular morbidity; very high relative position is associated with lower probabilities of reporting diabetes, ulcers, and hypertension. I observe few associations between health and either moderately high or moderately low positions. This analysis suggests that the mechanism underlying the relative deprivation model may only have significant effects for those at the very bottom or the very top.
Keywords: USA, Relative deprivation, Reference groups, Relative income, Income inequality
Introduction and background
Empirically, income has consistently been shown to be highly correlated with health; in both aggregate and micro studies, richer people have better health and longer life expectancies (for reviews, see Adler, Boyce, Chesney, Folkman, & Syme, 1993; Adler & Ostrove, 1999). There also appears to be a strong correlation between income inequality and health. Whether comparing across countries, U.S. states, or smaller sampling regions, those geographic areas with higher levels of inequality also appear to have higher rates of mortality (see for example, Daly, Duncan, Kaplan, & Lynch, 1998; Kaplan, Pamuk, Lynch, Cohen, & Balfour, 1996; Kennedy, Kawachi, & Prothrow-Stith, 1996; Waldmann, 1992; or the review by Wilkinson and Pickett, 2006).1
One hypothesis put forth to explain these associations between health and both income and income inequality is that health is determined, not only by one’s absolute material resources, but also by one’s relative position (Marmot & Wilkinson, 2001; Wilkinson, 1996, 1997). According to this hypothesis, poor people have worse health not only because they are less able to afford health-promoting goods, but also because they experience health deficits related to the gap between their own circumstances and those of others. These health deficits are thought to stem from the psychosocial effect of finding oneself less worthy in social comparisons – in other words, from the stress of being of lower social rank. According to the relative deprivation hypothesis, the greater this difference between one’s circumstances and those of others, the worse one’s health. In the aggregate, then, the more unequal a society – that is, the greater the difference between a society’s haves and have-nots – the worse the health of society’s poorest members because of relative deprivation. This leads to worse overall (average) health, and so we observe the negative association between income inequality and health.
That low social rank has negative health effects is somewhat supported by animal studies. Among non-human primates, lower social rank is associated with higher levels of stress hormones, which if chronically elevated, lead to worse immune function, increased inflammation, and increased susceptibility to disease (Cohen et al., 1997; Sapolsky, Alberts, & Altmann, 1997). Most primate studies, however, do not attempt to exogenously change social rank; they therefore cannot rule out the possibility that an unobserved factor affects both an animal’s social dominance and its immune status, or that susceptibility to infection leads to low social rank. The one study that does manipulate the social status of monkeys finds a clear effect of rank on stress hormone response but does not directly evaluate health outcomes (Shively, Laber-Laird, & Anton, 1997).
Among humans, the hypothesis that low relative position has an independent effect on health has been more difficult to test. The biggest problem, aside from humans’ natural aversion to the randomization of their economic status, has been that, within a society, lower income implies both lower absolute resources and lower relative position; stated differently, lower income is perfectly correlated with lower relative (economic) position within a given society.
Because of this difficulty, individual-level studies that have attempted to test the relative deprivation hypothesis have evaluated, not the effect of an individual’s relative position, but rather the effect of income inequality of someone’s area of residence –state, MSA, or census sampling unit – on his or her health (for example, Fiscella & Franks, 1997; Mellor & Milyo, 2002; Sturm & Gresenz, 2002). Notably, unlike the studies that use aggregate data – which consistently report a negative association between inequality and health – these individual-level studies find no relationship between the inequality of an individual’s geographic area and his or her health.
These tests, however, do not quite estimate the effect of relative position on health. As Eibner and Evans (2005) point out, two individuals may experience the same level of inequality because they live in the same community, but their relative position within the community may be very different – and it is their relative position that affects health. These individual-level tests of inequality therefore do not truly test the relative deprivation hypothesis.
Attempts to test this hypothesis by constructing individual-level measures of relative deprivation have met with mixed results. In these papers, relative deprivation is typically determined by an individual’s income relative to the incomes of those who have the same demographic characteristics (e.g. gender, race, age, education, region of residence, occupation). Kondo, Kawachi, Subramanian, Takeda, and Yamagata (2008) unambiguously find a relationship between relative deprivation and worse self-reported health, while Jaffe, Eisenbach, Neumark, and Manor (2005), and Yngwe, Fritzell, Lundberg, Diderichsen, and Burstrom (2003) report a similar relationship in men but no such relationship among women. Others, like Eibner and Evans (2005), Gravelle and Sutton (2006), and Jones and Wildman (2008), find that empirical associations between relative position and health tend to be very sensitive to the measures of deprivation used as well as to the form of the models being estimated.
In this paper, I empirically examine the relationship between relative position and health but address an important issue that has not been attended to in previous studies. A difficulty that arises in the empirical study of relative deprivation is that individuals’ reference groups are unobserved. Consequently, an individual’s relative position must be imputed by the researcher, most often by defining someone’s relative income as this person’s income relative to the incomes of those with similar demographic characteristics. Thus, the imputed relative income of, say, Chief Justice John G. Roberts, Jr., would be his income relative to the income of – as of the time of this writing – white males, approximately 50 years old, living in Washington, DC.
While this method of constructing reference groups is reasonable given data constraints, it is not unproblematic. First, there is a fair amount of sociological evidence suggesting that someone’s reference group is not typically as broad as his geographic region or demographic classification. Reference groups tend to be more localized and are mostly limited to family, friends, neighbors, work colleagues, and others people know personally (for overviews, see Frank, 1985; Merton, 1957).
Moreover, while it is true that these localized reference groups tend to be comprised of people who have the same demographic characteristics as the primary individual (McPherson, Smith-Lovin, & Cook, 2001), it is unclear whether demographic and geographic groupings are accurately capturing that individual’s reference group. For example, that the social network of a Supreme Court Justice tends to consist of lawyers does not mean that we would be accurately representing his or her socioeconomic reference group by pooling all U.S. lawyers or indeed even all Washington, DC lawyers. Justices’ professional reference groups are more likely to be comprised of federal judges or law professors or professionally elite non-lawyers. Further, anthropological work provides evidence for the importance of locally defined norms and cultural models in specifying the criteria for social status; consonance with these local cultural models has been shown to be associated with health status (Dressler, Balieiro, Ribeiro, & Dos Santos, 2005; Dressler & Bindon, 2000; Dressler, Bindon, & Neggers, 1998), and standard demographic variables do not adequately capture these localized norms and models.
We suspect, then, that individuals are likely to be drawing, for their reference group, from a pool of demographically similar people in a way that is idiosyncratic to the individual and his/her local environment, and that is biased in important unobserved ways. Consequently, geographic or demographic classifications may not simply be innocuous approximations of actual reference groups but may be misleading indicators of them.
For this reason, this paper focuses on local reference groups as identified by the individual. Note that reference groups are ‘local’ in the sense of being part of one’s social, work, or kin network, but need not be geographically concentrated; for example, two brothers may reflexively compare themselves to each other even though one lives in New York and the other in San Francisco. To account for the social locality of reference groups, this paper uses newly available data on individuals’ positions within their local network to construct measures of relative position. These local measures will allow us to test the relative deprivation hypothesis by examining whether the mechanism behind the theory of relative deprivation could be operating: if the relative deprivation hypothesis holds and relative income has an effect on health independent of absolute income, we should observe associations between local position (relative to a reference group) and health status.
In addition to these relative position measures, this data set contains a particularly rich set of health indicators. I can thus examine associations between relative position and a broad range of health status measures. Most studies examining health use either a self-reported summary measure of health or the rather extreme outcome of death. This paper uses indicators that capture a range of well-being and morbidity. Like other papers, this paper looks at self-reported health, but I also consider reports of diagnoses of important health conditions such as diabetes, cancer, arthritis, and reports of previous strokes and heart attacks. I also use a body mass index measure calculated from height and weight measurements, and interviewer-recorded blood pressure readings. Since the health effect of social comparison is posited to work through a specific physiological stress pathway, the various measures of health will help me detect different ways in which the stress mechanism underlying the relative deprivation hypothesis may influence health.
In brief, this paper finds a relationship between relative position and health status, and finds indirect support for the biological mechanism underlying the relative deprivation model. I also find, however, that only extremes of relative position matter: very low relative position is associated with worse self-rated physical health and mobility, increased overall disease burden, and increased reporting of cardiovascular morbidity; very high relative position is associated with lower probabilities of reporting diabetes, hypertension, and ulcers. I observe few associations between health and either moderately high or moderately low positions. This analysis suggests that the mechanism underlying the relative deprivation model may only have significant effects for those at the very bottom or the very top.
Data and methods
Data
Data for the analysis were obtained from the National Social Life, Health, and Aging Project (NSHAP). NSHAP is a household survey of 3005 civilian non-institutionalized Americans aged 57–85. The first wave of the survey was conducted in 2005–06.
The sample population for NSHAP is somewhat older than the samples typically used to study the relative deprivation hypothesis, and there are benefits and limits to using such a sample. On the one hand, we might be concerned with the potential of selection bias since some individuals who had bad health outcomes would be absent from our sample because of death (in contrast to remaining in the sample and exhibiting worse health). This would tend to bias our estimates towards zero. On the other hand, individuals in this older age group would be more likely to exhibit the chronic health conditions (which require a long time to manifest themselves) most related to the conjectured mechanism underlying the relative deprivation model. Thus, an analysis using this kind of sample would provide a better test of the relative deprivation mechanism than previous studies.
Not all 3005 observations could be used for this analysis. As with many surveys that include questions on financial status, the biggest constraints on sample size were the response rates for the income and assets’ questions. In the NSHAP survey, the response rate for the income question was 71%, the response rate for the assets’ question was 62%, and the response rate for the relative income questions (described in more detail in the next section) was 79%. Excluding those observations in which there was at least one non-response among the variables of interest, the sample was reduced to 1580 observations when income was used as a resource measure, and 1408 observations when assets were used as a resource measure. Table 1 reports the descriptive statistics of these two samples.
Table 1.
Descriptive statistics.
| Variable | Weighted mean or proportion (standard deviation) |
|
|---|---|---|
| Income sample | Asset sample | |
| Age | 67.5 | 67.7 |
| % Male | 53.4 | 53.9 |
| % Black | 8.5 | 7.4 |
| % Less than high school education | 12.6 | 11.8 |
| % High school diploma | 25.5 | 24.9 |
| % College degree or higher | 29.3 | 29.9 |
| Number of adults in household | 2 | 2 |
| % Married or cohabiting | 70.2 | 70.4 |
| Household assets in 2004 ($) | 694,196 (1,633,523) | |
| Household income in 2004 ($) | 60,216 (83,886) | |
| Perceived income relative to US families (1 = far below average, 5 = far above average) | 3 (1.0) | 3 (1.0) |
| Perceived income relative to local reference group (1 = far below average, 5 = far above average) | 2.9 (0.9) | 2.9 (0.9) |
To counteract possible bias from non-response (since non-responders might be different in important ways from responders), I reweight the sample observations according to the probabilities of non-response. I first identify the ways in which non-responders (to the economic status questions) demographically differ from responders. I then predict the probability of non-response for the assets, income, and relative income questions as a function of these characteristics. Using these probabilities, I rescale the weights in my sample, upweighting the observations from those respondents whose characteristics are associated with higher probabilities of non-response. All results are reported using these new weights.
In addition to the NSHAP data, I use data from the March 2005 Annual Social and Economic Supplement to the Current Population Survey through IPUMS-CPS (Integrated Public Use Microdata Series: Current Population Survey). The 2004 distribution of U.S. household income from this survey was used to construct a measure of perception bias with respect to income (the construction of this measure is described in more detail in the Results section).
Measures of relative income
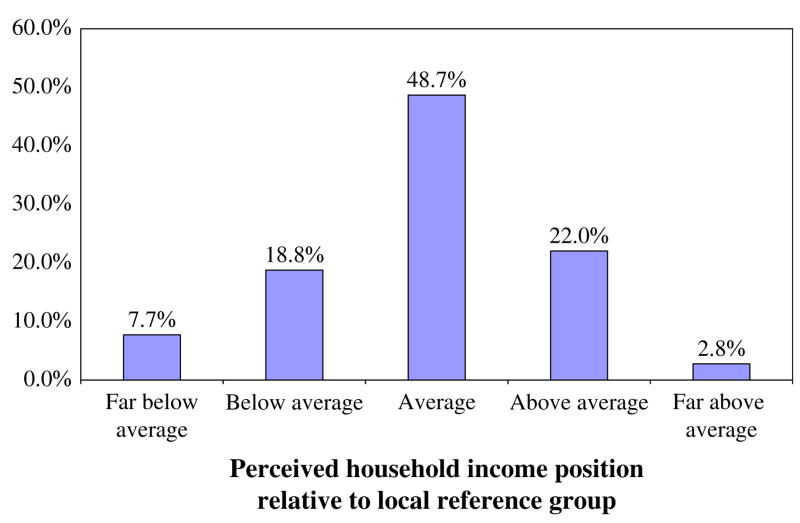
This paper uses a measure of local position reported by NSHAP. In the survey, the following question is asked: “Compared with most of the people you know personally, like your friends, family, neighbors, and work associates, would you say that your household income is far below average, below average, average, above average, or far above average?” Despite the ex ante suspicion that there might be very little variation in the responses to this question – perhaps everyone considers himself to be average – the histogram of responses (Fig. 1) shows a reasonable distribution. Moreover, although local relative position was positively correlated with income and assets, there was a wide range of assessments of local positions across the breadth of reported income and assets. For this paper, the answer to the above question is taken to be a measure of an individual’s economic position relative to his reference group.
Fig. 1.
Weighted distribution of perceived local relative position (asset sample).
Since there may be non-linearities in the association between relative position and health, I use 4 dummy variables based on the above 5-category measure for the main analysis. I create separate dummy variables for reporting having a household income “far below [the] average” of one’s local group, having an income “below average,” having an income “above average,” and having an income “far above average”. In this way, we will be able to distinguish whether being in a low position is associated with poor health (relative to being average) or being in a high relative position has a protective effect. This distinction is important because different mechanisms may be at work with low versus high relative positions.
Perception bias
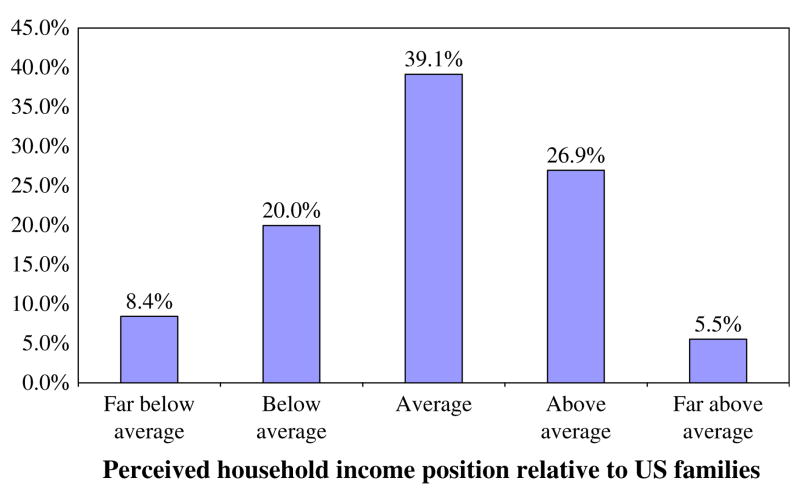
Now, if we believe that what matters for health is an individual’s perception of his relative position, then the above measure is the appropriate one. On the other hand, if the relative deprivation hypothesis is meant to explain the relationship between observed inequality and health, then we might care about an individual’s actual relative position. Although we have no direct information about someone’s local reference group, it might be possible to infer his actual relative position by using the answer to the above question and the answer to another, related survey question. In addition to the local relative position question, the survey asks: “Compared to American families in general, would you say that your household income is far below average, below average, average, above average, or far above average?” The distribution of responses to this question is shown in Fig. 2.
Fig. 2.
Weighted distribution of perceived U.S. relative position (asset sample).
The answers to the local position and U.S. position questions are positively but not perfectly correlated (ρ = 0.776). What is interesting is that, at every perceived U.S. position, there is a wide range of assessments of local positions (cross-tabulation available upon request). For example, among those who believe that they are above average among Americans, there are some who believe that they are at the bottom of their local reference group, others who believe they are at the very top of their local group, and others in the middle.
We can use the answer to this question about U.S. relative position to infer an individual’s actual local position. The obvious problem with accepting an individual’s perception of her local position as her actual position is that her responses may be biased; the respondent may be self-deprecating or grandiose in her assessment. One way to account for this bias is to compare the respondent’s assessment of her relative U.S. position to her actual U.S. position, the latter which we can determine because we know her household income. The degree to which respondents underestimate or overestimate their actual U.S. position is a measure of this bias, which I call the perception bias, in their economic self-assessment.
In more specific terms, the perception bias is calculated as follows. I use the distribution of responses to the U.S. relative income question to determine the percentiles that respondents are associating with the 5 classifications (far below average, below average, average, above average, far above average). According to the distribution of responses, “far below average” includes those from the 0th to approximately the 8th percentile, “below average” captures those from the 8th percentile to the 28th percentile, and so on (see Fig. 2). Now, using the actual distribution of household income, I identify the income thresholds corresponding to each of the 5 percentile groups. I then assign a U.S. relative rank based on respondents’ numerical income and the thresholds corresponding to the percentile groups. For example, if a respondent reports an income that is between the 8th and 28th percentile of the actual U.S. income distribution, she is assigned a rank of 2. The bias in respondents’ estimates of their economic position is their relative position as given by their answer to the U.S. relative income question, minus their actual U.S. income rank, i.e. rankperceived − rankactual. Thus, if a respondent who is in the 50th percentile group of the income distribution (rankactual = 3) claims he is far above the U.S. household average (rankperceived = 5), his bias is 5–3 = 2. Constructed in this way, the perception bias variable measures the difference between a respondent’s perceived relative income position among Americans and his actual relative income position. Of course, the effectiveness of this measure in adjusting for subjectivity depends on the degree to which grandiosity about one’s local position is similar in magnitude to grandiosity about one’s position among American households. On its face, this appears to be a not implausible assumption.
Measures of health status
Three different types of health measures are used. I first look at self-rated measures of physical well-being. I use the standard survey measure of self-rated physical health wherein respondents are asked to rate their physical health on a 5-point scale (“poor”, “fair”, “good”, “very good”, “excellent”). I also use a self-rated measure of functional health, which asks respondents to rate the difficulty they have in walking a block. For ease of interpretation, I dichotomize these two measures as, respectively, reporting bad health – rating physical health as “poor” or “fair” (versus not), and reporting any difficulty in walking a block (versus not).
In addition to these self-rated summary measures, I look at self-reports of clinically diagnosed health conditions. The survey asks the respondent to indicate whether she has ever been told by a doctor that she has a certain condition. In this paper, I focus on health conditions that are thought to be associated with biological stress responses, as well as on the leading causes of poor health in this age group. These conditions include cardiovascular morbidity (having had a heart attack or a stroke, having had treatment for heart failure, or having had leg artery bypass surgery), hypertension, diabetes, arthritis, cancer, and ulcers. I also use a summary index of disease burden, which is the total number of health conditions (from among a set list of conditions) that the respondent reports as having been diagnosed; this index, reported by NSHAP, is loosely based on the Charlson comorbidity index (Charlson, Pompei, Ales, & MacKenzie, 1987), and includes only those health conditions that have been shown to be predictive of mortality. The NSHAP Charlson-based index ranges from 0 conditions to 9 conditions.
Finally, I use two objective health measures: an obesity indicator based on anthropometric measurements and interviewer-recorded blood pressure readings. NSHAP reports the respondent’s height, weight, and waist circumference as measured by the interviewer. Height and weight are used to compute the respondent’s body mass index (BMI), and this index is used in conjunction with waist circumference to classify the respondent as obese or non-obese. The criteria used for obesity classification are those established by the National Heart, Lung, and Blood Institute (1998) and the World Health Organization (1995).
In addition to the obesity measure, I include several measures based on the blood pressure readings taken by the interviewer. I look at the individual systolic and diastolic blood pressure readings and also construct two dichotomous measures based on these readings. The first dichotomous measure indicates whether the respondent’s blood pressure would be considered hypertensive (a systolic pressure of greater than 140 mm Hg or a diastolic pressure of greater than 90 mm Hg), and the second measure indicates whether his measured blood pressure would be considered pre-hypertensive or hypertensive (a systolic blood pressure of greater than 120 mm Hg or a diastolic blood pressure of greater than 80 mm Hg). These obesity and blood pressure measures will give us health indicators that are not affected by respondent reporting.
Measure of self-esteem
One concern with simply regressing relative position on health status is the possibility of the omitted variable of negative disposition. One might imagine that an individual who has a negative psychological orientation might be more likely to report being in a low relative position and also more likely to have worse health.
There is no formal construct in the psychological literature that exactly corresponds to this idea, but the closest among commonly measured psychological constructs is self-esteem. Self-esteem refers to the positive evaluation of oneself in terms of one’s value or worth. One justification for using self-esteem as a measure of psychological attitude is that negativity specifically in relation to oneself is the aspect of personality and psychological orientation that would be most likely to affect relative position. NSHAP reports a single-item 5-point measure of self-esteem taken from the Rosenberg Self-Esteem Scale (Robins, Hendin, & Trzesniewski, 2001; Rosenberg, 1965). I use the responses to this item as a measure of psychological disposition that might influence both relative position and health.
Model estimation
Probit models were used for all health measures except for the models of the Charlson-based comorbidity index and of systolic and diastolic blood pressure. For these last three models (whose outcome variables have a wide range of values) OLS was used. In all models, weights adjusted for sampling and non-response were used, and standard errors were clustered to account for the sampling design. The base model estimated was:
| (1) |
where Healthi is the health status of individual i, RPi is the vector of relative position dummy variables, Incomei is the natural log of per capita household income (or assets), PerceptionBiasi is the perception bias measure, SelfEsteemi is the self-esteem measure, Demographici is a vector of demographic characteristics (age, race, gender, education, marital/cohabitation status, and partner’s education), and Φ indicates the cumulative distribution function of the normal distribution.
Results
Probit and OLS estimates
According to the probit and OLS estimates (Table 2), relative position is associated with certain self-reported morbid conditions; this association, however, appears limited to extreme relative positions. In particular, very low rank is associated with a higher Charlson index – that is, of reporting more health conditions predictive of mortality. At the other extreme, very high rank is associated with lower probabilities of reporting diagnoses of hypertension and diabetes. Neither moderately low nor moderately high relative positions are associated with any health measures.
Table 2.
Probit and OLS estimates of health in relation to local position and income.
| Health measure | Marginal effect or coefficient (standard error) |
||||
|---|---|---|---|---|---|
| Very low rank | Low rank | High rank | Very high rank | Income | |
| Self-rated physical health measures | |||||
| Poor or fair physical health (0 = excellent/very good/good, 1 = fair/poor) | 0.168* (0.082) | 0.091 (0.061) | −0.041 (0.047) | −0.028 (0.091) | −0.047** (0.018) |
| Difficulty in walking a block (0 = no difficulty, 1 = some diff/much diff/unable) | 0.126* (0.067) | 0.044 (0.039) | −0.052 (0.047) | −0.093 (0.065) | −0.043*** (0.015) |
| Self-reported morbidity | |||||
| Cardiovascular morbidity (0 = none, 1 = diagnosis) | 0.126 (0.078) | 0.040 (0.050) | −0.041 (0.048) | −0.066 (0.075) | −0.016 (0.019) |
| Hypertension (0 = none, 1 = diagnosis) | −0.037 (0.074) | −0.052 (0.053) | −0.056 (0.048) | −0.213** (0.088) | −0.005 (0.021) |
| Diabetes (0 = none, 1 = diagnosis) | 0.025 (0.056) | 0.007 (0.036) | 0.015 (0.028) | −0.122** (0.057) | −0.024 (0.016) |
| Arthritis (0 = none, 1 = diagnosis) | 0.134* (0.077) | 0.006 (0.052) | 0.003 (0.053) | −0.056 (0.126) | −0.011 (0.026) |
| Cancer (0 = none, 1 = diagnosis) | −0.015 (0.041) | 0.003 (0.030) | 0.019 (0.030) | 0.103 (0.065) | −0.003 (0.015) |
| Ulcer (0 = none, 1 = diagnosis) | 0.064 (0.051) | 0.041 (0.032) | 0.064 (0.043) | −0.067* (0.037) | −0.007 (0.014) |
| Charlson-based morbidity index (0, 1, 2, …, 9 conditions) | 0.657*** (0.151) | 0.261* (0.149) | 0.087 (0.099) | −0.082 (0.346) | −0.074 (0.057) |
| Interviewer-based measures | |||||
| Obese (0 = non-obese, 1 = obese) | −0.004 (0.079) | 0.035 (0.042) | 0.028 (0.062) | −0.014 (0.099) | −0.024 (0.023) |
| Systolic blood pressure (mm Hg) | 1.831 (3.228) | −1.091 (2.029) | 0.183 (1.435) | −3.506 (4.939) | 0.506 (0.867) |
| Diastolic blood pressure (mm Hg) | 0.949 (1.795) | −1.113 (1.010) | −0.186 (0.885) | −2.588 (2.110) | 0.005 (0.465) |
| Hypertensive based on BP, Pr{hypertensive} | −0.015 (0.090) | −0.049 (0.044) | −0.043 (0.045) | −0.195 (0.117) | 0.034 (0.025) |
| Pre-hypertensive or hypertensive based on BP, Pr{pre-hypertensive or hypertensive} | 0.045 (0.056) | −0.041 (0.058) | −0.023 (0.038) | −0.047 (0.070) | −0.004 (0.018) |
Significant at α = 0.01;
significant at α = 0.05;
significant at α = 0.10.
All regressions include age, age2, race, gender, education, marital/cohabitation status, partner’s education, log of per capita assets, and the self-esteem measure. Interviewer-based blood pressure regressions also include diagnosis of hypertension. All reported results are from probit regressions with the exception of results for the Charlson-based comorbidity index, systolic blood pressure, and diastolic blood pressure, which are from OLS regressions.
One interesting result is that, once we disaggregate health into individual conditions, the association between health and income is less evident. We observe an association with income for the two self-rated aggregate health measures, but not for individual health diagnoses, and not for the objective measures of obesity and blood pressure. One reason for this result may be that disaggregation of health conditions leads to too few cases for each condition to be able to discriminate any effect, especially if the effect size is small.
A second reason for the lack of association with income may be that, for this age group of 57–85, income may not be a good measure of material resources. Several studies (see for example, House, Kessler, & Herzog, 1990; Sorlie, Backlund, & Keller, 1995) have shown that the health-income gradient diminishes after middle-age; furthermore, for those who are at or near the end of their working lives, the stock of accumulated assets rather than the current flow of income may better reflect an individual’s material resources. Income is often used as a measure of resources because it is typically the only measure available in survey data; Robert and House (1996) have shown, however, that when both asset and income data are available, assets are more predictive of health status than income in older populations.
NSHAP is one of the few surveys that includes self-reported assets, so I repeat the above analysis conditioning on assets (Table 3). A potentially serious disadvantage of using assets rather than income, however, is a reduction in sample size. With income alone, the sample size is 1580 observations; with assets alone, the sample is reduced to 1408 observations. (A sample of both income and assets reduces the sample size even further to 1297 observations. The resultant standard errors are large, and I do not report the results for that analysis here.) I compute the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) for each of the models, first using income as the resource variable and then separately using assets. I find that all of the asset models strictly dominate the corresponding income models by both the AIC and BIC criteria (results available upon request), and so focus on the results from the asset models here.
Table 3.
Probit and OLS estimates of health in relation to local position and assets.
| Health measure | Marginal effect or coefficient (standard error) |
||||
|---|---|---|---|---|---|
| Very low rank | Low rank | High rank | Very high rank | Assets | |
| Self-rated physical health measures | |||||
| Poor or fair physical health (0 = excellent/very good/good, 1 = fair/poor) | 0.223*** (0.084) | 0.119* (0.070) | 0.000 (0.035) | −0.012 (0.114) | −0.012** (0.005) |
| Difficulty in walking a block (0 = no difficulty, 1 = some diff/much diff/unable) | 0.155*** (0.052) | 0.064** (0.031) | 0.019 (0.038) | −0.016 (0.083) | −0.025*** (0.007) |
| Self-reported morbidity | |||||
| Cardiovascular morbidity (0 = none, 1 = diagnosis) | 0.161** (0.063) | 0.028 (0.039) | −0.007 (0.037) | −0.023 (0.098) | 0.005 (0.008) |
| Hypertension (0 = none, 1 = diagnosis) | −0.030 (0.075) | −0.058 (0.052) | −0.032 (0.056) | −0.280*** (0.084) | −0.027** (0.011) |
| Diabetes (0 = none, 1 = diagnosis) | −0.008 (0.041) | −0.037 (0.037) | −0.010 (0.036) | −0.127** (0.053) | −0.015* (0.009) |
| Arthritis (0 = none, 1 = diagnosis) | 0.149* (0.079) | 0.008 (0.047) | 0.007 (0.047) | 0.042 (0.125) | −0.010 (0.010) |
| Cancer (0 = none, 1 = diagnosis) | 0.004 (0.045) | 0.013 (0.035) | 0.020 (0.026) | 0.093 (0.092) | −0.007 (0.005) |
| Ulcer (0 = none, 1 = diagnosis) | 0.054 (0.041) | 0.019 (0.030) | 0.048 (0.036) | −0.093*** (0.034) | −0.003 (0.005) |
| Charlson-based morbidity index (0, 1, 2, …, 9 conditions) | 0.632*** (0.156) | 0.178 (0.106) | 0.072 (0.082) | 0.079 (0.304) | −0.051* (0.029) |
| Interviewer-based measures | |||||
| Obese (0 = non-obese, 1 = obese) | −0.002 (0.068) | 0.055 (0.062) | 0.046 (0.046) | 0.014 (0.116) | −0.018 (0.016) |
| Systolic blood pressure (mm Hg) | 4.455 (3.547) | −1.669 (2.025) | 1.071 (1.298) | −1.015 (5.305) | 0.424* (0.242) |
| Diastolic blood pressure (mm Hg) | 1.125 (1.848) | −0.662 (1.864) | −0.260 (1.099) | −0.568 (0.837) | 0.093 (2.039) |
| Hypertensive based on BP, Pr{hypertensive} | 0.050 (0.067) | −0.047 (0.058) | −0.007 (0.048) | −0.089 (0.141) | 0.023** (0.010) |
| Pre-hypertensive or hypertensive based on BP, Pr{pre-hypertensive or hypertensive} | 0.104* (0.056) | −0.019 (0.031) | −0.013 (0.036) | −0.071 (0.100) | 0.005 (0.008) |
Significant at α = 0.01;
significant at α = 0.05;
significant at α = 0.10.
All regressions include age, age2, race, gender, education, marital/cohabitation status, partner’s education, log of per capita assets, and the self-esteem measure. Interviewer-based blood pressure regressions also include diagnosis of hypertension. All reported results are from probit regressions with the exception of results for the Charlson-based comorbidity index, systolic blood pressure, and diastolic blood pressure, which are from OLS regressions.
From Table 3, we see that we obtain similar results using assets as we do using income. All health measures that were related to relative position when we conditioned on income are also related when we condition on assets. Some results, such as those for cardiovascular morbidity and self-rated physical health and self-rated difficulty in walking a block, are more statistically significant. Notably, even though statistical power is in principle reduced with a smaller sample size (when we move from income to assets), the standard errors of the two sets of estimates are of similar sizes.
With the asset models, we see that only the extreme relative positions are strongly associated with health status. Very low relative position is associated with worse self-rated health and worse self-rated mobility; it is also associated with an increased probability of reporting cardiovascular morbidity and a higher Charlson morbidity index. At the other extreme, a very high position is associated with a decreased probability of reporting hypertension, a decreased probability of reporting diabetes, and a decreased probability of reporting an ulcer. In general, a very low relative position appears to increase the probability of reporting poor health or a morbid condition by between 16 and 22 percentage points; a very high relative position decreases the probability of reporting a morbid condition by between 9 and 28 percentage points.
Moderately low and moderately high positions are not linked to any health conditions except the self-rated mobility measure. In addition, there is no association between relative position and reports of arthritis or cancer, nor does there appear to be a relationship between relative position and obesity, nor between relative position and either systolic or diastolic blood pressure.
These results appear to be robust. I estimate each of the models with and without the perception bias and self-esteem measures, with and without state fixed effects, and with and without reweighting for non-response. The resultant estimates across the different specifications are similar to those reported in this paper and are available upon request.
Gender differences
The previous models control for gender differences through a gender dummy variable, but there may well be more complex differences in the relationship between relative position and health for men versus women (for a review of sex differences in mortality, morbidity, and physiological responses to stress, see Kudielka & Kirschbaum, 2004 and Waldron, 1983). To investigate this possibility, I re-estimate the models for males and females separately. Tables 4 and 5 report results for the male subsample and the female subsample, respectively.
Table 4.
Probit and OLS estimates of health in relation to local position and assets (male subsample).
| Health measure | Marginal effect or coefficient (standard error) |
||||
|---|---|---|---|---|---|
| Very low rank | Low rank | High rank | Very high rank | Assets | |
| Self-rated physical health measures | |||||
| Poor or fair physical health (0 = excellent/very good/good, 1 = fair/poor) | 0.387*** (0.145) | 0.136* (0.081) | 0.019 (0.045) | 0.040 (0.163) | −0.017*** (0.006) |
| Difficulty in walking a block (0 = no difficulty, 1 = some diff/much diff/unable) | 0.184 (0.116) | 0.018 (0.038) | −0.007 (0.038) | −0.051 (0.072) | −0.025*** (0.008) |
| Self-reported morbidity | |||||
| Cardiovascular morbidity (0 = none, 1 = diagnosis) | 0.129 (0.090) | 0.039 (0.054) | −0.016 (0.056) | 0.054 (0.163) | 0.006 (0.012) |
| Hypertension (0 = none, 1 = diagnosis) | −0.100 (0.127) | −0.111 (0.084) | −0.051 (0.064) | −0.285*** (0.109) | −0.030* (0.016) |
| Diabetes (0 = none, 1 = diagnosis) | −0.046 (0.069) | −0.020 (0.058) | 0.022 (0.045) | −0.085 (0.093) | −0.022* (0.013) |
| Arthritis (0 = none, 1 = diagnosis) | 0.203 (0.131) | 0.005 (0.084) | 0.032 (0.055) | −0.203 (0.170) | 0.002 (0.016) |
| Cancer (0 = none, 1 = diagnosis) | 0.016 (0.050) | 0.016 (0.033) | 0.088** (0.039) | 0.267* (0.146) | −0.004 (0.007) |
| Ulcer (0 = none, 1 = diagnosis) | −0.013 (0.059) | 0.003 (0.050) | 0.040 (0.045) | 0.003 (0.008) | |
| Charlson-based morbidity index (0, 1, 2, …, 9 conditions) | 0.704** (0.321) | 0.287 (0.192) | 0.241* (0.125) | 0.177 (0.485) | −0.045 (0.039) |
| Interviewer-based measures | |||||
| Obese (0 = non-obese, 1 = obese) | 0.106 (0.095) | 0.044 (0.098) | 0.067 (0.070) | 0.101 (0.159) | 0.002 (0.016) |
| Systolic blood pressure (mm Hg) | 8.620** (4.136) | −5.275*** (1.868) | 0.477 (2.271) | −0.383 (6.834) | 0.881** (0.422) |
| Diastolic blood pressure (mm Hg) | 4.029* (2.230) | −0.652 (1.123) | 0.911 (1.155) | 3.476 (2.551) | 0.342 (0.228) |
| Hypertensive based on BP, Pr{hypertensive} | 0.076 (0.082) | −0.102* (0.056) | 0.014 (0.078) | 0.038 (0.185) | 0.039** (0.018) |
| Pre-hypertensive or hypertensive based on BP, Pr{pre-hypertensive or hypertensive} | 0.139** (0.064) | −0.083* (0.050) | −0.024 (0.058) | −0.006 (0.103) | 0.018 (0.012) |
Significant at α = 0.01;
significant at α = 0.05;
significant at α = 0.10.
All regressions include age, age2, race, gender, education, marital/cohabitation status, partner’s education, log of per capita assets, and the self-esteem measure. Interviewer-based blood pressure regressions also include diagnosis of hypertension. All reported results are from probit regressions with the exception of results for the Charlson-based comorbidity index, systolic blood pressure, and diastolic blood pressure, which are from OLS regressions. Conditions for which there are no reported results mean that there is insufficient variation in the subsample to identify the parameter for this health condition.
Table 5.
Probit and OLS estimates of health in relation to local position and assets (female subsample).
| Health measure | Marginal effect or coefficient (standard error) |
||||
|---|---|---|---|---|---|
| Very low rank | Low rank | High rank | Very high rank | Assets | |
| Self-rated physical health measures | |||||
| Poor or fair physical health (0 = excellent/very good/good, 1 = fair/poor) | 0.114 (0.080) | 0.092 (0.063) | −0.031 (0.061) | −0.008 (0.007) | |
| Difficulty in walking a block (0 = no difficulty, 1 = some diff/much diff/unable) | 0.148** (0.075) | 0.114 (0.069) | 0.053 (0.057) | 0.022 (0.154) | −0.028** (0.012) |
| Self-reported morbidity | |||||
| Cardiovascular morbidity (0 = none, 1 = diagnosis) | 0.136** (0.066) | 0.004 (0.054) | 0.020 (0.046) | 0.002 (0.008) | |
| Hypertension (0 = none, 1 = diagnosis) | 0.037 (0.099) | 0.001 (0.103) | −0.011 (0.084) | −0.275** (0.136) | −0.020 (0.013) |
| Diabetes (0 = none, 1 = diagnosis) | 0.008 (0.046) | −0.062 (0.054) | −0.052 (0.062) | −0.008 (0.012) | |
| Arthritis (0 = none, 1 = diagnosis) | 0.085 (0.089) | 0.018 (0.079) | −0.044 (0.086) | 0.360*** (0.080) | −0.033* (0.020) |
| Cancer (0 = none, 1 = diagnosis) | −0.032 (0.044) | 0.006 (0.064) | −0.062 (0.038) | −0.013 (0.009) | |
| Ulcer (0 = none, 1 = diagnosis) | 0.071 (0.064) | 0.031 (0.041) | 0.050 (0.056) | −0.016 (0.085) | −0.011* (0.006) |
| Charlson-based morbidity index (0, 1, 2, …, 9 conditions) | 0.433* (0.217) | 0.010 (0.120) | −0.155 (0.197) | 0.053 (0.217) | −0.080* (0.043) |
| Interviewer-based measures | |||||
| Obese (0 = non-obese, 1 = obese) | −0.116 (0.103) | 0.081 (0.067) | 0.020 (0.077) | −0.072 (0.222) | −0.043 (0.026) |
| Systolic blood pressure (mm Hg) | 1.162 (4.327) | 2.787 (2.537) | 1.939 (1.881) | −1.200 (5.017) | −0.187 (0.383) |
| Diastolic blood pressure (mm Hg) | −1.636 (2.719) | −0.477 (1.465) | −1.438 (1.142) | −5.106** (2.262) | −0.172 (0.272) |
| Hypertensive based on BP, Pr{hypertensive} | 0.017 (0.111) | 0.027 (0.092) | −0.024 (0.080) | −0.242** (0.096) | 0.004 (0.013) |
| Pre-hypertensive or hypertensive based on BP, Pr{pre-hypertensive or hypertensive} | 0.038 (0.093) | 0.061 (0.056) | 0.008 (0.051) | −0.115 (0.198) | −0.022 (0.015) |
Significant at α = 0.01;
significant at α = 0.05;
significant at α = 0.10.
All regressions include age, age2, race, gender, education, marital/cohabitation status, partner’s education, log of per capita assets, and the self-esteem measure. Interviewer-based blood pressure regressions also include diagnosis of hypertension. All reported results are from probit regressions with the exception of results for the Charlson-based comorbidity index, systolic blood pressure, and diastolic blood pressure, which are from OLS regressions. Conditions for which there are no reported results mean that there is insufficient variation in the subsample to identify the parameter for this health condition.
Analyzing subsamples generates new methodological issues. Although the subsampling decreases the accuracy of some estimates because of smaller sample size (so that a loss of statistical significance with the subsamples may not be meaningful), it can be useful to look at the associations that persist or emerge as a result of the subsampling.
For both men and women separately, there remains a strong protective effect against hypertension when the respondents are of very high rank. In addition, for men, there remains a strong association between very low rank and poor self-rated health. For women, there remains a strong association between very low rank and self-rated mobility, as well as between very low rank and increased probability of cardiovascular morbidity.
In addition, we see for the first time associations between relative position and the objective measures. Women who are in very high positions have lower diastolic blood pressure readings and lower probabilities of having hypertensive blood pressure readings. Among men, we do not see a similar protective association with high rank, but we do observe a symmetric association with low rank. That is, men who report very low rank have higher systolic blood pressure readings and higher probabilities of having hypertensive blood pressure readings. For the blood pressure readings, then, we see a protective association with high rank in women and a deleterious association with low rank in men. These results suggest that, even for apparently the same health condition, the mechanism through which relative position operates could be very different for men and women.
Relative position and causality
In general, it is not possible to interpret the above estimates as unambiguously causal. This is so because reference groups (and consequently relative positions within these groups) are fundamentally endogenous. Put differently, individuals use, for their social comparisons, reference groups that are always at least partially chosen (although individuals may not choose their kin, they can and do choose their friends, and to a lesser degree, their co-workers and neighbors). The above estimates would only be causal if we believed that health and all other characteristics correlated with health were irrelevant for the choice of reference group (and position within that reference group). If we believe that health determines the choice of reference group, we have a reverse causality problem; if we believe that some other characteristic that is correlated with health affects the choice of reference group, we have an omitted variables’ problem.
Although I proxy for an important omitted variable – psychological disposition – the general problem of omitted variables and reverse causality remains. Even so, it is instructive to look at the statistical association between relative position and health. We are helped by the fact that the reverse causal story and many omitted variables’ stories suggest a clear direction of bias. Specifically, in thinking about reverse causality, we would expect that poor health leads to low relative position, and so if there were any reverse causality, there would be an upward bias in our estimate. Similarly, when we consider likely omitted variables – aspirational tendencies, preferences towards risk-seeking behaviors, low motivation, high discount rates –we might think that these omitted factors would bias our estimate upward.
Thus, one way in which these non-causal estimates might be helpful is that they suggest an upper bound on the causal effect coming through relative position. That is, we could assume hypothetically that there were no reverse causality or omitted variables and interpret the estimate as giving us the largest possible causal effect of relative position on health. In this way, we would be able to assess whether relative income, once we condition on absolute material resources, has the potential to have a large effect on health. If the estimate is large, we have reason to investigate further into the mechanisms underlying this potentially large effect. If, however, the upper bound estimate is small or zero (which I find for some health conditions and for some relative position statuses), this tells us that relative deprivation may not be an important mechanism underlying health disparities in these instances; we would then, for these particular cases, reasonably focus our efforts on investigating other mechanisms and causes of disparities.
In a similar way, we can look at patterns in the relationship between relative position and health even if the estimates are not causal. We might, for example, look at asymmetries. In particular, it might be possible that being in a low relative position has a negative effect on health relative to being in an average position, but being in a high relative position confers no protective effect relative to being in an average position. Or, as suggested by the foregoing analysis, relative position is relevant only if individuals are at the extreme ends of the relative position spectrum. Examining these asymmetries, even if the estimates are not causal, will help us to focus our attention on the social locations that have the potential for the greatest impact on health.
Finally, we can consider these estimates in the context of the biological theory underlying the relative deprivation hypothesis. The mechanism through which relative deprivation is conjectured to affect health is the chronic physiological stress induced by unfavorable social comparison. The stress hormones that are released trigger biological changes have been strongly linked to certain health conditions, while the evidence is mixed or narrower for the relationship between stress and other conditions. For example, there is strong evidence for cardiovascular disease resulting from the stress pathway (McEwen, 1998), but narrower evidence for cancer, with only some neoplasms appearing to be affected by psychosocial stress (Chida, Hamer, Wardle, & Steptoe, 2008). By examining the non-causal estimates for individual conditions, we can refine our views about the importance of the relative deprivation hypothesis for specific conditions.
Discussion
What do these results mean for the relative deprivation hypothesis? First, they are somewhat consistent with the hypothesis. We find that all three summary measures of health – the self-rated physical health measure, the self-rated mobility measure, and the comorbidity measure – are associated with very low position. In addition, we find that the two conditions most strongly linked to the conjectured stress mechanism of relative deprivation – cardiovascular morbidity and hypertension – are associated with relative position. Increased cardiovascular morbidity is associated with very low position, while a decreased probability of reporting hypertension is associated with very high position. We also find that very high position is associated with a lower probability of reporting diabetes.
On the other hand, there are ways in which these results appear to diverge from the predictions of the relative deprivation hypothesis. First, a lower probability of reporting having been diagnosed with an ulcer is associated with very high position. The causative agent behind most peptic ulcers is the bacterium Helicobacter pylori, and it is difficult to see how exposure to H. pylori might be associated with relative position. One possibility is that depressed immune function is associated with psychosocial stress, and this lowered immunity may well be associated with greater susceptibility to infection with H. pylori and a higher prevalence of ulcers among those in relatively low positions.
Second, we do not observe an association between relative position and obesity, even though increased visceral body fat is thought to be associated with physiological stress. One possible reason may be that the WHO BMI criteria for obesity are too crude to capture the anthropometric characteristics that are relevant for health. Some studies (see for example, Romero-Corral et al., 2006) have shown that the WHO obesity criteria do not discriminate health risks associated with body fat very well. We also do not observe an association between relative position and cancer, although this null result may be because the cancer measure aggregates many types of neoplasms, many of which may be insensitive to stress.
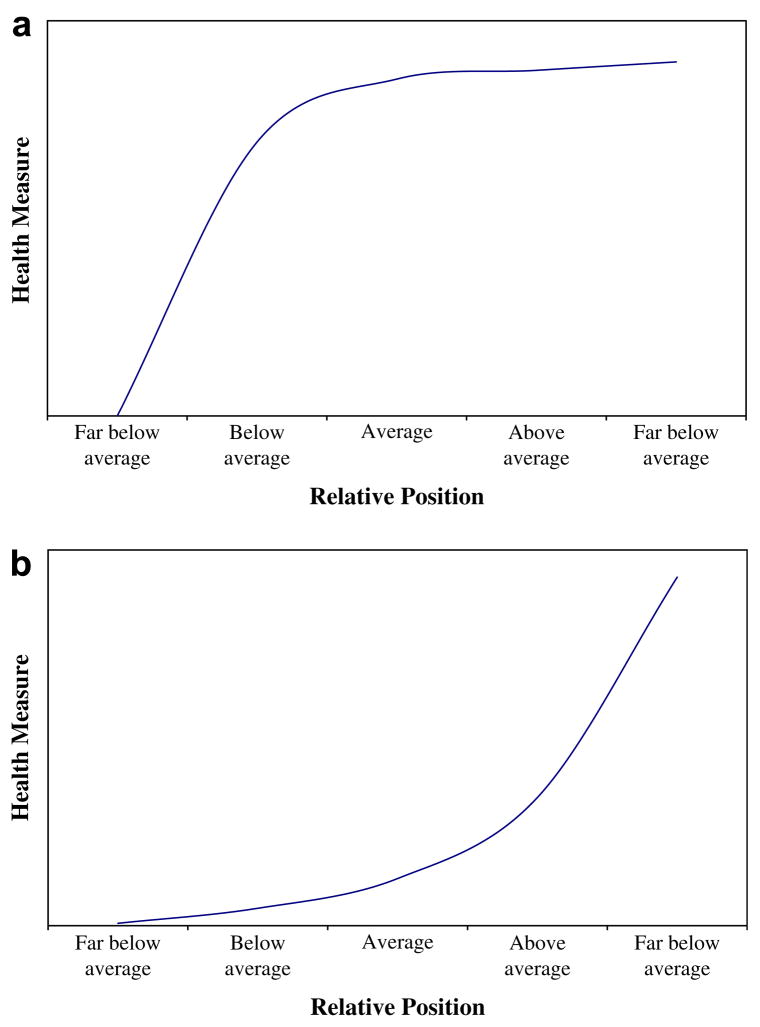
Interestingly, for health conditions for which we observe some relative position associations, there are strong non-linearities. For summary measures of health (self-rated health and mobility and the comorbidity index), there is a negative association between being of low position relative to the average, but (if interpreted causally) no protective effect of being above average. That is, there is a concave relationship between health and relative position for these summary measures (see Fig. 3a for a graphical representation of concavity). Similarly, we observe a concave relationship between cardiovascular health and relative position. On the other hand, there are other conditions – diabetes and ulcers – for which there appears to be a convex relationship. That is, there is no deleterious health effect of being in a below average position relative to being in an average position (see Fig. 3b for a graphical representation of convexity). These different concave and convex relationships for the various health conditions are not necessarily inconsistent with the relative deprivation hypothesis; since the precise biological mechanisms vary for the different conditions (and even across genders for the same conditions), it is not surprising that we observe different dose–response relationships vis-a-vis relative deprivation.
Fig. 3.
(a) Graphical representation of a concave relationship. (b) Graphical representation of a convex relationship.
These results are suggestive of a relative deprivation effect at the extremes, but there are a number of caveats that should be mentioned. First, the survey question asks about current relative income, and we might think that permanent relative income (relative position over the life cycle) is relevant for health (see for example, Reagan, Salsberry, & Olsen, 2007). In principle, we would like an average measure of relative position over individuals’ life cycles since current health status likely reflects lifetime stressors. It is not possible, however, to derive such a full life cycle measure with the cross-sectional NSHAP data set. Nevertheless, current relative position may be a reasonable measure of permanent position if we think that people tend to be consistent, over their life cycle, in their positions within their reference groups.
Do individuals move up or down within their reference groups as they age? On the one hand, individuals in this age group (57–85) have less current income since they are no longer working – but if their reference group consists of other individuals of the same age, everyone in the reference group also has less income, and so there is no unambiguous prediction about whether individuals’ relative positions within their reference group move up or down over the life cycle. On the other hand, if high relative position has a positive effect on health, and those of low relative position tend to die sooner, there will be selection in favor of those in high relative positions. These remaining (formerly high position) individuals will then regroup among themselves, and since not everyone can now be in a high position, there will be an average decline in relative position as individuals’ age. This story suggests that current relative position among this sample population tends to underestimate permanent relative position; since some high relative position individuals (with presumably good health) are misidentified as having lower relative position based on their current standing, the negative effect of low relative position on health may be underestimated (i.e. biased towards zero).
A second caveat is the possibility that many of these associations may reflect a reverse causal direction – with poor health causing relative position, and not relative position causing health, as conjectured by the relative deprivation hypothesis – or may reflect bias from omitted variables. As noted earlier, these problems may be fundamentally impossible to resolve, but the reported estimates could arguably be viewed as an upper bound of any existing causal effect. Interpreted as the upper bound of the effect of relative deprivation, these estimates suggest that the effect of relative income, independent of the health effect of absolute material means, is limited to the extreme positions (very high or very low), but is potentially large. Moreover, that the upper bound appears to be negligible for moderately low and moderately high relative positions for most conditions is evidence that relative deprivation is of much less importance for moderate-sized differences in relative position.
Since we observe strong associations between relative position and those health conditions that are thought to be influenced by position, the conjectured physiological basis of the relative deprivation hypothesis appears supported. What remains unclear, however, is how broad, relative to the theory, the effects of relative deprivation are within the population. Overall, this analysis suggests that there may very well be a biopsychological mechanism of social comparison that has deleterious effects on health, but its effects are limited to the very top or very bottom.
Acknowledgments
I thank Stacy Tessler Lindau, Sam Schulhofer-Wohl, Linda Waite, and three reviewers for helpful comments on an earlier draft. This research was supported by a National Institute on Aging predoctoral fellowship from the Center on Demography and Economics of Aging at NORC and the University of Chicago, a fellowship from the Chicago Center of Excellence in Health Promotion Economics, and by Grant 5R01AG021487 from the Office of the Demography of Aging, Behavioral and Social Research Program, National Institute on Aging. The National Social Life, Health, and Aging Project (NSHAP) is supported by the National Institutes of Health, including the National Institute on Aging, the Office of Women’s Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research (5R01AG021487).
Footnotes
More recently, the association between inequality and health has been questioned (see for example, Deaton, 2001, 2003; Deaton & Lubotsky, 2003; Deaton & Paxson, 2001a, 2001b; Lynch, Smith, Kaplan, & House, 2000; Miller & Paxson, 2006).
References
- Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health: no easy solution. Journal of the American Medical Association. 1993;269:3140–3145. [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nature Clinical Practice Oncology. 2008;5:466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- Cohen S, Line S, Manuck S, Rabin B, Heise E, Kaplan J. Chronic social stress, social status, and susceptibility to upper respiratory infections in nonhuman primates. Psychosomatic Medicine. 1997;59:213–221. doi: 10.1097/00006842-199705000-00001. [DOI] [PubMed] [Google Scholar]
- Daly MC, Duncan GJ, Kaplan GA, Lynch JW. Macro-to-micro links in the relation between income inequality and mortality. Milbank Quarterly. 1998;76:315–339. doi: 10.1111/1468-0009.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton A. Relative deprivation, inequality, and mortality. 2001 NBER working paper no. 8099. [Google Scholar]
- Deaton A. Health, inequality, and economic development. Journal of Economic Literature. 2003;41:113–158. [Google Scholar]
- Deaton A, Lubotsky D. Mortality, inequality, and race in American cities and states. Social Science & Medicine. 2003;56:1139–1153. doi: 10.1016/s0277-9536(02)00115-6. [DOI] [PubMed] [Google Scholar]
- Deaton A, Paxson C. Mortality, education, income and inequality among American cohorts. In: Wise D, editor. Themes in the economics of aging. Chicago: University of Chicago Press; 2001a. [Google Scholar]
- Deaton A, Paxson C. Mortality, income, and income inequality over time in Britain and the United States. 2001b NBER working paper no. 8534. [Google Scholar]
- Dressler WW, Balieiro MC, Ribeiro RP, Dos Santos JE. Cultural consonance and arterial blood pressure in urban Brazil. Social Science & Medicine. 2005;61:527–540. doi: 10.1016/j.socscimed.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Dressler WW, Bindon JR. The health consequences of cultural consonance: cultural dimensions of lifestyle, social support, and arterial blood pressure in an African American community. American Anthropologist. 2000;102:244–260. [Google Scholar]
- Dressler WW, Bindon JR, Neggers YH. Culture, socioeconomic status, and coronary heart disease risk factors in an African American community. Journal of Behavioral Medicine. 1998;21:527–544. doi: 10.1023/a:1018744612079. [DOI] [PubMed] [Google Scholar]
- Eibner C, Evans WN. Relative deprivation, poor health habits, and mortality. Journal of Human Resources. 2005;40:591–620. [Google Scholar]
- Fiscella K, Franks P. Poverty or income inequality as predictor of mortality: longitudinal cohort study. British Medical Journal. 1997;314:1724–1727. doi: 10.1136/bmj.314.7096.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank RH. Choosing the right pond: Human behavior and the quest for status. New York: Oxford University Press; 1985. [Google Scholar]
- Gravelle H, Sutton M. Income, relative income, and self-reported health in Britain (1979–2000) 2006 doi: 10.1002/hec.1354. Centre for Health Economics working paper no. 10. [DOI] [PubMed] [Google Scholar]
- House JS, Kessler RC, Herzog AR. Age, socioeconomic status, and health. Milbank Quarterly. 1990;68:383–411. [PubMed] [Google Scholar]
- Jaffe DH, Eisenbach Z, Neumark YD, Manor O. Individual, household and neighborhood socioeconomic status and mortality: a study of absolute and relative deprivation. Social Science & Medicine. 2005;60:989–997. doi: 10.1016/j.socscimed.2004.06.047. [DOI] [PubMed] [Google Scholar]
- Jones AM, Wildman J. Health, income and relative deprivation: evidence from the BHPS. Journal of Health Economics. 2008;27:308–324. doi: 10.1016/j.jhealeco.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. British Medical Journal. 1996;312:999–1003. doi: 10.1136/bmj.312.7037.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. British Medical Journal. 1996;312:1004–1007. doi: 10.1136/bmj.312.7037.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N, Kawachi I, Subramanian SV, Takeda Y, Yamagata Z. Do social comparisons explain the association between income inequality and health?: relative deprivation and perceived health among male and female Japanese individuals. Social Science & Medicine. 2008;67:982–987. doi: 10.1016/j.socscimed.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudielka B, Kirschbaum C. Sex differences in HPA axis responses to stress: a review. Biological Psychology. 2004;69:113–132. doi: 10.1016/j.biopsycho.2004.11.009. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. British Medical Journal. 2001;322:1233–1236. doi: 10.1136/bmj.322.7296.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annual Review of Sociology. 2001;27:415–444. [Google Scholar]
- Mellor J, Milyo J. Income inequality and health status in the United States: evidence from the current population survey. Journal of Human Resources. 2002;37:510–539. [Google Scholar]
- Merton RK. Social theory and social structure. New York: Free Press; 1957. [Google Scholar]
- Miller D, Paxson C. Relative income, race, and mortality. Journal of Health Economics. 2006;25:979–1003. doi: 10.1016/j.jhealeco.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Rockville, MD: National Institutes of Health; 1998. National Heart, Lung, and Blood Institute in Cooperation with National Institute of Diabetes and Digestive and Kidney Diseases. (NIH publication no. 98-4083) [Google Scholar]
- Reagan P, Salsberry PJ, Olsen RJ. Does the measure of economic disadvantage matter? Exploring the effect of individual and relative deprivation on intrauterine growth restriction. Social Science & Medicine. 2007;64:2016–2029. doi: 10.1016/j.socscimed.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert S, House JS. SES differentials in health by age and alternative indicators of SES. Journal of Aging and Health. 1996;8:359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg self-esteem scale. Personality and Social Psychology Bulletin. 2001;27:151–161. [Google Scholar]
- Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368:666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the self. New York: Basic Books; 1965. [Google Scholar]
- Sapolsky RM, Alberts SC, Altmann J. Hypercortisolism associated with social subordinance or social isolation among wild baboons. Archives of General Psychiatry. 1997;54:1137–1143. doi: 10.1001/archpsyc.1997.01830240097014. [DOI] [PubMed] [Google Scholar]
- Shively CA, Laber-Laird K, Anton RF. Behavior and physiology of social stress and depression in female Cynomolgus monkeys. Biological Psychiatry. 1997;41:871–882. doi: 10.1016/S0006-3223(96)00185-0. [DOI] [PubMed] [Google Scholar]
- Sorlie PD, Backlund E, Keller JB. U.S. mortality by economic, demographic, and social characteristics: the national longitudinal mortality study. American Journal of Public Health. 1995;85:949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm R, Gresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. British Medical Journal. 2002;324:1–5. doi: 10.1136/bmj.324.7328.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldmann RJ. Income distribution and infant mortality. Quarterly Journal of Economics. 1992;107:1283–1302. [Google Scholar]
- Waldron I. Sex differences in illness incidence, prognosis and mortality: issues and evidence. Social Science & Medicine. 1983;17:1107–1123. doi: 10.1016/0277-9536(83)90004-7. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG. Unhealthy societies: The afflictions of inequality. New York: Routledge; 1996. [Google Scholar]
- Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? British Medical Journal. 1997;314:591–595. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Social Science & Medicine. 2006;62:1768–1784. doi: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Physical status: The use and interpretation of anthropometry. Geneva, Switzerland: World Health Organization; 1995. WHO technical report series. [Google Scholar]
- Yngwe MA, Fritzell J, Lundberg O, Diderichsen F, Burstrom B. Exploring relative deprivation: is social comparison a mechanism in the relation between income and health? Social Science & Medicine. 2003;57:1463–1473. doi: 10.1016/s0277-9536(02)00541-5. [DOI] [PubMed] [Google Scholar]